Abstract
Purpose
EGFR mutations underlie the sensitivity of lung cancers to erlotinib and gefitinib and can occur in any patient with this illness. Here we examine the frequency of EGFR mutations in smokers and men.
Methods
We determined the frequency of EGFR mutations and characterized their association with cigarette smoking status and male sex.
Results
We tested 2,142 lung adenocarcinoma specimens for the presence of EGFR exon 19 deletions and L858R. EGFR mutations were found in 15% of tumors from former smokers (181 of 1,218; 95% CI, 13% to 17%), 6% from current smokers (20 of 344; 95% CI, 4% to 9%), and 52% from never smokers (302 of 580; 95% CI, 48% to 56%; P < .001 for ever v never smokers). EGFR mutations in former or current smokers represented 40% of all those detected (201 of 503; 95% CI, 36% to 44%). EGFR mutations were found in 19% (157 of 827; 95% CI, 16% to 22%) of tumors from men and 26% (346 of 1,315; 95% CI, 24% to 29%) of tumors from women (P < .001). EGFR mutations in men represented 31% (157 of 503; 95% CI, 27% to 35%) of all those detected.
Conclusion
A large number of EGFR mutations are found in adenocarcinoma tumor specimens from men and people who smoked cigarettes. If only women who were never smokers were tested, 57% of all EGFR mutations would be missed. Testing for EGFR mutations should be considered for all patients with adenocarcinoma of the lung at diagnosis, regardless of clinical characteristics. This strategy can extend the use of EGFR tyrosine kinase inhibitors to the greatest number individuals with the potential for substantial benefit.
INTRODUCTION
Ninety percent of clinically relevant EGFR (epidermal growth factor receptor) mutations are either missense mutations in exon 21 or deletions in exon 19.1 Patients with lung adenocarcinomas and EGFR exon 19 or 21 mutations have high rates of radiologic response to gefitinib and erlotinib.2–4 In the Iressa Pan-Asia Study (IPASS), individuals with EGFR mutations treated with gefitinib had a 69% absolute improvement in objective response rate and a longer progression-free survival when compared with those without EGFR mutations.5
Randomized phase III studies of patients with metastatic non–small-cell lung cancer (NSCLC) and EGFR mutations have demonstrated improved progression-free survival and response rates for treatment with gefitinib compared with conventional doublet chemotherapy. On the basis of these data, EGFR tyrosine kinase inhibitors (TKIs) have emerged as a recommended first-line therapy in patients with EGFR-sensitizing mutations.6–9
Many clinicians have adopted a strategy to either treat all never smokers with lung adenocarcinoma with gefitinib or erlotinib or to only order mutation testing on tumor specimens from women who have never smoked. Although EGFR mutations are more common in tumors from patients with these characteristics, they can be found in men and in those who smoked cigarettes. In a multi-institutional study conducted in Spain, 2,105 patients were screened for the presence of EGFR mutations. EGFR mutations were found in 350 patients (17%). The incidence of EGFR mutations was 8%, 10%, and 6% in men, former smokers, and current smokers, respectively.10 Pham et al11 found EGFR mutations in 51% of patients with lung adenocarcinoma who were never smokers, with a similar incidence of mutations in men (27%) and women (23%; P = .55). EGFR mutations also were found in the tumors of former and current smokers. Patients who smoked from 16 to 75 pack-years had a 10% incidence of EGFR mutations as compared with 46% among those with 15 or fewer pack-years (P < .001). We have now expanded this effort to examine the frequency of EGFR mutations in men and cigarette smokers with lung adenocarcinomas in a cohort of 2,142 patients with stage I to IV lung adenocarcinoma. We hypothesized that, although less frequent than in women and never smokers, a significant proportion of lung adenocarcinomas with EGFR mutations occur in men and current/former smokers.
