Summary
Post-partum cervicocephalic artery dissection (pp-CAD) is a rare and poorly understood condition. To our knowledge, only 21 cases have been reported. Reversible cerebral segmental vasoconstriction (RCSV) was first described by Call and Fleming in 1988, and its association with pp-CAD has only been reported in three cases. However, in those cases it is unclear whether the pp-CAD may have been caused by straining during labor and therefore merely coincidental to the intracranial arteriopathy. We describe a 41-year-old right-handed African-American woman who developed the syndrome of pp-CAD (headaches, trace subarachnoid hemorrhage and diffuse cerebral arteriopathy on angiogram) two weeks after delivery. In this unique case, the patient had fortuitously undergone an MR study twice over a four day period which included the carotid bifurcations. During that time the patient was an inpatient, on bed rest and subject to continuous cardiac monitoring. The interval studies documented a true spontaneous right internal carotid artery dissection occurring without obvious cause. The patient had noted moderate right neck pain developing between the two MR studies but experienced no neurological deficits. Subsequent conventional angiography confirmed the presence of postpartum cerebral arteriopathy and the cervical dissection. The patient was managed conservatively with antiplatelet medication and had an otherwise uneventful course. We hypothesize whether transient arterial wall abnormalities, postpartum hormonal changes or subtle connective tissue aberrations play a similar role in the pathogenesis of these two associated conditions.
Key words: internal carotid artery dissection, reversible cerebral segmental vasoconstriction, Call-Fleming syndrome, post-partum spontaneous cervicocephalic dissection
Introduction
Post-partum reversible cerebral segmental vasoconstriction syndrome (RCSV or “Call Fleming syndrome”) 1 and postpartum cervical carotid dissection are both rare, poorly understood conditions and, to our knowledge, their association has only been described three times in the literature 2,3. We describe a case of a definite truly spontaneous cervical carotid dissection documented on serial imaging of a patient during an admission with a classic RCSV syndrome and who was intensively monitored before, during and after the event – unique in clearly depicting the order of onset of these two events. We discuss the hypothesis that the underlying etiology of RCSV may not be limited to involvement of the cerebral circulation.
Case Report
A previously healthy right-handed 41-year-old G2P1 African-American woman with a medical and family history of migraines was admitted at full term for a cesarean section under spinal anesthesia due to cephalopelvic disproportion. She experienced an uneventful delivery but developed a right-sided positional headache, without neurological deficit, three days post-partum and was treated with a blood patch for a presumed CSF leak related to the epidural procedure. Both an MRI and MRA of the brain were unremarkable at the time.
The patient returned six days later with worsening headache and a non-contrast CT brain demonstrated a trace amount of blood over the left parietal and bilateral frontal lobes. She was admitted to the intensive care unit and, notably, her blood pressure remained normal throughout her stay.
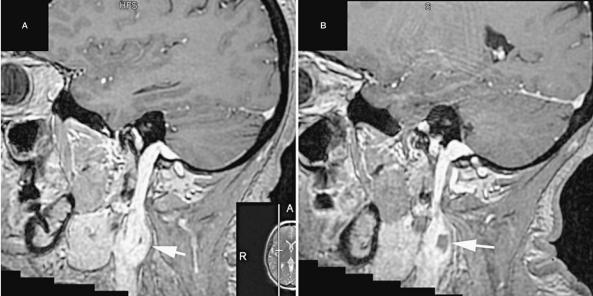
Figure 1.
Sagittal post gad MPRAGE demonstrates the proximal internal carotid segment (arrows) pre (A) and post (B) spontaneous dissection.
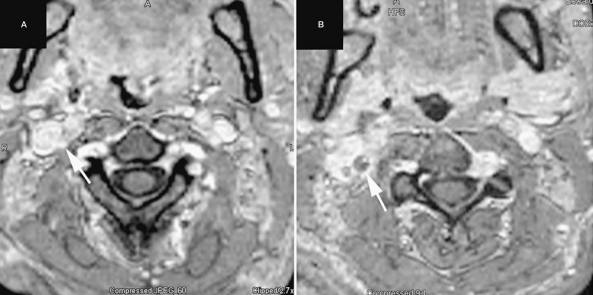
Figure 2.
