Abstract
Background
Caffeine is the world’s most widely used central nervous system stimulant, with about 80% consumed in form of coffee. However, studies that analyzed prospectively the relation of coffee or caffeine consumption and depression risk are scarce.
Methods
A total of 50,739 U.S. women (mean age=63 years) free from depressive symptoms at baseline (1996) were prospectively followed until 2006. Caffeine and coffee consumption, and other caffeinated and decaffeinated beverages, were obtained from validated questionnaires completed between 1980 through 2002 and computed as cumulative average of consumption with a 2-year latency applied. Clinical depression was defined as reporting both physician-diagnosed depression and antidepressant use. Relative risks of clinical depression were estimate using Cox proportional hazards regression models.
Results
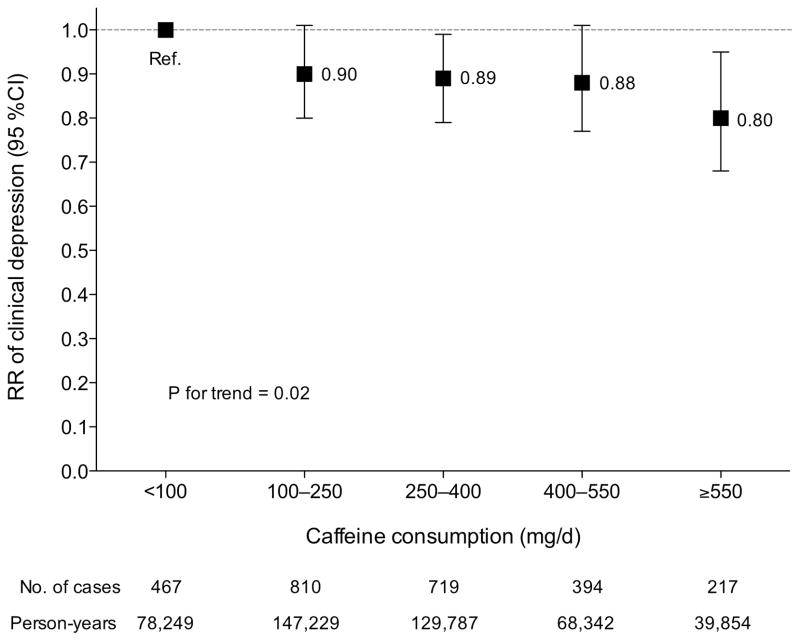
During 10 years of follow-up (1996–2006), 2,607 incident cases of depression were identified. Compared to women consuming caffeinated coffee less frequently (≤1 cup/wk), multivariate relative risk of depression was 0.85 (95% confidence interval [CI], 0.75 to 0.95) for those consuming 2–3 cups/d and 0.80 (95%CI, 0.64 to 0.99; P trend <0.001) for those consuming ≥4 cups/d. Multivariate relative risk for depression was 0.80 (95%CI, 0.68 to 0.95; P trend=0.02) for women in the highest (≥550 mg/d) vs. lowest (<100 mg/d) of the 5 caffeine consumption categories. Decaffeinated coffee was not associated with depression risk.
Conclusions
In this large longitudinal study we found that depression risk decreases with increasing caffeinated coffee consumption. Further investigations are needed to confirm this finding and to determine whether usual caffeinated coffee consumption may contribute to depression prevention.
Caffeine (1,3,7-trimethylxanthine) is the world’s most frequently ingested psychoactive substance,1 with about 80% consumed in the form of coffee.2 However, its impact on depression is poorly understood and under-studied. To our knowledge, only one prospective study among men has examined the association between coffee/caffeine consumption and depression risk reporting a significant inverse association between coffee drinking and depression, but no association with tea or caffeine.3 In 2 U.S.4–6 cohort studies, strong inverse associations have been reported between coffee/caffeine consumption and suicide, which is strongly associated with depression, and a J-shaped relation was noted for coffee and suicide risk in a Finnish cohort.6
Depression is a chronic and recurrent illness that affects 2 times more women than men,7 and about 20% of the US women will be affected during their lifetime.8 Identification of risk factors for depression among women and developing new preventive strategies is therefore a public health priority. Thus, we accessed data from the Nurses’ Health Study, a large cohort of women, to examine prospectively whether caffeine consumption or intake of certain caffeine-containing beverages is associated with the risk of depression.
Methods
Study population
The Nurses’ Health Study is a prospective cohort of 121,700 U.S. female registered nurses aged 30 to 55 years at enrollment in 1976. Every 2 years, participants provide updated information, via mailed questionnaires, about lifestyle, medical history and newly-diagnosed medical illnesses. Women were first asked to report their use of antidepressants in 1996 and their history of physician-diagnosed depression in 2000. A total of 97,103 women had completed one of the 1996, 1998, or 2000 questionnaires. To examine prospectively the relation of caffeine consumption to depression, we excluded from the analyses those women who could have had depression before 1996. This group included 35,892 women with incomplete depression history (i.e. those who did not report their depressive status in 1996, 1998, or 2000, or did not return or answer the 1992 or 1996 Mental Health Index (MHI-5) questionnaires,9–11 a 5-item subscale of the Short-Form 36 Health Status Survey), as well as women who reported in 1996 using antidepressants (n=2,052) or had a physician-diagnosed episode of depression in 1996 or before (n=3,445), or with an unknown start date (n=131), or reported severe depressive symptoms (score ≤52) on the 1992 (n=2,381) or 1996 (n=2,271) MHI-5 questionnaire. A total of 50,931 women were considered depression-free in 1996 and comprised the baseline population for the current analyses. After excluding those who had missing values for exposure variables (N=192), the final 1996 baseline population comprised 50,739 women. The study protocol was approved by the Institutional Review Boards of Brigham and Women’s Hospital and the Harvard School of Public Health.
