Abstract
Pituitary tumour have a wide way of presentation. Epistaxis due to pituitary adenoma has been rarely reported. There is no report of bleeding from nose as clinical first presentation in a child. We report the first case in literature where a child had epistaxis for eight months before deterioration of vision. He was found to be having a invasive prolactinoma with normal prolactin levels.
Keywords: Epistaxis, hook effect, invasive pituitary adenoma, prolactinoma
Introduction
Epistaxis (bleeding from nose) in children is generally traumatic in origin, the most common site of bleed being little's area. It generally settles spontaneously with the help of cold or mechanical compressions. Sometimes, the bleeding can be torrential leading to severe hemodynamic alterations. Besides trauma that generally occurs due to finger nails eroding the nasal mucosa, there are several tumors which can present with epistaxis.[1]
Rarely, giant prolactinoma has been reported as the cause of epistaxis in adults.[2]
We report the first case in literature where a child with giant prolactinoma has presented with epistaxis as a primary complaint with normal serum prolactin level.
Case Report
A thirteen-year-old child had presented with bleeding from right nostril about eight months back. The bleeding was moderate, almost daily soaking a handkerchief every day. He started taking some homoeopathic medicine which decreased the quantity of bleeding but not the frequency. Later he was also prescribed some nasal decongestant drops by the treating doctor, which resulted in some control temporarily. Patient had no CSF rhinorrhoea, had occasional feeling of nasal obstructions more so after the bout of nasal bleed, he had no respiratory problem.
On anterior rhinoscopy examination, turbinates were hypertrophied along with deviated nasal septum toward left side. There was no evidence of any nasal mass or active bleeder.
After about three months, he noticed diminution of vision in right eye which progressed to loss of vision in a month's time. He was referred to us at this stage. There was no headache, vomiting, blurring of vision or any complaints pertaining to endocrinopathy.
Patient was fully conscious with Glasgow Coma Scale (GCS) 15/15. His pulse was 66/min, BP 110/74 mm Hg. There was no vision in right eye. On left side, vision was 6/6 partial. Fundus examination showed bilateral optic atrophy, more in right eye. On examination, there were no clinical features of any endocrine abnormality.
In view of visual deterioration, MRI of brain was done which revealed sellar-suprasellar, solid-cystic mass. The cystic component was predominantly suprasellar and hyperintense on T1 and T2 with peripheral rim enhancement. The solid component was both sellar-suprasellar and isointense on T1and T2 with contrast enhancement. The mass was encasing both cavernous sinuses, extending up to bilateral optic canal, encasing canalicular segment of both optic nerves. It was posteriorly extending into interpeduncular fossa and anteroinferiorly into nasopharynx, posterior nasal cavity, eroding the basisphenoid, clivus and posterior ethmoid and sphenoid sinuses [Figure 1].
Figure 1.
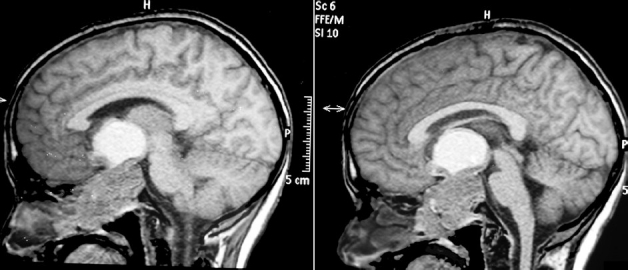
MRI sagital section showing invasive mass in the sellar, suprasellar, and infrasellar regions
His routine investigations included Hb 10.8 gm%, Hct 37.7%, TLC 9000/micL, DLC -P64, L32, E4 M0.,platelets 1.59 lac/micL. Bleeding time was 1.25 min, clotting time 5.10 min, prothrombin time 15.2 s(control 16 s). His hormonal profile included FT3 -1.35(2.0-4.4 pg/ml.), FT4 - 0.40(0.93-1.7 ng/dl.), TSH-7.6(0.27-4.2 mic IU/L). Serum prolactin was 203.7(86-324 mic IU/ml.).Growth hormone was 5.4 ngm/ml(< 7 ngm/ml).
Patient was operated by transcranial route. Right frontotemporal craniotomy and decompression of tumor was achieved via inter-optic and carotico-optic spaces. Tumor was well encapsulated, of variable consistency and highly vascular. Near total decompression was achieved. Child had some bleeding from nose for about two days which settled in due course of time.
In postoperative period, child also had diabetes insipidus which settled in three days. Post operative scan showed near total removal of the tumor.
