Abstract
Neuroendocrine tumours (NETs) are often indolent malignancies that commonly present with metastatic disease in the liver. Surgical, locoregional, and systemic treatment modalities are reviewed. A multidisciplinary approach to patient care is suggested to ensure all therapeutic options explored.
1. Introduction
Neuroendocrine tumours (NETs) are uncommon tumours that can arise anywhere within the body, but predominantly from the gastroenteropancreatic tract. Recent epidemiological evidence suggest that the incidence of all NETs is approximately 3–5 per 100,000 population per year with a prevalence of 35 per 100,000 population because of slow tumour growth [1, 2]. Though most NETs are nonfunctional, others secrete peptide hormones that can cause clinical syndromes, like flushing, diarrhoea, bronchospasm and palpitations seen with carcinoid syndrome. The majority of these tumours are indolent, slow growing malignancies, commonly presenting with metastatic disease. The most common site of distant metastases is the liver. Consequently, many therapies are focused at treating the primary and also the metastatic disease in the liver. Due to the indolent nature of most of these tumours, the 5-year survival of patients with metastatic disease at presentation is approximately 50%. There may have been some improvement in survival from medical and surgical therapies. New molecular-targeted therapies and an aggressive surgical approach to resection of primary and secondary tumours show benefit.
This paper focuses on management of liver metastases of NETs and covers both surgery, locoregional, and systemic therapy. In general, local therapies to the liver should be considered first if disease is confined to the liver. This allows systemic therapies to be given at a later stage if there is extrahepatic spread. Results for liver-directed and systemic therapy of neuroendocrine tumour liver metastases are summarised in Tables 1 and 2, respectively.
Table 1.
Summary of results for liver-directed therapy of neuroendocrine tumour liver metastases.
| Modality author [Ref] | Intervention | Number of patients |
Overall survival (5 years) | Median survivals (months) | Progression/disease-free survival | Clinical response | Biochemical response | Radiological response |
|---|---|---|---|---|---|---|---|---|
| Liver surgery | ||||||||
|
| ||||||||
| Sarmiento et al. [3] | Resection | 170 | 61% | |||||
| Touzios et al. [4] | Resection ± ablation | 18 | 72% | >96 | ||||
| Grazi et al. [5] | Resection | 19 | 92% (4 yrs) | |||||
| Kianmanesh et al. [6] | Resection | 23 | 94% | 50% (5 yrs) | ||||
| Gomez et al. [7] | Resection | 18 | 86% | 66% (5 yrs) | ||||
| Scigliano et al. [8] | Resection | 41 | 79% | 3% (5 yrs) | ||||
| Osborne et al. [9] | Cytoreduction | 61 | Curative-50 (mean) | |||||
| Palliative-32 (mean) | ||||||||
| Musunuru et al. [10] | Resection ± ablation | 13 | 83% (3 yrs) | |||||
| Mayo et al. [11] | Resection ± ablation | 339 | 74% | 125 | ||||
|
| ||||||||
| Liver transplantation | ||||||||
|
| ||||||||
| Lehnert [12] | 103 | 47% | ||||||
| Olausson et al. [13] | 15 | 90% | 20% (5 years) | |||||
| Le Treut et al. [14] | 85 | 47% | ||||||
|
| ||||||||
| Embolisation | ||||||||
|
| ||||||||
| Ho et al. [15] | TAE or TACE | 46 | 42 | 18 months | ||||
| Ruutiainen et al. [16] | TACE | 57 | 50% | 35% (3 yrs) | ||||
| Strosberg et al. [17] | TAE | 84 | 36 | |||||
| Dong and Carr [18] | TACE | 123 | 36% | 39 (mean) | ||||
| Ruszniewski et al. [19] | TACE | 24 | 73% | 57% | 33% | |||
| Gupta et al. [20] | TAE or TACE | 69 (Carcinoid) | 22 months | 67% | ||||
| 54 (Pancreatic) | 16 months | 35% | ||||||
|
| ||||||||
| RFA | ||||||||
|
| ||||||||
| Mazzaglia et al. [21] | 63 | 46 (after RFA) | 70% | |||||
|
| ||||||||
| SIRT | ||||||||
|
| ||||||||
| King et al. [22] | 37 | 29 (mean) | 55% | 43% | 50% | |||
| Kennedy et al. [23] | 148 | 70 | 63% | |||||
| Cao et al. [24] | 58 | 47% (3 yrs) | 36 | 34% | ||||
| Saxena et al. [25] | 48 | 35 | 55% | |||||
Table 2.
Summary of results for systemic therapy of neuroendocrine tumour liver metastases.
| Modality author [Ref] | Intervention | Number of patients |
Overall survival (5 years) | Median survivals (months) | Progression/disease-free survival | Clinical response | Biochemical response | Radiological response |
|---|---|---|---|---|---|---|---|---|
| Biological Therapy | ||||||||
|
| ||||||||
| Ducreux et al. [26] | Lantreotide | 46 | 5% | |||||
| Aparicio et al. [27] | Octreotide | 35 | 11 months | 3% (57% stabilised) | ||||
| Rinke et al. [28] | Octreotide LAR | 85 | 14.3 months | 67% stabilised | ||||
| Oberg and Eriksson [29] | IFN α | 111 | >80 | 34 months | 68% | 42% | 15% (39% stabilised) | |
| Arnold et al. [30] | Octreotide ± IFN α | 109 | 32 versus 54 (combined) | 1.9% (27% stabilised) | ||||
| Fjällskog et al. [31] | Somatostatin ± IFN α | 16 | 62.5% | 19% | ||||
|
| ||||||||
| Chemotherapy | ||||||||
|
| ||||||||
| Moertel et al. [32] | STZ + doxorubicin | 36 | 26 | 20 months | 69% | |||
| STZ + 5FU | 33 | 18 | 6.9 months | 45% | ||||
| Turner et al. [33] | 5FU + cisplatin + STZ | 79 | 31.5 | 9.1 months | 33% | |||
| Sun et al. [34] | STZ + doxorubicin | 85 | 15.7 | 4.5 months | 15.9% | |||
| STZ + 5FU | 78 | 24.3 | 5.3 months | 16% | ||||
| Kouvaraki et al. [35] | 5FU + doxorubicin + STZ | 61 | 74% (2 yrs) | 41% (2 years) | ||||
| Strosberg et al. [36] | Temolozomide + capecitabine | 30 | 92% (2 yrs) | 18 months | 70% | |||
| Moertel et al. [37] | Etoposide + cisplatin | 18 | 19 | 8 months | 67% | |||
|
| ||||||||
| Molecular-targeted therapy | ||||||||
|
| ||||||||
| Raymond et al. [38] | Sunitinib | 171 | 11.4 months | 9.3% | ||||
| Yao et al. [39] | Everolimus | 410 | 34% (1.5 yrs) | 11 months | ||||
| Yao et al. [40] | Bevacizumab | 44 | 95% (18 weeks) | |||||
|
| ||||||||
| PPRT | ||||||||
|
| ||||||||
| Cwikla et al. [41] | DOTATATE Y-90 | 60 | 22 | 17 months | 72% | 23% | ||
| Kwekkeboom et al. [42] | 177Lu-octreotate | 131 | >36 months | 28% | ||||
| Pfeifer et al. [43] | Y-DOTATOC or 177Lu-DOTATOC | 69 | 29 months | 23.6% | ||||
| Kwekkeboom et al. [44] | 177Lu-DOTA 0,Tyr3 | 310 | 46 | 40 months | 30% | |||
2. Liver-directed Therapies
Consensus guidance recommends surgery for liver metastases in well-differentiated NETs if complete resection or debulking of <90% tumour load is feasible [45]. However, intended curative surgery is only possible in less than 10% of patients who are diagnosed with hepatic metastases at presentation [3, 46–49]. The distribution of liver metastases affects survival; solitary metastases, isolated metastatic bulk with smaller accompanying deposits, and disseminated metastatic spread have 5-year survival rates of 100%, 84%, and 51%, respectively [50].
An aggressive surgical approach to resecting liver metastases is supported by significantly improved actuarial survival in series compared to nonrandomised controls [3–5]. A number of different surgical approaches are available depending on the distribution of metastases. If primarily unilobar metastases are present, a one-step approach can be adopted. In these cases, resection of the primary plus liver resection can be performed. A two-step surgical approach to bilobar metastases from luminal NETs with resection of the primary, limited resection of left liver lobe metastases, and right portal vein ligation followed by right hepatectomy has been proposed [6]. Overall survival and disease-free rates at 5 years were 94% and 50% with this approach. Other series report a range of overall survival and disease-free rates [7–9, 51]. A significant improvement in 3-year survival for surgical resection over medical treatment or embolisation has been demonstrated in a study limited by bias. [10]. The completeness of resection, in particular resection margin involvement, is thought to be more important than the number, localization, and size of liver metastases [7, 52, 53]. Histological grade and extrahepatic disease are predictive of overall survival [54, 55]. Disease has been shown to recur in 78–94% of patients at 5 years [3, 8, 11].
After surgery, patients with functioning tumours have prolonged partial or complete symptomatic response rates that can contribute to improved quality of life [11, 56, 57]. Patients with carcinoid tumours have reduced biomarkers (e.g., Chromogranin A and urinary 5-HIAA) after surgery that correlate with symptom relief and disease control [3, 58]. Some rarer functioning syndromes, like those related to PTHrP or VIP secretion, can be improved by debulking surgery [59].
