Introduction
Synovitis (inflammation of the synovial lining) is increasingly recognized as a characteristic of the osteoarthritic joint. Over the past decade, many have documented that synovitis is present in various stages of the disease and is detectable by advanced imaging techniques [3], the presence of soluble mediators [5], or histopathologic assessment [9]. Despite using different methods of detection and different outcome measurements, studies from these multiple research groups have often led to similar conclusions.
Synovitis and Clinical Severity of OA
Synovial inflammation detectable by magnetic resonance imaging (MRI) [3] or histopathologic analysis of synovial tissues [11] is associated with greater levels of pain and joint symptoms in osteoarthritis (OA) and post-injury patients. A recent systematic review of MRI investigation of knee osteoarthritis suggested that this relationship is moderate to strong [4]. Consistent with the imaging studies, Ishijima et al. demonstrated that a systemic biomarker of synovial inflammation (sHA) is also associated with increased pain in patients with osteoarthritis [5]. Others have demonstrated that osteoarthritis patients with moderate to marked synovitis have decreased functional capacity measured objectively by timed walking and stair climbing [13]. Furthermore, when defined either by MRI [10] or intra-operative appearance at arthroscopy [2], synovial inflammation was associated with more rapid progression of cartilage degeneration. Its severity increases with increasing radiographic grade (Kellgren–Lawrence score) [6].
Histopathologic Analysis of Synovitis in OA
Histopathologic analysis of synovitis in osteoarthritis has demonstrated variability in the synovial response. At the cellular level, synovial infiltration by lymphocytes and macrophages occurs in both early and advanced diseases [8]. The perivascular cellular infiltrates within the synovial membrane of patients undergoing meniscectomy for meniscal tears are associated with greater levels of pain and joint symptoms measured by the Lysholm score [11]. The majority of these patients had intra-operative evidence of early osteoarthritis cartilage changes, even in the absence of radiographic abnormality. This is consistent with reports in established osteoarthritis patients and suggests that synovitis has important clinical implications at early, “pre-clinical” stages of disease. Other changes such as synovial lining hyperplasia and increased vascularity are also observed and often included in summed histologic scores of “inflammation” [9]. Whether these varying patterns of synovial histopathologic change reflect different molecular mechanisms, different stages of the inflammatory process, or have the same impact on disease progression and symptomatology, are important questions that remain.
Inflammatory Cytokines and Synovitis
Soluble inflammatory mediators produced within the osteoarthritic joint are diverse. Although IL-1, TNF-α, and TGF-β are the most widely studied cytokines in osteoarthritis pathogenesis, other mediators warrant discussion. Our group demonstrated that IL-15 levels in synovial fluid were associated with CD8+ infiltration of the synovial membrane and were detectable in the majority of knee osteoarthritis patients even in early-stage disease [12]. IL-15, a common-γ chain cytokine, had previously been associated with development of radiographic osteoarthritis [7]. In meniscectomy patients with intra-operative evidence of early-stage osteoarthritis, synovial expression of an additional set of chemokines and receptors (IL-8, CCL5, CCL19, CCR7) was associated with histologic synovitis [11]. These chemokines are involved in leukocyte recruitment and activation and may be potential targets in future efforts to block development or progression of synovitis in osteoarthritis patients.
Summary
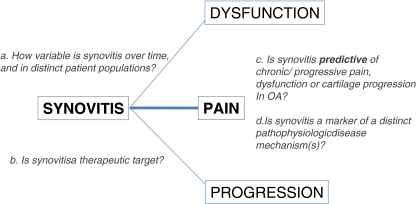
Our current understanding of the role of synovitis in osteoarthritis has evolved substantially over the past decade. We understand that inflammation is present even early in the course of the disease and is associated with symptoms, function, and progression of cartilage damage (Fig. 1). Whether synovitis is a predictive marker in posttraumatic osteoarthritis remains to be established. Data from a recently published rodent model suggested that synovitis may be a good therapeutic target in posttraumatic osteoarthritis [1]. Elucidating how synovial inflammation is triggered and sustained in the joint is likely to guide the design of future treatment regimens targeting synovitis in osteoarthritis.
Fig. 1.
Relationship between synovitis and outcomes in osteoarthritis and important remaining questions. Synovitis has been associated with pain, joint dysfunction, and rate of structural progression in osteoarthritis. Important questions remaining are how variable synovitis is in this setting, if synovitis is a therapeutic target, and whether synovitis is predictive of disease course or a marker of a distinct disease phenotype
Acknowledgement
Carla R. Scanzello is supported by 1K08AR057859 award from the National Institute of Arthritis, Musculoskeletal and Skin Diseases. Rush University Medical Center and the Hospital for Special Surgery have filed a patent application on behalf of the author on inflammatory biomarkers in osteoarthritis.
