Abstract
Background. There is an increasing need for programmatic prevention of cardiometabolic diseases (cardiovascular disease, type 2 diabetes and chronic kidney disease). Therefore, in the Netherlands, a prevention programme linked to primary care has been developed. This initiative was supported by the national professional organizations of GPs and occupational physicians as well as three large health foundations.
Objectives. To describe and discuss the content, structure of and first experiences with this initiative.
Methods. Description of context, risk assessment tool, guideline, content of the Prevention Consultation and pilot studies.
Results. Preceding surveys revealed a need for proactive disease prevention, linked to primary care. An evidence-based guideline was developed using a validated eight-question screening list. According to the guideline, high-risk participants were advised to attend two consultations at the general practice, for completing the risk assessment and for tailored advice. Three pilot studies revealed that the programme was feasible and that (sufficient) participants with a condition requiring treatment were detected. We learned that with a ‘passive’ recruitment (with only posters and brochures), screening uptake is limited. A more active approach with a personal invitation from the GP is more effective. Both an Internet as written questionnaire should be available and reminders are necessary. The need for a consultation with the GP practice after a high-risk test result should be emphasized. The first consultation can be performed by a practice nurse.
Conclusions. A national systematic screening programme for cardiometabolic diseases linked to primary care is feasible. The cost-effectiveness still has to be established.
Keywords: Cardiovascular disease, diabetes, hypertension, kidney disease, prevention, primary care, screening, the Netherlands
Introduction
Cardiovascular diseases (CVDs), type 2 diabetes (DM2) and chronic kidney diseases (CKDs) are three of the most common and most burdensome chronic diseases in the western world.1 For this reason, prevention of these diseases receives increasing attention. Primary care plays an important role in this.2
In this article, we want to share the experiences in the Netherlands with an evidence-based integrated approach to prevention, which is well embedded in regular primary health care. We felt the need for this initiative because over the past years the Dutch government, not-for-profit organizations and for-profit companies had set up various initiatives to make the public aware of the importance to assess their risk profile and to encourage people at risk to take action in order to prevent these diseases.
Although all these initiatives worked towards the same goal, namely the early detection of risk factors and appropriate interventions, several threats could be identified:
The diversity in health checks, screening tools and interventions was confusing for the general public.
The quality of the available health checks was sometimes questionable; at the same time, lay persons may not have the knowledge to distinguish the better quality checks from the lesser quality checks.
Health professionals lacked sufficient skills and know-ledge for detecting and managing high-risk patients.
People who were identified as ‘at risk’ often did not know where to go next and what to do to reduce their risk.3 A follow-up in regular health care was not arranged properly or not at all.
To contribute to similar initiatives in other countries, we will discuss the development of a guideline, lessons learned from the pilot studies and challenges in further implementation and research.
Background and content of the evidence-based guideline
In the Netherlands, the above-mentioned threats drove the need for an evidence-based integrated approach to prevention, which is well embedded in regular health care. We chose for a single strategy for the prevention and early detection of CVD, DM2 and CKD since the link between CVD and DM2 has been well documented and both CVD and DM2 play a role in the aetiology of CKD. Furthermore, all the three diseases have similar determinants for development and progression of these diseases. In many cases, these can be prevented or delayed by a healthy lifestyle consisting of sufficient physical activity, a healthy diet and smoking cessation.
