Abstract
Objective: Procedural skills education has a high priority for medical students. However, it is not clear what kind of skills they consider important and whether their perception differs from the physicians’ view.
Methods: We conducted a survey on 26 skills in internal medicine among medical students and physicians. Ninety-five fourth year and 62 final year students along with 67 physicians working in medical departments participated in the survey. A similar but smaller survey was completed earlier before the implementation of a skills training at the faculty.
Results: Students generally preferred technically complex skills while, in contrast, physicians found “bed-side-skills” more important. The result was independent of the students’ participation in the skills training or of the physicians’ experience. A similar result was achieved in the smaller survey before the implementation of the skills training.
Conclusion: Students and physicians significantly differ in their entitlement towards procedural skills education. This should be considered when educational strategies are being discussed.
Keywords: procedural skills education, skills lab, needs assessment, internal medicine, survey
Abstract
Zielsetzung: Der Wunsch nach praktischer Ausbildung im Medizinstudium wird vor allem von den Studierenden selbst formuliert. Was genau sie sich darunter vorstellen und ob diese Vorstellung mit derjenigen der Ärzte übereinstimmt, ist nicht bekannt.
Methodik: Wir führten eine Umfrage zu 26 Fertigkeiten der Inneren Medizin durch, die zuvor unter Studierenden und Ärzten ermittelt worden waren. An der Umfrage nahmen 95 Studierende im vierten Studienjahr, 62 Studierende im Praktischen Jahr und 67 internistisch tätige Ärzte teil. Eine gleichartige, aber kleinere Umfrage hatten wir bereits vor Einführung des Skills-Trainings an unserer Fakultät durchgeführt.
Ergebnisse: Während den Studierenden vor allem Fertigkeiten wichtig waren, die hohen technischen Aufwand erfordern, waren das bei den Ärzten eher solche, die mit einfachen Mitteln am Krankenbett ausgeführt werden. Dieses Ergebnis galt unabhängig davon, ob die Studierenden bereits trainiert waren oder nicht, beziehungsweise unabhängig vom Ausbildungsstand der Ärzte. Auch stimmte das Ergebnis der aktuellen Umfrage gut mit derjenigen vor Beginn des Skills-Trainings überein.
Schlussfolgerungen: Der Anspruch von Studierenden und Ärzten an die praktische Ausbildung unterscheidet sich grundlegend. Dies sollte bei der Diskussion um Lerninhalte Berücksichtigung finden.
Introduction
Today simulator training is a key component in medical education. So called skills labs offer exercises with part-task-models, full-scale-simulators and programs with standardized patients that are supposed to prepare medical students for the clinical practice. The idea of observational learning makes sense: Practical skills can be trained in skills labs until students are comfortable performing the tasks safely in actual clinical settings [1], [2]. However, it has not been analyzed so far to which extent the ability of medical students in practical clinical skills actually does improve. Enhancement of capability can often only be shown in tests with the simulator but not in a real clinical setting [3]. So far it was only possible to demonstrate a benefit of simulator training in very complex tasks such as laparoscopy, cardiac life support or the insertion of a central line [4], [5] in clinical context.
Good reasons exist to believe that the actual effect of skills training declines over time. A skills training tends to result in higher self-assessment and self-confidence of the medical students and this may be seen even after years have passed since the training [6], [7]. However, compared to untrained students, no differences in practical ability is evident after a short clinical rotation [5]. If skills labs are meant to improve manual skills of young professionals, the effect of training should be sustainable. If one argues that skills labs are predominantly supposed to enhance students‘ self-confidence and that practical skills can only be long lastingly learned by increasing contact to actual clinical settings, it is hence indispensable to address the self-assumed deficits of the students as very important. These assumed deficits may well differ from the deficits in practical ability assessed by young professionals at the start of their career [8]. Thus, the efficiency of skills labs should rather be determined by skills, which students believe to be of importance and not by concrete training to vocational preparation.
