Abstract
Objectives
To evaluate lipid profiles in subjects with preeclampsia. To determine if there is any change in lipid profiles in subject of preeclampsia as compared to normal antenatal females, non-pregnant females and post partum females.
Methods
Study was carried out on pregnant women and non pregnant women attending or admitted in the Obstetrics and Gynecology Department of SSG Hospital, Baroda between 1st June 2007 to 31st May 2008. Each serum sample from different groups was evaluated for Total cholesterol(mg/dl), Triglyceride (mg/dl), HDL-cholesterol (mg/dl), LDL-cholesterol (mg/dl) and VLDL-cholesterol (mg/dl) using diagnostic kits and a comparison drawn and analyzed using t-test and chi-square test.
Results
Dyslipidemia in the form of significantly decreased HDL concentration and significantly increased total cholesterol, LDL, VLDL & Triglycerides concentration is conspicuously evident in subjects of preeclampsia as compared to non pregnant, normotensive pregnant and postpartum subjects.
Conclusion
Dyslipidemia is significantly evident in preeclampsia and plays an important pathological role. The various causative factors for dyslipidemia and its prevention need to be further studied and evaluated.
Keywords: Lipid Profile, Preeclampsia
Introduction
Preeclampsia is a pregnancy specific condition characterized by hypertension and proteinuria that remits after delivery. It is a characteristic multisystem disorder of pregnancy, is one of the most common complications of pregnancy and is a leading cause of maternal and perinatal morbidity and mortality [1].
Preeclampsia occurs in 7–10% of pregnancies world wide [2]. In India, the national incidence is reported to be 8–10% of pregnancies.
The etiology of preeclampsia is still unknown. The hypotheses currently accepted are the placental ischemia hypothesis, genetic hypothesis, the immune maladaptation and hypothesis of the imbalance between free oxygen radicals and scavengers in favour of oxidants. At present, the most popular is the theory of oxidative stress. Abnormal lipid profiles and species may have a role in the promotion of oxidative stress and vascular dysfunction seen in preeclampsia. Predominantly the atherogenic small low density lipoproteins (LDL) and the Vascular Cell Adhesion Molecules (VCAM) are increased in association with hyperlipidemia in preeclampsia. Although there is growing evidence indicating that the risk of preeclampsia is increased in women with elevated levels of oxidized low density lipoproteins and triglycerides [3], the causal relationship of lipid peroxidation in the pathogenesis of preeclampsia is not clear.
The study is designed to evaluate the changes in lipid profile that develops during normal pregnancy and preeclampsia.
Materials and Methods
The present clinical study “Lipid profile estimation in subjects of preeclampsia” was a case control study carried out on pregnant women and non pregnant women attending or admitted in the Obstetrics and Gynecology Department of SSG Hospital, Baroda. The study was carried out over a period of 1 year starting from 1st June 2007 to 31st May 2008. Women were placed in following 4 groups:
Group A—Non-pregnant normotensive (Normal women of peak childbearing age 19–35).
Group B—Pregnant women without preeclampsia between 32 and 36 weeks of gestation presenting immediately following the ‘cases’.
Group C—Antenatal subjects of gestational age between 32 and 36 weeks with mild/severe preeclampsia. This group constitutes ‘cases’. (Blood pressure >140/90 mmHg, with proteinuria, with or without pathological oedema).
Group D—Post partum preeclamptic women {15 or more days after delivery}
5 ml venous blood samples were drawn from all subjects under all aseptic precautions.
Those who had Diabetes mellitus, Chronic hypertension, Hepatitis, Medical disorders like renal disease, thyroid disease, collagen vascular disease, Hemoglobin <8 g%, BMI >30, Patients treated for PCOS in past and eclampsia were excluded from the study.
After collection of blood sample, the blood was allowed to clot (for 10 min) and serum was separated by centrifugation at 2500 rpm for 20 min. Each serum sample from different groups was evaluated for the following parameters using diagnostic kit.
