Abstract
Background:
To benefit from therapy and to avoid contracting treatment resistant strains, the individuals must adhere to medications.
Aim:
The study was designed to assess the degree of drug adherence and its determinants in patients living with HIV/AIDS and TB comorbidity.
Materials and Methods:
A cross-sectional study was conducted to assess the degree of drug adherence and its determinants with the help of self-administered questionnaires in Tercha District Hospital in South Ethiopia.
Result:
A total of 24 patients were included in the study. The majority were females (54.2%) and the mean age was 32.4 (SD±9.6) years. Adherence level was 95.8% for Antiretroviral (ARV) medications and 79.2% for anti TB medications. Educational status was associated with anti TB (P=0.021) medication adherence. The reason for the missed doses were mostly lack of money for transport (23.7% for antiretroviral therapy (ART), 26.0% for TB treatment) and forgetting to take medications (18.4% for ART, 17.4% for TB treatment.
Conclusion:
The adherence level obtained for both ARV and anti-TB where high. Transportation costs for patients could be reduced by bringing the services close to where they live.
Keywords: Comorbidity, Ethiopia, Health literacy, Medications adherence
Introduction
Human immunodeficiency virus (HIV) has spread all around the globe showing no sign of to be less strong.[1] Tuberculosis (TB), the commonest and often the first opportunistic infection to occur among HIV-infected persons, is associated with high mortality and morbidity.[1,2] Tuberculosis is the leading cause of morbidity and mortality and HIV is fuelling the TB epidemic in Ethiopia. The WHO global report 2008 estimates that in Ethiopia 40% of TB patients tested for HIV are HIV positive, while routine data from (2006/7) estimates that 31% of TB patients are HIV positive.[3]
Adherence is crucial for the success of both TB ad Antiretroviral (ARV) treatment patients. Patients with poor adherence are at very high risk for developing drug resistance. Directed observed therapy (DOTS) are recommended to reinforce adherence to TB treatment.[4] For antiretroviral therapy (ART), more than 95% adherence is required to achieve optimal HIV suppression and treatment outcome[5] and patients with TB are expected to have adherence level greater than 90% in order to facilitate cure.[6] Factors that influence adherence can be categorized into patient factors, treatment regimen, disease characteristics, patient provider relationship, and types of clinical settings. To benefit from therapy and to avoid contracting treatment resistant strains, the individuals must adhere rigorously to an often complex and side-effect prone therapeutic regimen.[7]
To reduce the consequences of poor adherence, monitoring and evaluation of the practice is very important. Thus, the objective of the study was to assess the degree of drug adherence and its determinants in patients living with HIV/ Acquired immune deficiency syndrome (AIDs) and TB co morbidity in Tercha district hospital in South Ethiopia.
Materials and Methods
The study was approved by the Ethics Committee of Jimma University. Interviewer explained the purpose of the study and assured confidentiality to each respondents and participation was totally voluntary.
Study design
A cross-sectional study was conducted from January 18 to February 30, 2010 in Tercha District Hospital, which is found in Dawuro Zone in South West of Ethiopia. All patients with HIV and TB comorbidity who came for refill at the time of data collection were included in this study.
Data collection
A structured questionnaire for the study of ART and anti TB medication adherence and its determinants was designed and the validity of the questionnaires was assessed through in-depth discussion with experienced professors working in College of Public Health and Medical Science of Jimma University. The questionnaire was pre tested on eight patients on TB and ART concomitant treatment attending Jimma University Specialized Hospital and necessary correction was made accordingly. The questionnaire used was divided in to five parts: The first part was uses to record the overall patients sociodemographic characteristics and clinical information. The second part was the Medication adherence tool containing questions like frequency of times the patient missed a dose per month, reason of missing doses, how to compensate for the missed doses, what to do it you finished medications before refilling. The third one was the patient and health provider (physician, pharmacist, nurse) relationship questionnaire. The fourth sets of questions were treatment regimen questionnaire (number of pills for HIV/AIDS and TB per day and frequency of taking ARV and anti-TB medications per day. The final part was used to asses health literacy of the patients which included questions such as whether the patient know missing doses of ARV and anti-TB will result in treatment failure or development of drug resistant, possible ways of transmission of HIV/TB and measure taken to prevent possible transmission of TB to the family members.
The questionnaire was developed in English, then translated into local languages (dawregna) and back translated into English to check for accuracy. Interviewers were fluent in both local languages and English. The questionnaires were checked by supervisors at the end of each day during the survey, for omission of incomplete answers and for coding the responses.