There is no evidence from randomised clinical trials supporting liver surgery, either for curative resection or for debulking in nonresectable disease, over other treatment modalities. Liver surgery only achieved significance in improving survival in univariate but not multivariate analysis [60–62]. Neoadjuvant strategies for downsizing liver metastases or adjuvant chemotherapy following hepatic resection have not yet been subject to controlled clinical trials [63–65].
2.1. Surgery to Primary Tumour in Metastatic NETs
Recent guidelines recommend resection of the primary tumour and mesenteric lymph nodes in jejunum/ileum NETs [66–68]. Tumour mass reduction or debulking of primary jejunal and ileal NETs reduces the possibility of bowel ischaemia and obstruction from tumour and mesenteric lymph nodes mass effect even in the context of liver metastases. Resection of the primary tumour has been shown to be an independent positive predictor of survival (P = 0.015) and associated with a significantly longer survival than no resection (median survival 7.4 versus 4.0 years; P < 0.01) [62, 69]. Successful resection of mesenteric metastases and the desmoplastic reaction around the primary site are also associated with a significantly longer survival. Significant reductions in tumour-related symptoms are also seen after primary and mesenteric lymph node resections.
Aggressive surgery to primary tumours and resectable liver metastases in pancreatic NETs is recommended [67, 70]. Resection of pancreatic NETs has been suggested to be associated with significantly improved survival compared to those who did not undergo resection (114 months versus 35 months; P < .0001) though significant biases may exist in this study [71]. This survival benefit was demonstrated for patients with localized, regional, and metastatic disease with an adjusted odds ratio of 0.48. Independent predictors of survival after resection of pancreatic NETs include age, grade, presence of distant metastases, tumour functionality, and type of resection [72]. Current guidelines do not recommend surgery to the primary pancreatic tumour in patients with unresectable liver metastases [70, 73].
2.2. Transplantation
The role of orthotopic liver transplant is controversial given the demand for donor organs and a lack of clear selection criteria [74]. Patients with debilitating and poorly controlled hormonal syndromes from small intestine or pancreatic NETs are considered for transplantation as symptom relief is seen in 90% of patients following surgery [12, 13, 75–78]. Five-year recurrence-free rates vary from 25–50%. Overall five-year survival rates are around 50% but vary according to patient selection [13, 14, 79, 80]. Patients presenting with duodenal or pancreatic NET in association with hepatomegaly have poorer outcomes (12% versus 68% five-year survival rates) [14]. The presence of extensive extrahepatic tumour resected at the time of transplantation is associated with poorer median and five-year survival rates of ten months and 30%, respectively [12]. Important selection criteria include well-differentiated tumours, low proliferation rate (Ki-67 < 10%), and regular E-Cadherin staining [81, 82]. The Milan criteria for transplantation include age less than 55 years, low grade carcinoid NET, limited metastatic disease in the liver (<50%), previously resected tumours drained only by the portal system (pancreas and mid gut origin NETs), and stable disease for 6 months [83]. Combination treatment with chemotherapeutic agents, chemoembolisation, systemic radiopeptide treatment, and aggressive surgery for recurrence may lead to improved survival rates [84–86].
2.3. Embolisation
NET liver metastases are highly vascular with an arterial supply that if occluded will lead to ischaemia and necrosis. Normal tissue is supplied from the portal vein and preserved during embolisation of hepatic arteries. A catheter is guided to the hepatic artery or branch and material (gelfoam powder, microembospheres, and polyvinyl alcohol particles) released to occlude the vessel in bland embolisation. In chemoembolisation, cytotoxics (like cisplatin, mirplatin, gemcitabine, doxorubicin, streptozocin, and 5-FU) are injected prior to arterial embolisation in order to achieve higher concentrations and prolonged action in necrotic tissue [87–89]. Contraindications to embolisation include occlusion of the portal vein, severe liver dysfunction, and presence of biliary anastomosis. Relative contraindications include tumour burden, renal impairment, and heart disease (including carcinoid heart disease) [90, 91]. A postembolisation syndrome may occur with abdominal pain, vomiting, fever, and rise in transaminases.
Vascular occlusion can achieve reduced hormonal symptoms from NET syndromes, reduced tumour burden, and improved survival in patients who have tried medical therapy and who are not suitable for surgical resection [92–95]. Sequential hepatic artery occlusion can offer prolonged palliation for responsive patients even if performed later in their clinical course [90, 96, 97].
Median survival rates after transarterial embolisation (TAE) or chemoembolistaion (TACE) in patients with liver metastases is over 3 years with progression-free survival (PFS) of around 18 months [15–18, 98–100]. Clinical response rates of over 90% are seen following treatment [91]. Intact primary tumour, extensive liver disease, and bone metastases are associated with worse outcomes. Embolisation of nonresectable liver metastases often results in disease regression in patients with carcinoid or pancreatic NETs [17, 19]. TACE appears to benefit patients with pancreatic NETs while TAE benefits those with ileal NETs [20]. A small randomized study of TAE versus TACE in all liver NETs has shown no difference in time to progression [101].
2.4. Radiofrequency Ablation (RFA)
RFA of oligonodular liver metastases (fewer than 8) of less than 5 cm can result in symptomatic response in 70–80% of patients with hormonal syndromes for as long as 24 months [21, 63, 102, 103]. Electrical energy is delivered to tissues via a catheter, inserted percutaneously or laparoscopically, which leads to heating and cell death [104, 105]. Microwave RFA can reduce time required for this procedure. RFA can play an important role in the treatment of carcinoid metastases not suitable for surgical resection and refractory to TAE, improving symptom control, reducing octreotide dependence, and slowing progression in patients [106–108]. Limitations to using RFA include increased numbers and size of liver metastases as well as the detrimental cooling effect of blood flow from neighbouring blood vessels. Local recurrence has been identified in 21.7% of tumours on CT scans with a mean follow-up of 17 months. Recurrence can be predicted by tumour type and size, ablation margin, and blood vessel proximity [103, 109]. Median survival after starting RFA treatment is 3.9 years [21]. Although RFA may play a promising role in the treatment of liver metastases from NETs, its effect on survival and tumour progression needs to be explored in larger studies. In particular, studies are needed comparing surgical resection with RFA.
2.5. Selective Internal Radiation Therapy (SIRT)
Radioembolisation of liver metastases can be achieved with Yttrium-90 resin microspheres in patients with disseminated and inoperable liver disease even if previous TAE or TACE has taken place [22, 110]. (90 Y) microspheres are injected through a percutaneously placed hepatic artery catheter via the femoral or brachial artery. Contraindication to SIRT is similar to those of bland embolisation, vascular involvement such as portal vein thrombosis, severe liver dysfunction, and large tumour burden. Long-term radiologic and biological responses can be achieved with radioembolisation with partial or complete response seen in 63% [22, 23]. Median survival varies from 36 to 70 months [23, 24]. Prognostic factors include radiographic response to treatment, tumour grade, and presence of extrahepatic disease. Patients with hepatic tumour burden of 20–50% by volume, well-differentiated tumour, female gender, and no extrahepatic disease benefit most from treatment [25]. There is no randomized evidence that radiologic and symptom response rates following SIRT are different from those seen with TACE and TAE.
3. Systemic Therapies
3.1. Biological Therapy
Over 70% of NETs express cell-surface somatostatin receptors that are targeted by synthetic somatostatin analogues. Patients with functional NETs can derive significant symptomatic benefit from the use of somatostatin analogues that suppress the secretion of peptide hormones. Octreotide can provide symptomatic response in up to 85% of patients and biochemical response in up to 70% of patients within weeks of commencement [111, 112]. Patients with NETs undergoing interventional procedures can experience severe symptoms related to the release of vasoactive hormones, like serotonin, that can cause a carcinoid crisis with bronchospasm, tachycardia, and labile blood pressure. This can be ameliorated through the use of octreotide infusions before, during, and after interventional procedures.
Some groups have reported an antiproliferative property of somatostatin analogues [26, 27, 112, 113]. Octreotide LAR has been found to significantly lengthen the time to tumour progression compared to placebo injections (14.3 versus 6 months resp.) [28]. The benefit was seen in both functionally active and inactive tumours. Patients with low hepatic tumour load and resected primary tumour benefited the most from treatment with octreotide LAR. Overall, survival was not an endpoint of this study, consequently; survival benefit from the use of somatostatin analogues has not been confirmed.
Interferon alpha 3–5 megaunits 3–5 times per week have been used with some symptomatic response, but no clear reduction in tumour size or survival benefit [29–31, 114, 115]. Interferon alpha should be considered as second-line biological therapy after somatostatin analogues.
3.2. Chemotherapy
Systemic chemotherapy has a role in the treatment of pancreatic and high grade NETs. Patient selection and individualized treatment are required to minimize toxicity, maximize response, and improve overall quality of life. The degree of differentiation and tumour grade of NETs can guide management [116, 117]. Poorly differentiated and high-proliferative tumours (from histological grading like Ki-67 and mitotic index) behave more aggressively but are more sensitive to cytotoxic therapy than well-differentiated and low-proliferative tumours (Ki-67 < 10%) [33]. Objective response to chemotherapy varies between 25–78% with progression-free periods between 4–22 months [32, 34, 37, 118–124]. Therefore, it is essential to ensure that chemotherapy is offered to patients who are likely to respond; those with pancreatic NETs, aggressive phenotypes, and high proliferation rates [125]. Biochemical and radiological progression in asymptomatic patients identifies those with rapidly progressive disease and an aggressive phenotype [67]. Response to cytotoxic therapy can be established from radiological-quantified reduction in tumour size, improved biochemical markers as well as improvements in quality of life as measured by health questionnaires [126–128].