METHODS
Patients and Data Collection
Lung adenocarcinomas from consecutive patients evaluated at Memorial Sloan-Kettering Cancer Center between January 2002 and November 2009 with available tumor tissue underwent analysis for EGFR mutations. After microscopic examination confirmed the diagnosis of lung adenocarcinoma, DNA was extracted. EGFR exon 19 deletions and exon 21 L858R mutations were identified as previously described.12
With a waiver of authorization from the Memorial Sloan-Kettering Cancer Center institutional review board, we collected age, sex, smoking history, and stage of disease for all patients. Patients were categorized as never smokers (< 100 lifetime cigarettes), former smokers (quit ≥ 1 year ago), or current smokers (quit < 1 year ago).13
Statistical Analysis
The association between EGFR mutation status, sex, and amount of cigarettes smoked were evaluated using a χ2 test. We tested for the presence of a trend in the association between EGFR mutation status and the number of pack-years smoked (grouped in categories: 0, 1 to 5, 6 to 10, 11 to 15, 16 to 25, 26 to 50, 51 to 75, and > 75) using univariate logistic regression in which pack-year categories were treated in a continuous fashion, with the median number of pack-years assigned as the corresponding score. These cut points have been used in earlier studies.11,13,14 Overall survival was estimated from time of surgery (for stage I to IIIA patients) or diagnosis with advanced cancer (for stage IIIB to IV patients) until death or last available follow-up using Kaplan-Meier method. The log-rank test was used to detect differences in survival by sex and smoking history.
RESULTS
The presence of EGFR exon 19 deletions or L858R was determined in 2,142 lung adenocarcinomas, 1,085 with stage I to IIIA and 1,057 with stage IIIB to IV disease. There were 218 EGFR mutations (20%) detected in patients with early-stage lung adenocarcinoma and 285 (27%) in those with advanced stage disease. Among early-stage patients with EGFR mutations, 53% had exon 19 deletions and 47% had L858R. Of the advanced-stage patients with EGFR mutations, 61% had exon 19 deletions and 39% had L858R.
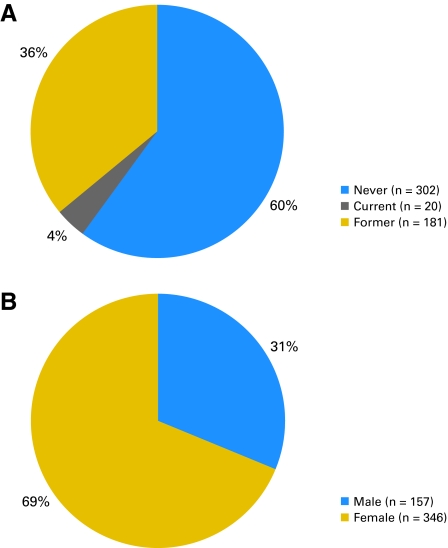
EGFR mutations were found in 15% of tumors from former smokers (181 of 1,218; 95% CI, 13% to 17%) and 6% of tumors from current smokers (20 of 344; 95% CI, 4% to 9%), compared with 52% of tumors from never smokers (302 of 580; 95% CI, 48% to 56%; P < .001 for ever v never smokers; Table 1). EGFR mutations in former and current smokers represented 40% of all mutations detected (201 of 503; 95% CI, 36% to 44%; Fig 1A). There was an inverse relationship between the incidence of EGFR mutations and the number of pack-years of cigarette smoking, with fewer mutations found in patients with greater smoking histories (P for trend < .001 for patients with early-stage disease, with advanced-stage disease, and for all patients; Table 2).
Table 1.
Incidence of EGFR Mutations by Cigarette Smoking History
| Smoking History | Stage I-IIIA |
Stage IIIB/IV |
All Stages |
P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. with Mutations | Total No. of Tumors | % | No. with Mutations | Total No. of Tumors | % | No. with Mutations | Total No. of Tumors | % | 95% CI | ||
| Never | 131 | 228 | 57 | 171 | 352 | 49 | 302 | 580 | 52 | 48 to 56 | < .001 χ2(df = 2) = 314 |
| Former | 83 | 714 | 12 | 98 | 504 | 19 | 181 | 1,218 | 15 | 13 to 17 | |
| Current | 4 | 143 | 3 | 16 | 201 | 8 | 20 | 344 | 6 | 4 to 9 | |
Fig 1.
EGFR mutation by (A) smoking status and (B) sex.
Table 2.