Data analysis
Data were cleared and checked every day for completeness and consistency before data processing and analysis. The data were then edited and were entered in Epi Info Version 6.0 (WHO) and analysis was conducted using statistical package for Social Sciences (SPSS) version 16.0. Descriptive statistics such as mean, frequencies and percentages were used to describe and summarize the data.
Results
Sciodemographic characteristics
There were 296 patients on ARV. From these patients, 24 (8.1%) were co-infected by HIV and TB and follow both ARV and anti TB treatment. The majority were (54.2%) females. The mean age of the participants was 32.4 (SD±9.6 years). About 41.7% were married. All married pairs were infected with HIV and TB. Regarding the educational status of the patients, 45.2 of them attended secondary school and above and majority of the participants were government employee (37.5%)
Medication adherence pattern
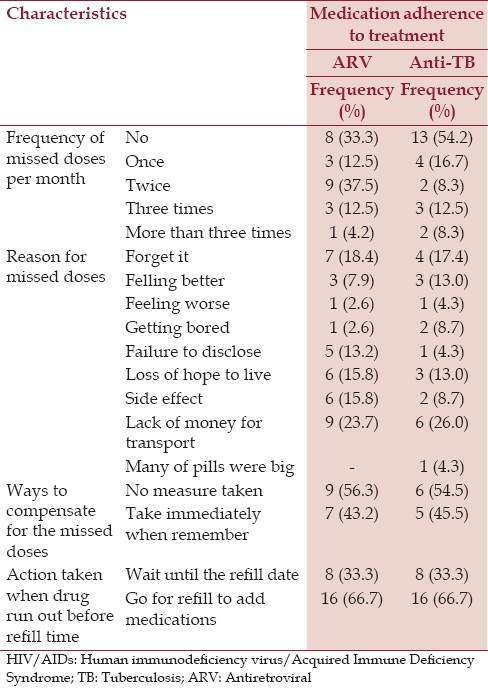
When asked about frequency of times the patient missed a dose per month; 33.3% of the participants did not miss a dose of ARV and the rest missed their doses. In the case of anti TB medications, 54.2% did not miss medications while the rest missed their doses for at least one day. Majority of the participants (23.7% for ART, 26.0% for TB treatment) said lack of money for transport and forgetting to take medications (18.4% for ART, 17.4% for TB treatment) were the reason for the missed doses.
Regarding ways to compensate for missed doses, (56.25 for ART, 54.5% for TB treatment) of the participants do not take any measure, (43.2% for ART, 45.5% for TB treatment) take the dose immediately when they remember and 66.7% of the participants went to the hospital to add more drugs before the refill date where as 33.3% patients wait until the refill date when the drugs run out before the refill time [Table 1].
Table 1.
Medication adherences of patients with HIV/AIDS and TB comorbidity treated at Tercha district Hospital
Patient–health care provider relationship
Table 2 shows patient provider relationships of patients with HIV/AIDS and TB comorbidity. About 41.6%, 45.83%, and 12.5% of the participants have good, very good and excellent relation with their physician respectively. All of them got adequate drug information's from the pharmacist.
Table 2.
Patient-provider relationships, treatment regimen and health literacy of patients with HIV/AIDS and TB comorbidity treated at Tercha district Hospital
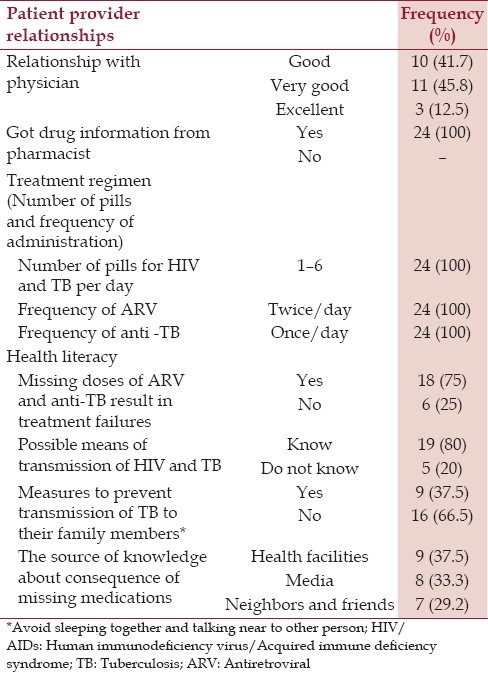
Treatment regimen of ARV and anti-TB
The number of pills of ARV and anti TB was in range 1–6 for all participants. The frequency of ARV is twice/day where as anti TB is once/day.