Axial reformats of the post gad MPRAGE sequence pre (A) and post (B) spontaneous dissection show the characteristic non-enhancing crescent representing thrombus in the wall of the proximal ICA (arrows).
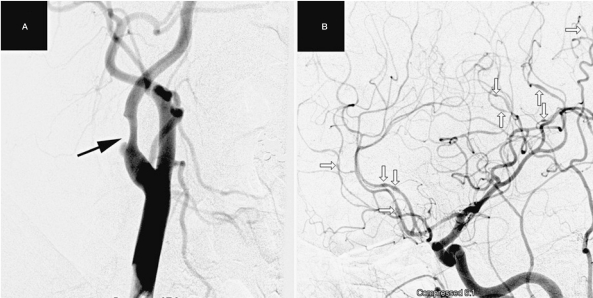
Subsequent CTA head and neck showed abnormal multifocal segmental caliber changes in all intracranial territories, whereas the cervical arteries appeared normal. A repeat MR brain showed no cerebral parenchymal abnormality and therefore no evidence of posterior reversible encephalopathy syndrome (PRES). A working diagnosis of RCVS was made and the patient was intensively monitored over that weekend with a view to performing conventional cerebral angiography on the following Monday. Prior to the conventional angiogram, she developed worse headache and a repeat MR brain showed no new intracranial changes. However, as the Institute's MR brain protocol included 3D contrast enhanced MPRAGE sequences with a field of view that extended through the neck as far as the carotid bifurcations, it was possible to detect a new stenosis and mural crescent of thrombus involving the previously normal right ICA just distal to the bulb. On questioning, the patient stated that she had developed moderate pain on the right side of her neck and had noted some tenderness over the carotid region in the four day period between the two studies but had not commented on it given the primacy of her other symptoms. Subsequent conventional angiography confirmed the presence of a frank multifocal segmental cerebral arteriopathy and an incompletely thrombosed right internal carotid artery dissection. The patient was managed initially with daily Aspirin 81 mg and after two weeks converted to standard Coumadin anticoagulation. She had an otherwise uneventful course. Her repeat CTA two months after discharge showed complete resolution of the cerebral vasculopathy and a stable right cervical ICA stenosis.
Figure 3.
Conventional angiography demonstrates the proximal right ICA dissection with a small amount of inflow into the predominantly thrombosed pseudolumen (A - arrow). The cerebral angiogram (B) shows multifocal stenosis and beading in the left anterior and middle cerebral territories.
Discussion
Postpartum Cervicocephalic Artery Dissection (pp-CAD) is a rare and poorly understood condition. To our knowledge, only 21 cases have been reported 2,3,4. The co-occurrence of RCSV and pp-CAD has only been reported in three of these cases 2,3. Arnold et al. first reported pp-CAD in association with RCSV in four cases but two of these were angiographically normal and none of them exhibited any clues as to the order of onset of the lesions 2. In these cases it was also uncertain whether the dissection was related to stressors such as straining during labor and/or hypertension. Our case is unusual both in confirming the association of RCSV with a truly spontaneous pp-CAD free of confounding insults and in demonstrating the stigmata of RCSV preceding the pp-CAD. The patient experienced an uneventful pregnancy and delivery without hypertension. There was a two week interval between the onset of pp-CAD and the delivery. Moreover, her initial MR brain and CTA neck studies confirm that there was no cervical dissection up to the time of her admission. Interestingly, there was a strong personal and family history of migraines which have been previously associated both with RCSV and CAD 1,5.
RCSV, first described by Call and Fleming in 1988 and also known as “post partum angiopathy”, is characterized by prolonged reversible vasoconstriction of the cerebral arteries, usually associated with acute-onset, severe, recurrent headaches with or without additional neurologic symptoms 1. Although ischemic infarction is rare, small subarachnoid hemorrhages are occasionally associated and are presumed to indicate an underlying loss of arterial mural integrity. Postpartum angiopathy can be associated with pre-eclampsia, eclampsia, and delayed postpartum eclampsia 6.