Incidence of EGFR Mutations by Pack-Years of Cigarettes Smoked
| Pack-Years | Stage I-IIIA |
Stage IIIB/IV |
All Stages |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. With Mutations | Total No. of Tumors | % | No. With Mutations | Total No. of Tumors | % | No. With Mutations | Total No. of Tumors | % | 95% CI | |
| Never smokers | 131 | 228 | 57 | 171 | 352 | 49 | 302 | 580 | 52 | 48 to 56 |
| 1 to 5 | 22 | 57 | 39 | 20 | 68 | 29 | 42 | 125 | 34 | 25 to 43 |
| 6 to 10 | 11 | 47 | 23 | 29 | 69 | 42 | 40 | 116 | 34 | 26 to 44 |
| 11 to 15 | 10 | 59 | 17 | 9 | 49 | 18 | 19 | 108 | 18 | 11 to 26 |
| 16-25 | 13 | 129 | 10 | 13 | 110 | 12 | 26 | 239 | 11 | 7 to 16 |
| 26 to 50 | 16 | 294 | 5 | 27 | 246 | 11 | 43 | 540 | 8 | 6 to 11 |
| 51 to 75 | 10 | 148 | 7 | 11 | 95 | 12 | 21 | 243 | 9 | 5 to 13 |
| > 75 | 3 | 116 | 3 | 4 | 66 | 6 | 7 | 183 | 4 | 2 to 8 |
| P(trend test) | < .001 χ2(df = 1) = 129 | < .001 χ2(df = 1) = 90.2 | < .001 χ2(df = 1) = 224 | |||||||
The incidence of EGFR mutations among all patients decreases from 52% in never smokers to 29% in patients with smoking histories of 1 to 15 pack-years to 8% in patients who reported 16 or more pack-years of cigarette smoke (P < .001). However, EGFR mutations were found even in those patients with a greater than 75 pack-year smoking history, with a 3% and 6% incidence in those with early-stage and in those with advanced adenocarcinoma, respectively.
EGFR mutations were found in 19% (157 of 827; 95% CI, 16% to 22%) of tumors from men and 26% (346 of 1,315; 95% CI, 24% to 29%) of tumors from women (P < .001; Table 3), with mutations in men representing 31% (157 of 503; 95% CI, 27% to 35%) of all those detected (Fig 1B). The smoking status was analyzed separately for males and females. We found that the incidence of mutations in female smokers and male smokers was 14% and 11%, respectively (P = .073), whereas in female never smokers and male never smokers, it was 55% and 47%, respectively (P = .15, Table 4).
Table 3.
Incidence of EGFR Mutations by Sex
| Sex | Stage I-IIIA |
Stage IIIB/IV |
All Stages |
P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. With Mutations | Total No. of Tumors | % | No. With Mutations | Total No. of Tumors | % | No. With Mutations | Total No. of Tumors | % | 95% CI | ||
| Female | 161 | 690 | 23 | 185 | 625 | 30 | 346 | 1,315 | 26 | 24 to 29 | < .001 χ2(df = 1) = 15.2 |
| Male | 57 | 395 | 14 | 100 | 432 | 23 | 157 | 827 | 19 | 16 to 22 | |
| Total | 218 | 1,085 | 20 | 285 | 1,057 | 27 | 503 | 2,142 | 23 | 22 to 25 | |
Table 4.
Incidence of EGFR Mutations by Cigarette Smoking History and Sex
| Smoking History and Sex | Stage I-IIIA |
Stage IIIB/IV |
All Stages |
P* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. With Mutations | Total No. of Tumors | % | No. With Mutations | Total No. of Tumors | % | No. With Mutations | Total No. of Tumors | % | 95% CI | ||
| Never smokers | |||||||||||
| Female | 101 | 176 | 57 | 116 | 222 | 52 | 217 | 398 | 55 | 49 to 59 | .15 |
| Male | 30 | 52 | 57 | 55 | 130 | 42 | 85 | 182 | 47 | 39 to 54 | χ2(df = 1) = 2.12 |
| Total | 131 | 228 | 57 | 171 | 322 | 53 | 302 | 580 | 52 | 48 to 56 | |
| Smokers | |||||||||||
| Female | 60 | 514 | 12 | 69 | 403 | 17 | 129 | 917 | 14 | 12 to 16 | .073 |
| Male | 27 | 343 | 8 | 45 | 302 | 15 | 72 | 645 | 11 | 9 to 14 | χ2(df = 1) = 3.21 |
| Total | 87 | 857 | 10 | 114 | 705 | 16 | 201 | 1,562 | 13 | 11 to 15 | |
P value was adjusted for stage.
