Abstract
The discussions about medical education in the public focus upon quantity. The quality of the teaching process isn’t questioned. But the professionalization of medical education should start with a close look at bedside teaching because it is the core of training medical doctors.
Patient-centered teaching: German medical leicensure act (Approbationsordnung) defines the quality of medical education by standard setting for group sizes and fixing the hours of bedside teaching. Although there are some fuzzy definitions it is possible to extract some special forms of bedside teaching. The capacity act (Kapazitätsverordnung) interprets these definitions for calculating the number of students who could be enrolled each year.
Types of bedside teaching: The different forms of contact with patients which are necessary for a good medical education can be transformed into distinct types of courses. Our classification of courses with specific forms of patient contact is suitable to describe each German program of medical studies. This quantitative profile offers new opportunities for comparing medical education at the different faculties.
Discussion: In many German medical schools the hours of bedside teaching are allocated in a verv pragmatical way according to the medical leicensure act. A more professional curriculum planning leads to a sophisticated use of these diverse forms of patient-centered teaching. Because this professional planning is better derived from the legal basis it offers new arguments against an economically oriented hospital management.
Keywords: quality control, clinical training, professional education
Abstract
Während sich die öffentliche Diskussion über die medizinische Ausbildung vor allem um die Quantität dreht, wird die Qualität der Ausbildung praktisch nicht geprüft. Eine Akademisierung der medizinischen Ausbildung sollte aber an der Ausbildung am Patienten ansetzen, wenn sie zur Qualitätsverbesserung beitragen will.
Patienteneinbindung in der ÄAppO: Die Qualität der medizinischen Ausbildung wird in der Approbationsordnung für Ärzte vor allem über Gruppengrößen und Stundenzahlen für den Unterricht mit Patienteneinbindung definiert. Trotz einiger Ungenauigkeiten in der Approbationsordnung lassen sich in ihr Angaben zur Art und Menge des Unterrichts mit Patienteneinbindung finden und systematisch unterscheiden. Darauf greift die Kapazitätsverordnung zurück, wenn sie die Anzahl der auszubildenden Studierenden bestimmen will.
Formen der Patienteneinbindung: Den verschiedenen Lehrveranstaltungsformen lassen sich auf Basis der Vorgaben der Approbationsordnung verschiedene Formen der Patienteneinbindung zuordnen. Die hier vorgeschlagene Systematik der Patienteneinbindung kann auf jeden konkreten medizinischen Studiengang angewendet werden und liefert dann ein für diesen Studiengang charakteristisches Mengenprofil.
Diskussion: Die an den meisten Fakultäten pragmatisch vorgenommene Verteilung der Stunden mit Patienteneinbindung deckt sich mit den Formulierungen der Approbationsordnung. Die korrekte Berücksichtigung der verschiedenen Formen einer Patienteneinbindung im Unterricht liefert über eine professionellere Unterrichtsplanung hinaus Argumentationshilfen für ein Qualitätsmanagement der medizinischen Ausbildung auf der Basis rechtlicher Vorgaben, die über eine Wirtschaftlichkeitsbetrachtung im Klinikalltag hinaus gehen.
Introduction
While the debates in this journal or the annual GMA conferences debate the quality of medical education, the current political focus on revolves primarily around solving an alleged shortage of physicians [1], [2], [3], i.e. a debate about the number of physicians in terms of doctors in training, always assuming a certain qualification [4].
Unlike in all other degree courses in Germany, in determining the number of students for medical studies both number of medical staff at medical schools and the number of patients treated in the previous year is taken into account. Apart from theoretical instruction, patient-related teaching is thus a defining criterion for medical education and is discussed at various points in the Medical Licensure Act (ÄAppO) and the Capacity Regulations (KapVO). As Fischer & Rüping deal with the issue of congruence between ÄAppO and KapVO elsewhere [5], we will focus our attention on the question of how the last amendments of the ÄAppO can make the targeted quality improvements in the curriculum of each faculty visible.
Patient-related training will be used as a starting point as it is the one aspect which distinguishes medical studies from most other degree courses and because, apart from university exams, most of the changes caused by the various amendments to the ÄAppO are related to teaching involving patients. Because the ÄAppO only defines the minimum quality standards regarding group size and hours of teaching per week [6], each medical school can develop its own profile within a nationally comparable framework as long as it is possible to clearly differentiate the involvement of patients through the types of classes taught. This could allow for a better differentiation of quality and quantity in medical education, interwoven with each other, and to substantiate the debate about the further development of medical studies which has been reinvigorated through the Science Council [7], [8], [9].
