Abstract
Background
Attention Bias Modification Treatment (ABMT) is a newly-emerging promising treatment for anxiety disorders. While recent randomized control trials (RCTs) suggest that ABMT reduces anxiety, therapeutic effects have not been summarized quantitatively.
Methods
Standard meta-analytic procedures were used to summarize the effect of ABMT on anxiety. Using MEDLINE, January 1995 to February 2010, we identified RCTs comparing the effects on anxiety of ABMT and quantified effect sizes using Hedge’s d.
Results
Twelve studies met inclusion criteria, including 467 participants from 10 publications. ABMT produced significantly greater reductions in anxiety than control training, with a medium effect (d = 0.61, p <.001). Age and gender did not moderate the effect of ABMT on anxiety, while several characteristics of the ABMT training did.
Conclusions
ABMT shows promise as a novel treatment for anxiety. Additional RCTs are needed to fully evaluate the degree to which these findings replicate and apply to patients. Future work should consider the precise role for ABMT in the broader anxiety-disorder therapeutic armamentarium.
Keywords: cognitive bias, attention bias modification treatment, anxiety disorders, meta-analysis, novel treatment, psychotherapy
Introduction
Anxiety disorders affect between 10 and 30% of individuals (1-3), creating significant clinical burden (4). Nevertheless, many affected individuals do not receive treatment (5), and, among those who do, many continue to suffer (6, 7). Hence, novel treatments are needed.
Selective serotonin reuptake inhibitors (SSRIs) are an established medication treatment. Nevertheless, some patients are reluctant to take SSRIs because of known side-effects or because much remains unknown about their mechanism of action. Particular concerns arise in children (8). Cognitive behavioral therapy (CBT) is an established psychotherapeutic treatment (9). Nevertheless, as with SSRIs, problems arise with this treatment. Many patients do not have access, and the treatment is demanding for some of those who do (10). This is because some aspects of CBT require patients to understand complex concepts and build relationships with a therapist. Finally, not all patients achieve remission with CBT. Thus, data on SSRIs and CBT suggest the need for novel therapies.
Recent work generates interest in one such treatment: Attention Bias Modification Treatment (ABMT). ABMT arises from the notion that cognitive biases cause pathological anxiety, which also underlies models of CBT. Based on this idea, CBT targets a range of biases. It engages patients in explicit integrative processes by way of verbalization, coupled with exposure to feared situations, so that they can interpret or learn that feared objects/situations are safe. ABMT differs from CBT in that its therapeutic action targets a specific bias in attention, extending work implicating threat-related attention bias in anxiety (11).
ABMT’s focus on attention resonates with findings in translational neuroscience. Research in animal models suggests that anxiety-related attention bias emerge from parallel-distributed neural pathways, some of which place relatively limited demands on cortically-based networks and associated top-down interpretive processes (8). Human brain imaging research implicates such parallel neural pathways in threat-related attention bias and inter-individual differences in anxiety (8, 12-14), suggesting that attention bias in anxiety disorders involves both cortical and sub-cortical perturbations. Forms of CBT targeting top-down interpretive processes may fail to fully target this sub-cortical component. Compared to the explicit training techniques of CBT, attention perturbation may be more easily shaped by ABMT, with its use of repetitive, computer-based training methods targeting implicit, sub-cortical processes (8). As such, ABMT may represent a novel treatment that directly targets perturbed neural circuitry function.
In 1995, MacLeod et al. first suggested that ABMT might augment available anxiety-disorder treatments (15). Training used the now classic dot-probe task, as illustrated in Figure 1. The task requires subjects to identify a non-emotional probe, such as a letter or symbol (e.g., a colon in Figure 1), which can appear in one of two spatial locations, as also shown in Figure 1. Immediately prior to the probe presentation, a threatening and a non-threatening stimulus appear simultaneously in two separate locations. Differences in response time to probes appearing behind threatening and non-threatening stimuli indexes attention bias. For example, in Figure 1 A, the probe appears behind the threat-related word, and responses on these trials are expected to be slower for individuals whose attention is captured by threat or has difficulty disengaging from threat to identify the probe’s spatial location.