Single-agent chemotherapy is seldom used because of limited response rates, toxicity, and poor survival rates. Newer agents like paclitaxel, temozolomide, topotecan, and gemcitabine are not markedly better than older agents like streptozocin, dacarbazine, 5 flourouracil, and doxorubicin when used as monotherapy [121, 126, 129–135]. In patients with pancreatic NET, combination chemotherapy with streptozocin and doxorubicin is superior to streptozocin and 5FU in terms of response rates, time to progression, and overall survival [32, 136, 137]. Response rates from streptozocin and doxorubicin combination treatment vary between 30–70% [33–35, 138]. Recently, a retrospective analysis of capecitabine and temozolomide combination chemotherapy has demonstrated good response rates, superior to traditional streptozocin-based chemotherapy [36]. In 30 patients treated with capecitabine and temozolomide, response rates of 70%, progression-free survival of 18 months and overall survival of 92% at 2 years were observed. However, streptozocin-based therapy remains the standard chemotherapy regime for pancreatic NETs given the lack of data from randomised trials demonstrating benefit from other regimes [36, 116, 123, 139, 140]. Poorly differentiated or anaplastic NETs respond to a combination of cisplatin and etoposide, a regime used in small cell lung cancer [37, 118–120]. Despite chemotherapy, the prognosis remains poor in this group with a 2-year survival between 20–30%.
3.3. Molecular-Targeted Therapies
Novel systemic agents target the molecular mechanisms that are implicated in the pathogenesis of NETs [141, 142].
Sunitinib, a multitargeted tyrosine kinase inhibitor, has activity against a range of molecular targets, including VEGF receptors and platelet-derived growth factor receptors, and has been shown to have antitumour activity in pancreatic NETs [143]. Median PFS is significantly longer in patients treated with sunitinib over placebo (11.4 versus 5.5 months) [38]. Objective response rates and overall survival are also improved with sunitinib treatment. Frequent adverse events encountered include diarrhoea, nausea, vomiting, asthenia, and fatigue.
Everolimus, an oral inhibitor of mammalian target of rapamycin (mTOR), has activity against pancreatic NET tumours through a mechanism of cellular apoptosis and antiangiogenesis [144, 145]. Median PFS is significantly longer in those treated with everolimus over placebo (11 versus 4.6 months) [39]. Severe adverse events like hyperglycaemia and anaemia were rare, with stomatitis, diarrhoea, and fatigue are more commonly seen.
Vascular endothelial growth factor (VEGF) is overexpressed in NETs and targeted by the ligand monoclonal antibody Bevacizumab [40, 146, 147]. There are reports of clinical benefit when combined with existing chemotherapy treatments [148, 149].
3.4. Peptide Receptor Radionuclide Therapy (PRRT)
Somatostatin receptors subtype 2 are expressed in the majority of NETs and confirmed through uptake in octreotide scintigraphy or somatostatin-based PET imaging [150–152]. Beta-emitting 90 Y- and 177 Lu-labeled somatostatin analogues have been studied in patients with metastatic and inoperable disease [41, 42, 153–156]. The majority of patients develop stable disease with the average time to progression of 40 months from commencing therapy. Partial and complete objective responses are seen in up to 30% of patients with median PFS of over 2 years [43, 157]. From diagnosis, there is a survival benefit of 40–72 months compared to historical controls [44]. Predictive factors include high tumour uptake on scintigraphy and limited liver metastases. Adverse events include bone marrow and liver toxicity as well as radiation-induced lose of renal function and gastrointestinal disturbance from the use of renoprotective agents [158, 159]. The addition of radiosensitisers like gemcitabine and capecitabine to PPRT may improve clinical outcomes [160, 161]. Alpha-emitting isotopes, such as actinum-225 (225Ac), have a higher cytotoxic activity than beta emitters and may be used in PRRT [162].
MIBG scans are also used to identify patients with metastatic NETs. 131 I-MIBG therapy is associated with significantly improved 5-year survival rates of 85% (nonrandomized studies) as well as marked symptomatic and hormonal improvement [163–165]. Symptomatic response predicts improved survival.
4. Conclusion
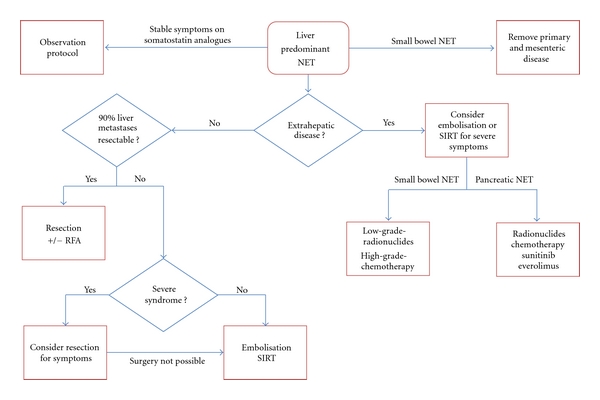
There are a number of treatment modalities available in the management of neuroendocrine tumour liver metastases with a treatment algorithm outlined in Figure 1. Proactive surgical resection, with curative intent or for debulking (cytoreduction), has been shown to improve outcomes and should be pursued initially. In patients with more advanced disease or not amenable to surgical resection, locoregional therapies, like embolisation and SIRT, offer improved outcomes and may downstage disease. Newer systemic therapies, in particular PRRT and molecular targeted therapies, can play a role in patients with extrahepatic and progressive disease. Although there is a lack of robust evidence-based data in the management of patients with metastatic NETs, the future appears more positive with the range of treatment options available. An individualized approach to patient care is needed given the breadth of symptoms and disease, the lack of a validated treatment pathway as well as the indolent nature of NETs. Patient care should be managed under the auspices of a multidisciplinary team to ensure that all treatment options are explored both at diagnosis and follow-up.
Figure 1.
References
- 1.Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. Journal of Clinical Oncology. 2008;26(18):3063–3072. doi: 10.1200/JCO.2007.15.4377. [DOI] [PubMed] [Google Scholar]
- 2.Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934–959. doi: 10.1002/cncr.11105. [DOI] [PubMed] [Google Scholar]
- 3.Sarmiento JM, Heywood G, Rubin J, Ilstrup DM, Nagorney DM, Que FG. Surgical treatment of neuroendocrine metastases to the liver: a plea for resection to increase survival. Journal of the American College of Surgeons. 2003;197(1):29–37. doi: 10.1016/S1072-7515(03)00230-8. [DOI] [PubMed] [Google Scholar]
- 4.Touzios JG, Kiely JM, Pitt SC, et al. Neuroendocrine hepatic metastases: does aggressive management improve survival? Annals of Surgery. 2005;241(5):776–785. doi: 10.1097/01.sla.0000161981.58631.ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grazi GL, Cescon M, Pierangeli F, et al. Highly aggressive policy of hepatic resections for neuroendocrine liver metastases. Hepato-Gastroenterology. 2000;47(32):481–486. [PubMed] [Google Scholar]
- 6.Kianmanesh R, Sauvanet A, Hentic O, et al. Two-step surgery for synchronous bilobar liver metastases from digestive endocrine tumors: a safe approach for radical resection. Annals of Surgery. 2008;247(4):659–665. doi: 10.1097/SLA.0b013e31816a7061. [DOI] [PubMed] [Google Scholar]
- 7.Gomez D, Malik HZ, Al-Mukthar A, et al. Hepatic resection for metastatic gastrointestinal and pancreatic neuroendocrine tumours: outcome and prognostic predictors. HPB. 2007;9(5):345–351. doi: 10.1080/13651820701504199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scigliano S, Lebtahi R, Maire F, et al. Clinical and imaging follow-up after exhaustive liver resection of endocrine metastases: a 15-year monocentric experience. Endocrine-Related Cancer. 2009;16(3):977–990. doi: 10.1677/ERC-08-0247. [DOI] [PubMed] [Google Scholar]
- 9.Osborne DA, Zervos EE, Strosberg J, et al. Improved outcome with cytoreduction versus embolization for symptomatic hepatic metastases of carcinoid and neuroendocrine tumors. Annals of Surgical Oncology. 2006;13(4):572–581. doi: 10.1245/ASO.2006.03.071. [DOI] [PubMed] [Google Scholar]
- 10.Musunuru S, Chen H, Rajpal S, et al. Metastatic neuroendocrine hepatic tumors: resection improves survival. Archives of Surgery. 2006;141(10):1000–1004. doi: 10.1001/archsurg.141.10.1000. [DOI] [PubMed] [Google Scholar]