Patient Involvement from the ÄAppO Point of View
Apart from the distinctions between different types of events common in all degree courses, the ÄAppO both uses an unusual name for problem-oriented teaching (subject-related study groups) and describes two special forms of practical exercises, which relate to patient-related teaching (§ 2, paragraph 3 ÄAppO), namely teaching at the bedside and the blocked clerkships. Furthermore, it is important to note that because according to § 2, paragraph, 4, sentence 3 ÄAppO presenting patients is explicitly listed at least for seminars, teaching involving patients can be distinguished into theoretical courses and practical exercises. The extent of involvement will thereby be largely ignored for the purposes of classification although it is obviously important for degree course planning.
A second differentiation results from the provisions in § 2, paragraph 3, sentence 5 which states that instruction in the practical exercises should ideally take place using healthy people at first and then, as the students’ skills progress, increasingly using patients. Against this backdrop, it is understandable why the 7th and 8th amendment to the ÄAppO had 560 hours of teaching involving patients in its corresponding sample timetable, while the 9th amendment only required 476 hours of bedside teaching. The reason for this change is simply due to the fact that since the 9th amendment of 2002 a course in clinical examination techniques is no longer required. Until the 8th amendment, this had contributed at least 84 hours in the calculation of bedside teaching.
The third distinction of patient involvement concerns the practical exercises. The two forms of training relevant here (bedside teaching and blocked clerkships) not only differ in their temporal organization in the timetable [6] but also in the type of patient involvement [10]. In bedside teaching, a patient is usually assigned to a small group of students while in a student blocked clerkship, a student meets a number of patients which has not been predetermined (“under the conditions of everyday clinical and out-patient practice”). Legally, this difference may be marginal for the course planning but this is much trickier when it comes to timetable design. While in bedside teaching student-patient contact can be relatively precisely defined via the timetable, it can vary considerably in a blocked clerkship which means there can be no mapping of student-patient contact in the timetable beyond the day-level [10]. Also, the student-teacher ratio should be different because a ward doctor or a GP cannot supervise 3-4 students on the ward or in their surgery throughout the day.
The fourth and last differentiation of patient involvement from a legal point of view concerns the period of studies at which patients are introduced into the classroom. § 3, paragraph 4 ÄAppO makes it very clear that the Practical Year is part of undergraduate training where training needs have priority over other goals [11]. So in a linguistic differentiation of the various teaching events involving patients, it must be included. The Practical Year is also significant for the planning of timetables in the first five years of study because one can hardly expect patients on a ward in a teaching hospital to be able to distinguish between students and Practical Year students when it comes to consenting to being examined by students.
Figure 1 (Fig. 1) shows the four distinctions which arise from the ÄAppO, from left to right and marked with Roman numerals. Of the five types of courses with patient involvement (lectures, seminars, courses, bedside teaching and blocked clerkships), four are of central importance for medical education in terms of content and organization. The thickness of the border surrounding them symbolises the importance of patient involvement in the various courses and sections of study in terms of practical relevance of medical studies.
Figure 1. The involvement of patients in medical education according to the ÄAppO.
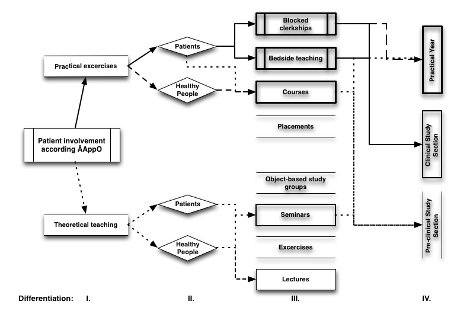
Solid arrows stand for regular patient involvement, no arrows for a lack of patient involvement in this event and study section. The two event types which are most important for clinical and practical training quality (bedside teaching and blocked clerkships) are additionally marked with double vertical lines in Figure 1 (Fig. 1). They are significant for both curriculum planning and for the economic outcome of each university hospital.
Traditional exercises, as in medical biometrics, are not specifically addressed in the ÄAppO but are assigned to the various theoretical courses in accordance with the classification of the German Rectors’ Conference [12]. The resulting consequences for personnel-related capacity assessment will not be discussed here.