Figure 1.
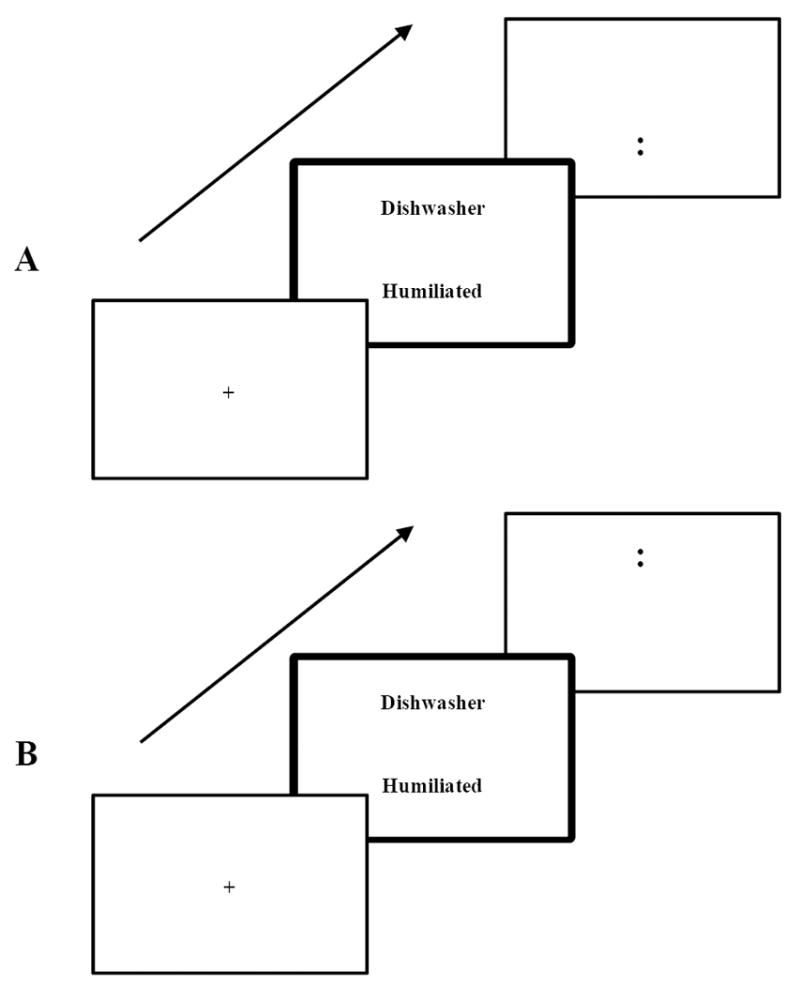
Two stimuli differing in emotional valence (threat or non-threat) are presented at the same time usually for 500ms, and then followed by a probe (i.e. colon). In the classic dot probe task to measure an attention bias, a probe appears shortly after either of the locations that the two stimuli were presented, with the same frequencies (i.e. 50%, trials A and B are equally mixed). On the other hand, in the modified dot probe task (i.e. Attention Bias Modification Treatment), a probe always appears in the location of neutral stimulus (i.e. 100%, only B trials).
MacLeod et al. were the first to show that healthy individuals could be trained to exhibit an attention bias toward threat, with an associated increase in stress reactivity (16). Since then, other investigators attempted to utilize and extend this effect to reduce stress reactivity by the way of reducing an attention bias toward threat, for example using such modified task composed of trials only from Figure 1 B (17-34). While the number of studies is small, enough data have accumulated to generate questions on the utility of ABMT. The current report provides a quantitative meta-analysis to estimate effects of ABMT on anxiety.