References
- 1.Ashraf S, Mapp PI, Walsh DA. Contributions of angiogenesis to inflammation, joint damage, and pain in a rat model of osteoarthritis. Arthritis Rheum. 2011;63:2700–2710. doi: 10.1002/art.30422. [DOI] [PubMed] [Google Scholar]
- 2.Ayral X, Pickering EH, Woodworth TG, Mackillop N, Dougados M. Synovitis: a potential predictive factor of structural progression of medial tibiofemoral knee osteoarthritis – results of a 1 year longitudinal arthroscopic study in 422 patients. Osteoarthritis Cartilage. 2005;13:361–367. doi: 10.1016/j.joca.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Guermazi A, Roemer FW, Hayashi D, Crema MD, Niu J, Zhang Y, Marra MD, Katur A, Lynch JA, El-Khoury GY, Baker K, Hughes LB, Nevitt MC, Felson DT. Assessment of synovitis with contrast-enhanced MRI using a whole-joint semiquantitative scoring system in people with, or at high risk of, knee osteoarthritis: the MOST study. Ann Rheum Dis. 2011;70:805–811. doi: 10.1136/ard.2010.139618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter DJ, Zhang W, Conaghan PG, Hirko K, Menashe L, Reichmann WM, Losina E. Responsiveness and reliability of MRI in knee osteoarthritis: a meta-analysis of published evidence. Osteoarthritis Cartilage. 2011;19:589–605. doi: 10.1016/j.joca.2010.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishijima M, Watari T, Naito K, Kaneko H, Futami I, Yoshimura-Ishida K, Tomonaga A, Yamaguchi H, Yamamoto T, Nagaoka I, Kurosawa H, Poole RA, Kaneko K. Relationships between biomarkers of cartilage, bone, synovial metabolism and knee pain provide insights into the origins of pain in early knee osteoarthritis. Arthritis Res Ther. 2011;13:R22. doi: 10.1186/ar3246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krasnokutsky S, Belitskaya-Levy I, Bencardino J, Samuels J, Attur M, Regatte R, Rosenthal P, Greenberg J, Schweitzer M, Abramson SB, Rybak L. Quantitative magnetic resonance imaging evidence of synovial proliferation is associated with radiographic severity of knee osteoarthritis. Arthritis Rheum. 2011;63:2983–2991. doi: 10.1002/art.30471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ling SM, Patel DD, Garnero P, Zhan M, Vaduganathan M, Muller D, Taub D, Bathon JM, Hochberg M, Abernethy DR, Metter EJ, Ferrucci L. Serum protein signatures detect early radiographic osteoarthritis. Osteoarthritis Cartilage. 2009;17:43–48. doi: 10.1016/j.joca.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pearle AD, Scanzello CR, George S, Mandl LA, DiCarlo EF, Peterson M, Sculco TP, Crow MK. Elevated high-sensitivity C-reactive protein levels are associated with local inflammatory findings in patients with osteoarthritis. Osteoarthritis Cartilage. 2007;15:516–523. doi: 10.1016/j.joca.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Pessler F, Dai L, Diaz-Torne C, Gomez-Vaquero C, Paessler ME, Zheng DH, Einhorn E, Range U, Scanzello C, Schumacher HR. The synovitis of "non-inflammatory" orthopaedic arthropathies: a quantitative histological and immunohistochemical analysis. Ann Rheum Dis. 2008;67:1184–1187. doi: 10.1136/ard.2008.087775. [DOI] [PubMed] [Google Scholar]
- 10.Roemer FW, Zhang Y, Niu J, Lynch JA, Crema MD, Marra MD, Nevitt MC, Felson DT, Hughes LB, El-Khoury GY, Englund M, Guermazi A. Tibiofemoral joint osteoarthritis: risk factors for MR-depicted fast cartilage loss over a 30-month period in the multicenter osteoarthritis study. Radiology. 2009;252:772–780. doi: 10.1148/radiol.2523082197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scanzello CR, McKeon B, Swaim BH, DiCarlo E, Asomugha EU, Kanda V, Nair A, Lee DM, Richmond JC, Katz JN, Crow MK, Goldring SR. Synovial inflammation in patients undergoing arthroscopic meniscectomy: molecular characterization and relationship to symptoms. Arthritis Rheum. 2011;63:391–400. doi: 10.1002/art.30137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scanzello CR, Umoh E, Pessler F, Diaz-Torne C, Miles T, Dicarlo E, Potter HG, Mandl L, Marx R, Rodeo S, Goldring SR, Crow MK. Local cytokine profiles in knee osteoarthritis: elevated synovial fluid interleukin-15 differentiates early from end-stage disease. Osteoarthritis Cartilage. 2009;17:1040–1048. doi: 10.1016/j.joca.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Sowers M, Karvonen-Gutierrez CA, Jacobson JA, Jiang Y, Yosef M. Associations of anatomical measures from MRI with radiographically defined knee osteoarthritis score, pain, and physical functioning. J Bone Joint Surg Am. 2011;93:241–251. doi: 10.2106/JBJS.I.00667. [DOI] [PMC free article] [PubMed] [Google Scholar]