Forms of Patient Involvement
For a classification of patient-related training these legal requirements do not suffice because they usually only implicitly include the educational rationale for the need for bedside teaching, blocked clerkships and other types of events. In addition, this attempt at more differentiated classification of teaching with patient involvement results in a general problem due to the fact that some expressions in the various amendments to the ÄAppO are ambiguous. A more detailed analysis of the 8th amendment’s classification of the course of clinical examination methods as bedside teaching quickly raises questions about whether this training is conducted exclusively using patients, as suggested by the term “instruction at the bedside”.
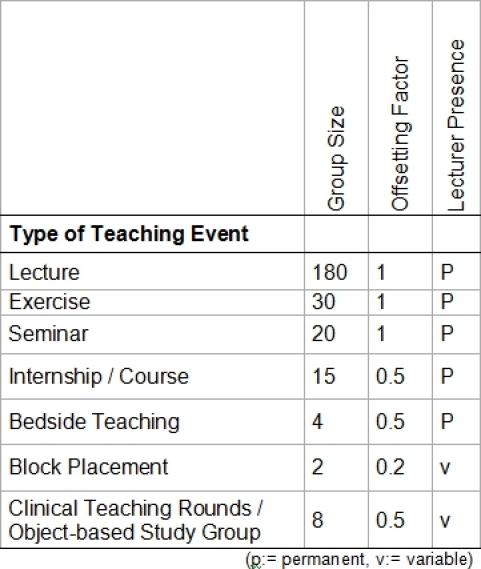
Thus it raises the question whether one can specify the type of patient involvement within the existing legal framework in such a way it becomes more useful for timetable planning and capacity calculation. So far, at least in Hannover, the events listed in Figure 1 (Fig. 1) have only been differentiated by the number of students per lecturer and the duration of lecturer presence in the annual capacity calculations and performance-based allocation of resources in teaching within the Hannover Medical School (MHH) [13]. Table 1 (Tab. 1) shows this traditional legal capacity grid for the MHH.
Table 1. Differentiation of various types of courses by group size, offsetting factor (KapVO) and lecturer presence.
A similar grid is likely to be present at all medical schools. For the following considerations it is not important how big the differences between the medical faculties are. The only important aspect is primarily general transferability. The empirical basis for further considerations is the data on lectures collected at the MHH for the current expert evaluation on patient-related capacity calculation in the model degree course HannibaL carried out by Lohfert & Lohfert [14]. This necessarily entails an abstraction of the rich variety of patient-related training in the various subjects at the respective faculties to produce a simple classification. Since the classification places the extent of patient involvement (PE) in the foreground, the various categories are simply numbered in series.
Patient-related Teaching in Large Groups
Traditionally, healthy and sick people are presented in lectures and seminars to illustrate the relevant topics. In terms of legal capacity, both types of events are not considered. Quantitatively, the inclusion of healthy and/or sick patients in these types of events is relevant however if within a period of a few days or weeks a particular pattern is to be presented to all seminar groups of a year. In a way, this is the base category (PE_0). Also included in this category are exercises or object-based study groups as theoretical courses, although they primarily involve case vignettes or virtual patients. Because this teaching is not included in the patient-related capacity calculation, the ratio of duration of the patient’s presence (= patient load in the terminology of capacity calculation) to teaching duration does not have to be calculated.
Patient-related Teaching in Small Groups without In-patients
Since the 9th amendment to the ÄAppO in 2002, training in clinical examination techniques no longer explicitly forms apart of the legally relevant teaching capacity at the bedside. From the minutes of the Federal Council it cannot be inferred [15], [16] whether this is related to the elimination of the corresponding performance certificate or whether the legislature intended to take into account the fact that this teaching in part was carried out on other students or simulated patients (PE_1a) and increasingly uses simulators and puppets (PE_1b). Fact is that training using these resources requires significant organisation which is not taken into account in patient-related capacity calculation. Also, at the first stage of patient-related capacity calculation (§ 17, paragraph 1 No. 1 KapVO) only in-patients are considered. It is therefore necessary to account for training using out-patients (PE_1c) separately, especially as according to § 17, paragraph 1 No. 2 KapVO a polyclinic’s capacity is limited to a maximum 50% surcharge on in-patient capacity. If this delineation is removed, the faculty risks overloading their steady-state operation even at the planning stage in favour of teaching.