Methods and Materials
Literature search and selection criteria
Studies were selected through a computer search of English reports in MEDLINE from January 1995 to February 2010 using the following key words: attentional training and anxiety, attentional retraining and anxiety, or attention modification and anxiety. This search was supplemented through a review of reference lists and correspondence with researchers. Studies were selected using five criteria: (1) the study investigated the impact of ABMT on anxiety symptoms in a randomized-controlled trial (RCT); (2) use of the dot-probe task 1; (3) use of a control group; (4) intention of reducing anxiety; (5) inclusion of at least two anxiety assessment points. These criteria initially were applied by the first author (YH) and then independently reviewed by another (DSP), with disagreements adjudicated by all authors.
The search produced 817 articles, which were reduced to 19 published reports on ABMT treatment. Application of the above-noted criteria led to the exclusion of nine reports. The first reported study, by MacLeod et al. (16), was removed because the experimental manipulation was not designed to reduce anxiety; the assessment points for Experiment 1 were embedded in training trials (i.e., no pre-ABMT assessment); and the control group in Experiment 2 involved training subjects to attend toward negative stimuli, which could enhance rather than reduce anxiety. The lack of an appropriate control group and the use of a design intended to increase anxiety led to exclusion of three other studies: Eldar et al. (22), Krebes et al. (25) and Browning et al. (35). MacLeod et al. (33) (Study 2) and Wadlinger et al. (30) were excluded because they did not include an anxiety outcome measure. A final set of two studies was excluded because neither used a modified dot-probe task (36, 37). After these exclusions, 12 sample data sets from 10 published reports served as the target data. Three studies examined the effect of ABMT on anxiety following stress exposure (19, 24, 29), and one included a four-month follow-up (21). Otherwise, designs for eight other studies were similar: parallel-group RCT and brief follow-up. Corresponding authors were contacted to facilitate effect size calculations. Study characteristics appear in Table 1.
Table 1.
Study characterictics and mean effect sizes (Hedge d a)
| Post-training | Post-stressor | Follow-Up (4 months) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | # of Subjects | Population | Mean age of subjects | Female % of subjects | Random assignment (Yes/No) | Blind (Double/Semi) | Stimulus type of training target | Stimulus Duration (ms) | Stimulus Location (Left-Right/Top-Bottom) | # of training trials | #of sessions (days) | Type of stressor | Outcome measures | Hedge d | ||
| Comparison between a group trained toward neutral stimulus and control group: Neutral vs Control | ||||||||||||||||
| Amir et al. (2009) | 48 | Patients with GSP | 29.35 | 59 | Yes | Double | Neutral Face | 500 | Top-Bottom | 160 | 8 | None | STAI-T | -0.10 | - | - |
| LSAS | 0.43 | - | - | |||||||||||||
| SPAI | -0.33 | - | - | |||||||||||||
| BDI-II | 1.12 *** | - | - | |||||||||||||
| HAM-D | 0.58 | - | - | |||||||||||||
| SDS | 0.89 ** | - | - | |||||||||||||
| Elder & Bar-Haim (2009) | 30 | Low anxious students | 22.64 | 73 | Yes | Semi | Neutral Face | 500 | Left-Right | 480 | 1 | None | STAI-S | 0.01 | - | - |
| 30 | High anxious students | 22.72 | 87 | Yes | Semi | Neutral Face | 500 | Left-Right | 480 | 1 | None | STAI-S | -0.34 | - | - | |
| Klump & Amir (2009) | 53 | High anxious students | 19.55 | 40 | Yes | Double | Neutral Face | 500 | Top-Bottom | 160 | 1 | Speech Task | STAI-S | -0.06 | 0.36 | - |