Assessment of exposure
In 1980, 1984, 1986, 1990, 1994, 1998 and 2002, caffeine consumption and other dietary variables among participants were assessed using a semi-quantitative food-frequency questionnaire.12 Among items of these questionnaires were coffee (“coffee with caffeine” and “decaffeinated coffee”), tea (“nonherbal tea”), soft drinks with caffeine (sugared or low-calorie Coke, Pepsi, or other cola), soft drinks without caffeine (sugared or low-calorie caffeine-free Coke, Pepsi, or other carbonated beverage, e.g. 7-Up), and chocolate. All of the food-frequency questionnaires addressed the usual consumption during the previous 12 months of a specified amount (e.g., 1 cup for coffees and tea, 1 glass or can for soft drinks, 1 bar or packet for chocolate) and allowed 9 possible response categories ranging from never to 6 or more per day. Consumptions of nutrients and caffeine were calculated, as described elsewhere,12 primarily using concurrent U.S. Department of Agriculture food composition data. In these calculations, we assumed that the content of caffeine was 137 mg per cup of coffee, 47 mg per cup of tea, 46 mg per can or bottle of soft drink, and 7 mg per serving of chocolate. The food-frequency questionnaires have been evaluated in detail with regard to reproducibility and validity.12–14 The validation studies revealed high correlations between self-reported coffee consumption according to the food-frequency questionnaires and the 2 or 4 weeks of diet records (r =0.78).13 High correlations were also observed for other caffeinated beverages (tea: 0.93; soft drinks: 0.84).
Case ascertainment
Incident depression was defined as reporting both a new physician-diagnosed depression and beginning regular antidepressant use (i.e. used regularly in past 2 years). In 2000, participants were asked to report the year of their first physician-diagnosed depression (1996 or before, 1997, 1998, 1999, or 2000). Thereafter, this information was updated biennially through 2006. The question on regular antidepressant medication use was first asked in 1996 and then biennially updated through 2006. Hence, the 1996 questionnaire cycle was considered as baseline.
Covariates assessment
Demographic, lifestyle behavior, and comorbidity information were collected using the standardized questionnaires mailed to the nurses. In the baseline questionnaire (1996), we requested information about age, weight and smoking, menopausal status and use of postmenopausal hormone therapy, previously diagnosed medical conditions, including diabetes, cancer, myocardial infarction or angina, and high blood pressure. This information has been updated in the biennial follow-up questionnaires. Marital status, retirement and social or community group involvement (eg, “How many hours each week do you participate in any church, volunteer, or other community group?”) were obtained at baseline (1996) and updated in 2000 and 2004. Participants were asked to report the hours spent per week on moderate (eg, brisk walking) and vigorous (eg, strenuous sports and jogging) exercise, and then the total hours of metabolic equivalent tasks per week (METh/wk) were estimated on the basis of the MET score assigned to each activity.15 Dietary variables were assessed using validated semi-quantitative food-frequency questionnaire.12 Mental health was assessed using SF-36 Health Status Survey in the 1996 questionnaire. MHI-5 score was categorized as 86–100, 76–85, and 53–75.
Statistical analysis
Instead of using a single measurement, and to reduce random measurement error, analyses were conducted using the cumulative average of caffeine consumption from all the available questionnaires prior to the beginning of each 2-year period follow-up.16 Since our last food-frequency questionnaire used before baseline was in 1994, our analyses imply a latency of exposure of 2-year minimum. For example, the cumulative average of caffeine consumption information of 1980 through 1994 was used to predict clinical depression episode in 1996–1998, consumptions of 1980 through 1994 for 1998–2000 follow-up period, intakes of 1980 through 1998 for 2000–2002 follow-up period, and so on. Similar analyses were conducted for categories of coffee consumption and other sources of caffeine. Person-years of follow-up were calculated from the date of return of the 1996 questionnaire to the earliest of: the return date of the questionnaire with first occurrence of depression, date of death, end of follow-up (June 1, 2006), or return date of their last questionnaire. Cox proportional hazards models, stratified on age in months and questionnaire cycle, were used to estimate the relative risks and their 95% confidence intervals (95%CIs) of developing clinical depression. All relevant covariates that remained significant at P<0.20 in the multivariate model and made an important difference in the exposure effect estimate (i.e. more than a 10 % change in RRs) were kept in the final multivariate model.17 Initially, the relative risks were adjusted for known and putative risk factors of depression including current postmenopausal hormonal use (binary), body-mass index (BMI; <25, 25–29.9, ≥30 kg/m2), marital status (married/partnership, widowed, separated/divorced/single), social or community group involvement (binary), smoking (never smoked, past smoker, current smoker), total energy intake (continuous), physical activity (quintiles), retirement (binary), self-reported history of diagnosis of diabetes (binary), cancer (binary), myocardial infarction or angina (binary), and high blood pressure (binary), and the MHI-5 score (86–100, 76–85, 53–75) in 1996, as in a previous study.18 In the sensitivity analysis of multivariate model, a minimum of 8-year latency was applied, i.e. cumulative average consumption from 1980 through 1986 was used for 1996–1998 follow-up period, consumption from 1980 through 1990 for 1998–2000 follow-up period, and so on. It is well-known that the caffeine half-life is reduced by 30–50% in smokers and doubled in women taking oral contraceptives or other exogenous estrogens.19 Therefore, we tested the interactions between these factors and caffeine/coffee consumption for depression risk. Since a significant percentage of depressed cases might never receive treatment, and some proportion of those who do may receive treatments other than antidepressants, we repeated our main analyses using a broader definition of depression that required a physician diagnosis or use of antidepressants (Supplemental Table 1). All analyses were performed with SAS software, version 9.1 (SAS Institute Inc., 2003). All P values reported are 2-sided.