Total cholesterol(mg/dl)
Triglyceride (mg/dl)
HDL-cholesterol (mg/dl)
Additional two parameters were calculated using Friedewald formula.
LDL-cholesterol (mg/dl)
VLDL-cholesterol (mg/dl)
The results in each parameter under study were graded as follows:
| Non-significant (NS) | P > 0.05 |
| Significant | P < 0.05 |
| Significant | P < 0.01 |
| Highly Significant | P < 0.001 |
Tests applied
‘t’ Test (Parameter)
χ2 Test (Chi-square test) (Non-concentric)
Results
Age (in years)
In the study, women in reproductive age group that is between 19 and 35 years were included. The age-wise distribution of subjects in various groups is shown in Table 1. Maximum subjects in each group were between 19 and 26 years as this is the peak child bearing age at our set up.
Table 1.
Age-wise distribution of subjects in various groups
| Age | Group | |||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | |||||
| No. | % | No. | % | No. | % | No. | % | |
| 19–22 | 9 | 18 | 18 | 36 | 26 | 52 | 24 | 48 |
| 23–26 | 13 | 26 | 19 | 38 | 17 | 34 | 18 | 36 |
| 27–30 | 17 | 34 | 11 | 22 | 6 | 12 | 7 | 14 |
| 31–34 | 10 | 20 | – | – | – | – | – | – |
| 35 | 1 | 2 | 2 | 4 | 1 | 2 | 1 | 2 |
Religion
As our hospital is located in a Hindu dominated area, maximum subjects were Hindu only with few being Muslims or Nepali. The distribution of Religion amongst various groups was not significant.
The incidence of Religion was statistically not significant (P > 0.05 by Chi-Square Test) (Table 2).
Table 2.
Distribution of religion in the groups
| Religion | Group | |||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | |||||
| No. | % | No. | % | No. | % | No. | % | |
| Hindu | 47 | 94 | 44 | 88 | 46 | 92 | 46 | 92 |
| Muslim | 3 | 6 | 6 | 12 | 3 | 4 | 3 | 6 |
| Nepali | – | – | – | – | 1 | 2 | 1 | 2 |
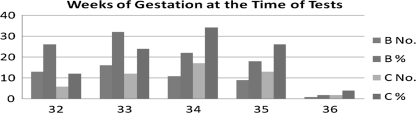
Weeks of gestation at the time of tests
The subjects between 32 and 36 weeks of gestation (late third trimester) were selected for the study and all the parameters were checked on a single visit. The week wise distribution pattern of all pregnant subjects (group B & C) is given in Fig. 1. Maximum proportion (32%) of subjects in group B were at 32 weeks and in group C (34%) were at 33 weeks of gestation.
Fig. 1.
Weeks of gestation at the time of test
There was no statistically significant difference in the two groups based on the weeks of gestation (by Chi-Square Test P > 0.05)
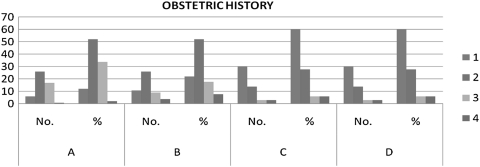
Obstetric history
The obstetric history of subjects in test group as well as control group was studied and it was observed that preeclampsia is significantly more common in primigravida females. Of the 50 preeclamptic subjects included in this study, as high as 60% were primigravida (Fig. 2).
Fig. 2.
Obstetric history of subjects in study groups
Specific investigations
Total cholesterol (Mg/dl)
Table 3 shows the mean total cholesterol values in all the four groups. In my study, the total cholesterol increased significantly during pregnancy from the non pregnant state. That is further significant increase in Preeclamptic females as compared to n pregnant females & it starts falling again post partum.
Table 3.