- 11.Mayo SC, de Jong MC, Pulitano C, et al. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Annals of Surgical Oncology. 2010;17(12):3129–3136. doi: 10.1245/s10434-010-1154-5. [DOI] [PubMed] [Google Scholar]
- 12.Lehnert T. Liver transplantation for metastatic neuroendocrine carcinoma: an analysis of 103 patients. Transplantation. 1998;66(10):1307–1312. doi: 10.1097/00007890-199811270-00007. [DOI] [PubMed] [Google Scholar]
- 13.Olausson M, Friman S, Herienius G, et al. Orthotopic liver of multivisceral transplantation as treatment of metastatic neuroendocrine tumors. Liver Transplantation. 2007;13(3):327–333. doi: 10.1002/lt.21056. [DOI] [PubMed] [Google Scholar]
- 14.Le Treut YP, Grégoire E, Belghiti J, et al. Predictors of long-term survival after liver transplantation for metastatic endocrine tumors: an 85-case French multicentric report. American Journal of Transplantation. 2008;8(6):1205–1213. doi: 10.1111/j.1600-6143.2008.02233.x. [DOI] [PubMed] [Google Scholar]
- 15.Ho AS, Picus J, Darcy MD, et al. Long-term outcome after chemoembolization and embolization of hepatic metastatic lesions from neuroendocrine tumors. American Journal of Roentgenology. 2007;188(5):1201–1207. doi: 10.2214/AJR.06.0933. [DOI] [PubMed] [Google Scholar]
- 16.Ruutiainen AT, Soulen MC, Tuite CM, et al. Chemoembolization and bland embolization of neuroendocrine tumor metastases to the liver. Journal of Vascular and Interventional Radiology. 2007;18(7):847–855. doi: 10.1016/j.jvir.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 17.Strosberg JR, Choi J, Cantor AB, Kvols LK. Selective hepatic artery embolization for treatment of patients with metastatic carcinoid and pancreatic endocrine tumors. Cancer Control. 2006;13(1):72–78. doi: 10.1177/107327480601300110. [DOI] [PubMed] [Google Scholar]
- 18.Dong XD, Carr BI. Hepatic artery chemoembolization for the treatment of liver metastases from neuroendocrine tumors: a long-term follow-up in 123 patients. Medical Oncology. 2010;28, supplement 1:286–290. doi: 10.1007/s12032-010-9750-6. [DOI] [PubMed] [Google Scholar]
- 19.Ruszniewski P, Rougier P, Roche A, et al. Hepatic arterial chemoembolization in patients with liver metastases of endocrine tumors: a prospective Phase II study in 24 patients. Cancer. 1993;71(8):2624–2630. doi: 10.1002/1097-0142(19930415)71:8<2624::aid-cncr2820710830>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 20.Gupta S, Johnson MM, Murthy R, et al. Hepatic arterial embolization and chemoembolization for the treatment of patients with metastatic neuroendocrine tumors: variables affecting response rates and survival. Cancer. 2005;104(8):1590–1602. doi: 10.1002/cncr.21389. [DOI] [PubMed] [Google Scholar]
- 21.Mazzaglia PJ, Berber E, Milas M, Siperstein AE. Laparoscopic radiofrequency ablation of neuroendocrine liver metastases: a 10-year experience evaluating predictors of survival. Surgery. 2007;142(1):10–19. doi: 10.1016/j.surg.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 22.King J, Quinn R, Glenn DM, et al. Radioembolization with selective internal radiation microspheres for neuroendocrine liver metastases. Cancer. 2008;113(5):921–929. doi: 10.1002/cncr.23685. [DOI] [PubMed] [Google Scholar]
- 23.Kennedy AS, Dezarn WA, McNeillie P, et al. Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. American Journal of Clinical Oncology. 2008;31(3):271–279. doi: 10.1097/COC.0b013e31815e4557. [DOI] [PubMed] [Google Scholar]
- 24.Cao CQ, Yan TD, Bester L, Liauw W, Morris DL. Radioembolization with yttrium microspheres for neuroendocrine tumour liver metastases. British Journal of Surgery. 2010;97(4):537–543. doi: 10.1002/bjs.6931. [DOI] [PubMed] [Google Scholar]
- 25.Saxena A, Chua TC, Bester L, Kokandi A, Morris DL. Factors predicting response and survival after yttrium-90 radioembolization of unresectable neuroendocrine tumor liver metastases: a critical appraisal of 48 cases. Annals of Surgery. 2010;251(5):910–916. doi: 10.1097/SLA.0b013e3181d3d24a. [DOI] [PubMed] [Google Scholar]
- 26.Ducreux M, Ruszniewski P, Chayvialle JA, et al. The antitumoral effect of the long-acting somatostatin analog lanreotide in neuroendocrine tumors. American Journal of Gastroenterology. 2000;95(11):3276–3281. doi: 10.1111/j.1572-0241.2000.03210.x. [DOI] [PubMed] [Google Scholar]
- 27.Aparicio T, Ducreux M, Baudin E, et al. Antitumour activity of somatostatin analogues in progressive metastatic neuroendocrine tumours. European Journal of Cancer. 2001;37(8):1014–1019. doi: 10.1016/s0959-8049(01)00073-9. [DOI] [PubMed] [Google Scholar]
- 28.Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID study group. Journal of Clinical Oncology. 2009;27(28):4656–4663. doi: 10.1200/JCO.2009.22.8510. [DOI] [PubMed] [Google Scholar]
- 29.Oberg K, Eriksson B. The role of interferons in the management of carcinoid tumours. British Journal of Haematology. 1991;79(1, supplement):74–77. doi: 10.1111/j.1365-2141.1991.tb08125.x. [DOI] [PubMed] [Google Scholar]
- 30.Arnold R, Rinke A, Klose K-J, Müller H-H, Wied M, Zamzow K. Octreotide versus octreotide plus interferon-alpha in endocrine gastroenteropancreatic tumors: a randomized trial. Clinical Gastroenterology and Hepatology. 2005;3(8):761–771. doi: 10.1016/s1542-3565(05)00481-7. [DOI] [PubMed] [Google Scholar]
- 31.Fjällskog M-L, Sundin A, Westlin J-E, Öberg K, Janson ET, Eriksson B. Treatment of malignant endocrine pancreatic tumors with a combination of α-interferon and somatostatin analogs. Medical Oncology. 2002;19(1):35–42. doi: 10.1385/MO:19:1:35. [DOI] [PubMed] [Google Scholar]
- 32.Moertel CG, Lefkopoulo M, Lipsitz S, Hahn RG, Klaassen D. Streptozocin-doxorubicin, streptozocin-fluorouracil, or chlorozotocin in the treatment of advanced islet-cell carcinoma. New England Journal of Medicine. 1992;326(8):519–523. doi: 10.1056/NEJM199202203260804. [DOI] [PubMed] [Google Scholar]
- 33.Turner NC, Strauss SJ, Sarker D, et al. Chemotherapy with 5-fluorouracil, cisplatin and streptozocin for neuroendocrine tumours. British Journal of Cancer. 2010;102(7):1106–1112. doi: 10.1038/sj.bjc.6605618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun W, Lipsitz S, Catalano P, Mailliard JA, Haller DG. Phase II/III study of doxorubicin with fluorouracil compared with streptozocin with fluorouracil or dacarbazine in the treatment of advanced carcinoid tumors. Eastern Cooperative Oncology Group Study E1281. Journal of Clinical Oncology. 2005;23(22):4897–4904. doi: 10.1200/JCO.2005.03.616. [DOI] [PubMed] [Google Scholar]
- 35.Kouvaraki MA, Ajani JA, Hoff P, et al. Fluorouracil, doxorubicin, and streptozocin in the treatment of patients with locally advanced and metastatic pancreatic endocrine carcinomas. Journal of Clinical Oncology. 2004;22(23):4762–4771. doi: 10.1200/JCO.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 36.Strosberg JR, Fine RL, Choi J, et al. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer. 2011;117(2):268–275. doi: 10.1002/cncr.25425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moertel CG, Kvols LK, O’Connell MJ, Rubin J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin: evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer. 1991;68(2):227–232. doi: 10.1002/1097-0142(19910715)68:2<227::aid-cncr2820680202>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 38.Raymond E, Dahan L, Raoul J-L, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. New England Journal of Medicine. 2011;364(6):501–513. doi: 10.1056/NEJMoa1003825. [DOI] [PubMed] [Google Scholar]
- 39.Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. New England Journal of Medicine. 2011;364(6):514–523. doi: 10.1056/NEJMoa1009290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yao JC, Phan A, Hoff PM, et al. Targeting vascular endothelial growth factor in advanced carcinoid tumor: a random assignment phase ii study of depot octreotide with bevacizumab and pegylated interferon alfa-2b. Journal of Clinical Oncology. 2008;26(8):1316–1323. doi: 10.1200/JCO.2007.13.6374. [DOI] [PubMed] [Google Scholar]