The median overall survival in former/current smokers with stage I to III disease whose tumors harbor an EGFR mutation has not yet been reached, whereas in never smokers it is 6.9 years (P = .36). For those with stage IIIB/IV disease harboring EGFR mutations, the median overall survival in never smokers is 2.8 years and in former/current smokers is 3.5 years (P = .09).
The median overall survival for patients whose tumors harbor EGFR mutations with stage I to III disease has not yet been reached in men and is 6.9 years in women (P = .30). There is no difference in median overall survival by sex in individuals with stage IIIB/IV disease with EGFR mutations (P = .96).
DISCUSSION
Before the discovery of EGFR mutations in the tumors of patients with dramatic responses to gefitinib and erlotinib, clinical characteristics were the only way to predict response. Since 2004, multiple prospective studies have proven that mutations in the EGFR tyrosine kinase domain are the best predictors of response and progression-free survival benefit with EGFR TKI.5,7,8
Although mutations are clearly more common in adenocarcinomas from women and never smokers, a substantial proportion of these specimens do not harbor mutations, and patients with these characteristics derive little or no benefit from gefitinib (a 1% partial response rate and lower progression-free survival, hazard ratio of 2.93 in IPASS). Many studies have attempted to select patients likely to respond to gefitinib and erlotinib (and with EGFR mutations) using established clinical characteristics such as female sex, never or “light” smoking history, and bronchioloalveolar features in tumor specimens.5,15,16 When mutation testing was done, the proportion of patients with EGFR mutations ranged from 42% to 60%. Even in IPASS, in which nearly all patients were female never smokers from East Asia, just 60% had EGFR mutations. Mutations were less frequent (40% and 42%) in the two North American series.
In this analysis, EGFR mutations occur with an incidence of 23% in 2,142 patients with stage I through IV lung adenocarcinoma, similar to our previous findings. Tumors from 19% of men and 13% of current/former smokers harbor EGFR sensitizing mutations. Although there is a decrease in the incidence of mutations with increased number of pack-years smoked, a substantial number of EGFR mutations were found in patients with a significant history of smoking. EGFR mutations in men and former/current smokers represent 31% and 40% of all mutations, respectively. Further demonstrating that it is the mutation and not the clinical characteristic that underlies the clinical outcomes seen after EGFR TKI treatment, the overall survival of men and former/current smokers with EGFR mutations was similar to that seen in women and never smokers. The results in these North American patients (predominantly of European heritage) are comparable to the results reported among patients from East Asia.5,7,8 Similar findings were reported in a multi-institutional study conducted in Spain where EGFR mutations were found 350 (17%) of 2,105 patients. The incidence of EGFR mutations was 8%, 10%, and 6% in men, former, and current smokers, respectively.10
Limitations in this analysis are that this is a single-institution series and we did not test for the L861Q and G719A/S, which may be sensitive to EGFR TKI treatment during the time period of this study. We now routinely assay for these less common EGFR sensitivity mutations, and their incidence remains quite rare. Of 119 EGFR mutations, we discovered only five (4%). The exon 19 deletions and L858R point mutations we assayed in all patients represent 90% of EGFR sensitizing mutations. This is the largest series reported, and the analytic methods used have been consistent and reproducible over this time period.11,12 The methods used to collect tobacco exposure and the documentation of never smoking status have been standardized.11,13
With the “proof of principle” experience with EGFR mutations and EGFR TKIs in lung adenocarcinomas, since January 1, 2009, we have tested the tumors of all patients diagnosed with lung adenocarcinoma tumors and adequate tissue for the presence of driver mutations (KRAS, EGFR, BRAF, HER2, PIK3CA, AKTI, MEKI [MAP2K1], NRAS, and EML4-ALK). We have also joined with 13 other US institutions to form the Lung Cancer Mutation Consortium to test 1,000 adenocarcinoma specimens for the presence of the driver mutations listed above, in an attempt to link patients with “actionable” mutations to clinical trials of targeted agents.