This case also promotes an inquiry into our current knowledge of arterial wall pathologies that may underlie both conditions. Several studies have performed dermal analyses of patients with spontaneous CAD showing ultrastructural derangements of type I and III collagen fibrils that were not present in controls 7,8. It is uncertain whether there may be an underlying genetic etiology 8 or if previously normal collagen fibrils and other matrix components (e.g. elastic fibers or networks) are altered by acquired inflammatory and autoimmune processes 7. Another study looked at superficial arterial biopsy specimens and found that eight of nine patients with spontaneous CAD had areas of degradation with inflammatory and erythrocytic accumulation between the tunica media and adventitia, whereas none of the control group had this finding. This further supports the theory of a more generalized arteriopathy underlying the CAD in these spontaneous cases. Spontaneous CAD has also been reported in association with other arteriopathies, namely posterior reversible encephalopathy syndrome (PRES), which could point to a common underlying etiology-arterial wall instability and dysfunction 6,9. Our case exhibited none of the imaging stigmata of PRES.
Given its association with sub-arachnoid hemorrhage, the arteriopathy of RCSV may also comprise an accelerated matrix breakdown and a disruption in the arterial wall in addition to the more apparent vasoconstrictive nature of the disease. Pathological analysis is lacking, given the condition's usually benign course and lack of surgical intervention. One can currently only speculate as to whether the increased immune system activity associated with pregnancy and the postpartum period could activate proteolytic enzymes such as matrix metalloproteinases to cause weakening of the arterial wall. With more widespread recognition of the Call-Fleming RCSV syndrome we should anticipate the discovery of more clues to its pathogenesis, its association with the puerperal period and spontaneous cervical artery dissection.
References
- 1.Call GK, Fleming MC, Sealfon S, et al. Reversible cerebral segmental vasoconstriction. Stroke. 1988;19:1159–1170. doi: 10.1161/01.str.19.9.1159. [DOI] [PubMed] [Google Scholar]
- 2.Arnold M, Camus-Jacqmin M, Stapf C, et al. Post-partum cervicocephalic artery dissection. Stroke. 2008;39:2377–2379. doi: 10.1161/STROKEAHA.107.510107. [DOI] [PubMed] [Google Scholar]
- 3.Sharshar T, Lamy C, Mas JL. Incidence and causes of strokes associated with pregnancy and puerperium. A study in public hospitals of Ile de France. Stroke. 1995;26:930–936. doi: 10.1161/01.str.26.6.930. [DOI] [PubMed] [Google Scholar]
- 4.Abisaab J, Nevadunsky N, Flomenbaum N, et al. Emergency department presentation of bilateral carotid artery dissections in a postpartum patient. Ann Emerg Med. 2004;44:484–489. doi: 10.1016/j.annemergmed.2004.03.031. [DOI] [PubMed] [Google Scholar]
- 5.Wiebers DO, Mokri B. Internal carotid artery dissection after childbirth. Stroke. 1985;16:956–959. doi: 10.1161/01.str.16.6.956. [DOI] [PubMed] [Google Scholar]
- 6.Singhal AB, Bernstein RA. Postpartum angiopathy and other cerebral vasoconstriction syndromes. Neurocrit Care. 2005;3:91–97. doi: 10.1385/NCC:3:1:091. [DOI] [PubMed] [Google Scholar]
- 7.Uhlig Ph, Bruckner P, Dittrich R, et al. Aberrations of dermal connective tissue in patients with cervical artery dissection (sCAD) J Neurol. 2008;255:340–346. doi: 10.1007/s00415-008-0585-4. [DOI] [PubMed] [Google Scholar]
- 8.Brandt T, Hausser I, Orberk E, et al. Ultrastructural connective tissue abnormalities in patients with spontaneous cervicocerebral artery dissections. Ann Neurol. 1998;44:281–285. doi: 10.1002/ana.410440224. [DOI] [PubMed] [Google Scholar]
- 9.Mellion ML, Rizvi S. Spontaneous bilateral carotid artery dissection and posterior reversible encephalopathy syndrome. Neurology. 2005;65:1990–1991. doi: 10.1212/01.wnl.0000188883.26456.2a. [DOI] [PubMed] [Google Scholar]