Whether there is a difference between “assumed need” and “actual requirement” has never been studied. We investigated the entitlement in procedural skills education of students and physicians in the field of internal medicine. A small survey was conducted before the implementation of the local skills lab. It was followed by an additional survey three semesters afterwards, which was larger and more representative. That way we sought to determine whether practical skills that students assumed to be of importance for them differ from those that physicians assume to be important for the students. Additionally, we were able to estimate the effect of the implementation of a skills training on the perception of the students by comparing the results of the two surveys.
Methods
Six months before the implementation of a skills training at the University of Lübeck in the field of internal medicine in October 2009 we conducted a survey among fourth-year students and physicians from the departments of internal medicine. The participants were asked to assess the importance of a training of defined practical clinical skills in the under-graduate curriculum for the start of the professional career. A group of students and consultants in the field of internal medicine had defined the items. The chosen skills were supposed to be trainable in a setting of short peer-teaching units with the possibility to expand their knowledge by means of self-study and structured exercises. Communicative skills were excluded in the first place. Twenty-six skills were selected and compiled by the selection process (see table 1 (Tab. 1)). The participants of the survey were asked to rate these skills from 0 (totally unimportant) to 10 (exceptionally important). Twenty-eight students and 30 physicians completed the form in 2009.
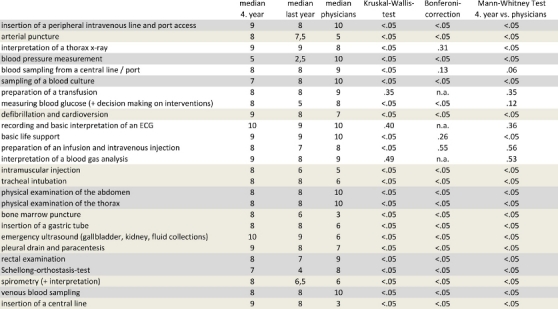
Table 1. List of items according to the questionnaire, medians of the rating (0=totally unimportant, 10=exceptionally important) and level of significance (P) of the comparisons. The Kruskal-Wallis-test detects general differences between the three groups; the Bonferoni-correction was performed to avoid the α-error of multiple testing. In a final step, the ratings of the fourth-year students were compared to the ratings of the physicians. Light-grey background colour indicates skills that were rated higher by students; dark-grey background colour indicates skills that were rated higher by physicians. n.a.= not applicable.
In April 2011 the same questionnaire was handed out to all fourth-year students of the University of Lübeck (n=214), to all final-year-students, who were doing their practical year (n=192) and to all physicians of the departments of internal medicine (n=108). Each participant completed one form only. Nine final-year students and 10 physicians had already participated in 2009 but were nonetheless included in the present analysis. The questionnaire did not collect personal data and was performed anonymously. The survey was presented to the local ethics committee, which did not consider a vote necessary due to the kind of survey that was being used (AZ 11-085A).
Additionally, in the survey the students were asked whether they had already completed the local skills training. The physicians were asked to indicate their qualification and position (less than one year of experience, more than one year of experience, specialist or consultant). If the participants could not decide between two consecutive ratings the mean value was accepted. Thus, numbers with decimal markers entered the analysis. SPSS version 12.0 was used for analysis. To detect a group difference between the three groups, the items were compared by the Kruskal-Wallis-test. To avoid the α-error, a Bonferoni-correction was performed. To compare paired samples we used the Mann-Whitney-test. A P<.05 was considered as significant.