In the Netherlands, several recent surveys indicated that screening for cardiometabolic disorders could be more efficient and acceptable when it is embedded in the health care setting.4,5 In the Netherlands, the GP plays an important role in preventing CVD, type2 diabetes mellitus and kidney disease6 since (i) all Dutch inhabitants are registered obligatory with a general practice and ∼75% visit their GP at least once a year; (ii) GPs keep electronic medical records of all listed patients and (iii) patients highly trust their GP.3,6 In addition, Dutch GPs have successfully been involved in other prevention programmes, such as influenza vaccination and cervical cancer screening. A recent survey showed that Dutch GPs have a positive attitude towards integrated primary prevention of cardiometabolic diseases and they consider general practice the right care setting for detecting and treating patients at risk for these diseases.7
Therefore, the Dutch College of General Practitioners (NHG), the Dutch National Association of General Practitioners (LHV) and the Netherlands Society of Occupational Medicine (NVAB) together with three health foundations (Netherlands Heart Foundation, Dutch Diabetes Research Foundation and Dutch Kidney Foundation) developed an evidence-based guideline [PreventieConsult (PreventionConsultation) cardio-metabolic risk (CMR)] to improve the early detection and management of patients with an increased risk for CVD, DM2 and CKD.8,9
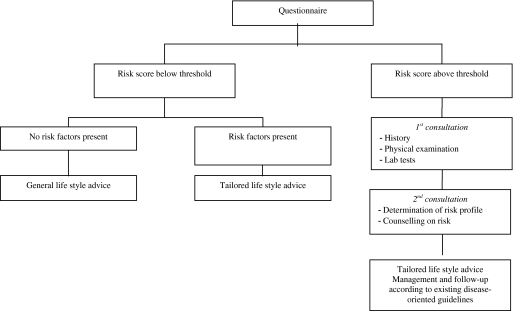
The guideline PreventieConsult CMR was published in its definite form in 2011, after being piloted. The guideline was validated by an authorizing committee of experts, after an external review procedure among external experts and practicing GPs. It was developed to improve the early detection and treatment of persons with an increased risk for cardiometabolic disorders (CVD, DM2 and CKD). All individuals between 45 and 70 years of age without known cardiometabolic diseases and who do not use anti-hypertensive or lipid-lowering treatment are eligible for the PreventieConsult CMR (for certain ethnic groups of South Asian origin the lower age limit is set at 35 years).10 The PreventieConsult CMR is based on current evidence regarding cardiometabolic risk estimation and includes a stepwise approach (Fig. 1). Based on a risk estimation (first step), patients with a high-risk score are referred to the general practice (second step).
FIGURE 1.
Design PreventieConsult CMR8
First step: risk estimation
The first step of the PreventieConsult CMR is an integrated risk estimation for the three cardiometabolic diseases.8,9 This risk estimation has specifically been developed for persons who have not yet been diagnosed with any of these diseases nor with a treatable risk factor (e.g. hypertension or hypercholesterolaemia) and is therefore specifically suitable for prevention in the general public or high-risk groups. The risk estimation contains elements from the SCORE risk function11 and the already validated FINDRISK questionnaire.12 The eight items that can be filled out by self-report are age, gender, body mass index (BMI), waist circumference, current smoking, family history of myocardial infarction or stroke and family history of type 2 diabetes mellitus.9 Scores per item are gender specific and the sum score indicates the total risk estimation. The risk score was developed in a merged dataset of three population-based cohorts from different Netherlands regions8,9 (see also M Alssema, RS Newson, SJL Bakker et al., unpublished work). The predicted outcome is the incidence of any cardiometabolic disease. Based on the sum score, participants are categorized as having a below or above threshold risk for a cardiometabolic disease8,9 (see also M Alssema, RS Newson, SJL Bakker et al., unpublished work). Persons with a normal risk score (below the threshold) receive a general or tailored lifestyle advice, based on the present risk factors (Fig. 1). Persons with a high-risk score (above the threshold) are advised to visit their GP for the second step of the PreventieConsult CMR.
Second step: follow-up of high risk at the general practice
In the second step of the PreventieConsult CMR, persons estimated as having a high-risk score according to the risk estimation are advised to visit their general practice for two prevention consultations with a GP or practice nurse (PN). During these consultations, the complete risk profile will be assessed and follow-up actions will be discussed. The risk profile includes the assessments of serum cholesterol ratio (total cholesterol and high-density lipoprotein), glucose level and blood pressure measurements in order to estimate the 10-year risk on cardiovascular mortality11 and/or to establish a diagnosis of diabetes. Follow-up actions usually include lifestyle advice and/or starting with (preventive) drug treatment (e.g. lipid-lowering drugs). In the guideline, the local availability of a variety of evidence-based lifestyle programmes is considered an essential requirement for initiating the PreventionConsultation. At present, many local and nationwide integrated lifestyle programmes have been developed, such as the Beweegkuur (exercise on prescription) and smoking cessation programmes. We ensured that the inclusion criteria for these programmes are identical to the indications derived from the PreventieConsult. In additions to specific programmes, persons can also be referred to physiotherapists for exercise programmes and/or dieticians for dietary advice.
Pilot studies: findings and adaptations made
To test the feasibility of the PreventieConsult CMR in a general practice setting, three pilots have been conducted.
Pilot 1: Nielen et al.