Mean total cholesterol levels in the study groups
| A | B | C | D | |
|---|---|---|---|---|
| Mean ± SEM | 216.4 ± 2.8 | 219.1 ± 3.1 | 232.0 ± 2.9 | 230.1 ± 2.6 |
The significant values for A & B, A & C, A & D, B & D and C & D are P < 0.001. Also for B & C it is P < 0.01
High density lipoprotein (Mg/dl)
Comparing the mean HDL levels in all the four groups, there is a significant increase of HDL level in normal pregnancy compared to the non pregnant state. But its level falls highly significantly in Preeclampsia which may be a reason for the atherosclerosis like features mentioned in Preeclampsia in some studies. It again begins to rise post partum (Table 4).
Table 4.
Mean HDL concentration in subjects of all groups
| A | B | C | D | |
|---|---|---|---|---|
| Mean ± SEM | 46.38 ± 1.01 | 60.3 ± 1.2 | 42.1 ± 1.9 | 44.4 ± 1.2 |
The significant values for A & B, A & C, A & D, B & C, B & D and C & D are P < 0.001
Low density lipoprotein (LDL) (Mg/dl)
Table 5 shows the mean LDL values in the four groups. It was found in the study that LDL concentration increase significantly during pregnancy compared to non pregnant females. It increased further significantly in preeclamptic females as compared to normal pregnant females. Post partum the LDL concentration again started falling. LDL is considered to be the most harmful lipoprotein.
Table 5.
Mean LDL concentrations in the study groups
| A | B | C | D | |
|---|---|---|---|---|
| Mean ± SEM | 105.7 ± 3.19 | 115.7 ± 3.4 | 135.8 ± 4.1 | 121.2 ± 2.8 |
The significant values for A & B, A & C, A & D, B & C, B & D and C & D are P < 0.001
Very low density lipoprotein (VLDL) (Mg/dl)
Table 6 gives the mean VLDL concentration in all the four groups under study. The VLDL concentration follows the same pattern as LDL. It increases during pregnancy compared to nonpregnant-females. In preeclampsia, there is further significant increase which begins to fall post partum.
Table 6.
Mean VLDL concentrations in the various study groups
| A | B | C | D | |
|---|---|---|---|---|
| Mean ± SEM | 24.37 ± 0.34 | 43.04 ± 0.40 | 54.1 ± 0.31 | 44.9 ± 1.1 |
The significant values for A & B, A & C, A & D, B & C, B & D and C & D are P < 0.001
Triglyceride (mg/dl)
On calculating the mean Triglyceride concentration in all the four groups and comparing, we found that it is significantly more in pregnant females as compared to non pregnant females. In preeclampsia, there is further significant increase than the normal pregnant females. The Triglyceride concentration again falls post partum (Table 7).
Table 7.
Mean triglyceride concentration in the study groups
| A | B | C | D | |
|---|---|---|---|---|
| Mean ± SEM | 121.8 ± 1.7 | 215.2 ± 1.9 | 270 ± 2.1 | 216 ± 1.2 |
The significant values for A & B, A & C, A & D, B & C, B & D and C & D are P < 0.001
Discussion and analysis
In this study, conducted over a period of one year, all the four groups were comparable in terms of age, religion and socio economic status. The two pregnant groups were also carefully chosen at same gestational period. The single most important predisposing factor that came up was the first pregnancy (primigravida).
Preeclampsia is a complex pathophysiological state where regulatory systems of inflammation and endothelial function are stimulated beyond the physiological limits of normal pregnancy. There is increasing evidence that lipids may play an important role in the modifications of the endothelial structure and function.
Different lines of evidence indicate that abnormal lipid metabolism is not a mere manifestation but is also involved in the pathogenesis of disease. High density lipoprotein is one of the four major plasma lipoprotein classes that are involved in lipid metabolism and the exchange of cholesterol, cholesterol esters and triacylglycerols between tissues. One function of HDL cholesterol is to facilitate reverse cholesterol transport by carrying excess, potentially harmfully cholesterol from peripheral tissues to the liver, where it can be excreted. In addition, it is involved in activating lipoprotein which releases fatty acids that can be oxidized by the B-oxidation pathway to provide energy. Low levels of HDL-Cholesterol may compromise the function of all these processes. In this study, preeclamptic pregnant female have been found to have highly significantly (P < 0.001) deceased levels of HDL cholesterol than the normal pregnant females & the nonpregnant females. Its level started increasing post partum. This is in consistency with the results of several other studies. In a study of portuguese women, subjects with preeclampsia had a lower HDL cholesterol level compared with healthy pregnant women. Another study conducted at Turkey showed significantly lower HDL-cholesterol levels in preeclamptic females than in normal pregnant women. Similarly, Rubin Aziz & Tabassum Mehboob conducted study & concluded that HDL-cholesterol decreased significantly in preeclampsia.