Results
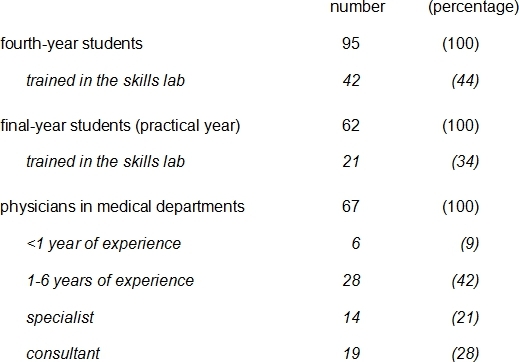
95 fourth-year students (44%), 62 final-year students (32%), and 67 physicians (62%) took part in the survey (see table 2 (Tab. 2)). Apart from missing out some items on very few forms, each form contained complete information. The results are summarized in table 1 (Tab. 1).
Table 2. Characteristics of interviewed subjects.
Skills that were assumed to be more important for students than for physicians were emergency ultrasound, defibrillation and cardioversion, pleural drainage and paracentesis, insertion of a central line, arterial puncture, intramuscular injection, intubation, bone marrow puncture, insertion of a gastric tube, and spirometry. In contrast, physicians believed blood pressure measurement, physical examination of abdomen and chest, taking a blood sample, insertion of a peripheral intravenous line, sampling of a blood culture, rectal examination, and the Schellong-orthostasis-test to be of higher importance. Students and physicians did not differ in their perspective in the following skills (in descending order): Recording and interpreting ECGs, basic life support, interpretation of chest x-rays, interpretation of blood gas analysis, taking blood from a central line, preparation of a transfusion, preparation of an intravenous injection, and measuring blood glucose (including deciding about further interventions).
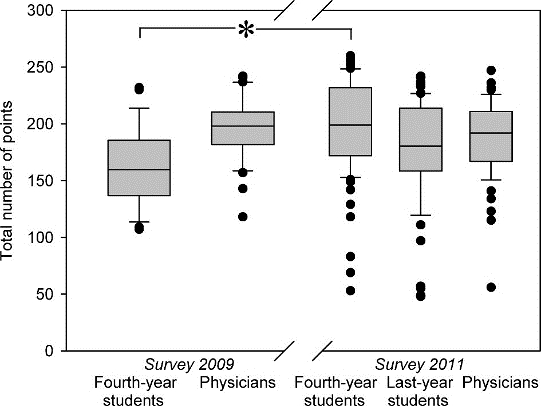
No differences could be detected in the perspective of students that already had completed a skills training and those that had not. Also, the perspective of the physicians was independent of their degree in training or their position. A high consistency in the order of ratings could be found when comparing the survey before the implementation of the local skills training and the one afterwards, both in students and in physicians (see table 3 (Tab. 3)). Merely the total number of rating points given by the students was significantly lower before the implementation of the training. No difference was noted in the group of physicians, regarding the total number of rating points (see figure 1 (Fig. 1)).
Table 3. Top ten rated skills out of the total number of 26. A comparison between fourth-year students and physicians before the implementation of a skills training in the field of internal medicine (2009) and afterwards (2011). The skills are abbreviated, for precise information and phrasing see Table 1.
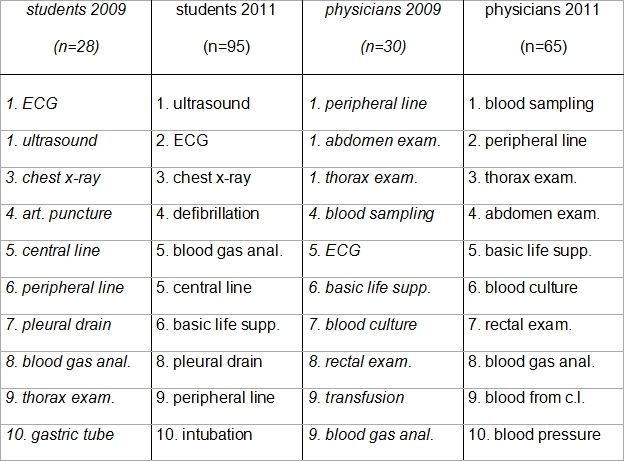
Figure 1. Total number of points given by each group. In the survey before the implementation of skills training (2009) students gave a significantly less number of points than three semesters after the implementation (2011). * P<.05.
