Introduction
Osteoarthritis (OA) is the most common form of arthritis and is a major cause of morbidity, limitation of physical activity, and health care utilization, especially in people aged 45 and above [1]. OA has been defined as “… a progressive disease of synovial joints that represents failed repair of joint damage. This ultimately results in the breakdown of cartilage and bone, leading to symptoms of pain, stiffness, and functional disability” [2]. The term “degenerative joint disease (DJD)” should not be used by health care practitioners to describe this entity; it is a misnomer and suggests to patients that nothing can be done for their condition. Thus, OA can be considered as a disease characterized by structural abnormalities at the joint level and an illness defined by a person’s symptoms [2]. The symptoms that characterize knee OA include frequent pain, aching or discomfort, stiffness, fatigue, and sleep disturbance. These symptoms result in functional limitations leading to reduced participation in activities and decreased health-related quality of life.
OA’s Impact on Health and Quality of Life
Health care practitioners must recognize that OA is associated with increased mortality and reduced health-related quality of life [3–5]. Losina and colleagues [4] reported earlier this year that obesity and osteoarthritis combine to reduce quality-adjusted life years (QALYs) due to disability and mortality; this finding ranged from 1.86 QALYs lost in nonobese persons with knee OA to 3.5 QALYs lost in persons affected by both conditions. Losses were disproportionately higher in black and Hispanic women. Nuesch and colleagues [5] extended results of a prior systematic review and best evidence synthesis to show that persons with symptomatic hip or knee OA had 55% greater all-cause mortality compared with the general population and that a history of walking disability was associated with excess all-cause mortality and mortality due to cardiovascular disease, even after adjustment for age and sex.
As no curative therapies for OA exist at this time, health care providers must recognize that management of OA should be directed toward control of pain and other symptoms, reduction in functional limitation, and improvement in health-related quality of life [6, 7]. Patient complaints need to be taken seriously and not dismissed as an inevitable consequence of aging. As Professor Kraus said to Dr. Kusevitsky, “If there is one thing a patient expects from his physician, it is gravitas” [8]. Current recommendations suggest that patients receive a combination of non-pharmacologic and pharmacologic modalities, with consideration being given not only to the efficacy and safety/tolerability but also to the cost–benefit of treatments.
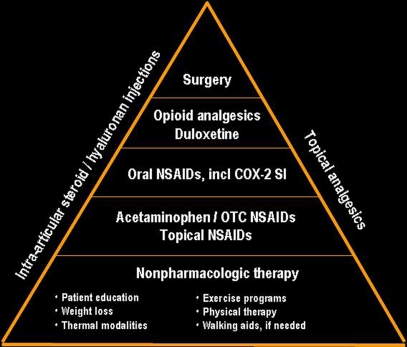
Table 1 lists non-pharmacologic and pharmacologic modalities recommended for the management of patients with symptomatic OA. A “pyramid” approach to management is advocated which begins with non-pharmacologic modalities and adds pharmacologic therapy as necessary; patients who fail to respond to medical management are referred for surgery as appropriate (Fig. 1). Despite the large number of available treatments, a large unmet need remains for safe, tolerable, efficacious medications, particularly for those patients who are intolerant of and/or have contraindications to non-steroidal anti-inflammatory drugs and opioid analgesics. Patients with symptoms that are not satisfactorily controlled by medical therapy are considered candidates for total joint replacement; indeed, symptomatic radiographic knee OA accounts for the vast majority of total knee replacement procedures performed annually in the USA [9].
Table 1.
A multidisciplinary approach
| Nonpharmacologic | Pharmacologic |
|---|---|
| Self-management programs | Acetaminophen |
| Referral to PT | NSAIDs including COX-2-selective inhibitors |
| Regular exercise | Topical agents |
| Aerobic, aquatic, resistance | Capsaicin and NSAIDs |
| Weight loss, if overweight | Intra-articular therapies |
| Walking aids | Glucocorticoids |
| Thermal modalities | Hyaluronates |
| Patellar taping | Centrally acting agents |
| Bracing | Tramadol |
| Appropriate footwear | Duloxetine |
| Tai Chi | Opioid analgesics |
| TENS/TESA | |
| Traditional Chinese acupuncture |
Fig. 1.
An overview of osteoarthritis management
Indications for Joint Replacement Surgery
Recent data from an international study conducted under the auspices of a task force of the Osteoarthritis Research Society International (OARSI) and Outcome Measures in Rheumatology (OMERACT) suggest that the decision of the orthopedic surgeon to perform total joint arthroplasty in the patient with hip or knee OA cannot be satisfactorily predicted on the basis of the severity of the patient’s pain and/or physical limitation [10]. Additional analyses of data collected in this study, however, suggest that patients who were recommended for total joint arthroplasty can be categorized on the basis of their self-reported quality of life and the severity of the joint space narrowing on an X-ray of the symptomatic joint [11]. Further evaluation of this approach in additional patient cohorts is necessary before it can be recommended for use in either clinical practice or clinical trials.
Disclosure
Dr. Hochberg serves as a consultant to Abbott Laboratories, Astra- Zeneca Pharmaceutical, Eli Lilly, EMD Serono, Merck & Co., NiCox, Pfizer, Pozen, and Theralogix and is a member of the Medical Advisory Board and has stock ownership in Theralogix.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum. 2008;58:26–5. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lane NE, Brandt K, Hawker G, et al. OARSI–FDA Initiative: Defining the disease state of osteoarthritis. Osteoarthritis Cart. 2011;19:478–82. doi: 10.1016/j.joca.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Hochberg MC. Mortality in osteoarthritis. Clin Exp Rheumatol. 2008;26:S120–4. [PubMed] [Google Scholar]
- 4.Losina E, Walensky RP, Reichmann WM, et al. Impact of obesity and knee osteoarthritis on morbidity and mortality in older Americans. Ann Intern Med. 2011;154:217–26. doi: 10.1059/0003-4819-154-4-201102150-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nuesch E, Dieppe P, Reichenbach S, et al. All cause and disease specific mortality in patients with knee or hip osteoarthritis: Population based cohort study. BMJ. 2011;342:d1165. doi: 10.1136/bmj.d1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum. 2000;46:1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 7.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis. Osteoarthritis Cart. 2008;16:137–62. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Tallis F. Vienna Secrets. U.K.: Arrow Books; 2009. [Google Scholar]
- 9.Skinner J, Weinstein JN, Sporer SM, Wennberg ME. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 10.Gossec L, Paternotte S, Mailefert JF. The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: An international cross-sectional study of 1909 patients. Report of the OARSI–OMERACT task force on total joint replacement. Osteoarthritis Cart. 2011;19:147–54. doi: 10.1016/j.joca.2010.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shurupoff K, Park DH, Hochberg MC. The use of classification trees to determine criteria for “virtual total joint replacement” for patients with hip and knee osteoarthritis. Osteoarthritis Cart 2011;19:in press