Histological examination revealed pituitary adenoma which was staining strongly positive for prolactin and negative for TSH, LH, ACTH and somatostatin [Figures 2 and 3].
Figure 2.
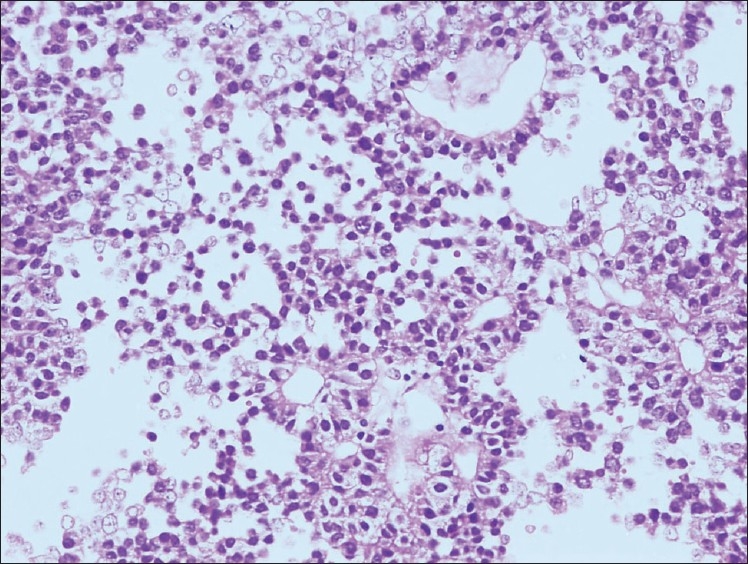
H and E, ×10. Adenoma cells are in sheets with focal glandular arrangement. Nucleus is round to eccentric, monomorphic with salt and pepper appearance. Mitosis/necrosis and sinusoidal arrangement is not seen
Figure 3.
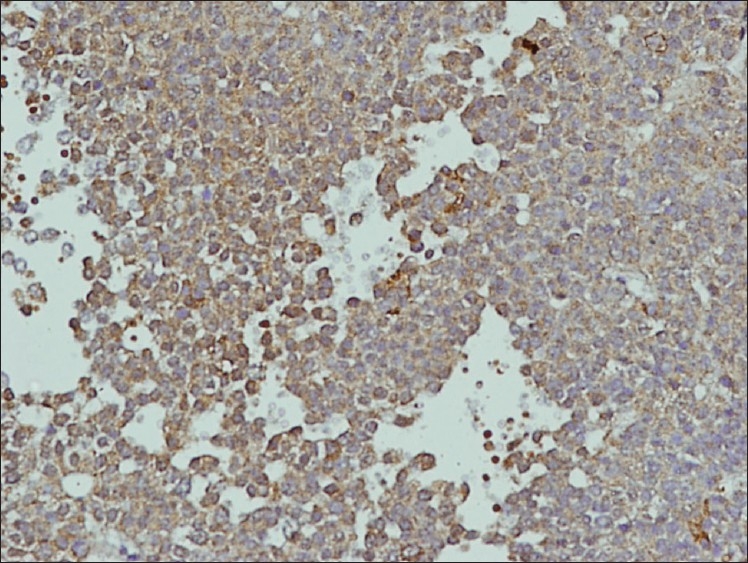
IHC, ×10.Tumor is moderate to intense diffusely positive for antiprolactin antibodies
Discussion
Pituitary adenoma presents with headache, visual deterioration and various kinds of endocrinopathies. Rarely pituitary adenoma can present with epistaxis or apoplexy.[3]
Epistaxis in pituitary adenoma can happen when the patient is on anticoagulants.[3]
Epistaxis in pituitary adenoma can be fatal. The case of a 72-year-old lady has been reported in literature presenting with fatal epistaxis due to rupture of aneurysm enclosed in a large prolactinoma.[4]
Not all invasive tumors present with epistaxis.[5]
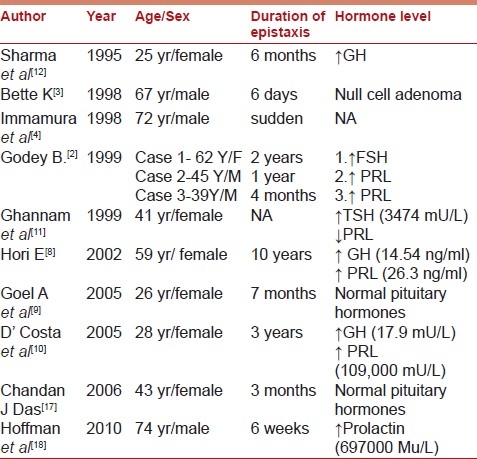
In most of the published literature [Table 1], epistaxis was found to be associated with pituitary macroadenoma and in pituitary adenoma with infrasellar extension into nasopharynx.[2]
Table 1.