Discussion
Interestingly, we found considerable differences in the perspective of students and physicians regarding which practical skills should be taught in the undergraduate curriculum. In fact, only for very few items there was an agreement between physicians and students. While fourth-year students focus more on complicated technical skills such as the insertion of a central line or emergency ultrasound, physicians rather assume bedside skills such as the physical examination as important. Final-year students (who are in their practical year) supported most of the views of their younger fellow students, but differed substantially from the other two groups in some items such as blood pressure measurement, measuring blood glucose and orthostatic testing. These three skills could -from the clinical point of view- be considered as “too easy” or “not worth learning”, and final-year students may believe that they should rather be concerned about learning “more important” skills. However, this effect seems to vanish when becoming a professional: No difference in ratings of physicians at the beginning of their career as compared to more experienced ones could be ascertained.
One reason for this clear discrepancy in the perspective of undergraduates and professionals could be the fact that complex practical skills are usually performed by physicians with more than two years of practical experience [9]. Students might not notice this allocation and therefore believe these technical skills as basic when working as a physician. From the physicians perspective, however, it might be less important for a beginner to perform well in these skills since the ability is important only later in career and these skills can still be trained when they are necessary. In contrast, the basic bedside skills play a much more crucial role at the start of the career. Another reason could be that students feel like they are being left alone: Especially in complex skills there is a strong correlation between the level of confidence in their own ability and the chance to be able to perform the skills under instruction [10]. Moreover, there are hardly any opportunities for undergraduate students to practice these skills, which might aggravate their insecurity.
The exact point of time for this change of perspective is not clear. In a comparison between physicians in their first year and members of the faculty, in what they believe they are required to know, the young physicians (just like the students in our study) tended to focus on technical skills such as lumbar punctures, incisions, drains and insertions of a central lines [11]. The authors, however, interpreted this result as a failure in teaching and did not conclude that different perspectives may exist. According to our results it is possible that physicians at the very beginning of their career still have the students’ point of view, since there were only six physicians that took part in our survey that were in their first year. Another study had already reported a prioritization of technical skills in third- and fourth-year students, however, this took place in a different context [12]. Although the study did not include basic clinical skills such as physical examination a similar trend was evident in the rating of 22 skills in general practice. A difference to our study can be noted in two of the skills (pleural drainage and paracentesis), which only played a minor role for the students. However, this may be linked to the reported low rate of appliance and practice of these procedures.
The impact of an implementation of a skills lab on the different ratings of skills is also an intriguing question. Despite the small size of our first survey before the implementation of the skills lab, a comparison to the latter survey sheds revealing information: The total number of points given by the students was significantly higher in the second survey. This could be due to the fact that the implementation of a skills lab might actually enhance the interest to procedural training. However, the rating of the skills, i.e. the prioritization of technical skills by the students, was the same in both surveys. Out of the ten most important rated skills only three failed to return to the top and only to be substituted by three other technical skills. This may be seen as random deviation and proof of principle particularly because in the group of physicians were also three items that were likewise replaced by three other bedside skills. Indeed, the fact that no difference in the ratings of trained and untrained students could be detected in the latest survey also argues against an impact of a skills training regarding the choice of what is assumed to be important.
