Commentary
The Federal Ministry of Health (BMG) has recently submitted a draft bill amending the licensing regulations for doctors (ÄAppO), which pursues the goal of a targeted recruitment and promotion of medical students and the strengthening of general practice ([1], p. 1). One of the proposed measures in the draft is the extension of the minimum duration of the blocked clerkship in general medicine from one to two weeks. As many faculties have already established such a two-week block in general medicine since 2003, it would have been better to wait another five to seven years with the implementation of such a change until there is empirical data on whether the graduates of these faculties are more often board-certified in general medicine than graduates with a one-week clerkship in general medicine. Now the empirical hypothesis testing is replaced by a political goal.
But since 2003 there is a severe misinterpretation in the legal implementation of the currently valid ÄAppO which will be simply renewed with the planned amendment to the nationwide detriment of the quality formation. To overcome this problem would be a real action to support medical students.
In the current ÄAppO [2] most of the teaching hours are considered minimum times, but the licensing regulation determines that the hours for bedside teaching (UaK) should amout to exactly 476 (§ 2, paragraph 3, sentence 11, ÄAppO). In these 476 hours the teaching with healthy persons and with outpatients is included, because the ÄAppO explicitly doesn’t establish a difference between these different forms of bedside teaching (§ 2, paragraph 3, sentence 5). Furthermore, the ÄAppO demands a minimum of five additional blocked clerkships of one to six weeks length each (or 190 to 1380 hours) (§ 2 paragraph 3 sentence 12 in conjunction with § 27 paragraph 4). Whether these blocked clerkships also include hours with healthy people or outpatients, depends on the conditions within the clinic or the ambulatory, but it is rather unlikely. Overall, the actual ÄAppO seems to define 666 specific patient-related teaching hours as a minimum, which have to be realized only in parts with stationary patients.
In the proposed amendment of the ÄAppO the hours for the UaK remain unchanged. But the doubling of the minimal duration of the general medicine clerkship increases the necessary hours for these courses to at least 228. Therefore the joined requirement for UaK and clerkships would then increase to 704–1856 hours.
The fact that the training in general medicine is not performed within the university hospital, is of no importance for the individual students workload. Nevertheless for the calculation of the number of students which can be trained, the curriculum design and the funding, it is definitely important.
But the regulation of capacity (KapVO) [3] uses an interpretation of the ÄAppO by the “Unterausschuss Kapazitätsverordnung” of the federal central office for the allocation of university places (similar to English UCAS) that declares the 476 hours as a common base for the UaK and the blocked clerkships [4]. As a substantiation they cite a comment of the BMG during the legislative process, according to whichthe only difference between UaK and blocked clerkships is that the latter are temporally blocked classes. But an explicit statement that blocked clerkships and UaK are part of the 476 hours can only be found in the paper of the “Unterausschuss Kapazitätsverordnung”. The comment of Haage [5] says nothing about this integration within the 476 hours.
In the KapVO-formula for the calculation of the patient-related training capacity healthy persons and outpatients are initially excluded because the formula calculates the capacity on the basis of the occupied beds of a whole year. In the second step another 50% inpatient training capacity is added as an upper approximation for the outpatient capacity. This corresponds to 238 additional hours of inpatient training. Altogether the KapVO claimes 714 training hours with outpatients and inpatients or 476 hours for 1.5 times the number of students. But in the latter case one has to subtract the hours with healthy persons, standardized patients or simulators of from the curriculum of the faculty. Simply Because of the fact that the first is not a scarce resource and the latter two categories didn’t matter in the late 70s of the last century when the KapVO-formula was developed! In other words the didactic concept of the actual ÄAppO (§ 2, paragraph 3, sentence 5) is completely dropped in favour of maintaining an old formula.
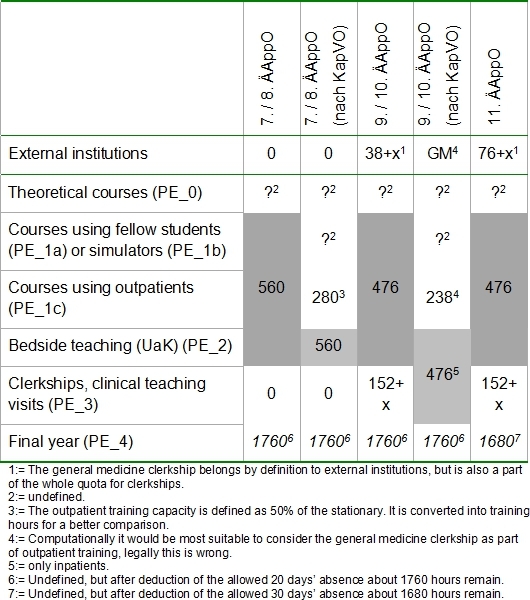
Table 1 (Tab. 1) summarizes the patient-related training hours for some of the amendments of the ÄAppO and their interpretations by the KapVO. Table 1 (Tab. 1) doesn’t consider at all the different educational concepts of these regulations. The mentioned forms of patient involvement are described elsewhere [6].