The published series of epistaxis and pituitary adenoma with duration of bleed and hormone status
The massive size of the tumor leading to outstripping its blood supply and resulting in hemorrhagic infarction and necrosis of the tumor may also be responsible for epistaxis. The association of epistaxis and apoplexy with pituitary adenoma has also been described which is related to lymphocytic infiltration of pituitary adenoma, suggesting an immune-mediated response.[3]
There are other reports of epistaxis due to ectopic pituitary adenoma which develops from ectopic cell rests that are entrapped along the pathway of craniopharyngeal duct during embryonic development which have aberrantly migrated.[6]
Ectopic pituitary adenoma is generally more aggressive than regular pituitary adenoma.[7]
Epistaxis has also been reported to be associated with adenoma in paranasal sinuses and nasopharynx with empty sella. In such cases, however, pituitary stalk is found to be extending up to floor of the sella.[8]
Epistaxis is more common in invasive pituitary adenoma if they extend into paranasal sinuses.[7]
Epistaxis in a pituitary adenoma should raise the suspicion of a pituitary apoplexy in a giant pituitary adenoma with an infrasellar extension into the nasopharynx.[9]
Epistaxis can present for several months in pituitary adenoma. V D’Costa et al.,[10] have reported a case where pituitary adenoma remained undiagnosed for three years with history of intermittent epistaxis.
There is no specific correlation between epistaxis and staining property of the pituitary adenoma. It has been reported that epistaxis can occur with prolactinoma, growth hormone secreting adenoma and rarely due to co secreting pituitary acidophilic stem cell adenoma.[10]
Other reported causes of epistaxis related to pituitary tumors are an aggressive TSH-secreting adenoma,[11] extensive acidophil-stem-cell adenoma.[10] In patients with acromegaly[12] and another case of rupture of an intratumoral aneurysm enclosed in a large prolactinoma resulting in fatal epistaxis.[4] The pituitary adenoma in our case presented with epistaxis and remained undiagnosed for eight months. Despite the complaint of visual deterioration, the child never had a CT/MRI study of brain. Anterior rhinoscopic examination was essentially normal.
Invasive prolactinoma can have very high levels of prolactin upto 1,000 ng/ml and epistaxis. There may be simultaneous mass effect in the form of compressive optic neuropathy, visual field deficits and ophthalmoplegia.[13,14]
Falsely low serum prolactin level due to hook effect has been reported in giant prolactinoma.[15,16]
The hook effect occurs when excessive antigen is added to a hand held assay (HHA), which then results in false negative. In this assay, the amount of antigen exceeds the finite amount of colloidal gold antibody or the colored labeling material. The excess unlabeled antigen migrates across the membrane more rapidly than the heavier color-labeled antigen, thus saturating or binding all the binding site on the capture antibodies. When the color-labeled antigen arrives, there are no binding sites available and the colored antigen cannot create the colored test line that would produce a positive result. This, in turn, presents the user a false negative result (hook effect) even though high level of the antigen is present.
The pituitary adenoma in our case presented with epistaxis and remained undiagnosed for eight months. Despite the complaint of visual deterioration the child never had a CT/MRI study of brain. Anterior rhinoscopic examination was essentially normal. The pituitary adenoma remained undiagnosed initially and became invasive in about eight month's time.
Pituitary adenoma can also present with epistaxis in children and should be considered as the differential diagnosis along with other uncommon causes. It should be further suspected if there is associated visual loss and in normal anterior rhinoscopy. However, posterior rhinoscopic examination in such cases may pick up the lesion at early stage. Moreover, invasive prolactinoma can have normal prolactin levels due to hook effect.