A limitation of this study is that it is restricted to skills in the field of internal medicine. Also, choice und characterization of the skills that were defined with respect to the intended training may be criticized. Rather theoretical items were put next to very practical skills or both were combined in one exercise. The list of skills may also be incomplete. Nevertheless, our data clearly show the specific perspective of students on their procedural training particularly with regard to the profound and reproducible differences to the physicians’ perspective on this issue. In our faculty we consider the skills training as an instrument to activate students and to enhance their self-confidence for the clinical practice. For this reason we focus our training on the needs that the students believe to be of importance to them.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Ogden PE, Cobbs LS, Howell MR, Sibbitt SJ, DiPette DJ. Clinical simulation: importance to the internal medicine educational mission. Am J Med. 2007;120(9):820–824. doi: 10.1016/j.amjmed.2007.06.017. Available from: http://dx.doi.org/10.1016/j.amjmed.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 2.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420–1423. doi: 10.1001/archinternmed.2009.215. Available from: http://dx.doi.org/10.1001/archinternmed.2009.215. [DOI] [PubMed] [Google Scholar]
- 3.Lynagh M, Burton R, Sanson-Fisher R. A systematic review of medical skills laboratory training: where to from here? Med Educ. 2007;41(9):879–887. doi: 10.1111/j.1365-2923.2007.02821.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2007.02821.x. [DOI] [PubMed] [Google Scholar]
- 4.Okuda Y, Bryson EO, DeMaria S, Jr, Jacobson L, Quinones J, Shen B, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76(4):330–343. doi: 10.1002/msj.20127. Available from: http://dx.doi.org/10.1002/msj.20127. [DOI] [PubMed] [Google Scholar]
- 5.Smith CC, Huang GC, Newman LR, Clardy PF, Feller-Kopman D, Cho M, et al. Simulation training and its effect on long-term resident performance in central venous catheterization. Simul Healthc. 2010;5(3):146–151. doi: 10.1097/SIH.0b013e3181dd9672. Available from: http://dx.doi.org/10.1097/SIH.0b013e3181dd9672. [DOI] [PubMed] [Google Scholar]
- 6.Liddell MJ, Davidson SK, Taub H, Whitecross LE. Evaluation of procedural skills training in an undergraduate curriculum. Med Educ. 2002;36(11):1035–1041. doi: 10.1046/j.1365-2923.2002.01306.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.2002.01306.x. [DOI] [PubMed] [Google Scholar]
- 7.Niemi-Murola L, Helenius I, Turunen J, Remes V. Graduating medical students and emergency procedure skill teaching in Finland--does a clinical skills centre make the difference? Med Teach. 2007;29(8):821–826. doi: 10.1080/01421590701601568. Available from: http://dx.doi.org/10.1080/01421590701601568. [DOI] [PubMed] [Google Scholar]
- 8.Turner SR, de Gara CJ. Medical students and recent graduates may disagree on the importance of procedural skills education. Med Teach. 2010;32(2):182. [PubMed] [Google Scholar]
- 9.Connick RM, Connick P, Klotsas AE, Tsagkaraki PA, Gkrania-Klotsas E. Procedural confidence in hospital based practitioners: implications for the training and practice of doctors at all grades. BMC Med Educ. 2009;9:2. doi: 10.1186/1472-6920-9-2. Available from: http://dx.doi.org/10.1186/1472-6920-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen W, Liao SC, Tsai CH, Huang CC, Lin CC, Tsai CH. Clinical skills in final-year medical students: the relationship between self-reported confidence and direct observation by faculty or residents. Ann Acad Med Singapore. 2008;37(1):3–8. [PubMed] [Google Scholar]
- 11.Fitch MT, Kearns S, Manthey DE. Faculty physicians and new physicians disagree about which procedures are essential to learn in medical school. Med Teach. 2009;31(4):342–347. doi: 10.1080/01421590802520964. Available from: http://dx.doi.org/10.1080/01421590802520964. [DOI] [PubMed] [Google Scholar]
- 12.Wu EH, Elnicki DM, Alper EJ, Bost JE, Corbett EC, Jr, Fagan MJ, Mechaber AJ, Ogden PE, Sebastian JL, Torre DM. Procedural and interpretive skills of medical students: experiences and attitudes of fourth-year students. Acad Med. 2008;83(10 Suppl):S63–S67. doi: 10.1097/ACM.0b013e318183c5a7. Available from: http://dx.doi.org/10.1097/ACM.0b013e318183c5a7. [DOI] [PubMed] [Google Scholar]


