Abstract
Basal cell carcinoma (BCC) of the breast is a rare occurrence. To the best of our knowledge, only 34 cases of this rare malignancy have been reported worldwide. We report the case of a 48 year old lady who presented with history of rapid enlargement of a nevus over breast since three months. On initial examination a diagnosis of melanoma was considered. However the histopathology showed features suggestive of BCC. This case report highlights an atypical presentation of BCC.
Keywords: Basal cell carcinoma, Melanoma, histopathology
INTRODUCTION
Even though basal cell carcinoma (BCC) is amongst the commonest human malignancies, the involvement of breast is uncommon. This is easily explainable as the breast is seldom sun exposed and the etiology of BCC primarily involves sun exposure leading to ultraviolet-ray-induced carcinogenesis. The BCC of the breast is believed to be more aggressive than BCC reported elsewhere in the body. It usually arises as a de novo lesion in the breast.
CASE REPORT
A 48-year-old lady presented with a history of rapidly enlarging hyperpigmented mass over right nipple areola complex and surrounding area for the past 3 months. There was no history of discharge from the nipple or the lesion. The patient was having history suggestive of congenital melanocytic nevi over the affected area. There was no family history of similar complaint. There was no history of exposure to radiation or arsenic exposure. Examination showed a single hyper pigmented, erythematous plaque of about 6 × 4 cm size, with erosions and ulceration, over the nipple and areola of right breast [Figure 1]. No lymph node enlargement was detected clinically. The ultrasonographic and the mammographic examinations were normal. Fine needle aspiration cytology of the lesion was inconclusive. Excision biopsy with 2 cm margin was taken. The histopathological study unexpectedly showed features of BCC [Figure 2]. HMB-45 staining was done to rule out melanoma. Enzyme linked immunosorbent assay done for Human immunodeficiency virus was negative.
Figure 1.

Basal cell carcinoma of breast
Figure 2.
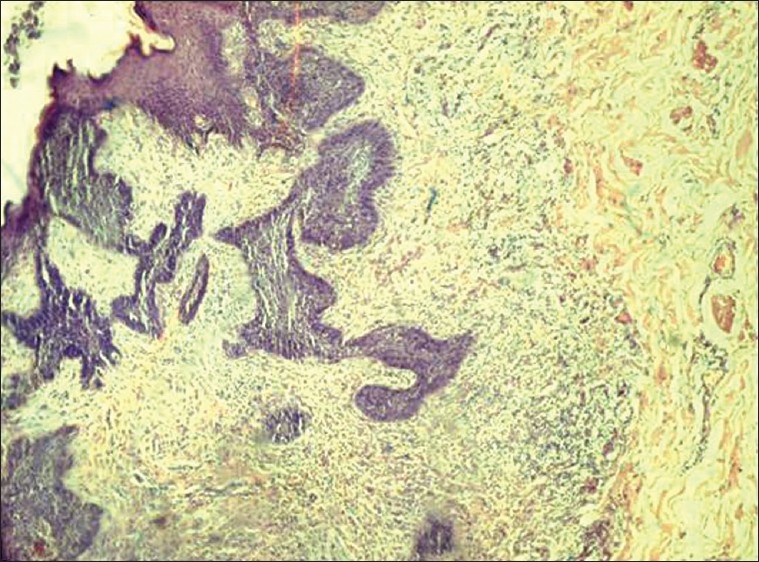
Histopathology diagnostic of basal cell carcinoma
DISCUSSION
BCC is the most common human malignancy in the western world.[1] The skin of the nipple areola complex is however a very rare site of occurrence. A case report published by Takeno et al. in 2010 states that only 34 cases have been reported.[2] A case report published by Chu et al. in 2007 showed that out of 25 reported cases, 16 were male.[3] BCC of the breast involving the female breast is therefore a true rarity.
BCC is typically associated with sun exposure in a light skinned person.[1] However, an immunocompromised status, exposure to radiation, prior burns, exposure to arsenic, and genetic predisposition are other predisposing factors.[4] Heckmann et al. said that areas of high incidence of BCC despite low Ultra violet ray exposure, such as the medial quadrant of orbit are characterized by a concave shape, reduced skin tension, and presence of marked skin folds. They hypothesized that the disturbed cell matrix interaction found at these sites could be a cofactor for the development of BCC.[5] The nipple areola complex may share these characteristics.
The BCC is known for low propensity to metastasize. The overall rate of metastasis in BCC ranges from 0.0028 to 0.5%.[6] However, 3 of the 31 reported cases of nipple areola complex have apparent axillary lymph node enlargement with one histologically confirmed case.[6] It reflects BCC in this region may be more aggressive.
Varying modes of treatment have been described ranging from medical treatment, photodynamic therapy, lasers to Mohs’ microsurgery to simple excision with or without radiotherapy, as well as a partial mastectomy with axillary dissection and plastic reconstruction of the breast.
However, in most cases, simple excision is not followed by recurrence. Mohs’ microsurgery offers maximum tissue shaping and hence may be advantageous.[4] The place of sentinel lymph node biopsy in such cases demands further validation.[7]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gloster HM, Jr, Brodland DG. The epidemiology of skin cancer. Dermatol Surg. 1996;22:217–26. doi: 10.1111/j.1524-4725.1996.tb00312.x. [DOI] [PubMed] [Google Scholar]
- 2.Takeno S, Kikuchi N, Miura T, Anami K, Takahashi Y, Hashimoto T, et al. Basal cell carcinoma of the nipple in male patients with gastric cancer recurrence: Report of a case. Breast Cancer. 2010 doi: 10.1007/s12282-010-0217-6. [In Press] [DOI] [PubMed] [Google Scholar]
- 3.Chu PY, Teng TH, Lee CC. Primary superficial basal cell carcinoma of the nipple. Ann Saudi Med. 2007;27:296–7. doi: 10.5144/0256-4947.2007.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nouri K, Ballard CJ, Bouzari N, Saghari S. Basal cell carcinoma of the areola in a man. J Drugs Dermatol. 2005;4:352–4. [PubMed] [Google Scholar]
- 5.Heckmann M, Zolgeimer F, Konz B. Frequency of facial basal cell carcinoma does not correlate with site-specific UV exposure. Arch Dermatol. 2002;138:1494–7. doi: 10.1001/archderm.138.11.1494. [DOI] [PubMed] [Google Scholar]
- 6.Sinha A, Langtry JA. Secondary intention healing following Mohs micrographic surgery for basal cell carcinoma of the nipple and areola. Acta Derm Venereol. 2010;91:78–9. doi: 10.2340/00015555-0935. [DOI] [PubMed] [Google Scholar]
- 7.Huang CW, Pan CK, Shih TF, Tsai CC, Juan CC, Ker CG. Basal cell carcinoma of the nipple-areola complex: A case report. Kaohsiung J Med Sci. 2005;21:480–3. doi: 10.1016/S1607-551X(09)70155-X. [DOI] [PubMed] [Google Scholar]


