To the Editor,
Extramedullary plasmacytoma is a plasma cell tumor arising outside the bone marrow and usually occurs as a solitary tumor in the upper respiratory tract, such as the pharynx, paranasal sinuses, nasal cavity, or oral cavity [1]. Other cases develop in the lymph nodes, skin, gastrointestinal tract, genitourinary tract, and other regions. Primary pulmonary plasmacytomas are very rare and usually present as solitary lung nodules or masses [2]. Unusual cases manifest as diffuse pulmonary infiltration [3,4]. We describe here a unique case of primary pulmonary plasmacytoma, which presented as multiple lung nodules during regular screening in a patient with systemic lupus erythematosus.
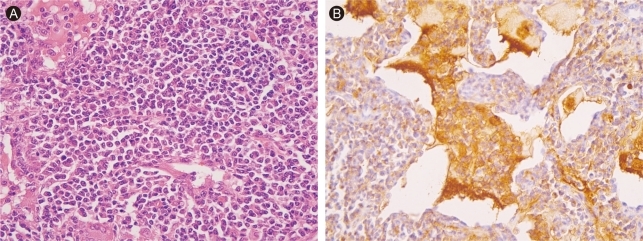
A 26-year-old woman was admitted and referred to the pulmonary service for an evaluation of multiple lung lesions on simple chest radiographs. The patient was diagnosed with systemic lupus erythematosus 11 years ago and had been treated with methotrexate, hydroxycholoroquine, and deflazacort. At the time of the systemic lupus erythematosus diagnosis, she was treated successfully for pulmonary tuberculosis with antituberculosis medication, and follow-up chest radiographs showed no active lung lesions. A chest radiograph, taken 3 months before admission as a screening for chest abnormalities, showed infiltrative lesions in both lower lung fields and focal consolidation in the right lower lobe but no specific change in her condition. Chest radiographs just before admission showed a slight aggravation of multiple patchy opacities. On admission, she presented slight sputum without other respiratory symptoms such as dyspnea or chest pain, and a review of systems was unremarkable. Vital signs were normal and there were no abnormal findings in the chest. A chest computed tomography (CT) scan revealed ill-defined nodular opacity and consolidation in both lungs (Fig. 1). Nodular lesions were scattered in both lung parenchymas and some were accompanied by ground glass opacities. A CT-guided needle aspiration biopsy specimen was non-diagnostic and, therefore, a subsequent surgical wedge resection via a thoracotomy was performed. The biopsy samples showed two relatively poorly demarcated round grayish white colored masses measuring 1.2 and 3 cm in diameter, respectively. A microscopic examination demonstrated diffuse infiltration of plasma cells (Fig. 2A), which were positive for lambda chain immunohistochemical staining (Fig. 2B). Serum protein and albumin levels were 8.2 g/dL and 3.4 g/dL, respectively. An electrophoretic analysis of serum proteins showed decreased albumin and an increased gamma globulin region without the M component. Serum immunoelectrophoresis detected no abnormal findings. Urine protein electrophoresis and immunoelectrophoresis were normal. An examination of serum immunoglobulins showed the following: IgG, 2,280 mg/dL; IgM, 1,540 mg/dL; IgA, 312 mg/dL; and IgD, 11 mg/dL. A peripheral blood white cell count was 3,800/mm3, and hemoglobin was 9.5 g/dL. A morphological analysis of the peripheral blood smear showed a slight microcytic and hypochromic pattern. A bone marrow examination revealed a normocellular pattern with about 50% cellularity and no increase in the plasma cell proportion. No hypercalcemia or increase in serum creatinine was noted. Chemotherapy with melphalan and prednisolone was initiated, because multiple plasmacytoma nodules were scattered in both lungs. Chest radiographs and CT scans taken after 4 months of pharmacological treatment showed near complete resolution of previously observed ill-defined nodular lesions and ground glass opacities.
Figure 1.
Chest computed tomography (CT) scan on admission showing ill defined nodular opacities and consolidations in both lungs.
Figure 2.
Histology of lung nodule showing diffuse infiltration of plasma cells (A, H&E, × 200; B, immunohistochemical stain for lambda chain, × 200).