RESULTS
Participant characteristics according to categories of caffeinated coffee are presented in Table 1. Compared with women with least frequent consumption of coffee, regular coffee drinkers were more likely to be current smokers and to consume more alcohol, less likely to be involved in social/community groups, and reported lower prevalence of obesity, high blood pressure and diabetes. In this cohort, 13.1% (n=6,669) of the women reported that they never drink caffeinated coffee. In 1994, the most recent measure of diet before baseline, mean caffeine consumption was 236 mg/d for the entire cohort, and ranged from 73 mg/d in women drinking coffee less frequently (≤1 cup/wk) to 649 mg/d in women drinking ≥4 cups/d. Caffeinated coffee contributed to 82% of total daily consumption of caffeine, whereas tea contribution was 13%, and caffeinated soft drinks was 5.7%. Caffeinated coffee consumption was negatively correlated with decaffeinated coffee (r=−0.13) and tea (r=−0.19) consumption.
Table 1.
Age-Standardized Characteristics of the Cohort.a
| Caffeinated coffee consumption (cupsb)
|
|||||
|---|---|---|---|---|---|
| ≤1/wk | 2–6/wk | 1/d | 2–3/d | ≥4/d | |
| No. of women | 12,215 | 6,617 | 17,234 | 12,290 | 2,383 |
| Mean (SD) | |||||
| Age, y | 62.7 (7.3) | 63.8 (7.0) | 63.3 (7.0) | 62.8 (6.7) | 62.1 (6.6) |
| BMI, kg/m2 | 26.4 (5.2) | 26.4 (5.0) | 26.2 (4.9) | 26.0 (4.7) | 25.8 (4.7) |
| Physical activity, MET-h/wk | 18.7 (21.1) | 19.6 (25.5) | 19.3 (22.5) | 18.9 (22.0) | 17.5 (22.0) |
| Daily intake (1994) | |||||
| Total energy, kcal | 1695 (503) | 1720 (503) | 1729 (499) | 1770 (512) | 1791 (533) |
| Alcohol, %energy | 2.9 (4.0) | 3.1 (4.1) | 3.6 (4.3) | 3.9 (4.4) | 3.6 (4.4) |
| Caffeine, mgc | 73 (75) | 127 (110) | 232 (165) | 386 (180) | 649 (220) |
| Decaffeinated coffee, cups | 0.5 (0.9) | 0.8 (1.1) | 0.7 (1.1) | 0.5 (1.1) | 0.3 (1.0) |
| Tea, cups | 0.9 (1.3) | 0.7 (1.0) | 0.6 (0.9) | 0.5 (0.8) | 0.3 (0.8) |
| Chocolate, bar or packet | 0.1 (0.2) | 0.1 (0.2) | 0.1 (0.2) | 0.1 (0.2) | 0.1 (0.2) |
| Caffeinated sugared soft drink, glasses or cans | 0.1 (0.3) | 0.1 (0.2) | 0.1 (0.2) | 0.1 (0.3) | 0.1 (0.3) |
| Caffeinated low-calorie soft drink, glasses or cans | 0.2(0.6) | 0.2(0.5) | 0.2(0.5) | 0.3(0.6) | 0.2(0.6) |
| % of group | |||||
| MHI-5 scored | |||||
| ≥86 | 45.2 | 44.2 | 43.9 | 42.7 | 44.8 |
| 76–85 | 35.1 | 37.4 | 36.6 | 37.2 | 35.3 |
| 53–75 | 19.5 | 18.2 | 19.3 | 19.9 | 19.4 |
| Caucasian | 97.3 | 97.3 | 98.2 | 98.8 | 99.0 |
| Involved in social/community group, ≥1hr/wk | 67.8 | 66.2 | 61.5 | 59.4 | 54.3 |
| Retired | 49.1 | 49.8 | 48.8 | 49.2 | 50.0 |
| Marital status | |||||
| Married/Partnership | 81.5 | 81.2 | 79.4 | 78.3 | 73.2 |
| Widowed | 12.4 | 12.6 | 13.4 | 14.1 | 17.4 |
| Separated/divorced/single | 6.1 | 6.2 | 7.3 | 7.6 | 9.4 |
| Current menopausal hormones | 41.4 | 42.3 | 41.3 | 40.0 | 34.6 |
| Reported diagnosis of | |||||
| Myocardial infarction or angina | 4.0 | 4.0 | 3.8 | 3.0 | 2.9 |
| High blood pressure | 31.0 | 32.7 | 30.1 | 26.5 | 22.5 |
| Diabetes | 5.3 | 4.8 | 3.9 | 3.7 | 2.5 |
| Cancer | 6.7 | 6.6 | 6.7 | 6.0 | 6.8 |
| Smoking status | |||||
| Never smoker | 60.1 | 51.9 | 44.0 | 35.5 | 25.0 |
| Past smoker | 34.9 | 42.8 | 47.5 | 49.0 | 40.3 |
| Current smoker | 5.0 | 5.3 | 8.5 | 15.5 | 34.7 |
| BMI, kg/m2 | |||||
| < 25 | 46.4 | 46.3 | 47.1 | 47.3 | 47.9 |
| 25–29.9 | 32.4 | 33.8 | 33.9 | 34.8 | 34.8 |
| ≥ 30 | 20.9 | 19.7 | 18.8 | 17.7 | 17.1 |
All characteristics are for 1996, except if otherwise indicated. Caffeinated coffee consumption was computed as the cumulative average between 1980 through 2002. BMI indicates body-mass index. MET=metabolic equivalents of task.
