Abstract
Jarcho–Levin syndrome (JLS) is a type of segmental costovertebral malformation. It is a congenital disorder characterized by a variety of vertebral and costal anomalies. Only four cases of Jarcho–Levin syndrome with diastematomyelia have been reported in the literature. We report the fifth case of Jarcho–Levin syndrome with diastematomyelia and review the literature. A one-and-half-year-old male child born of full-term normal delivery was brought with complaints of progressively increasing weakness in lower limbs with inability to stand since 1 month. Radiological examination revealed irregular fusion of ribs, spina bifida, and diastematomyelia at L2–L3 vertebral level. The patient underwent L1 to L3 laminectomy. A large bony spur was identified and excised with microrongeurs. Spondylocostal dysplasia may be associated with diastematomyelia or other surgically correctable occult intraspinal anomalies which may be diagnosed in early asymptomatic stage by magnetic resonance image screening of spine.
Keywords: Costovertebral malformation, diastematomyelia, Jarcho–Levin syndrome, spondylocostal dysostosis, spondylothoracic dysostosis
Introduction
Jarcho–Levin syndrome is an eponym that represents a spectrum of short-trunk skeletal dysplasias with variable involvement of the vertebrae and ribs. Other abnormalities have also been described in Jarcho–Levin syndrome, including neural tube defects, Arnold–Chiari malformation, renal/urinary tract abnormalities, hydrocephalus, hydroureteronephrosis, and meningomyelocoele.[1–3] Malformations of the spinal cord with a separation into two hemicords have been termed “diastematomyelia.” Only four cases of Jarcho–Levin syndrome with diastematomyelia have been reported in the literature. We report the fifth case of Jarcho–Levin syndrome with diastematomyelia.
Case Report
A one-and-half-year-old male child born of full-term normal delivery after a nonconsanguineous marriage was brought by his mother with complaints of progressively increasing weakness in lower limbs with inability to stand since 1 month. On examination, the child was found to be conscious, alert, and active. Neurological examination revealed grade 4 power in the left lower limb. Local examination revealed a lipomatous swelling in the lumbar region. The patient also had a congenital groove at the left costal margin which was not investigated at birth. Chest x0 -ray revealed irregular fusion of left sided ribs and scoliosis of thoracolumbar spine [Figure 1]. Magnetic resonance imaging and computerized tomography of the spine were done which revealed spina bifida defect at multiple levels in lumbosacral region. There was evidence of diastematomyelia with a large intraspinal bony bar at L2–L3 vertebral level. The two hemicords were asymmetric; left smaller than right and each hemicord was seen in a separate dural sac [Figures 2 and 3]. Tip of conus medullaris was low in position at L4 vertebral level. The patient underwent L1 to L3 laminectomy. A large bony spur was identified on the left side which was dividing the spinal canal into two parts. Two dural sacs were identified which were separated by the bony spur. The right dural tube was larger than the left. The spur was excised with microrongeurs till it was flush with the vertebral body. The dura was then opened and the two hemicords were converted into one sac. The patient had no added neurological deficit postoperatively. The patient has been on follow-up since the last 3 years, but remains unable to walk without support.
Figure 1.

Chest x-ray showing irregular fusion of left sided ribs and scoliosis of thoracolumbar spine
Figure 2.
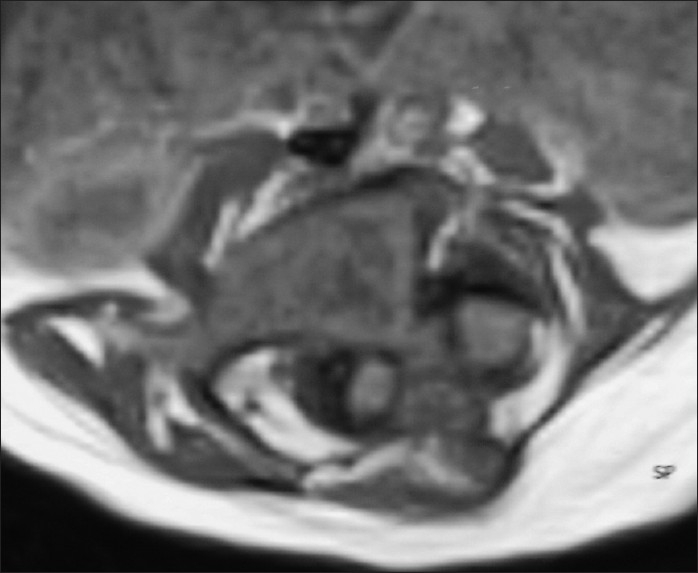
Magnetic resonance imaging of the spine axial section showing evidence of diastematomyelia with a large intraspinal spur at L2–L3 vertebral level. The two hemicords were asymmetric; left one smaller than right and each hemicord was seen in a separate dural sac
Figure 3.