Treatment of epistaxis with pituitary adenoma is largely symptomatic followed by surgical interventions. For large tumors, there may be some palliative role of chemotherapy or hormone therapy particularly in hormone secreting adenomas. It can be used both pre-op to reduce the size of lesion or post-op for residual lesions.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Cohen ZR, Marmor E, Fuller GN, DeMonte F. Misdiagnosis of olfactory neuroblastoma. Neurosurg Focus. 2002;15(12):e3. doi: 10.3171/foc.2002.12.5.4. [DOI] [PubMed] [Google Scholar]
- 2.Godey B, Morandi X, Le Gall F, Feat S, Brassier G, Le Clech G. Pituitary adenomas with infra-sellar extension into the nasopharynx. J Laryngol Otol. 1999;113:1109–11. doi: 10.1017/s0022215100158037. [DOI] [PubMed] [Google Scholar]
- 3.Kleinschmidt-Demasters BK, Lillehei KO. Pathological correlates of pituitary adenomas presenting with apoplexy. Hum Pathol. 1998;29:1255–65. doi: 10.1016/s0046-8177(98)90254-4. [DOI] [PubMed] [Google Scholar]
- 4.Imamura J, Okuzono T, Okuzono Y. Fatal epistaxis caused by rupture of an intratumoral aneurysm enclosed by a large prolactinoma–Case report. Neurol Med Chir (Tokyo) 1998;38:654–6. doi: 10.2176/nmc.38.654. [DOI] [PubMed] [Google Scholar]
- 5.Molitch ME. Prolactin-secreting tumors: What's new? Expert Rev Anticancer Ther. 2006;6(Suppl 9):S29–35. doi: 10.1586/14737140.6.9s.S29. [DOI] [PubMed] [Google Scholar]
- 6.Hori A. Suprasellarperi-infundibular ectopic adenohypophysis in fetal and adult brains. J Neurosurg. 1985;63:113–5. doi: 10.3171/jns.1985.63.1.0113. [DOI] [PubMed] [Google Scholar]
- 7.Luk IS, Chan JK, Chow SM, Leung S. Pituitary adenoma presenting as sinonasal tumor: Pitfalls in diagnosis. Hum Pathol. 1996;27:605–9. doi: 10.1016/s0046-8177(96)90170-7. [DOI] [PubMed] [Google Scholar]
- 8.Hori E, Akai T, Kurimoto M, Hirashima Y, Endo S. Growth hormonesecreting pituitary adenoma confined to the sphenoid sinus associated with a normal-sized empty sella. J Clin Neurosci. 2002;9:196–9. doi: 10.1054/jocn.2001.0988. [DOI] [PubMed] [Google Scholar]
- 9.Goel A, Phalke U, Cacciola F, Muzumdar DP. Giant pituitary adenoma invading the clivus. Neurol India. 2005;53:105–7. doi: 10.4103/0028-3886.15073. [DOI] [PubMed] [Google Scholar]
- 10.D’Costa RV, Kalk WJ. Bromocriptine-sensitive acidophil-stem-cell adenoma co-secreting growth hormone and prolactin - A case report. Endocrine Abstracts. 2005;9:198. [Google Scholar]
- 11.Ghannam NN, Hammami MM, Muttair Z, Bakheet SM. Primary hypothyroidism-associated TSH-secreting pituitary adenoma/ hyperplasia presenting as a bleeding nasal mass and extremely elevated TSH level. J Endocrinol Invest. 1999;22:419–23. doi: 10.1007/BF03343584. [DOI] [PubMed] [Google Scholar]
- 12.Sharma K, Tyagi I, Banerji D, Chhabra DK. Intranasal Pituitary adenoma with epistaxis in an Acromegaly – An unusual presentation. Indian J Otol Head Neck Surg. 1995;47:25–7. [Google Scholar]
- 13.Murphy FY, Vesely DL, Jordan RM, Flanigan S, Kohler PO. Giant invasive prolactinomas. Am J Med. 1987;83:995–1002. doi: 10.1016/0002-9343(87)90668-1. [DOI] [PubMed] [Google Scholar]
- 14.Batchelet AR. Wills eye resident case series. Rev Ophthalmol. 2010;17:90. [Google Scholar]
- 15.Barkan AL, Chandler WF. Giant pituitary prolactinoma with falsely low serum prolactin: The pitfall of high-dose hook effect”: Case report. Neurosurgery. 1998;42:913–5. doi: 10.1097/00006123-199804000-00126. discussion 915-6. [DOI] [PubMed] [Google Scholar]
- 16.Petakov MS, Damjanović SS, Nikolić-Durović MM, Dragojlović ZL, Obradović S, Gligorović MS, et al. Pituitary adenomas secreting large amounts of prolactin may give false low values in immunoradiometric assays. The hook effect. J Endocrinol Invest. 1998;21:184–8. doi: 10.1007/BF03347299. [DOI] [PubMed] [Google Scholar]
- 17.Das CJ, Seith A, Gamangati S, Goswami R. Ectopic pituitary adenoma with an empty sella. AJR Am J Roentgenol. 2006;186:1468–9. doi: 10.2214/AJR.05.0329. [DOI] [PubMed] [Google Scholar]
- 18.Hofman R, Franken AA, Rosingh HJ. Just epistaxis? Neth J Med. 2010;68:227–8. [PubMed] [Google Scholar]