One cup=150 ml.
Caffeine was calculated from coffee and non-coffee sources (tea, soft drink, chocolate) and adjusted for total energy intake with residual model.
MHI-5 indicates 5-items Mental Health Index score measured in 1996. A higher score denotes a better mental health.
Among the 50,739 women who were free from clinical depression or severe depressive symptoms at baseline, we documented 2,607 incident cases of clinical depression during the 10-year (463,462 person-years) follow-up (1996–2006). There was an inverse age-adjusted dose-response relationship between caffeinated coffee and depression risk (P for trend = 0.03, Table 2). This inverse gradient became slightly stronger after adjusting for all covariates, mainly reflecting negative confounding by smoking status. Similar results were noted when we ran our multivariate-models with a minimum 8-year latency of exposure (Table 2, sensitivity model). We also observed similar risk estimates, somewhat stronger for caffeinated coffee, when we utilized the broader definition of depression that required a physician diagnosis or use of antidepressants (Supplemental Table 1). Further adjustment for alcohol intake did not materially affect the results.
Table 2.
Relative Risks (95% CI) of Clinical Depression According to Coffee Consumption.a
| Caffeinated coffee consumption (cups)
|
||||||
|---|---|---|---|---|---|---|
| ≤1/wk | 2–6/wk | 1/d | 2–3/d | ≥4/d | P Trend | |
| No. of cases | 670 | 373 | 905 | 564 | 95 | |
| Person-years | 113,305 | 63,322 | 163,256 | 105,619 | 17,960 | |
| Age-adjustedb | 1.00 | 1.02 (0.90–1.16) | 0.96 (0.87–1.06) | 0.90 (0.80–1.01) | 0.88 (0.71–1.09) | 0.03 |
| Multivariate modelc | 1.00 | 1.00 (0.88–1.14) | 0.92 (0.83–1.02) | 0.85 (0.75–0.95) | 0.80 (0.64–0.99) | <0.001 |
| Sensitivity modeld | 1.00 | 0.96 (0.84–1.01) | 0.98 (0.88–1.09) | 0.88 (0.78–0.98) | 0.82 (0.68–0.98) | 0.005 |
| Decaffeinated coffee consumption (cups)
|
||||||
|---|---|---|---|---|---|---|
| ≤1/wk | 1–4/wk | 5–6/wk | 1/d | ≥2/d | P Trend | |
| No. of cases | 1,413 | 355 | 154 | 560 | 125 | |
| Person-years | 258,704 | 59,296 | 23,743 | 95,469 | 26,249 | |
| Age-adjustedb | 1.00 | 1.12 (1.00–1.26) | 1.25 (1.05–1.47) | 1.10 (1.00–1.21) | 0.87 (0.72–1.04) | 0.77 |
| Multivariate modelc | 1.00 | 1.12 (1.00–1.26) | 1.24 (1.05–1.46) | 1.09 (0.98–1.20) | 0.84 (0.70–1.01) | 0.89 |
| Sensitivity modeld | 1.00 | 1.09 (0.95–1.25) | 1.00 (0.83–1.21) | 1.15 (1.04–1.28) | 0.85 (0.73–0.99) | 0.75 |
| Excluding coffee drinkerse | ||||||
| No. of cases | 521 | 141 | 56 | 262 | 63 | |
| Person-years | 89,993 | 23,150 | 9,553 | 41,443 | 12,487 | |
| Multivariate modelc | 1.00 | 1.05 (0.87–1.27) | 1.04 (0.79–1.38) | 1.07 (0.92–1.24) | 0.80 (0.61–1.05) | 0.45 |
Coffee consumption was computed as the cumulative average between 1980 through 2002 (see Methods section). Clinical depression = physician-diagnosed depression and antidepressant medication use (1996–2006).
Adjusted for age (continuous) and time interval.