Although clinical selection factors to choose EGFR TKIs have guided the care of individual patients and facilitated research for a decade, this strategy has been eclipsed by our ability to use the presence of EGFR sensitizing mutations as the basis for treatment. If we only perform mutation testing in selected patients based on clinical features, we will fail to detect a substantial number of mutations in smokers and men, denying them the benefits of gefitinib or erlotinib at diagnosis. Thirty-one percent of all EGFR mutations would be missed if testing were restricted to women, 40% would be missed if testing were restricted to never smokers, and 57% would be missed if testing were restricted to women who never smoked cigarettes (Table 5). Our findings in men and smokers add evidence to support the growing consensus that all patients with adenocarcinoma and large-cell carcinoma of the lung and NSCLC not otherwise specified should undergo mutation testing at diagnosis if tissue is available, now part of the National Comprehensive Cancer Network guidelines for the treatment of NSCLC.6 EGFR mutations can be accurately and quickly determined by widely available tests. Although these analyses now require the availability of sufficient tumor, new approaches hold promise to permit the detection of EGFR mutations on cytology specimens17,18 and circulating tumor cells.19
Table 5.
Patients Tested and EGFR Mutations Missed Under Different Testing Strategies
| Population Tested | Patients Tested |
EGFR Mutations Detected |
EGFR Mutations Missed |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Women only | 1,315 | 61 | 346 | 69 | 157 | 31 |
| Never smokers only | 580 | 27 | 302 | 60 | 201 | 40 |
| Never smoking women | 398 | 19 | 217 | 43 | 286 | 57 |
| All patients | 2,142 | 100 | 503 | 100 | 0 | 0 |
Glossary Terms
- Driver mutations:
Driver mutations are those that are causally implicated in oncogenesis or tumor survival. Such mutations have been positively selected during carcinogenesis and often show a recurrent pattern within or across tumor types. This is in contrast with passenger events, which arise from the background mutation rate and do not contribute to oncogenesis.
- EGFR (epidermal growth factor receptor):
Also known as HER-1, EGFR belongs to a family of receptors (HER-2, HER-3, HER-4 are other members of the family) and binds to the EGF, TGF-α, and other related proteins, leading to the generation of proliferative and survival signals within the cell. It also belongs to the larger family of tyrosine kinase receptors and is generally overexpressed in several solid tumors of epithelial origin.
- Erlotinib:
Also known as Tarceva, erlotinib is a small molecule that inhibits the tyrosine kinase activity of EGFR/HER-1 and has been evaluated extensively in clinical trials in patients with non-small-cell lung cancer, pancreatic cancer, and glioblastoma multiforme.
- Gefitinib:
Belonging to the class of tyrosine kinase inhibitors, gefitinib (also known as Iressa) binds to the cytoplasmic region of the EGFR that also binds ATP. By competing with ATP binding that is essential for tyrosine phosphorylation, gefitinib inhibits activation of EGFR and blocks the cascade of reactions leading to cellular proliferation.
Footnotes
Presented in part at the 46th Annual Meeting of the American Society of Clinical Oncology, June 4-8, 2010, Chicago, IL.
Terms in blue are defined in the glossary, found at the end of this article and online at www.jco.org.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: Gregory J. Riely, AstraZeneca (C), Boehringer Ingelheim (C); Vincent A. Miller, Boehringer Ingelheim (C), Genentech (C), OSI Pharmaceuticals (C), Roche (C); Marc Ladanyi, AstraZeneca Canada (C); Mark G. Kris, Boehringer Ingelheim (C), Pfizer (C) Stock Ownership: None Honoraria: Marc Ladanyi, Genzyme, Sequenom Research Funding: None Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Sandra P. D'Angelo, M. Catherine Pietanza, Melissa L. Johnson, Gregory J. Riely, Vincent A. Miller, Camelia S. Sima, Maureen F. Zakowski, Valerie W. Rusch, Marc Ladanyi, Mark G. Kris
Financial support: Mark G. Kris
Administrative support: Mark G. Kris
Provision of study materials or patients: Mark G. Kris
Collection and assembly of data: Sandra P. D'Angelo, M. Catherine Pietanza, Melissa L. Johnson, Maureen F. Zakowski, Valerie W. Rusch, Marc Ladanyi, Mark G. Kris