The concentration of total cholesterol, LDL, VLDL & Triglycerides was found to be significantly increased in preeclamptic females as compared to normal pregnant females & the non-pregnant females. All of these again started to fall post partum. Elevated triglyceride values may compromise vascular function in several ways. For example, triglyceride rich lipoprotein has a prothrombotic activity. Elevated triglycerides might shift the pattern of LDL subclass towards disproportionate increase in smaller denser, more allergenic LDL particles .
The association of LDL concentration with preeclampsia is biologically plausible. It has been shown that LDL (specially oxidized LDL) increases artery sensitivity to presser agents and inhibits endothelial-dependant vasodilatation.
The Dyslipidemia noted in the study is consistent with many studies conducted world wide over the years. Hubel et al. concluded that ante partum serum triglyceride & free fatty acid concentrations were increased approximately two fold in women with preeclampsia relative to uncomplicated pregnancies may contribute to endothelial cell dysfunction in preeclampsia. One study found that women with preeclampsia had 10.4, 13.6 and 15.5% higher concentrations of LDL cholesterol, triglycerides and LDL/HDL ratios and 7.0% lower HDL cholesterol. It also stated that early pregnancy dyslipidemia is associated with increased risk of preeclampsia. Belo et al. in their study concluded that preeclamptic women exhibited, in third trimester, higher mean serum triglyceride concentration and lower high density lipoprotein cholesterol [4]. They emphasized that this ‘atherogenic’ lipid profile in preeclamptic females may be a potential contributor to endothelial cell dysfunction. In India, Usha Adiga et al. conducted study at Mangalore which showed 20% increased in total cholesterol, 27% decreased in HDL cholesterol levels [5]. They also stated that hypercholesterolemia promoted the formation of free radicals.
Thus, considering the results in this study correlating with the various other studies throughout the world, it can safely be concluded that Dyslipidemia is significantly evident in preeclampsia and plays an important pathological role. The various causative factors for dyslipidemia and its prevention need to be further studied and evaluated.
References
- 1.Vanderjagt DJ. HDL & homocysteine levels correlate inversely in preeclamptic women in North Nigeria. Acta Obstet Gynecol Scand. 2004;83:536–542. doi: 10.1111/j.1600-0412.2004.00513.x. [DOI] [PubMed] [Google Scholar]
- 2.Mutlu Turkoglu U, Ademoglu E. Imbalance between lipid peroxidation, antioxidant status in preeclampsia. Gynecol Obstet Invest. 1998;46:37–40. doi: 10.1159/000009994. [DOI] [PubMed] [Google Scholar]
- 3.Qiu C, Phung TT, Vadachkoria T, et al. Oxidised low density lipoprotein and the risk of Preeclampsia. Physiol Res. 2005. [DOI] [PubMed]
- 4.Belo L, Caslake M, Gaffney D, et al. Changes in LDL size & HDL concentration in normal and preeclamptic pregnancies. Atherosclerosis. 2002;162(2):425–432. doi: 10.1016/S0021-9150(01)00734-1. [DOI] [PubMed] [Google Scholar]
- 5.Adiga U, D’souza V, Kamath A, et al. Antioxidant activity, lipid peroxidation in preeclampsia. J Chin Med. 2007;70:10. doi: 10.1016/S1726-4901(08)70034-0. [DOI] [PubMed] [Google Scholar]