Further adjusted for total energy intake (continuous), current menopausal hormones (binary), smoking status (never smoked, past smoker, current smoker), body-mass index (<25, 25–29.9, ≥30 kg/m2), physical activities (quintiles), marital status (married/partnership, widowed, separated/divorced/single), not involve in social or community group (binary), retired (binary), reported diagnosis of diabetes (binary), cancer (binary), high blood pressure (binary), myocardial infarction or angina (binary) and for Mental Health Index-5 score (86–100, 76–85, 53–75) in 1996.
The same as the multivariate model but using a latency of exposure of 8-year minimum (see Methods section).
Women drinking 1 or more cups of caffeinated coffee per day were excluded (1,043 cases remaining). ).
To evaluate if the association between caffeine and depression risk could be explained by some components of coffee other than caffeine, we examined association between decaffeinated coffee and depression (Table 2). After controlling for caffeinated coffee and other covariates, compared to women with the lowest consumption of decaffeinated coffee (≤1 cup/wk), risk of depression was increased for higher consumption, with the exception of the very highest consumption category (≥2/d). After further excluding women drinking ≥1 cup/d caffeinated coffee to avoid contamination by caffeinated coffee consumption, no significant association was noted between decaffeinated coffee and depression. In addition, no associations were found between caffeinated tea (P for trend=0.92), sugared soft drink (P for trend=0.58), or chocolate consumption (P for trend=0.89) and depression risk (data not shown).
There was an inverse dose-response relationship between caffeine consumption and depression risk in our multivariate model (P for trend=0.02, Figure 1). Compared to the lowest caffeine consumption group (<100 mg/d), multivariate relative risk for depression was 0.80 (95% CI, 0.68 to 0.95) for women in the highest caffeine consumption group (≥550 mg/d). As coffee contributes most to total caffeine consumption, we examined the association between caffeine from non-coffee sources and depression risk after excluding women who consumed one or more cups of caffeinated coffee daily (21,016 women and 1,043 cases remaining). No significant association was found between caffeine from non-coffee sources and depression risk (P for trend=0.18). Compared to the lowest caffeine from non-coffee sources (<50 mg/d), multivariate relative risk for depression was 0.99 (95% CI, 0.84 to 1.15) for consumption of 50–100 mg/d, 0.89 (95% CI, 0.71 to 1.11) for 100–150 mg/d, and 0.85 (95% CI, 0.63 to 1.14) for consumption ≥150 mg/d. For the 1,089 women (49 cases) who consumed ≥150 mg/d of caffeine from these sources, the wide confidence interval included both the null value and the relative risk seen for caffeine from coffee.
Figure 1. Multivariate-Adjusted Relative Risks (95% CI) of Clinical Depression According to Caffeine Consumptiona.
aCaffeine was calculated from coffee and non-coffee sources (tea, soft drink, chocolate) and adjusted for total energy intake with residual model. Adjusted for age (continuous), time interval, total energy intake (continuous), current menopausal hormones (binary), smoking status (never smoked, past smoker, current smoker), body-mass index (<25, 25–29.9, ≥30 kg/m2), physical activities (quintiles), marital status (married/partnership, widowed, separated/divorced/single), not involve in social or community group (binary), retired (binary), reported diagnosis of diabetes (binary), cancer (binary), high blood pressure (binary), myocardial infarction or angina (binary) and for Mental Health Index-5 score (86–100, 76–85, 53–75) in 1996.
A marginal significant interaction (P=0.06) was noted between current smoking (yes/no) and caffeinated coffee consumption (cups/d) for depression risk. For each 2 cups/d increase of caffeinated coffee, the multivariate relative risk for depression was 0.78 (95% CI, 0.66 to 0.93) for current smokers (n cases=263) and 0.95 (95% CI, 0.89 to 1.01) for never and past smokers (n cases=2,344). However, interaction between current menopausal hormone use (yes/no) and caffeinated coffee consumption (cups/d) was not significant (P=0.42) for depression risk.
Discussion
In this large prospective cohort of older women free from clinical depression or severe depressive symptoms at baseline, risk of depression decreased in a dose-dependent manner with increasing consumption of caffeinated coffee. Consumption of decaffeinated coffee was not associated with reduced risk of depression. Most previous studies that investigated the relationship between caffeine or coffee consumption and depression were cross-sectional20–28 and thus unable to determine whether coffee consumption affects depression or vice-versa. The only previous prospective study was conducted in Finland in a population-based cohort of 2,232 men; 49 cases of depression were identified after 17.5-year follow-up through the national hospital discharge register.3 In this cohort, the multivariate-adjusted relative risks of depression was 0.28 (95% CI, 0.08 to 0.96) for light coffee drinker (<375 ml/d), 0.45 (95% CI, 0.16 to 1.29) for moderate coffee drinker (375–813 ml/d) and 0.23 (95% CI, 0.06 to 0.83) for heavy coffee drinkers (>813 ml/d), compared to non-drinkers. Although no associations were observed for quartiles of caffeine consumption, an inverse association could have been obfuscated by the high caffeine consumption of the lowest quartile (up to 425 mg/d) and small sample size. In 2 U.S.4, 5 cohort studies, a lower risk of suicide has been reported with a higher coffee consumption. However, a J-shape association was noted for coffee and suicide risk in a cohort study from Finland. The risk of suicide decreased progressively until coffee consumption reached 6–7 cups/d, but increased with consumption of 8–9 and ≥10 cups/d.6 It is possible that persons with more severe forms of depression used very high doses of coffee as a form of self-medication that was, nevertheless, insufficient to elevate their mood. We observed an inverse dose-response relation between caffeine or caffeinated coffee consumption and depression risk, but we were unable address the effects of very high consumption because only 0.52% of our participants drank ≥6 cups/d of caffeineated coffee. We were also unable to see a relationship between caffeine from non-coffee sources and depression risk, perhaps due to insufficient power particularly after consumers of one or more cups of caffeinated coffee daily were excluded.