- 41.Cwikla JB, Sankowski A, Seklecka N, et al. Efficacy of radionuclide treatment DOTATATE Y-90 in patients with progressive metastatic gastroenteropancreatic neuroendocrine carcinomas (GEP-NETs): a phase II study. Annals of Oncology. 2009;21(4):787–794. doi: 10.1093/annonc/mdp372. [DOI] [PubMed] [Google Scholar]
- 42.Kwekkeboom DJ, Teunissen JJ, Bakker WH, et al. Radiolabeled somatostatin analog [177Lu-DOTA0, Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. Journal of Clinical Oncology. 2005;23(12):2754–2762. doi: 10.1200/JCO.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 43.Pfeifer AK, Gregersen T, Gronbaek H, Hansen CP, Muller-Brand J, Herskind Bruun K. Peptide receptor radionuclide therapy with Y-DOTATOC and (177)Lu-DOTATOC in advanced neuroendocrine tumors: results from a Danish cohort treated in Switzerland. Neuroendocrinology. 2011;93(3):189–196. doi: 10.1159/000324096. [DOI] [PubMed] [Google Scholar]
- 44.Kwekkeboom DJ, De Herder WW, Kam BL, Van Eijck CH, Van Essen M, Kooij PP. Treatment with the radiolabeled somatostatin analog [177Lu- DOTA0,Tyr3]octreotate: toxicity, efficacy, and survival. Journal of Clinical Oncology. 2008;26(13):2124–2130. doi: 10.1200/JCO.2007.15.2553. [DOI] [PubMed] [Google Scholar]
- 45.Steinmüller T, Kianmanesh R, Falconi M, et al. Consensus guidelines for the management of patients with liver metastases from digestive (neuro)endocrine tumors: foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2007;87(1):47–62. doi: 10.1159/000111037. [DOI] [PubMed] [Google Scholar]
- 46.Que FG, Sarmiento JM, Nagorney DM. Hepatic surgery for metastatic gastrointestinal neuroendocrine tumors. Advances in Experimental Medicine and Biology. 2006;574:43–56. doi: 10.1007/0-387-29512-7_7. [DOI] [PubMed] [Google Scholar]
- 47.Que FG, Sarmiento JM, Nagorney DM. Hepatic surgery for metastatic gastrointestinal neuroendocrine tumors. Cancer Control. 2002;9(1):67–79. doi: 10.1177/107327480200900111. [DOI] [PubMed] [Google Scholar]
- 48.Chamberlain RS, Canes D, Brown KT, et al. Hepatic neuroendocrine metastases: does intervention alter outcomes? Journal of the American College of Surgeons. 2000;190(4):432–445. doi: 10.1016/s1072-7515(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 49.Norton JA, Warren RS, Kelly MG, et al. Aggressive surgery for metastatic liver neuroendocrine tumors. Surgery. 2003;134(6):1057–1065. doi: 10.1016/j.surg.2003.07.025. [DOI] [PubMed] [Google Scholar]
- 50.Frilling A, Li J, Malamutmann E, Schmid KW, Bockisch A, Broelsch CE. Treatment of liver metastases from neuroendocrine tumours in relation to the extent of hepatic disease. British Journal of Surgery. 2009;96(2):175–184. doi: 10.1002/bjs.6468. [DOI] [PubMed] [Google Scholar]
- 51.Sarmiento JM, Que FG. Hepatic surgery for metastases from neuroendocrine tumors. Surgical Oncology Clinics of North America. 2003;12(1):231–242. doi: 10.1016/s1055-3207(02)00076-5. [DOI] [PubMed] [Google Scholar]
- 52.Elias D, Lasser P, Ducreux M, et al. Liver resection (and associated extrahepatic resections) for metastatic well-differentiated endocrine tumors: a 15-year single center prospective study. Surgery. 2003;133(4):375–382. doi: 10.1067/msy.2003.114. [DOI] [PubMed] [Google Scholar]
- 53.Nave H, Mössinger E, Feist H, Lang H, Raab HR. Surgery as primary treatment in patients with liver metastases from carcinoid tumors: a retrospective, unicentric study over 13 years. Surgery. 2001;129(2):170–175. doi: 10.1067/msy.2001.110426. [DOI] [PubMed] [Google Scholar]
- 54.Saxena A, Chua TC, Sarkar A, et al. Progression and survival results after radical hepatic metastasectomy of indolent advanced neuroendocrine neoplasms (NENs) supports an aggressive surgical approach. Surgery. 2011;149(2):209–220. doi: 10.1016/j.surg.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 55.Cho CS, Labow DM, Tang L, et al. Histologic grade is correlated with outcome after resection of hepatic neuroendocrine neoplasms. Cancer. 2008;113(1):126–134. doi: 10.1002/cncr.23523. [DOI] [PubMed] [Google Scholar]
- 56.Que FG, Nagorney DM, Batts KP, Linz LJ, Kvols LK. Hepatic resection for metastatic neuroendocrine carcinomas. American Journal of Surgery. 1995;169(1):36–43. doi: 10.1016/s0002-9610(99)80107-x. [DOI] [PubMed] [Google Scholar]
- 57.Chambers AJ, Pasieka JL, Dixon E, Rorstad O. The palliative benefit of aggressive surgical intervention for both hepatic and mesenteric metastases from neuroendocrine tumors. Surgery. 2008;144(4):645–653. doi: 10.1016/j.surg.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 58.Jensen EH, Kvols L, McLoughlin JM, et al. Biomarkers predict outcomes following cytoreductive surgery for hepatic metastases from functional carcinoid tumors. Annals of Surgical Oncology. 2007;14(2):780–785. doi: 10.1245/s10434-006-9148-z. [DOI] [PubMed] [Google Scholar]
- 59.Srirajaskanthan R, McStay M, Toumpanakis C, Meyer T, Caplin ME. Parathyroid hormone-related peptide-secreting pancreatic neuroendocrine tumours: case series and literature review. Neuroendocrinology. 2009;89(1):48–55. doi: 10.1159/000151222. [DOI] [PubMed] [Google Scholar]
- 60.Gurusamy KS, Ramamoorthy R, Sharma D, Davidson BR. Liver resection versus other treatments for neuroendocrine tumours in patients with resectable liver metastases. Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD007060.pub2. Article ID CD007060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gurusamy KS, Pamecha V, Sharma D, Davidson BR. Palliative cytoreductive surgery versus other palliative treatments in patients with unresectable liver metastases from gastro-entero-pancreatic neuroendocrine tumours. Cochrane Database of Systematic Reviews. 2009;(1) doi: 10.1002/14651858.CD007118.pub2. Article ID CD007118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ahmed A, Turner G, King B, et al. Midgut neuroendocrine tumours with liver metastases: results of the UKINETS study. Endocrine-Related Cancer. 2009;16(3):885–894. doi: 10.1677/ERC-09-0042. [DOI] [PubMed] [Google Scholar]
- 63.Eriksson J, Stålberg P, Nilsson A, et al. Surgery and radiofrequency ablation for treatment of liver metastases from midgut and foregut carcinoids and endocrine pancreatic tumors. World Journal of Surgery. 2008;32(5):930–938. doi: 10.1007/s00268-008-9510-3. [DOI] [PubMed] [Google Scholar]
- 64.Stoeltzing O, Huber E, Loss M, et al. Staged surgery with neoadjuvant 90Y-DOTATOC therapy for down-sizing synchronous bilobular hepatic metastases from a neuroendocrine pancreatic tumor. Langenbeck’s Archives of Surgery. 2010;395(2):185–192. doi: 10.1007/s00423-009-0520-x. [DOI] [PubMed] [Google Scholar]
- 65.Whitney R, Tatum C, Hahl M, et al. Safety of hepatic resection in metastatic disease to the liver after yttrium-90 therapy. Journal of Surgical Research. 2011;166(2):236–240. doi: 10.1016/j.jss.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 66.Eriksson B, Klöppel G, Krenning E, et al. Consensus guidelines for the management of patients with digestive neuroendocrine tumors—well-differentiated jejunal-ileal tumor/carcinoma. Neuroendocrinology. 2007;87(1):8–19. doi: 10.1159/000111034. [DOI] [PubMed] [Google Scholar]
- 67.Clark OH, Benson AB, III, Berlin JD, Choti MA, Doherty GM, Engstrom PF. NCCN Clinical Practice Guidelines in Oncology: neuroendocrine tumors. The Journal of the National Comprehensive Cancer Network. 2009;7(7):712–747. doi: 10.6004/jnccn.2009.0050. [DOI] [PubMed] [Google Scholar]
- 68.Boudreaux JP, Klimstra DS, Hassan MM, et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas. 2010;39(6):753–766. doi: 10.1097/MPA.0b013e3181ebb2a5. [DOI] [PubMed] [Google Scholar]
- 69.Hellman P, Lundström T, Öhrvall U, et al. Effect of surgery on the outcome of midgut carcinoid disease with lymph node and liver metastases. World Journal of Surgery. 2002;26(8):991–997. doi: 10.1007/s00268-002-6630-z. [DOI] [PubMed] [Google Scholar]