Data analysis and interpretation: Sandra P. D'Angelo, M. Catherine Pietanza, Melissa L. Johnson, Gregory J. Riely, Vincent A. Miller, Camelia S. Sima, Mark G. Kris
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Li AR, Chitale D, Riely GJ, et al. EGFR mutations in lung adenocarcinomas: Clinical testing experience and relationship to EGFR gene copy number and immunohistochemical expression. J Mol Diagn. 2008;10:242–248. doi: 10.2353/jmoldx.2008.070178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 3.Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: Correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 4.Pao W, Kris MG, Iafrate AJ, et al. Integration of molecular profiling into the lung cancer clinic. Clin Cancer Res. 2009;15:5317–5322. doi: 10.1158/1078-0432.CCR-09-0913. [DOI] [PubMed] [Google Scholar]
- 5.Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–957. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network. Fort Washington, PA: National Comprehensive Cancer Network; 2011. NCCN Guidelines: Non-Small Cell Lung Cancer, Version 2.2011. [Google Scholar]
- 7.Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–2388. doi: 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- 8.Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): An open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121–128. doi: 10.1016/S1470-2045(09)70364-X. [DOI] [PubMed] [Google Scholar]
- 9.Zhou C, Wu Y-L, Chen G, et al. Efficacy results from the randomised phase III OPTIMAL (CTONG 0802) study comparing first-line erlotinib versus carboplatin plus gemcitabine, in Chinese advanced non-small cell lung cancer patients. Ann Oncol. 2010;21(suppl):6. abstr LBA13. [Google Scholar]
- 10.Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361:958–967. doi: 10.1056/NEJMoa0904554. [DOI] [PubMed] [Google Scholar]
- 11.Pham D, Kris MG, Riely GJ, et al. Use of cigarette-smoking history to estimate the likelihood of mutations in epidermal growth factor receptor gene exons 19 and 21 in lung adenocarcinomas. J Clin Oncol. 2006;24:1700–1704. doi: 10.1200/JCO.2005.04.3224. [DOI] [PubMed] [Google Scholar]
- 12.Pan Q, Pao W, Ladanyi M. Rapid polymerase chain reaction-based detection of epidermal growth factor receptor gene mutations in lung adenocarcinomas. J Mol Diagn. 2005;7:396–403. doi: 10.1016/S1525-1578(10)60569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janjigian YY, McDonnell K, Kris MG, et al. Pack-years of cigarette smoking as a prognostic factor in patients with stage IIIB/IV nonsmall cell lung cancer. Cancer. 2010;116:670–675. doi: 10.1002/cncr.24813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riely GJ, Pao W, Pham D, et al. Clinical course of patients with non-small cell lung cancer and epidermal growth factor receptor exon 19 and exon 21 mutations treated with gefitinib or erlotinib. Clin Cancer Res. 2006;12:839–844. doi: 10.1158/1078-0432.CCR-05-1846. [DOI] [PubMed] [Google Scholar]
- 15.Janne PA, Wang XF, Socinski MA, et al. Randomized phase II trial of erlotinib (E) alone or in combination with carboplatin/paclitaxel (CP) in never or light former smokers with advanced lung adenocarcinoma: CALGB 30406. J Clin Oncol. 2010;28(suppl):539s. doi: 10.1200/JCO.2011.40.1315. abstr 7503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kris MG, Pao W, Zakowski M, et al. Prospective trial with preoperative gefitinib to correlate lung cancer response with EGFR exon 19 and 21 mutations and to select patients for adjuvant therapy. J Clin Oncol. 2006;24(suppl):369s. abstr 7021. [Google Scholar]
- 17.Brevet M, Arcila M, Ladanyi M. Assessment of EGFR mutation status in lung adenocarcinoma by immunohistochemistry using antibodies specific to the two major forms of mutant EGFR. J Mol Diagn. 2010;12:169–176. doi: 10.2353/jmoldx.2010.090140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kawahara A, Yamamoto C, Nakashima K, et al. Molecular diagnosis of activating EGFR mutations in non-small cell lung cancer using mutation-specific antibodies for immunohistochemical analysis. Clin Cancer Res. 2010;16:3163–3170. doi: 10.1158/1078-0432.CCR-09-3239. [DOI] [PubMed] [Google Scholar]
- 19.Maheswaran S, Sequist LV, Nagrath S, et al. Detection of mutations in EGFR in circulating lung-cancer cells. N Engl J Med. 2008;359:366–377. doi: 10.1056/NEJMoa0800668. [DOI] [PMC free article] [PubMed] [Google Scholar]