In 2009, the PreventieConsult CMR was piloted in 16 general practices.13 Patients between 45 and 70 years of age without known cardiometabolic disorders were invited to fill in an online questionnaire, which resulted in a low-, medium- or high-risk scores for cardiometabolic diseases (only after this pilot, the score was dichotomized). Half of the participating practices invited patients with a personal letter. In the other practices, patients were invited via leaflets and posters in the waiting room. The response rates to the invitation letter (active approach) and posters and leaflets (passive approach) were 33% and 1%, respectively. Initially, the response was low and slow, but this increased after a reminder letter from the GP. In total, 617 patients completed the online risk questionnaire, of which 392 persons (64%) had a high-risk score for cardiometabolic diseases. This resulted in 142 (36%) patients visiting their GP. In 28 of these patients (20%), one or more CVDs, DM2, CKD or risk factors for these (like hypertension or hypercholesterolaemia) were detected.13 The online risk estimation questionnaire identified 21% as current smokers (129 of 617) and overweight (BMI > 25) in 53% (327 of 617). A questionnaire to a random sample of non-responders showed that concerns about privacy was the most frequently mentioned reason for non-participation. The invitation or participation did not increase anxiety. Of the non-participants, 24% reported to have limited access to Internet (versus 11% of participants).
The pilot study also addressed the experiences and attitudes of the practice staff. Almost 90% of the participating GPs and PNs stated that the general practice is a suitable place for prevention activities as recommended in the PreventieConsult CMR guideline. Eighty-nine per cent of the GPs and PNs were of the opinion that these preventive activities can very well be done by the PNs.13 The participating practices reported that the first consultation was performed by either the PN or the GP and took on average 24 and 14 minutes, respectively. The average duration of the second consultation (always with the GP) took 14 minutes.
Two other pilot
Van de Kerkhof et al.14 and Klomp et al.15 used other age limits and invited patients aged 40–75 years (1704 and 2529 patients, respectively). Another difference was the availability of a written version of the questionnaire. Most findings were similar to those of Nielen et al.13 However, the response to the questionnaire was higher, namely 69%14 and 75%15, respectively. Based on the information provided, respectively, 55%14 and 29%15 were invited for an additional personal examination. Similar to the study from Nielen et al.,13 in both pilots one in one of five attenders, a condition was diagnosed that needed either treatment or follow-up according to the prevailing guidelines for a cardiometabolic condition.
Improvements based on the pilot studies
From these pilots, we learned that the guideline can be implemented in general practice. However, some minor adjustment had to be made. Inviting people to participate by sending a personal letter is much more effective than simply putting up a poster and having leaflets available at the practice. Furthermore, because age is such an important risk factor, it is justifiable to invite all patients over the age of 60 years (men) and 65 years (women) for a consultation without completing the questionnaire. The response rate to the invitation can be increased by also having a written questionnaire available. This may also address the privacy concerns people may have with an online questionnaire. Finally, more efforts should be invested to convince people with a high-risk score (above the threshold to go for follow-up with their GP) to actually seek advice from their GP.
Further implementation
In 2011, further implementation of the PreventieConsult CMR in general practice will take place. This should consist of supporting health professionals in providing the services stated in the guideline as well as making the general public aware of the possibility to take part in an integrated evidence-based health check in general practice.
Professionals
In March 2011, the guideline has been published.8 The Dutch GPs already have 90 guidelines covering 70% of the workload. Since the PreventieConsult CMR has the format of such a guideline, it makes use of all related quality aspects, such as supporting implementation materials, and uptake in the yearly updated guideline book.
In addition to this, other professional organizations will be involved in the wider implementation of the recommendations of the guideline. As a first step, the Dutch occupational physicians are planning a pilot in occupational health. On top of that, other professional organizations or groups like community nurses, pharmacists, physiotherapists and dieticians have shown an interest in taking part in the wider implementation. Also, commercial providers of health checks have offered to replace their module on cardiometabolic diseases by the PreventieConsult CMR.
We advocate the principles behind the PreventieConsult. This means that only persons not in care yet for the index diseases should be invited. In addition, good arrangements for referral (to the general practice) and lifestyle advice should be available and formalized. Finally, the PreventieConsult CMR is not a one-time initiative. Therefore, the provider should be willing to make longer term arrangements for follow-up and repeated invitations.
When GPs chose for inviting persons, we advise to invite the eligible population in small age cohorts. This enables efficient planning and facilitates an easier reinvitation for the non-responders. However, GPs are free to chose their approach and some GP practices will prefer to start with the passive approach. Since we do not have definite proof of cost-effectiveness of either of the approaches, the policy for invitation will be up to the practices themselves.
Public
The Dutch population is very interested in a reliable health check (as a result of the collaborative initiative from the six parties), especially offered by a health care professional such as the GP.3
The three Dutch health funds involved in the development of the PreventieConsult CMR will play a major role in making the public aware of the PreventieConsult and to encourage the people to complete the risk questionnaire by way of their means of communication. Together with the launch of the guideline for professionals, a user-friendly website for the general public has been launched. In addition to the risk estimation, this website provides tailored lifestyle advice especially for those people who, because of their risk estimate, are not recommended to seek advice from their GP (www.testuwleefstijl.nl).