Regarding the relationship of the temporal integration of the “patient” to the teaching time, a ratio of 0.1:1 results for category PE_1 and PE_1b precisely because virtually no patients are involved but the scarce resources used should not be neglected. But for category PE_1c this ratio would have to be set as 1:1 because the (out-)patients are present during the entire class time.
When trying to identify these forms of patient involvement in the broadest sense with specific names for the lecture form, it makes sense to use a traditional term like “course” as a special form of practical exercise. Apart from training general medicine where by definition there is no training with in-patients, uncertainties can be avoided in judicial reviews of the capacity calculation based on the curriculum.
Patient-related Teaching in Small Groups
The legally relevant capacity lecture-form “bedside teaching” forms the core of clinical training. In patient-related capacity calculation it is assumed that it is only performed on in-patients. After the above exclusion of other “patients groups” category PE_2 displays this correctly. Because of the large number of groups, this type of event requires exact time planning with rotation schedules. If one plans one patient per hour of teaching, this patient is (at least at the MHH) available only for that group on that day and is required to be present for between one and three hours of teaching. Traditionally, patient load and teaching periods are set in a 1:1 ratio because it is presumed that the patient is tied up during the entire teaching time.
This simple case in terms of legal capacity illustrates that the proposed classification is “just” a normative examination which does not intend to anticipate the planning of teaching on the ground aims to produce averages across the range of possibilities within each category and to differentiate between categories.
Patient-related Teaching in Small Groups in Healthcare
During the blocked clerkships the students are involved in clinical routines involving in- and out-patients in the sense of the ÄAppO. They are required to deal with a variety of patients during this period but patients are not explicitly removed from hospital care at a particular time of day for the purposes of teaching. Unlike the involvement of patients in bedside teaching (PE 2), students must visit the patient independently and extract them from patient care. The contact with the students thus represents a patient load in terms of patient-related capacity. But because the teaching staff examine patients together with the students only during a portion of the blocked clerkship, patients load does not equal teaching time. It would therefore be useful to set the involvement of different patients during a day at the ratio of 0.3:1. At least this is the value determined for the MHH through the latest surveys carried out in the context of the review by Lohfert & Lohfert [10] although this varies from discipline to discipline. It also corresponds to the Teaching Load Regulations’ offsetting factor for teaching events in which teachers do not have to be permanently present.
Clinical teaching rounds are a special type in this category which differ from the blocked clerkship in their temporal extent and the number of participating students. But apart from these two differences, clinical teaching rounds also fall into this category of patients involvement with a similar patient load as the blocked clerkships.
Patient-related Training with Healthcare
The last form of patient involvement (PE_4) consists of the Practical Year. One could also regard it as a series of particularly long blocked clerkships which are interrupted by occasional bedside teaching or seminars. But this would make the desired conceptual distinction more difficult. In addition, the Practical Year has the particular difficulty that, in terms of the curriculum, the load of the various subjects can only be controlled via restrictive measures at a university hospital and its associated academic teaching hospitals and during the clinical part of studies.
Curiously, the Practical Year is not considered in the calculation of patient-related capacity. Presumably this is because separating patient load for teaching purposes from healthcare is even harder in the Practical Year than in the blocked clerkship. If one were to define the patient load for the Practical Year, what applies to PE_3 would also apply to it, i.e. a factor of 0.3:1.
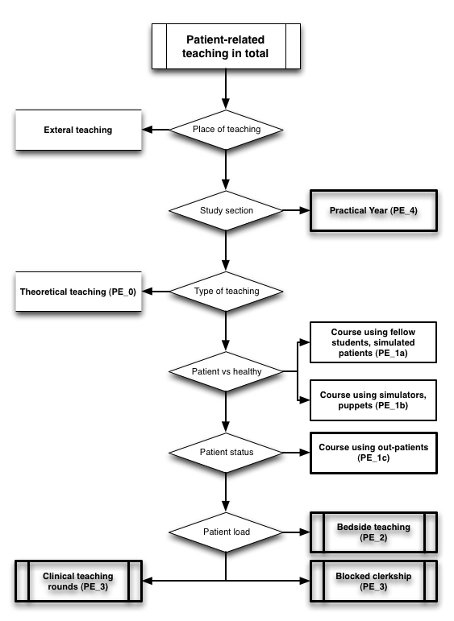
As Figure 2 (Fig. 2) shows, there are no difficulties in assigning the conceptual clarification of the involvement of patients to common types of courses, even in the form of a decision tree. Deviating from the line of argument, category PE_4 was classified higher up compared to the arguments above because they can be eliminated in the capacity calculation process earlier. But in terms of content it represents the highest form of integration of teaching and patient care. For the capacity calculation, one would also take into account if the lectures take place at the university hospital or at an external institution. In the second case the scheduled hours must be removed from the patient-related capacity calculation and the associated curriculum units in the workforce capacity calculation taken into account. Because this option is only explicitly allowed for model degree course (§ 41, paragraph 1, point 4 ÄAppO), they will not be discussed here further.