- 70.Falconi M, Plöckinger U, Kwekkeboom DJ, et al. Well-differentiated pancreatic nonfunctioning tumors/carcinoma. Neuroendocrinology. 2007;84(3):196–211. doi: 10.1159/000098012. [DOI] [PubMed] [Google Scholar]
- 71.Hill JS, McPhee JT, McDade TP, Zhou Z, Sullivan ME, Whalen GF. Pancreatic neuroendocrine tumors: the impact of surgical resection on survival. Cancer. 2009;115(4):741–751. doi: 10.1002/cncr.24065. [DOI] [PubMed] [Google Scholar]
- 72.Bilimoria KY, Talamonti MS, Tomlinson JS, et al. Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors: analysis of 3851 patients. Annals of Surgery. 2008;247(3):490–500. doi: 10.1097/SLA.0b013e31815b9cae. [DOI] [PubMed] [Google Scholar]
- 73.Kulke MH, Anthony LB, Bushnell DL, et al. NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010;39(6):735–752. doi: 10.1097/MPA.0b013e3181ebb168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gregoire E, Le Treut YP. Liver transplantation for primary or secondary endocrine tumors. Transplant International. 2010;23(7):704–711. doi: 10.1111/j.1432-2277.2010.01110.x. [DOI] [PubMed] [Google Scholar]
- 75.Le Treut YP, Delpero JR, Dousset B, et al. Results of liver transplantation in the treatment of metastatic neuroendocrine tumors: a 31-case French multicentric report. Annals of Surgery. 1997;225(4):355–364. doi: 10.1097/00000658-199704000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Blonski WC, Reddy KR, Shaked A, Siegelman E, Metz DC. Liver transplantation for metastatic neuroendocrine tumor: a case report and review of the literature. World Journal of Gastroenterology. 2005;11(48):7676–7683. doi: 10.3748/wjg.v11.i48.7676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Frilling A, Rogiers X, Knofel WT, Broelsch CE. Liver transplantation for metastatic carcinoid tumors. Digestion. 1994;55(3):104–106. doi: 10.1159/000201210. [DOI] [PubMed] [Google Scholar]
- 78.Routley D, Ramage JK, McPeake J, Tan KC, Williams R. Orthotopic liver transplantation in the treatment of metastatic neuroendocrine tumors of the liver. Liver Transplantation and Surgery. 1995;1(2):118–121. doi: 10.1002/lt.500010209. [DOI] [PubMed] [Google Scholar]
- 79.Lang H, Schlitt HJ, Schmidt H, et al. Total hepatectomy and liver transplantation for metastatic neuroendocrine tumors of the pancreas—a single center experience with ten patients. Langenbeck’s Archives of Surgery. 1999;384(4):370–377. doi: 10.1007/s004230050216. [DOI] [PubMed] [Google Scholar]
- 80.van Vilsteren FGI, Baskin-Bey ES, Nagorney DM, et al. Liver transplantation for gastroenteropancreatic neuroendocrine cancers: defining selection criteria to improve survival. Liver Transplantation. 2006;12(3):448–456. doi: 10.1002/lt.20702. [DOI] [PubMed] [Google Scholar]
- 81.Rosenau J, Bahr MJ, Von Wasielewski R, et al. Ki67, e-cadherin, and p53 as prognostic indicators of long-term outcome after liver transplantation for metastatic neuroendocrine tumors. Transplantation. 2002;73(3):386–394. doi: 10.1097/00007890-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 82.Ahlman H, Friman S, Cahlin C, et al. Liver transplantation for treatment of metastatic neuroendocrine tumors. Annals of the New York Academy of Sciences. 2004;1014:265–269. doi: 10.1196/annals.1294.029. [DOI] [PubMed] [Google Scholar]
- 83.Mazzaferro V, Pulvirenti A, Coppa J. Neuroendocrine tumors metastatic to the liver: how to select patients for liver transplantation? Journal of Hepatology. 2007;47(4):460–466. doi: 10.1016/j.jhep.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 84.Fernández JA, Robles R, Marín C, et al. Role of liver transplantation in the management of metastatic neuroendocrine tumors. Transplantation Proceedings. 2003;35(5):1832–1833. doi: 10.1016/s0041-1345(03)00584-0. [DOI] [PubMed] [Google Scholar]
- 85.Frilling A, Malago M, Weber F, et al. Liver transplantation for patients with metastatic endocrine tumors: single-center experience with 15 patients. Liver Transplantation. 2006;12(7):1089–1096. doi: 10.1002/lt.20755. [DOI] [PubMed] [Google Scholar]
- 86.Martin M, Tarara D, Wu YM, et al. Intrahepatic arterial chemoembolization for hepatocellular carcinoma and metastatic neuroendocrine tumors in the era of liver transplantation. American Surgeon. 1996;62(9):724–731. [PubMed] [Google Scholar]
- 87.Kim YH, Ajani JA, Humberto Carrasco C, et al. Selective hepatic arterial chemoembolization for liver metastases in patients with carcinoid tumor or islet cell carcinoma. Cancer Investigation. 1999;17(7):474–478. doi: 10.3109/07357909909032856. [DOI] [PubMed] [Google Scholar]
- 88.Vogl TJ, Gruber T, Naguib NNN, Hammerstingl R, Nour-Eldin NEA. Liver metastases of neuroendocrine tumors: treatment with hepatic transarterial chemotherapy using two therapeutic protocols. American Journal of Roentgenology. 2009;193(4):941–947. doi: 10.2214/AJR.08.1879. [DOI] [PubMed] [Google Scholar]
- 89.Iwazawa J, Ohue S, Yasumasa K, Mitani T. Transarterial chemoembolization with miriplatin-lipiodol emulsion for neuroendocrine metastases of the liver. World Journal of Radiology. 2010;2(12):468–471. doi: 10.4329/wjr.v2.i12.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Eriksson BK, Larsson EG. Liver embolizations of patients with malignant neuroendocrine gastrointestinal tumors. Cancer. 1998;83(11):2293–2301. [PubMed] [Google Scholar]
- 91.Roche A, Girish BV, De Baere T, et al. Prognostic factors for chemoembolization in liver metastasis from endocrine tumors. Hepato-Gastroenterology. 2004;51(60):1751–1756. [PubMed] [Google Scholar]
- 92.Nazario J, Gupta S. Transarterial liver-directed therapies of neuroendocrine hepatic metastases. Seminars in Oncology. 2010;37(2):118–126. doi: 10.1053/j.seminoncol.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 93.Carrasco CH, Chuang VP, Wallace S. Apudomas metastatic to the liver: treatment by hepatic artery embolization. Radiology. 1983;149(1):79–83. doi: 10.1148/radiology.149.1.6611956. [DOI] [PubMed] [Google Scholar]
- 94.Drougas JG, Anthony LB, Blair TK, Lopez RR, Wright JK, Chapman WC. Hepatic artery chemoembolization for management of patients with advanced metastatic carcinoid tumors. American Journal of Surgery. 1998;175(5):408–412. doi: 10.1016/s0002-9610(98)00042-7. [DOI] [PubMed] [Google Scholar]
- 95.Hajarizadeh H, Ivancev K, Mueller CR, Fletcher WS, Woltering EA. Effective palliative treatment of metastatic carcinoid tumors with intra-arterial chemotherapy/chemoembolization combined with octreotide acetate. American Journal of Surgery. 1992;163(5):479–483. doi: 10.1016/0002-9610(92)90392-5. [DOI] [PubMed] [Google Scholar]
- 96.Ajani JA, Carrasco CH, Charnsangavej C, Samaan NA, Levin B, Wallace S. Islet cell tumors metastatic to the liver: effective palliation by sequential hepatic artery embolization. Annals of Internal Medicine. 1988;108(3):340–344. doi: 10.7326/0003-4819-108-3-340. [DOI] [PubMed] [Google Scholar]
- 97.Swärd C, Johanson V, Nieveen Van Dijkum E, et al. Prolonged survival after hepatic artery embolization in patients with midgut carcinoid syndrome. British Journal of Surgery. 2009;96(5):517–521. doi: 10.1002/bjs.6587. [DOI] [PubMed] [Google Scholar]
- 98.Christante D, Pommier S, Givi B, Pommier R. Hepatic artery chemoinfusion with chemoembolization for neuroendocrine cancer with progressive hepatic metastases despite octreotide therapy. Surgery. 2008;144(6):885–894. doi: 10.1016/j.surg.2008.08.037. [DOI] [PubMed] [Google Scholar]
- 99.Loewe C, Schindl M, Cejna M, Niederle B, Lammer J, Thurnher S. Permanent transarterial embolization of neuroendocrine metastases of the liver using cyanoacrylate and lipiodol: assessment of mid- and long-term results. American Journal of Roentgenology. 2003;180(5):1379–1384. doi: 10.2214/ajr.180.5.1801379. [DOI] [PubMed] [Google Scholar]
- 100.Roche A, Girish BV, de Baère T, et al. Trans-catheter arterial chemoembolization as first-line treatment for hepatic metastases from endocrine tumors. European Radiology. 2003;13(1):136–140. doi: 10.1007/s00330-002-1558-0. [DOI] [PubMed] [Google Scholar]
- 101.Ruszniewski P. ENETS; Lisbon, Portugal, 2011.