Health literacy
About 75% of the participants have knowledge about the fact that missing doses of ARV and anti-TB result in treatment failures, 80% have knowledge about possible means of transmission of HIV and TB and only 37.5% of them took measures to prevent transmission of TB to their family members. The main measures they take to prevent TB transmission were to avoid sleeping together and talking near to other person [Table 2].
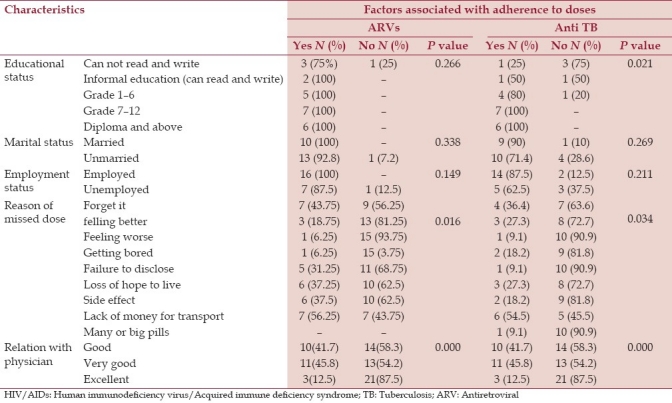
Factors associated with adherence to doses of ARVs and anti TB
Table 3 shows, factors associated with adherence to doses of ARV and anti TB of patient. None of socio-demographic factors were significantly associated with adherence of ARV but educational status was the only sociodemographic factors associated with anti TB (P = 0.021).
Table 3.
Factors associated with adherence to doses of ARV and anti-TB among patient with HIV/AIDs and TB comorbidity treated at Tercha district hospital
Discussion
The HIV epidemic has greatly altered the epidemiological course of tuberculosis. HIV and TB are associated with a higher mortality, although most deaths in those who receive an effective therapy are due to complications of HIV infection rather than tuberculosis.[8,9] In the current study, from 296 patients on ARV at hospital treatment center, 8.1% were confected by HIV and TB and follow both ARV and anti-TB treatment. About 95.8% of the study population had optimal adherence to ARV medications in this study. Other studies reported adherence level from 58.8% to 93.5%.[10–12]
In the case of anti-TB medications, adherence of 79.2% was observed unlike study in Mibarara Hospital in Uganda where the prevalence of non adherence was 25%.[13] The possible explanations for the greater adherence in our study might be that the patients were taking medication with a twice-daily dosing schedule for ARV where once per day for TB which relatively necessitate higher adherence and might be given strict counseling sessions in this study.
Age, sex, employment status, and marital status have insignificant role on adherence in this study. It might be due to the fact that younger took medication appropriately since they do not want to look ill in front of their families and friends and in the same way older took medication correctly since they know the value of life more than other age group, for their better survival. Employment status is not associated with adherence. This is may be due to availability of drugs with out charge in Ethiopia. While educational status had appositive impact on adherence. Possible explanations for such findings include, as the level of education increases, the understandings about the importance of adherence to treatment increases.
Resource-limited settings present unique challenges to ART adherence.[14] Mukherjee et al.,[14] showed that a multitude of structural barriers prevent access to health care and the regular supply of antiretroviral drugs. These include the cost of medical care, drugs, and the difficulty of making follow-up appointments due to long distances, family responsibilities, and the prohibitive cost of transportation. This finding is consistent with our study, in that cost of transportation becomes a huge burden to the. This manipulates several other studies.[15,16]
Okuno et al., showed[17] that poor provider-patient relationships have an impact on adherence. This study showed that patient health care provider relationship is significantly associated with adherence (P=0.000) unlike other study.[18] Creating a good environment might help the patients to tell what they felt at that time and about their medication course to care providers, but if health professionals do not show good relation ship, the patients might think that their condition is getting worsen and feel as if they are hopeless.
Conclusion
The adherence level obtained in this study was relatively high for both ARV and anti-TB treatment. Transport costs for patients could be reduced by brining the services closer to where they live or by providing transport to those who live far.
Acknowledgment and Funding
This study was financed by Students Research Project (SRP) of Jimma University. The authors are grateful to patients who participated in the study.
Footnotes
Source of Support: This study was financed by Students Research Project (SRP) of Jimma University.
Conflict of Interest: None declared.