In North-America as well as many European countries, coffee and tea are the primary dietary sources of caffeine for adults.2 According to the U.S. Department of Agriculture surveys data (1994–96, 1998), 90% of the US adult population consumed caffeine, and mean consumption ranged from 166 to 336 mg/d.2 Coffee accounts for about 81% of the total daily caffeine consumed by adults older than 36 years.2 Elimination half-life of caffeine can be influenced by many factors including sex, use of oral contraceptives or other exogenous estrogens (approximately twice among users), and smoking (reduced by 30–50%).19 At dose lower than 10 mg/kg caffeine half-life range between 2.5 and 4.5h.19 The significant interaction that we noted between caffeinated coffee and current smoking was unexpected, and may be due to chance. Alternatively, caffeine may antagonize the adverse effects of smoking on depression through still unknown mechanisms, or may interact with genetic factors that predispose to smoking and depression.29
Chronic caffeine consumption has several biological effects that should be taken into account when considering the plausibility of its potential to reduce depression risk. At low to moderate doses, caffeine has well-known psychostimulant effects such as improved psychomotor performance, increased vigilance, elevated arousal (lesser somnolence and greater activation), and increased sensations of well-being and energy.30, 31 The known effects of caffeine are dose-dependent, but typically biphasic, i.e. low doses are perceived as pleasant and stimulating whereas a reverse effect is observed with higher doses.32 Most individuals seem to adapt their caffeine consumption to their own tolerance, so that the habitual is within the range between reinforcing and aversive effects.32 Caffeine affects brain function mainly by its antagonist action on the adenosine A2a receptor and, therefore, plays a role in the modulation of dopaminergic transmission.30, 33 The antagonist effect of caffeine on adenosine might also imply non-dopaminergic mechanisms, such as modulation of the release of acetylcholine and serotonin.30
The major strengths of this study include its large sample size, prospective design, and repeated measures of caffeine, caffeinated beverages and other covariates, which relied on the use of validated food-frequency questionnaires administered 7 times over a period of 22 years. This study also has limitations and the results should thus be interpreted with caution. First and foremost, because of its observational design, this study cannot prove that caffeine or caffeinated coffee reduce the risk of depression, but only suggest the possibility of such protective effect. Reverse causation is another concern in most epidemiological studies. To minimize this bias, we excluded at baseline 10,280 women with severe depressive symptoms, and we computed the cumulative average of caffeinated and not-caffeinated beverages with at least 2-year latency; yet, we cannot exclude the possibility that mild depressive symptoms were the common reason for low caffeine/coffee consumption and incident depression. Furthermore, we confirmed the robustness of our results in sensitivity analyses using at least 8-year lag of exposure.
In individuals with a particular genetic background34 or otherwise sensitive, caffeine might induce sleep disturbances and insomnia35 or anxiogenic effects.20, 36, 37 It is possible that sleep-sensitive or anxious women are aware of the stimulatory effects of caffeine and lower their consumption accordingly. A similar behavior among depressed women or women predisposed to depression in our cohort might thus explain our results, because the majority of late-life depressions occur among women who already had previous episodes,38 and lacking a lifetime history of depression we cannot exclude this possibility. Biased relative risk estimates may also result from error in assessing caffeine consumption. Dietary validation studies, however, have indicated that the frequency of coffee consumption reported on a food-frequency questionnaire is highly reproducible (r=0.78) and agrees well with assessments using diet records.13 Although between-person variation in cup size and strength of the coffee brew have probably contributed to some random misclassification with regard to the exposure, this would be more likely to weaken rather than strengthen observed associations between coffee consumption and depression risk. Finally, some outcome misclassification bias is inevitable because of a combination of errors in reporting depression and antidepressants use, low recognition of depression by physicians,39 under-treatment of depression,40 and use of antidepressant medication for indications other than depression.41–43 We tried to maximize the specificity of case definition, accepting as incident cases of depression only women who reported both a diagnosis of depression and the use of antidepressants. This definition excludes women with untreated depression, as well as women who used antidepressants for short period of time and were not regular users at the time of completing one of the biennial questionnaires. However, to the extent that the probability of correctly classifying women with an incident case of depression is independent from their dietary habits (non-differential misclassification of outcome), the low sensitivity of this strict case definition should not bias RR estimates.44 Over 10 years of follow-up, we noted an incident rate of clinical depression of 5.6 per 1,000 person-years. This incidence is not directly comparable to that observed in unselected populations because to minimize reverse causation we excluded women with severe depressive symptoms at baseline, thus eliminating a group of women at higher risk of depression.