- 102.Vogl TJ, Naguib NNN, Zangos S, Eichler K, Hedayati A, Nour-Eldin NEA. Liver metastases of neuroendocrine carcinomas: interventional treatment via transarterial embolization, chemoembolization and thermal ablation. European Journal of Radiology. 2009;72(3):517–528. doi: 10.1016/j.ejrad.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 103.Berber E, Siperstein A. Local recurrence after laparoscopic radiofrequency ablation of liver tumors: an analysis of 1032 tumors. Annals of Surgical Oncology. 2008;15(10):2757–2764. doi: 10.1245/s10434-008-0043-7. [DOI] [PubMed] [Google Scholar]
- 104.Siperstein AE, Rogers SJ, Hansen PD, Gitomirsky A. Laparoscopic thermal ablation of hepatic neuroendocrine tumor metastases. Surgery. 1997;122(6):1147–1155. doi: 10.1016/s0039-6060(97)90221-x. [DOI] [PubMed] [Google Scholar]
- 105.Siperstein AE, Berber E. Cryoablation, percutaneous alcohol injection, and radiofrequency ablation for treatment of neuroendocrine liver metastases. World Journal of Surgery. 2001;25(6):693–696. doi: 10.1007/s00268-001-0015-6. [DOI] [PubMed] [Google Scholar]
- 106.Siperstein A, Garland A, Engle K, et al. Laparoscopic radiofrequency ablation of primary and metastatic liver tumors: technical considerations. Surgical Endoscopy. 2000;14(4):400–405. doi: 10.1007/s004640000067. [DOI] [PubMed] [Google Scholar]
- 107.Wessels FJ, Schell SR. Radiofrequency ablation treatment of refractory carcinoid hepatic metastases. Journal of Surgical Research. 2001;95(1):8–12. doi: 10.1006/jsre.2000.5988. [DOI] [PubMed] [Google Scholar]
- 108.Tait IS, Yong SM, Cuschieri SA. Laparoscopic in situ ablation of liver cancer with cryotherapy and radiofrequency ablation. British Journal of Surgery. 2002;89(12):1613–1619. doi: 10.1046/j.1365-2168.2002.02264.x. [DOI] [PubMed] [Google Scholar]
- 109.Siperstein A, Garland A, Engle K, et al. Local recurrence after laparoscopic radiofrequency thermal ablation of hepatic tumors. Annals of Surgical Oncology. 2000;7(2):106–113. doi: 10.1007/s10434-000-0106-x. [DOI] [PubMed] [Google Scholar]
- 110.Murthy R, Kamat P, Nunez R, et al. Yttrium-90 microsphere radioembolotherapy of hepatic metastatic neuroendocrine carcinomas after hepatic arterial embolization. Journal of Vascular and Interventional Radiology. 2008;19(1):145–151. doi: 10.1016/j.jvir.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 111.Jacobsen MB, Hanssen LE. Clinical effects of octreotide compared to placebo in patients with gastrointestinal neuroendocrine tumours. Report on a double-blind, randomized trial. Journal of Internal Medicine. 1995;237(3):269–275. doi: 10.1111/j.1365-2796.1995.tb01175.x. [DOI] [PubMed] [Google Scholar]
- 112.Öberg K. Chemotherapy and biotherapy in the treatment of neuroendocrine tumours. Annals of Oncology. 2001;12(2, supplement):S111–S114. doi: 10.1093/annonc/12.suppl_2.s111. [DOI] [PubMed] [Google Scholar]
- 113.Imam H, Eriksson B, Lukinius A, et al. Induction of apoptosis in neuroendocrine tumors of the digestive system during treatment with somatostatin analogs. Acta Oncologica. 1997;36(6):607–614. doi: 10.3109/02841869709001323. [DOI] [PubMed] [Google Scholar]
- 114.Fazio N, de Braud F, Delle Fave G, Öberg K. Interferon-α and somatostatin analog in patients with gastroenteropancreatic neuroendocrine carcinoma: single agent or combination? Annals of Oncology. 2007;18(1):13–19. doi: 10.1093/annonc/mdl144. [DOI] [PubMed] [Google Scholar]
- 115.Faiss S, Pape U-F, Böhmig M, et al. Prospective, randomized, multicenter trial on the antiproliferative effect of lanreotide, interferon alfa, and their combination for therapy of metastatic neuroendocrine gastroenteropancreatic tumors—the International Lanreotide and Interferon Alfa Study Group. Journal of Clinical Oncology. 2003;21(14):2689–2696. doi: 10.1200/JCO.2003.12.142. [DOI] [PubMed] [Google Scholar]
- 116.Bajetta E, Catena L, Procopio G, et al. Are capecitabine and oxaliplatin (XELOX) suitable treatments for progressing low-grade and high-grade neuroendocrine tumours? Cancer Chemotherapy and Pharmacology. 2007;59(5):637–642. doi: 10.1007/s00280-006-0306-6. [DOI] [PubMed] [Google Scholar]
- 117.Vilar E, Salazar R, Pérez-García J, Cortes J, Öberg K, Tabernero J. Chemotherapy and role of the proliferation marker Ki-67 in digestive neuroendocrine tumors. Endocrine-Related Cancer. 2007;14(2):221–232. doi: 10.1677/ERC-06-0074. [DOI] [PubMed] [Google Scholar]
- 118.Toumpanakis C, Meyer T, Caplin ME. Cytotoxic treatment including embolization/chemoembolization for neuroendocrine tumours. Best Practice and Research. 2007;21(1):131–144. doi: 10.1016/j.beem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 119.Hainsworth JD, Spigel DR, Litchy S, Anthony Greco F. Phase II trial of paclitaxel, carboplatin, and etoposide in advanced poorly differentiated neuroendocrine carcinoma: a minnie pearl cancer research network study. Journal of Clinical Oncology. 2006;24(22):3548–3554. doi: 10.1200/JCO.2005.05.0575. [DOI] [PubMed] [Google Scholar]
- 120.Fjällskog M-LH, Granberg DPK, Welin SLV, et al. Treatment with cisplatin and etoposide in patients with neuroendocrine tumors. Cancer. 2001;92(5):1101–1107. doi: 10.1002/1097-0142(20010901)92:5<1101::aid-cncr1426>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 121.Kulke MH, Kim H, Clark JW, et al. A phase II trial of gemcitabine for metastatic neuroendocrine tumors. Cancer. 2004;101(5):934–939. doi: 10.1002/cncr.20466. [DOI] [PubMed] [Google Scholar]
- 122.Kulke MH, Wu B, Ryan DP, et al. A phase II trial of irinotecan and cisplatin in patients with metastatic neuroendocrine tumors. Digestive Diseases and Sciences. 2006;51(6):1033–1038. doi: 10.1007/s10620-006-8001-3. [DOI] [PubMed] [Google Scholar]
- 123.Kulke MH, Stuart K, Enzinger PC, et al. Phase II study of temozolomide and thalidomide in patients with metastatic neuroendocrine tumors. Journal of Clinical Oncology. 2006;24(3):401–406. doi: 10.1200/JCO.2005.03.6046. [DOI] [PubMed] [Google Scholar]
- 124.Rivera E, Ajani JA. Doxorubicin, streptozocin, and 5-fluorouracil chemotherapy for patients with metastatic islet-cell carcinoma. American Journal of Clinical Oncology. 1998;21(1):36–38. doi: 10.1097/00000421-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 125.Arnold R, Rinke A, Schmidt C, Hofbauer L. Endocrine tumours of the gastrointestinal tract: chemotherapy. Best Practice & Research Clinical Gastroenterology. 2005;19(4):649–656. doi: 10.1016/j.bpg.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 126.Kaltsas G, Mukherjee JJ, Plowman PN, Grossman AB. The role of chemotherapy in the nonsurgical management of malignant neuroendocrine tumours. Clinical Endocrinology. 2001;55(5):575–587. doi: 10.1046/j.1365-2265.2001.01396.x. [DOI] [PubMed] [Google Scholar]
- 127.Davies AHG, Larsson G, Ardill J, Friend E, Jones L, Falconi M. Development of a disease-specific quality of life questionnaire module for patients with gastrointestinal neuroendocrine tumours. European Journal of Cancer. 2006;42(4):477–484. doi: 10.1016/j.ejca.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 128.Hatton MQ, Reed NS. Chemotherapy for neuroendocrine tumors: the Beatson Oncology Centre experience. Clinical Oncology. 1997;9(6):385–389. doi: 10.1016/s0936-6555(97)80132-x. [DOI] [PubMed] [Google Scholar]
- 129.Bukowski RM, Tangen CM, Peterson RF, et al. Phase II trial of dimethyltriazenoimidazole carboxamide in patients with metastatic carcinoid. A Southwest Oncology Group study. Cancer. 1994;73(5):1505–1508. doi: 10.1002/1097-0142(19940301)73:5<1505::aid-cncr2820730530>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 130.Ansell SM, Pitot HC, Burch PA, Kvols LK, Mahoney MR, Rubin J. A phase II study of high-dose paclitaxel in patients with advanced neuroendocrine tumors. Cancer. 2001;91(8):1543–1548. doi: 10.1002/1097-0142(20010415)91:8<1543::aid-cncr1163>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 131.Ansell SM, Mahoney MR, Green EM, Rubin J. Topotecan in patients with advanced neuroendocrine tumors: a phase II study with significant hematologic toxicity. American Journal of Clinical Oncology. 2004;27(3):232–235. doi: 10.1097/01.coc.0000054535.19808.f4. [DOI] [PubMed] [Google Scholar]
- 132.Kulke MH, Kim H, Stuart K, et al. A phase II study of docetaxel in patients with metastatic carcinoid tumors. Cancer Investigation. 2004;22(3):353–359. doi: 10.1081/cnv-200029058. [DOI] [PubMed] [Google Scholar]
- 133.Moertel CG, Hanley JA, Johnson LA. Streptozocin alone compared with streptozocin plus fluorouracil in the treatment of advanced islet-cell carcinoma. New England Journal of Medicine. 1980;303(21):1189–1194. doi: 10.1056/NEJM198011203032101. [DOI] [PubMed] [Google Scholar]