Challenges
The PreventieConsult CMR is a nationwide integrated evidence-based preventive programme for cardiometabolic disease. It has been designed on the cutting edge between public health and primary care. Bridging these two worlds is not easy2 but considered as the only way to effectively deal with the increasing burden of lifestyle-related chronic disease.1
Adequate reimbursement of the participating professionals seems to be an essential factor for further implementation. Many of them do not yet consider this type of active life style-oriented prevention a role for the care providers,16 while the workload implications of such programmes are substantial.17 For the acceptance on the longer term, a parallel cost-effectiveness study is planned, which also enables us to make adaptations on aspects that are not sufficiently (cost-)effective.
In addition, proper collaboration between primary care and public health is essential for the longer term containment of the programme. It is important to reach the lower socio-economic groups and the ethnic minorities, who we know suffer more frequently from CVD, DM2 or CKD. Some will argue that screening on cardiometabolic diseases will only widen health inequalities.18 In general, this is true. However, because of the frequent contacts, high confidence and the low threshold primary care can play an important role in minimizing this gap.19,20 Primary care then acts as a part of a selective prevention approach, which requires a local community orientation.21 Besides professionals, the Municipal health services and the municipalities themselves also play an important role in creating an intersectoral community action for health.1,2,20
The success of the programme will not be determined by the identification of subjects at high risk only. Some will argue that the focus needs to be on detecting early stages of disease itself instead of focussing on risk factors.22 However, at present, there is still insufficient evidence for that.23 Although some screen positives will in the end need and profit from medication, the main focus should be on risk factors and lifestyle adaptation, which needs a concerted approach between primary care and public health.1,2,20
With the PreventieConsult CMR, we were able to establish a comprehensive national prevention initiative focussed on one of the largest disease groups in the western world. All parties involved (professionals, health funds, patient organizations, municipal health services, municipalities, health insurance companies, national health bodies, commercial providers, etc.) will have to take their own responsibility in the implementation of this guideline and by doing so make a difference to the health of many people. However, some important issues still need to be addressed. The evidence for cost-effectiveness of the whole approach (one of the criteria of Wilson and Jungner) is still lacking. Specific approaches to vulnerable groups (ethnic minorities and lower socio-economic status) need to be developed, aimed at improving participation as well as increasing compliance to advice. There is a need for evidence-based approaches for community-oriented collaboration between primary care and public health.
Declaration
Funding: Pilot study 113 was funded by a grant from the Netherlands Organization for Health Research and Development (ZonMw; 120720013). The funder had no role in the study design or in the collection, analysis, interpretation and reporting of data.
Ethical approval: none.
Conflict of interest: MMJN, VvdM and FGS were involved in pilot study 1.13 WJJA was chairman and MvV and AJMD were members of the steering committee of the PreventieConsult.
References
- 1.Anonymous . 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases: Prevent and Control Cardiovascular Diseases, Cancers, Chronic Respiratory Diseases and Diabetes. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 2.Martin-Misener R, Valaitis R. A Scoping Literature Review of Collaboration between Primary Care and Public Health. A Report to the Canadian Health Services Research Foundation. Hamilton, New Zealand: Strengthening Primary Health care through Primary Care and Public Health collaboration; 2009. [DOI] [PubMed] [Google Scholar]
- 3.Gelissen R, Jonkers R. Nulmeting Gezondheidscheck CMR. Uitkomsten van onderzoek onder de Nederlandse bevolking van 45-74 jaar in nhet kader van het project Checkstandaard Cardiometabool risico. Amsterdam, The Netherlands: Rescon; 2009. www.lekkerlangleven.nl/l/library/download/2113. (accessed on 5 December 2011) [Google Scholar]