In conclusion, our results support a possible protective effect of caffeine, mainly from coffee consumption, on risk of depression. These findings are consistent with earlier observations that suicide risk is lower among persons with higher consumption of coffee. Further investigations are needed to confirm this finding and to determine whether usual caffeinated coffee consumption may contribute to prevention or treatment of depression.
Supplementary Material
Acknowledgments
Funding/Support: The study was supported by National Institutes of Health (NIH) Grant DK58845. Dr Ascherio received a grant from the National Alliance for Research on Schizophrenia & Depression (Project ID: 5048070–01) and was supported by R01 NS061858. Dr Lucas received a postdoctoral fellowship from the Fonds de recherche en santé du Québec (FRSQ). The funding sources were not involved in data collection, data analysis, manuscript writing and publication.
Role of the Sponsors: The funding sources were not involved in the data collection, data analysis, manuscript writing, and publication.
Footnotes
Author Contributions: All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Lucas, Okereke, Willett, and Ascherio. Acquisition of data: Willett and Ascherio. Analysis and interpretation of data: Lucas, Mirzaei, Pan, Okereke, Willett, O’Reilly, Koenen, and Ascherio. Critical revision of the manuscript for important intellectual content: Lucas, Mirzaei, Pan, Okereke, Willett, O’Reilly, Koenen, and Ascherio. Statistical analysis: Lucas, Okereke, O’Reilly, and Ascherio. Obtained funding: Willett and Ascherio. Administrative, technical, and material support: Willett and Ascherio. Study supervision: Willett, Koenen, Okereke, and Ascherio.
Financial Disclosure: None reported
Additional Contributions: We thank the Nurses’ Health Study participants for their continuing contributions.
References
- 1.Heckman MA, Weil J, Gonzalez de Mejia E. Caffeine (1, 3, 7-trimethylxanthine) in foods: a comprehensive review on consumption, functionality, safety, and regulatory matters. J Food Sci. 2010;75(3):77–87. doi: 10.1111/j.1750-3841.2010.01561.x. [DOI] [PubMed] [Google Scholar]
- 2.Frary CD, Johnson RK, Wang MQ. Food sources and intakes of caffeine in the diets of persons in the United States. J Am Diet Assoc. 2005;105(1):110–113. doi: 10.1016/j.jada.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 3.Ruusunen A, Lehto SM, Tolmunen T, Mursu J, Kaplan GA, Voutilainen S. Coffee, tea and caffeine intake and the risk of severe depression in middle-aged Finnish men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Public Health Nutr. 2010;13(8):1215–1220. doi: 10.1017/S1368980010000509. [DOI] [PubMed] [Google Scholar]
- 4.Klatsky AL, Armstrong MA, Friedman GD. Coffee, tea, and mortality. Ann Epidemiol. 1993;3(4):375–381. doi: 10.1016/1047-2797(93)90064-b. [DOI] [PubMed] [Google Scholar]
- 5.Kawachi I, Willett WC, Colditz GA, Stampfer MJ, Speizer FE. A prospective study of coffee drinking and suicide in women. Arch Intern Med. 1996;156(5):521–525. [PubMed] [Google Scholar]
- 6.Tanskanen A, Tuomilehto J, Viinamaki H, Vartiainen E, Lehtonen J, Puska P. Heavy coffee drinking and the risk of suicide. Eur J Epidemiol. 2000;16(9):789–791. doi: 10.1023/a:1007614714579. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 9.Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Vol. 8. Boston, MA: The Health Institute, New England Medical Center; 1994. pp. 23–28. [Google Scholar]
- 10.Yamazaki S, Fukuhara S, Green J. Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan. Health Qual Life Outcomes. 2005;3:48. doi: 10.1186/1477-7525-3-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 13.Salvini S, Hunter DJ, Sampson L, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol. 1989;18(4):858–867. doi: 10.1093/ije/18.4.858. [DOI] [PubMed] [Google Scholar]
- 14.Willett WC. Nutritional epidemiology. 2. New York (NY): Oxford University Press; 1998. p. 414. [Google Scholar]
- 15.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 16.Hu FB, Stampfer MJ, Rimm E, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149(6):531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 17.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- 18.Kroenke CH, Bennett GG, Fuchs C, et al. Depressive symptoms and prospective incidence of colorectal cancer in women. Am J Epidemiol. 2005;162(9):839–848. doi: 10.1093/aje/kwi302. [DOI] [PubMed] [Google Scholar]
- 19.Arnaud MJ. The pharmacology of caffeine. Prog Drug Res. 1987;31:273–313. doi: 10.1007/978-3-0348-9289-6_9. [DOI] [PubMed] [Google Scholar]
- 20.Greden JF, Fontaine P, Lubetsky M, Chamberlin K. Anxiety and depression associated with caffeinism among psychiatric inpatients. Am J Psychiatry. 1978;135(8):963–966. doi: 10.1176/ajp.135.8.963. [DOI] [PubMed] [Google Scholar]