Table 1. Assignment of patient-related training hours within the ÄAppO to different categories of patient involvement. (The definition of UaK within a regulation is grayed out.).
Three other reasons can be identified why this interpretation of the ÄAppO by the KapVO can ‘t be correct, even if the current draft amendment seems to confirm it. The first two regard the organization of the clinical training. The third is a simple mathematical analysis of the specifications in the ÄAppO:
In normal bedside teaching (UaK) the students are trained at a certain time with the help of a certain patient. During a blocked clerkship this is not possible, if “the terms of the clinical and ambulatory everyday life” should be guaranteed, as the ÄAppO demands. Patients in the UaK have to be planned, in the blocked clerkship they drop in. This difference clearly has implications for the integration of teaching and patient care and the attendance times of the teachers.
The training ratio of 1 patient per 3 students in the normal bedside teaching is in the general medicine practice even less feasible than on a normal ward. A relation of 1 student per all patients in a ward or a doctor’s office seems suitable. These “clerkship patients” doesn’t have, unlike the situation for the “bedside teaching patients” an exactly predefined contact time.
At least 20% of the placements after the first part of the federal exam should be organized as blocked clerkships (§ 2, paragraph 3, sentence 12). If these 20% were included in the 476 hours UaK 93,2 hours would be sufficient. But five times a common working week of 38-46 hours sum up to 190-230 hours. If each of the five blocked clerkships lasts two weeks with 40 hours, the 476 hours UaK would be nearly absorbed. But a week of 40 hours is significantly shorter than the clinical and ambulatory everyday life and the ÄAppO allows blocked clerkships between one an six weeks duration. Therefore a fixed number of 476 hours for the UaK and the blocked clerkships together doesn’t fit.
The old master timetable according to the requirements of the eight amendment of the ÄAppO listed several courses of other placements with 420 hours. Combined with the hours for the bedside teaching the total amount of placements according to the 10th amendment could be calculated as follows 476+420+x. The x represents the requirements in § 2, paragraph 1, sentence 4 combined with § 2, paragraph 3 sentence 11 and 12 plus § 27 paragraph 4 ÄAppO for the blocked clerkships and would be solved if x=224. This represents a 44,8 hour week and seems to be much more realistic.
The planned extension of the blocked clerkship in general medicine isn’t important (although very expensive). What is really necessary is the correct consideration of all the blocked clerkships for calculating the training capacity of the medical faculties. The distributed amendment draft doesn’t solve the fuzziness in the actual law. The proposed interpretation offers a solution without contradictions which will only lead to a diminished number of medical students when the KapVO-formula doesn’t offer different parameters for the clinical training with standardized patients or outpatients and the classical bedside teaching with inpatients. Such a differentiated KapVO-formula would depict a correct picture of the real everyday life medical training and would match a modern educational curriculum. The only obstacle is the fact that there are only a few examples of wise and appropriate political decisions.
References
- 1.Bundesministerium für Gesundheit. Erste Verordnung zur Änderung der Approbationsordnung für Ärzte. Berlin: BMG; 2011. [Google Scholar]
- 2.Bundesministerium für Gesundheit. Approbationsordnung für Ärzte. Bundesgesetzbl. 2010;I(39):992. [Google Scholar]
- 3.Niedersächsisches Minsterium für Wissenschaft und Kultur. Verordnung zur Änderung der Kapazitätsverordnung. Hannover: GVBI; 2010. p. 436ff. [Google Scholar]
- 4.Zentralstelle für die Vergabe von Studienplätzen. Auswirkungen der neuen Approbationsordnung für Ärzte vom 27. Juni 2002 auf die Parameter zur Berechnung der Aufnahmekapazität. Dortmund: ZVS; 2002. p. 5. [Google Scholar]
- 5.Haage H. Das neue Medizinstudium - Medizinisches Ausbildungsrecht - mit Bundesärzteordnung und Approbationsordnung. Aachen: Shaker; 2003. [Google Scholar]
- 6.Fischer V. Die Einbindung von Patienten in die medizinische Ausbildung. GMS Z Med Ausbild. 2012;29(1):Doc13. doi: 10.3205/zma000783. Available from: http://dx.doi.org/10.3205/zma000783. [DOI] [PMC free article] [PubMed] [Google Scholar]