Primary plasmacotyma in the lung is a very rare form of extramedullary plasmacytoma. Clinical manifestations and courses are not well defined because of the small number of reported cases. A review article of 19 cases reported that about half of cases are asymptomatic, whereas the others developed cough, dyspnea, chest pain, and fever, mostly due to the mass effect [2]. The age of incidence was relatively old, and most cases developed in subjects > 40 years old. A slight male preference of incidence was noted with a ratio of 1.4:1. Contrary to previous cases, our patient was female and 24 years old at the time of diagnosis. The diagnosis of primary pulmonary plasmacotyma is based on the histological confirmation of plasma cell infiltration in lung lesions. Additionally, it requires normal bone marrow, normal skeletal survey, no related organ or tissue impairment, and no M protein in serum and/or urine. Thus, the current case fulfilled the diagnostic criteria.
Typical lung lesions in previous primary pulmonary plasmacotyma cases were solitary lung nodules or masses, and they occurred in the hilar or parenchymal areas with slight preference to the lower lobes [2]. These tumors were round or ovoid shape, with sizes of 1.5-6 cm. They appeared as homogeneous nodules or masses with smooth and well delineated margins. The most common form of primary pulmonary plasmacotyma is a solitary tumor but different radiographic presentations have been reported. Horiuchi et al. [3] reported a case in a 45-year-old Japanese woman with bilateral reticulonodular infiltration in the lower lobes accompanied by fever, dyspnea, and hypoxemia. In a case report by Lazarevic et al. [4], bilateral reticulonodular opacities in both lungs were noted in an elderly male, who developed malaise, weight loss, and dry cough without fever or dyspnea. In addition to diffuse lung infiltrates in both cases, two separate plasmacytoma masses involving bilateral lungs were reported [5]. In the current case, primary pulmonary plasmacotyma presented as multiple lung nodular opacities in both lungs, which were detected by routine follow-up chest radiographs. These lesions increased in size over time without causing definite symptoms except for slight sputum. The present case is the first report of primary pulmonary plasmacotyma presenting as multiple lung nodules in both lungs. These findings suggest primary pulmonary plasmacotyma should be considered in the differential diagnosis of multiple lung nodules.
While most cases of solitary pulmonary plasmacytoma are treated with surgical resection and/or irradiation [2], the previous two cases of diffuse pulmonary infiltration underwent combination chemotherapy including melphalan and prednisolone [3,4]. The clinical responses were relatively good, although the long-term response to chemotherapy remains to be evaluated. Similar to cases of diffuse lung infiltration, the patient in this study was also treated with melphalan and prednisolone, and near complete radiological resolution was observed after six cycles of treatment.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Galieni P, Cavo M, Pulsoni A, et al. Clinical outcome of extramedullary plasmacytoma. Haematologica. 2000;85:47–51. [PubMed] [Google Scholar]
- 2.Joseph G, Pandit M, Korfhage L. Primary pulmonary plasmacytoma. Cancer. 1993;71:721–724. doi: 10.1002/1097-0142(19930201)71:3<721::aid-cncr2820710311>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 3.Horiuchi T, Hirokawa M, Oyama Y, et al. Diffuse pulmonary infiltrates as a roentgenographic manifestation of primary pulmonary plasmacytoma. Am J Med. 1998;105:72–74. doi: 10.1016/s0002-9343(98)00131-4. [DOI] [PubMed] [Google Scholar]
- 4.Lazarevic V, Cemerikic-Martinovic V, Suvajdzic N, Subotic D, Colovic M. Diffuse primary plasmacytoma of the lung. Haematologia (Budap) 2001;31:161–165. doi: 10.1163/15685590152492972. [DOI] [PubMed] [Google Scholar]
- 5.Niitsu N, Kohri M, Hayama M, et al. Primary pulmonary plasmacy toma involving bi lateral lungs and marked hypergammaglobulinemia: differentiation from extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Leuk Res. 2005;29:1361–1364. doi: 10.1016/j.leukres.2005.04.009. [DOI] [PubMed] [Google Scholar]