Figure 2. The distinction of four types of patient involvement.
Analogous to Table 1 (Tab. 1), one can show the proposed classification in table form. For this purpose the above-defined patient load and patient involvement is mapped to the individual courses types in Table 2 (Tab. 2), resulting in a grid for clinical and practical training.
Table 2. Differentiation of various types of courses by patient load and patient involvement.
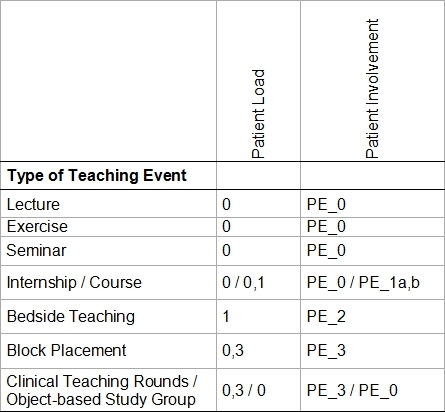
The blocked clerkship in general medicine represents a special case. In terms of its temporal organisation, it falls into category PE_3 but also in terms of the status of the patients involved, into category PE_1c. As it is held outside of the university clinic in external institutions, the number of hours is removed from the patient-related capacity calculation.
Discussion
If we apply the proposed categorisation of patients involvement to a specific medical degree course, we obtain a clinical-practical volume profile which is characteristic for this degree course. It is not a definitive description as long as it does not differentiate between the various clinical-practical subjects but allows a more nuanced view of the curriculum in question. It does not solve the question whether determining capacity following the traditional model of counting occupied beds at midnight is still appropriate in the DRG age. This, however, is a separate issue. The proposed classification represents an introduction to the general problem of how to connect patient-related instruction with a quality management system under worsening economic conditions.
At most faculties, the distribution of hours with patient involvement across individual subjects or modules is not done using the categories PE 1a/b, PE_1c and PE_2. However, approaches for distinguishing between traditional bedside teaching and blocked clerkships are seen more and more frequently. So academic practice is largely consistent with the ÄAppO but not KapVO. This discrepancy is not commonly observed but if the proposed differentiation were to be used, the problem becomes visible and solvable. For while the hourly requirements of the ÄAppO leave open whether such teaching constitutes patient involvement in the sense of categories PE_1a/b, PE_1c or PE_2 in terms of bedside teaching, the capacity regulation initially only uses category PE_2 for patient-related capacity calculation and increases this result by 50% to account for the out-patients of the hospital. It is presumably for this reason that KapVO overestimates patient-related capacity as it interprets bedside teaching and blocked clerkships differently than can be directly deduced from the ÄAppO [5], [10]. Unfortunately, extent of the overestimation is difficult to determine because how the ÄAppO is formulated far from clear in places. This increases the pressure on the ward doctors and will most certainly not improve the quality of medical education. While merging bedside teaching with the blocked clerkships by KapVO would benefit the university hospitals if they were able to realise an additional 50% of teaching with patient involvement using out-patients. However, assuming the improvements in medical training announced by the Federal Council for the 9th amendment of the ÄAppO then it is reduced to a mere reduction in group sizes (from 4.36 to 4). This means the reform aim as announced by the Working Group on Medical Reform to achieve 53 hours per week of patient-related teaching [17] seems to have been lost, at least in the implementation of the ÄAppO through the KapVO.
If the intention is not to lose sight of the quality of education in favour of quantity, a new version of the relevant regulations for medical education should aim for a better match. This is even more important as the legal requirements of KapVO and the ÄAppO also define thresholds, which cannot be touched, for quality and quantity of teaching via the healthcare system and its attempts to reducing waiting times. An important intermediate step for this is that faculties map patient involvement in the classroom in a more differentiated way than before. Only a transparent presentation of clinical instruction allows for teaching and patient care to be jointly planned and carried out in an organised fashion.