Computerized tomography of the spine showing diastematomyelia with a large intraspinal bony bar at L2–L3 vertebral level
Discussion
Jarcho–Levin syndrome (JLS), also known as spondylothoracic dysostosis (STD)/spondylocostal dysostosis (SCD), is a type of segmental costovertebral malformation. Solomom et al. classified cases of JLS into two groups – Spondylo costal dysostosis (SCD) and Spondylothoracic dysostosis (STD), based on the presence or absence of rib malformations. Individuals with SCD had vertebral anomalies, intrinsic rib malformation (broadening, bifurcation, abnormal orientation, and fusion), and flaring of iliac bones. Cases with STD had vertebral anomalies and a “fanlike” rib configuration but no intrinsic rib malformation.[4]
Mutations in the genes that are important components of the notch signaling pathway (gene DLL3 on chromosome 19 and MESP2 gene) are responsible for the development of spondylocostal dysostosis (costovertebral malformation) in Jarcho–Levin syndrome. According to Dias and Walker, split cord malformations and related malformations occur as a result of embryological failure of midline axial integration during gastrulation.[5]
Jarcho–Levin syndrome is characterized by a short and rigid neck, short thorax, protuberant abdomen, and inguinal and umbilical hernias. Vertebral and rib malformations are the major features. They present with multiple vertebral anomalies at different levels of the spine, including “butterfly vertebrae,” hemivertebrae, and fused hypoplastic vertebrae. Reported findings associated with Jarcho–Levin syndrome include congenital heart defects, abdominal wall malformations, genitourinary malformations, upper limb anomalies, neural tube defects and congenital diaphragmatic hernia.[6] Radiologically, the “crab-like” appearance of the thoracic cage on AP projection is characteristic of STD.[3] The prognosis is directly related to respiratory complications.
Neural tube defects (NTDs) like spina bifida, meningocele, meningomyelocoele, lipomyelomeningocele, and diastematomyelia have been reported to be associated with Jarcho–Levin syndrome.[7–9] Spina bifida appears to be a common finding in reported Jarcho–Levin syndrome cases.[2,7–9] Spina bifida is present in 25% of patients with Jarcho–Levin syndrome.[10] In 1991, Karnes et al. suggested that individuals with vertebral and rib malformations with the absence of fan like chest configurations are more often short statured, have almost double the survival rate, are less likely to have neural tube defects (spina bifida), and may inherit the disorder in autosomal recessive or autosomal dominant pattern. Individuals with a fanlike rib configuration and posterior tethering characteristic of STD have a higher mortality rate and a higher incidence of neural tube defects, and inherit the disorder in an autosomal recessive manner.[11]
In cases of congenital segmental costovertebral malformations with neural tube defects, cases with type I split cord malformation are quite rare.[6] Malformations of the spinal cord with a separation into two hemicords have been termed “diastematomyelia.” The term “diplomyelia” is reserved as a true duplication of the spinal cord which is, however, difficult to demonstrate. In 1992, Pang et al. recommended the term “split cord malformation” for all double spinal cords. A type I split cord malformation consists of two hemicords, each contained within its own dural tube and separated by a dura-sheathed rigid osseocartilaginous median septum. A type II split cord malformation consists of two hemicords housed in a single dural tube separated by a nonrigid, fibrous median septum.[12]