- 134.Ramanathan RK, Cnaan A, Hahn RG, Carbone PP, Haller DG. Phase II trial dacarbazine (DTIC) in advanced pancreatic islet cell carcinoma. Study of the Eastern Cooperative Oncology Group-E6282. Annals of Oncology. 2001;12(8):1139–1143. doi: 10.1023/a:1011632713360. [DOI] [PubMed] [Google Scholar]
- 135.Ekeblad S, Sundin A, Janson ET, et al. Temozolomide as monotherapy is effective in treatment of advanced malignant neuroendocrine tumors. Clinical Cancer Research. 2007;13(10):2986–2991. doi: 10.1158/1078-0432.CCR-06-2053. [DOI] [PubMed] [Google Scholar]
- 136.Gonzalez MA, Biswas S, Clifton L, Corrie PG. Treatment of neuroendocrine tumours with infusional 5-fluorouracil, folinic acid and streptozocin. British Journal of Cancer. 2003;89(3):455–456. doi: 10.1038/sj.bjc.6601167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Engstrom PF, Lavin PT, Moertel CG. Streptozocin plus fluorouracil versus doxorubicin therapy for metastatic carcinoid tumorr. Journal of Clinical Oncology. 1984;2(11):1255–1259. doi: 10.1200/JCO.1984.2.11.1255. [DOI] [PubMed] [Google Scholar]
- 138.Delaunoit T, Ducreux M, Boige V, et al. The doxorubicin-streptozotocin combination for the treatment of advanced well-differentiated pancreatic endocrine carcinoma: a judicious option? European Journal of Cancer. 2004;40(4):515–520. doi: 10.1016/j.ejca.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 139.Lopes GDL, Jr., Chiappori A, Simon G, et al. Phase I study of carboplatin in combination with gemcitabine and irinotecan in patients with solid tumors: preliminary evidence of activity in small cell and neuroendocrine carcinomas. Cancer. 2007;109(7):1413–1419. doi: 10.1002/cncr.22522. [DOI] [PubMed] [Google Scholar]
- 140.Ghosn M, Farhat F, Kattan J, et al. FOLFOX-6 combination as the first-line treatment of locally advanced and/or metastatic pancreatic cancer. American Journal of Clinical Oncology. 2007;30(1):15–20. doi: 10.1097/01.coc.0000235997.18657.a6. [DOI] [PubMed] [Google Scholar]
- 141.Gilbert JA, Adhikari LJ, Lloyd RV, et al. Molecular markers for novel therapies in neuroendocrine (carcinoid) tumors. Endocrine-Related Cancer. 2010;17(3):623–636. doi: 10.1677/ERC-09-0318. [DOI] [PubMed] [Google Scholar]
- 142.Yao JC. Molecular targeted therapy for carcinoid and islet-cell carcinoma. Best Practice and Research. 2007;21(1):163–172. doi: 10.1016/j.beem.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 143.Kulke MH, Lenz HJ, Meropol NJ, et al. Activity of sunitinib in patients with advanced neuroendocrine tumors. Journal of Clinical Oncology. 2008;26(20):3403–3410. doi: 10.1200/JCO.2007.15.9020. [DOI] [PubMed] [Google Scholar]
- 144.Zitzmann K, De Toni EN, Brand S, et al. The novel mTOR inhibitor RAD001 (everolimus) induces antiproliferative effects in human pancreatic neuroendocrine tumor cells. Neuroendocrinology. 2007;85(1):54–60. doi: 10.1159/000100057. [DOI] [PubMed] [Google Scholar]
- 145.Yao JC, Lombard-Bohas C, Baudin E, et al. Daily oral everolimus activity in patients with metastatic pancreatic neuroendocrine tumors after failure of cytotoxic chemotherapy: a phase II trial. Journal of Clinical Oncology. 2010;28(1):69–76. doi: 10.1200/JCO.2009.24.2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Christofori G, Naik P, Hanahan D. Vascular endothelial growth factor and its receptors, flt-1 and flk-1, are expressed in normal pancreatic islets and throughout islet cell tumorigenesis. Molecular Endocrinology. 1995;9(12):1760–1770. doi: 10.1210/mend.9.12.8614412. [DOI] [PubMed] [Google Scholar]
- 147.Terris B, Scoazec JY, Rubbia L, et al. Expression of vascular endothelial growth factor in digestive neuroendocrine tumours. Histopathology. 1998;32(2):133–138. doi: 10.1046/j.1365-2559.1998.00321.x. [DOI] [PubMed] [Google Scholar]
- 148.Lindholm DP, Eriksson B, Granberg D. Response to temozolomide and bevacizumab in a patient with poorly differentiated neuroendocrine carcinoma. Medical Oncology. 2012;29(1):301–303. doi: 10.1007/s12032-010-9789-4. [DOI] [PubMed] [Google Scholar]
- 149.Takeuchi S, Honma R, Taguchi J, et al. A case of high-grade neuroendocrine carcinoma that improved with bevacizumab plus modified FOLFOX6 as the fourth-line chemotherapy. Case Reports in Oncology. 2011;4(2):260–266. doi: 10.1159/000328802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Virgolini I, Ambrosini V, Bomanji JB, et al. Procedure guidelines for PET/CT tumour imaging with 68Ga-DOTA-conjugated peptides: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE. European Journal of Nuclear Medicine and Molecular Imaging. 2010;37(10):2004–2010. doi: 10.1007/s00259-010-1512-3. [DOI] [PubMed] [Google Scholar]
- 151.Kwekkeboom DJ, Krenning EP, Lebtahi R, Komminoth P, Kos-Kudła B, De Herder WW. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: peptide receptor radionuclide therapy with radiolabeled somatostatin analogs. Neuroendocrinology. 2009;90(2):220–226. doi: 10.1159/000225951. [DOI] [PubMed] [Google Scholar]
- 152.Kwekkeboom DJ, Mueller-Brand J, Paganelli G, et al. Overview of results of peptide receptor radionuclide therapy with 3 radiolabeled somatostatin analogs. Journal of Nuclear Medicine. 2005;46(1, supplement):62S–66S. [PubMed] [Google Scholar]
- 153.Van Essen M, Krenning EP, Kam BLR, De Jong M, Valkema R, Kwekkeboom DJ. Peptide-receptor radionuclide therapy for endocrine tumors. Nature Reviews Endocrinology. 2009;5(7):382–393. doi: 10.1038/nrendo.2009.105. [DOI] [PubMed] [Google Scholar]
- 154.Van Essen M, Krenning EP, De Jong M, Valkema R, Kwekkeboom DJ. Peptide receptor radionuclide therapy with radiolabelled somatostatin analogues in patients with somatostatin receptor positive tumours. Acta Oncologica. 2007;46(6):723–734. doi: 10.1080/02841860701441848. [DOI] [PubMed] [Google Scholar]
- 155.Forrer F, Valkema R, Kwekkeboom DJ, de Jong M, Krenning E P. Neuroendocrine tumors. Peptide receptor radionuclide therapy. Best Practice & Research. 2007;21(1):111–129. doi: 10.1016/j.beem.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 156.Kwekkeboom DJ, de Herder WW, van Eijck CHJ, et al. Peptide receptor radionuclide therapy in patients with gastroenteropancreatic neuroendocrine tumors. Seminars in Nuclear Medicine. 2010;40(2):78–88. doi: 10.1053/j.semnuclmed.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 157.Bodei L, Pepe G, Paganelli G. Peptide receptor radionuclide therapy (PRRT) of neuroendocrine tumors with somatostatin analogues. European Review for Medical and Pharmacological Sciences. 2010;14(4):347–351. [PubMed] [Google Scholar]
- 158.Bushnell DL, Jr., O’Dorisio TM, O’Dorisio MS, et al. 90Y-edotreotide for metastatic carcinoid refractory to octreotide. Journal of Clinical Oncology. 2010;28(10):1652–1659. doi: 10.1200/JCO.2009.22.8585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Valkema R, Pauwels SA, Kvols LK, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with 90Y-DOTA0,Tyr3-octreotide and 177Lu-DOTA0,Tyr3-octreotate. Journal of Nuclear Medicine. 2005;46(1):83S–91S. [PubMed] [Google Scholar]
- 160.Claringbold PG, Brayshaw PA, Price RA, Turner JH. Phase II study of radiopeptide 177Lu-octreotate and capecitabine therapy of progressive disseminated neuroendocrine tumours. European Journal of Nuclear Medicine and Molecular Imaging. 2011;38(2):302–311. doi: 10.1007/s00259-010-1631-x. [DOI] [PubMed] [Google Scholar]
- 161.Nayak TK, Atcher RW, Prossnitz ER, Norenberg JP. Enhancement of somatostatin-receptor-targeted 177Lu-[DOTA0-Tyr3]-octreotide therapy by gemcitabine pretreatment-mediated receptor uptake, up-regulation and cell cycle modulation. Nuclear Medicine and Biology. 2008;35(6):673–678. doi: 10.1016/j.nucmedbio.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Miederer M, Henriksen G, Alke A, et al. Preclinical evaluation of the α-particle generator nuclide 225Ac for somatostatin receptor radiotherapy of neuroendocrine tumors. Clinical Cancer Research. 2008;14(11):3555–3561. doi: 10.1158/1078-0432.CCR-07-4647. [DOI] [PubMed] [Google Scholar]
- 163.Mukherjee JJ, Kaltsas GA, Islam N, et al. Treatment of metastatic carcinoid tumours, phaeochromocytoma, paraganglioma and medullary carcinoma of the thyroid with 131i-meta-iodobenzylguanidine (131I-mIBG) Clinical Endocrinology. 2001;55(1):47–60. doi: 10.1046/j.1365-2265.2001.01309.x. [DOI] [PubMed] [Google Scholar]
- 164.Kaltsas G, Korbonits M, Heintz E, et al. Comparison of somatostatin analog and meta-iodobenzylguanidine radionuclides in the diagnosis and localization of advanced neuroendocrine tumors. Journal of Clinical Endocrinology and Metabolism. 2001;86(2):895–902. doi: 10.1210/jcem.86.2.7194. [DOI] [PubMed] [Google Scholar]
- 165.Safford SD, Coleman RE, Gockerman JP, et al. Iodine-131 metaiodobenzylguanidine treatment for metastic carcinoid: results in 98 patients. Cancer. 2004;101(9):1987–1993. doi: 10.1002/cncr.20592. [DOI] [PubMed] [Google Scholar]