- 21.Gilliland K, Andress D. Ad lib caffeine consumption, symptoms of caffeinism, and academic performance. Am J Psychiatry. 1981;138(4):512–514. doi: 10.1176/ajp.138.4.512. [DOI] [PubMed] [Google Scholar]
- 22.Leibenluft E, Fiero PL, Bartko JJ, Moul DE, Rosenthal NE. Depressive symptoms and the self-reported use of alcohol, caffeine, and carbohydrates in normal volunteers and four groups of psychiatric outpatients. Am J Psychiatry. 1993;150(2):294–301. doi: 10.1176/ajp.150.2.294. [DOI] [PubMed] [Google Scholar]
- 23.Quinlan PT, Lane J, Moore KL, Aspen J, Rycroft JA, O’Brien DC. The acute physiological and mood effects of tea and coffee: the role of caffeine level. Pharmacol Biochem Behav. 2000;66(1):19–28. doi: 10.1016/s0091-3057(00)00192-1. [DOI] [PubMed] [Google Scholar]
- 24.Haskell CF, Kennedy DO, Wesnes KA, Scholey AB. Cognitive and mood improvements of caffeine in habitual consumers and habitual non-consumers of caffeine. Psychopharmacology (Berl) 2005;179(4):813–825. doi: 10.1007/s00213-004-2104-3. [DOI] [PubMed] [Google Scholar]
- 25.Hintikka J, Tolmunen T, Honkalampi K, et al. Daily tea drinking is associated with a low level of depressive symptoms in the Finnish general population. Eur J Epidemiol. 2005;20(4):359–363. doi: 10.1007/s10654-005-0148-2. [DOI] [PubMed] [Google Scholar]
- 26.Kendler KS, Myers J, COG Caffeine intake, toxicity and dependence and lifetime risk for psychiatric and substance use disorders: an epidemiologic and co-twin control analysis. Psychol Med. 2006;36(12):1717–1725. doi: 10.1017/S0033291706008622. [DOI] [PubMed] [Google Scholar]
- 27.Smith AP. Caffeine, cognitive failures and health in a non-working community sample. Hum Psychopharmacol. 2009;24(1):29–34. doi: 10.1002/hup.991. [DOI] [PubMed] [Google Scholar]
- 28.Xu Q, Anderson D, Courtney M. A longitudinal study of the relationship between lifestyle and mental health among midlife and older women in Australia: findings from the Healthy Aging of Women Study. Health Care Women Int. 2010;31(12):1082–1096. doi: 10.1080/07399332.2010.486096. [DOI] [PubMed] [Google Scholar]
- 29.Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC. Smoking and major depression. A causal analysis. Arch Gen Psychiatry. 1993;50(1):36–43. doi: 10.1001/archpsyc.1993.01820130038007. [DOI] [PubMed] [Google Scholar]
- 30.Ferre S. An update on the mechanisms of the psychostimulant effects of caffeine. J Neurochem. 2008;105(4):1067–1079. doi: 10.1111/j.1471-4159.2007.05196.x. [DOI] [PubMed] [Google Scholar]
- 31.Adan A, Prat G, Fabbri M, Sanchez-Turet M. Early effects of caffeinated and decaffeinated coffee on subjective state and gender differences. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(7):1698–1703. doi: 10.1016/j.pnpbp.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Fredholm BB, Battig K, Holmen J, Nehlig A, Zvartau EE. Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol Rev. 1999;51(1):83–133. [PubMed] [Google Scholar]
- 33.Ferre S, Ciruela F, Borycz J, et al. Adenosine A1-A2A receptor heteromers: new targets for caffeine in the brain. Front Biosci. 2008;13:2391–2399. doi: 10.2741/2852. [DOI] [PubMed] [Google Scholar]
- 34.Yang A, Palmer AA, de Wit H. Genetics of caffeine consumption and responses to caffeine. Psychopharmacology (Berl) 211(3):245–257. doi: 10.1007/s00213-010-1900-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bchir F, Dogui M, Ben Fradj R, Arnaud MJ, Saguem S. Differences in pharmacokinetic and electroencephalographic responses to caffeine in sleep-sensitive and non-sensitive subjects. C R Biol. 2006;329(7):512–519. doi: 10.1016/j.crvi.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 36.Boulenger JP, Uhde TW, Wolff EA, 3rd, Post RM. Increased sensitivity to caffeine in patients with panic disorders. Preliminary evidence. Arch Gen Psychiatry. 1984;41(11):1067–1071. doi: 10.1001/archpsyc.1983.01790220057009. [DOI] [PubMed] [Google Scholar]
- 37.Lee MA, Cameron OG, Greden JF. Anxiety and caffeine consumption in people with anxiety disorders. Psychiatry Res. 1985;15(3):211–217. doi: 10.1016/0165-1781(85)90078-2. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 39.Lowe B, Spitzer RL, Grafe K, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78(2):131–140. doi: 10.1016/s0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- 40.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 41.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 42.Brown J, PMOB, Marjoribanks J, Wyatt K. Selective serotonin reuptake inhibitors for premenstrual syndrome. Cochrane Database Syst Rev. 2009;(2):CD001396. doi: 10.1002/14651858.CD001396.pub2. [DOI] [PubMed] [Google Scholar]
- 43.Stearns V, Ullmer L, Lopez JF, Smith Y, Isaacs C, Hayes D. Hot flushes. Lancet. 2002;360(9348):1851–1861. doi: 10.1016/s0140-6736(02)11774-0. [DOI] [PubMed] [Google Scholar]
- 44.Rothman KJ, Greenland S. Modern Epidemiology. Philadelphia (PA): Lippincott Williams & Wilkins; p. 737. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.