References
- 1.Corbett E, Watt C, Waler N, Maher D, Williams B, Raviglione M, et al. The growing burden of TB: Global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163:1009–21. doi: 10.1001/archinte.163.9.1009. [DOI] [PubMed] [Google Scholar]
- 2.Soumya S, Gopalan N, Perumal V, Sheik I, Rameshkumar S, Pradeep A, et al. Efficacy of a 6-month versus 9-month intermittent treatment regimen in HIV-infected patients with tuberculosis: A randomized clinical trial. Am J Respir Crit Care Med. 2010;181:743–51. doi: 10.1164/rccm.200903-0439OC. [DOI] [PubMed] [Google Scholar]
- 3.TB leprosy and TB/HIV prevention and control programmer. 4th ed. 2008. Federal Ministry of Health Ethiopia; pp. 34–49. [Google Scholar]
- 4.Bartlett JA. Addressing the challenges of adherence. J Acquir Immune Defic Syndr. 2002;29(Suppl 1):S2–10. doi: 10.1097/00126334-200202011-00002. [DOI] [PubMed] [Google Scholar]
- 5.Lange JM, Perriens J, Kuritzkes D, Zewdie D. What policymakers should know about drug resistance and adherence in the context of scaling-up treatment of HIV infection. AIDS. 2004;18(Suppl 3):S69–74. doi: 10.1097/00002030-200406003-00013. [DOI] [PubMed] [Google Scholar]
- 6.Adherence to antiretroviral therapy in adults: A guide for trainers. Kenya: Horizons/Population Council; 2004. Mombasa ART project; pp. 281–9. [Google Scholar]
- 7.Ickvics J, Meads C. Adherence to HAART among patients with HIV: Break through and barriers. AIDS Care. 2002;14:309–18. doi: 10.1080/09540120220123685. [DOI] [PubMed] [Google Scholar]
- 8.Rocha M, Pereira S, Ferreira L, Barros H. The role of adherence in tuberculosis HIV-positive patients treated in ambulatory regimen. Eur Respir J. 2003;21:785–8. doi: 10.1183/09031936.03.00077302. [DOI] [PubMed] [Google Scholar]
- 9.Gothi D, Joshi JM. Clinical and laboratory observations of TB at a Mumbai (India) clinic. Postgrad Med J. 2004;80:97–100. doi: 10.1136/pmj.2003.008185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beyene KA, Gedif T, Gebre-Mariam T, Engidawork E. Highly active antiretroviral therapy adherence and its determinants in selected hospitals from south and central Ethiopia. Pharmacoepidemiol Drug Saf. 2009;18:1007–15. doi: 10.1002/pds.1814. [DOI] [PubMed] [Google Scholar]
- 11.Cauldbeck MB, O’Connor C, O’Connor MB, Saunders JA, Rao B, Mallesh VG, et al. Adherence to anti-retroviral therapy among HIV patients in Bangalore, India. AIDS Res Ther. 2009;6:7. doi: 10.1186/1742-6405-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orell C. ART adherence in resource poor setting. Curr HIV/AIDS Rep. 2005;2:171–6. doi: 10.1007/s11904-005-0012-8. [DOI] [PubMed] [Google Scholar]
- 13.Monica GA, Paul KF, Richard OA, Joan NK. Non adherence to anti-TB drugs among TB/HIV co-infected patients in Mibarara Hospital Uganda: Prevalence and associated factors. Afr Health Sci. 2009;9:8–15. [PMC free article] [PubMed] [Google Scholar]
- 14.Mukherjee JS, Ivers L, Leandre F, Farmer P, Behforouz H. Antiretroviral therapy in resource-poor settings.Decreasing barriers to access and promoting adherence. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S123–6. doi: 10.1097/01.qai.0000248348.25630.74. [DOI] [PubMed] [Google Scholar]
- 15.Lanièce I, Ciss M, Desclaux A, Diop K, Mbodj F, Ndiaye B, et al. Adherence to HAART and its principal determinants in a cohort of Senegalese adults. AIDS. 2003;17(Suppl 3):S103–8. doi: 10.1097/00002030-200317003-00014. [DOI] [PubMed] [Google Scholar]
- 16.Nachega JB, Stein DM, Lehman DA, Hlatshwayo D, Mothopeng R, Chaisson RE, et al. Adherence to antiretroviral therapy in HIV-infected adults in Soweto, South Africa. AIDS Res Hum Retroviruses. 2004;20:1053–6. doi: 10.1089/aid.2004.20.1053. [DOI] [PubMed] [Google Scholar]
- 17.Okuno J, Yanagi H, Tomura S. Is cognitive impairment a risk factor for poor compliance among Japanese elderly in the community? Eur J Clin Pharmacol. 2001;57:589–94. doi: 10.1007/s002280100347. [DOI] [PubMed] [Google Scholar]
- 18.Waus D, Singhs AK. Non adherence to TB treatment in the eastern Tarai Nepal. Int J Tuberc Lung Dis. 2003;7:327–31. [PubMed] [Google Scholar]