Till date four cases of diastematomyelia in patients with Jarcho–Levin syndrome have been reported.[2,8,9,13] In 1976, Elier JL and Morton JM first reported a case in which diastematomyelia occurred in association with findings characteristic of the Jarcho–Levin syndrome in an infant born to a woman who abused lysergic acid diethylamide during pregnancy.[13] Reyes et al. in 1989 reported a case of Jarcho–Levin syndrome associated with diastematomyelia (type I split cord malformation) and claimed that neurological abnormalities should be considered a component of the Jarcho–Levin syndrome.[2] Giacoia GP and Say B in 1991 described a patient with the Jarcho–Levin syndrome who also had spina bifida and diastematomyelia (type I split cord malformation) and suggested that this association is not coincidental and may be aetiologically related.[9] Etus et al. in 2003 reported a case of Jarcho–Levin syndrome with diastematomyelia (type I split cord malformation) in a 7-year-old girl.[8]
Conclusion
Physicians and surgeons must be aware that spondylocostal dysplasia may be associated with diastematomyelia or other surgically correctable occult intraspinal anomalies which may be diagnosed in asymptomatic stage by magnetic resonance image screening of spine, because late diagnosis might have unsatisfactory outcome.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kulkarni ML, Navaz SR, Vani HN, Manjunath KS, Matani D. Jarcho-Levin syndrome. Indian J Pediatr. 2006;73:245–7. doi: 10.1007/BF02825493. [DOI] [PubMed] [Google Scholar]
- 2.Reyes MG, Morales A, Harris V, Barreta TM, Goldbarg H. Neural defects in Jarcho-Levin syndrome. J Child Neurol. 1989;4:51–4. doi: 10.1177/088307388900400109. [DOI] [PubMed] [Google Scholar]
- 3.Young S, Reyes MG, Uzoaru IL, Harris V. Arnold-Chiari malformation in Jarcho-Levin syndrome. J Child Neurol. 1989;4:229–30. doi: 10.1177/088307388900400318. [DOI] [PubMed] [Google Scholar]
- 4.Solomon L, Jimenez RB, Reiner L. Spondylothoracic dysostosis: Report of two cases and review of the literature. Arch Pathol Lab Med. 1978;102:201–5. [PubMed] [Google Scholar]
- 5.Dias MS, Walker ML. The embryogenesis of complex dysraphic malformations: A disorder of gastrulation? Pediatr Neurosurg. 1992;18:229–53. doi: 10.1159/000120670. [DOI] [PubMed] [Google Scholar]
- 6.Onay OS, Kinik ST, Otgün Y, Arda IS, Varan B. Jarcho-Levin syndrome presenting with diaphragmatic hernia. Eur J Pediatr Surg. 2008;18:272–4. doi: 10.1055/s-2008-1038364. [DOI] [PubMed] [Google Scholar]
- 7.Dane B, Dane C, Aksoy F, Cetin A, Yayla M. Jarcho-Levin syndrome presenting as neural tube defect: Report of four cases and pitfalls of diagnosis. Fetal Diagn Ther. 2007;22:416–9. doi: 10.1159/000106345. [DOI] [PubMed] [Google Scholar]
- 8.Etus V, Ceylan S, Ceylan S. Association of spondylocostal dysostosis and type I split cord malformation. Neurol Sci. 2003;24:134–7. doi: 10.1007/s10072-003-0099-x. [DOI] [PubMed] [Google Scholar]
- 9.Giacoia GP, Say B. Spondylocostal dysplasia and neural tube defects. J Med Genet. 1991;28:51–3. doi: 10.1136/jmg.28.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell RM., Jr . In: NORD Guide to Rare Disorders. The National Organization for Rare Disorders. Philadelphia: Lippincott Williams and Wilkins; 2003. Jarcho-Levin syndrome; pp. 207–8. [Google Scholar]
- 11.Karnes PS, Day D, Berry SA, Pierpont ME. Jarcho-Levin syndrome: Four new cases and classification of subtypes. Am J Med Genet. 1991;40:264–70. doi: 10.1002/ajmg.1320400304. [DOI] [PubMed] [Google Scholar]
- 12.Pang D, Dias MS, Ahab-Barmada M. Split cord malformation. Part I: A unified theory of embryogenesis for double spinal cord malformations. Neurosurgery. 1992;31:451–80. doi: 10.1227/00006123-199209000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Elier JL, Morton JM. Bizarre deformities in offspring of user of lysergic acid diethylamide. N Engl J Med. 1976;283:395–7. doi: 10.1056/NEJM197008202830803. [DOI] [PubMed] [Google Scholar]