Competing interests
The author declares that he has no competing interests.
References
- 1.Bundesministerium für Gesundheit. Eckpunkte zum Versorgungsgesetz. Berlin: Bundesministerium für Gesundheit; 2011. p. 37. [Google Scholar]
- 2.Bitter-Suermann D. Ärztemangel/Ärzteschwund. Wo liegen die Probleme? Forschung Lehre. 2011;18(1):42–44. [Google Scholar]
- 3.Stüwe H. Ärztemangel: FDP will mehr Medizinstudienplätze. Dtsch Arztebl. 2010;107(17):786. [Google Scholar]
- 4.Hibbeler B, Richter-Kuhlmann E. Zehn Prozent mehr Studienplätze wären angebracht. Interview mit Prof. Dr. med. habil. Jan Schulze. Dtsch Arztebl. 2010;107(41):1966–1968. [Google Scholar]
- 5.Fischer V, Rüping U. Das Kapazitätsrecht und die Qualität der medizinischen Ausbildung [submitted] GMS Z Med Ausbild [Google Scholar]
- 6.Haage H. Das neue Medizinstudium - Medizinisches Ausbildungsrecht - mit Bundesärzteordnung und Approbationsordnung. Aachen: Shaker; 2003. [Google Scholar]
- 7.Wissenschaftsrat. Empfehlungen zur Qualitätsverbesserung in Studium und Lehre. Köln: Wissenschaftsrat; 2008. [Google Scholar]
- 8.Wissenschaftsrat. Leitlinien zur Reform des Medizinstudiums. Köln: Wissenschaftsrat; 1992. [Google Scholar]
- 9.Wissenschaftsrat. Trends der Hochschulmedizin in Deutschland. Berlin: Wissenschaftsrat; 2010. [Google Scholar]
- 10.Lohfert P. Spielt die Patientenverfügbarkeit für die Kapazitätsberechnung eine große Rolle?. 71. ordentlicher Medizinischer Fakultätentag; 04. Juni 2010; Hannover. Hannover: Medizinischer Fakultätentag; 2010. 8 [Google Scholar]
- 11.Fischer V, Haller H. Erschweren die Approbationsordnung für Ärzte und die Kapazitätsverordnung die Planung einer patientenbezogenen Ausbildung?. Jahrestagung der Gesellschaft für Medizinische Ausbildung (GMA); 23.-25.09.2010; Bochum. Düsseldorf: German Medical Science GMS Publishing House; 2010. Available from: http://dx.doi.org/10.3205/10gma120.Doc10gma120 [DOI] [Google Scholar]
- 12.HRK. Empfehlung zur Sicherung der Qualität von Studium und Lehre in Bachelor- und Masterstudiengängen. Bonn: Hochschulrektorenkonferenz; 2005. [Google Scholar]
- 13.Just I, Beinhoff S, Haller H, Fischer V. Kriterien für eine leistungsorientierte Mittelvergabe in der Lehre. Jahrestagung der Gesellschaft für Medizinische Ausbildung (GMA); 23.-25.09.2010; Bochum. German Medical Science GMS Publishing House; 2010. [Düsseldorf]. Available from: http://dx.doi.org/10.3205/10gma233.Doc10gma233 [DOI] [Google Scholar]
- 14.Lohfert P, Lohfert C. Gutachten über die Kapazitätsberechnungsmethode für den Modellstudiengang HannibaL (UPPMK). Kurzfassung. Kopenhagen: Lohfert & Lohfert; 2011. [Google Scholar]
- 15.Bundesministerium für Gesundheit. Beschlussvorlage zur Änderung der Approbationsordnung für Ärzte. Berlin: Bundesrat; 2002. [Google Scholar]
- 16.Bundesministerium für Gesundheit. Beschlussvorlage zur Änderung der Approbationsordnung für Ärzte. Bonn: Bundesrat; 1997. [Google Scholar]
- 17.AG Medizinische Studienreform. Vorlage eines Entwurfes zur Änderung der Approbationsordnung für Ärzte - mit wichtigen, zu beachtenden Gesichtspunkten und Kapazitätsberechnungen - Heidelberg: Gesellschaft für Medizinische Ausbildung (GMA); 1999. [Google Scholar]