- 4.Nielen MM, Schellevis FG, Verheij RA. The usefulness of a free self-test for screening albuminuria in the general population: a cross-sectional survey. BMC Public Health 2009; 9: 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Jongh D, van Dijk L, Schellevis FG. Vroege opsporing en behandeling van mensen met risicofactoren voor hart—en vaatziekten. Evaluatie van initiatieven. Utrecht, The Netherlands: NIVEL; 2007. [Google Scholar]
- 6.Drenthen AJM, Assendelft WJJ, Van der Velden J. Preventie in de huisartsenpraktijk: kom in beweging. Huisarts Wet. 2008;29(S1):126–131. [Google Scholar]
- 7.Nielen MM, Assendelft WJ, Drenthen AJ, et al. Primary prevention of cardio-metabolic diseases in general practice: a Dutch survey of attitudes and working methods of general practitioners. Eur J Gen Pract. 2010;16:139–42. doi: 10.3109/13814788.2010.501372. [DOI] [PubMed] [Google Scholar]
- 8.Dekker JM, Alssema M, Janssen PGH, et al. NHG-Standaard ‘Het PreventieConsult’ Module Cardiometabool. Huisarts en Wetenschap. 2011;55:138–55. [Google Scholar]
- 9.Dekker JM, Alssema M, Janssen PG, Goudswaard LN. Samenvatting van de standaard ‘Het preventieconsult’ van het Nederlands Huisartsen Genootschap. Ned Tijdschr Geneeskd. 2011;155:A3428. [PubMed] [Google Scholar]
- 10.Middelkoop BJ, Kesarlal-Sadhoeram SM, Ramsaransing GN, Struben HW. Diabetes mellitus among South Asian inhabitants of The Hague: high prevalence and an age-specific socioeconomic gradient. Int J Epidemiol. 1999;28:1119–23. doi: 10.1093/ije/28.6.1119. [DOI] [PubMed] [Google Scholar]
- 11.Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur J Cardiovasc Prev Rehabil. 2007;14(suppl 2):S1–113. doi: 10.1097/01.hjr.0000277983.23934.c9. [DOI] [PubMed] [Google Scholar]
- 12.Lindstrom J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26:725–31. doi: 10.2337/diacare.26.3.725. [DOI] [PubMed] [Google Scholar]
- 13.Nielen MMJ, Van der Meer V, Assendelft WJJ, Schellevis FG. Eerste ervaringen met het PreventieConsult Cardiometabool risico. Huisarts Wet. 2011;54:414–9. [Google Scholar]
- 14.Godefrooij MB, van de Kerkhof RM, Wouda PJ, et al. Identification of risk factors in primary care: development, implementation and yield of a cardiometabolic health check. Fam Pract. 2011 doi: 10.1093/fampra/cmr068. September 9 [Epub ahead of print]. doi:10.1093/fampra/cmr068. [DOI] [PubMed] [Google Scholar]
- 15.Klomp M, Meulepas M, Anema B, Harms L. PreventieConsult in praktijk: een pilot. Medisch Contact. 2011;66:659–61. [Google Scholar]
- 16.Jochemsen-van der Leeuw HG, van Dijk N, Wieringa-de Waard M. Attitudes towards obesity treatment in GP training practices: a focus group study. Fam Pract. 2011;28:42–9. doi: 10.1093/fampra/cmq110. [DOI] [PubMed] [Google Scholar]
- 17.Dalton AR, Bottle A, Okoro C, Majeed A, Millett C. Implementation of the NHS Health Checks programme: baseline assessment of risk factor recording in an urban culturally diverse setting. Fam Pract. 2011;28:34–40. doi: 10.1093/fampra/cmq068. [DOI] [PubMed] [Google Scholar]
- 18.Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Med. 2010;7:e1000320. doi: 10.1371/journal.pmed.1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kant AC, Palm BT, Wentink E, van Weel C. General practitioner based screening for cervical cancer: higher participation of women with a higher risk? J Med Screen. 1997;4:35–9. doi: 10.1177/096914139700400111. [DOI] [PubMed] [Google Scholar]
- 20.Hiddink GJ, Hautvast JGAJ, Van Woerkum CMJ, Fieren CJ, Van ’t Hof MA. Consumers’ expectations about nutrition guidance: the importance of primary-care physicians. Am J Clin Nutr. 1997;65(suppl):1974S–9S. doi: 10.1093/ajcn/65.6.1974S. [DOI] [PubMed] [Google Scholar]
- 21.Ackermann RT. Description of an integrated framework for building linkages among primary care clinics and community organizations for the prevention of type 2 diabetes: emerging themes from the CC-Link study. Chronic Illn. 2010;6:89. doi: 10.1177/1742395310364857. [DOI] [PubMed] [Google Scholar]
- 22.Cohn JN, Duprez DA. Time to foster a rational approach to preventing cardiovascular morbid events. J Am Coll Cardiol. 2008;52:327–9. doi: 10.1016/j.jacc.2008.02.085. [DOI] [PubMed] [Google Scholar]
- 23.Greenland P, Lloyd-Jones D. Defining a rational approach to screening for cardiovascular risk in asymptomatic patients. J Am Coll Cardiol. 2008;52:330–2. doi: 10.1016/j.jacc.2008.04.029. [DOI] [PubMed] [Google Scholar]