| Schmidt et al. (2009) | 36 | Patients with GAD | 23 | 44 | Yes | Double | Neutral Face | 500 | Top-Bottom | 160 | 8 | None | BSPS | 1.22 ** | - | 1.91 *** |
| LSAS | 1.84 *** | - | 2.68 *** | |||||||||||||
| SPAI | 1.46 *** | - | 1.98 *** | |||||||||||||
| STAI-T | 3.98 *** | - | 8.68 *** | |||||||||||||
| BDI-II | 1.12 ** | - | 1.77 *** | |||||||||||||
| See et al. (2009) | 40 | Nonselected students | 21.55 | 60 | Yes | Semi | Neutral Word | 500 | Left-Right | 192 | 15 | Moving to a foreign country | STAI-S | - | 0.60 | - |
| STAI-T | - | 0.79 * | - | |||||||||||||
| Hazen et al. (2009) | 24 | High anxious students | 19.3 | 65 | Yes | Double | Neutral Word | 500 | Top-Bottom | 1080 | 5 | None | PSWQ | 1.10 | - | - |
| STAI-T | 0.79 | - | - | |||||||||||||
| BDI | 1.00 | - | - | |||||||||||||
| Amir et al. (2009) | 29 | Patients with GAD | 25.5 | 48 | Yes | Double | Neutral Word | 500 | Top-Bottom | 280 | 8 | None | STAI-T | 1.06 ** | - | - |
| STAI-S | 1.63 *** | - | - | |||||||||||||
| BDI-II | 0.09 | - | - | |||||||||||||
| WDQ | 0.72 | - | - | |||||||||||||
| PSWQ | 0.44 | - | - | |||||||||||||
| HRSA | 0.99 * | - | - | |||||||||||||
| HAM-D | 0.43 | - | - | |||||||||||||
| Amir et al. (2008) | High anxious adults | 94 | 19 | 51 | Double | Neutral Face | 500 | Top-Bottom | 128 | 1 | Public speaking | STAI-S | 0.11 | 1.07 *** | - | |
| Mathews & MacLeod (2002) Exp7 | High anxious adults | 29 | N/P | 55 | Semi | Neutral Word | 16 (as a mask, 50%) + 500 (50%) | Top-Bottom | 750 | 10 | Exam | STAI-T | 5.76 *** | - | - | |
| Mathews & MacLeod (2002) Exp8 | High anxious adults | 30 | N/P | 57 | Semi | Neutral Word | 16 (as a mask, 50%) + 500 (50%) | Top-Bottom | 750 | 8 | None | STAI-T | 2.60 *** | - | - | |
| Comparison between a group trained toward happy stimulus and control group: Positive vs Control | ||||||||||||||||
| Li et al. (2008) | High anxious adults | 24 | 20.54 | 42 | Semi | Happy Face | 500 | Left-Right | 480 | 7 | None | SIAS | 0.94 * | - | - | |
| SPS | -0.18 | - | - | |||||||||||||
| FNES | 0.48 | - | - | |||||||||||||
GSP, generalized social phobia; STAI-T, state-trait anxiety inventory-trait; LSAS, Liebowitz social anxiety scale (clinician-administered); SPAI, social phobia and anxiety scale; BDI-II, Beck depression inventory-II; HAM-D, Hamilton rating scale of depression (clinician-administered); SDS, Sheelan disability scale; STAI-S, state-trait anxiety inventory-state; GAD, generalized anxiety disorder; BSPS, brief social phobia scale (clinician-administered); PSWQ, Penn state worry questionnaire; WDQ, worry domains questionnaire; HRSA, Hamilton rating scale of anxiety (clinician-administered); SIAS, social interaction anxiety scale; SPS, social phobia scale; FNES, fear of negative evaluation scale; N/P, not provided.
Definition of categories for d: no effect (0 –.2), low effect (.2–.5), medium effect (.5–.8), and high effect (> .8).
Control groups got through a normal dot-probe task (i.e., probe appears in either location of two different stimuli with equal frequency).
Significant at p < .001.
Significant at p < .01.
Significant at p < .05.
To investigate sources of heterogeneity, we considered six modifiers: (1) subject characteristics (patients or healthy individuals, anxious or non-anxious); (2) training-target stimulus (faces or words); (3) stimulus location (right or left, top or bottom); (4) stressor exposure (presence or absence of stressor exposure after training); (5) outcome measures (self-reported or clinician assessed); and (6) extent of training (number of trials and sessions).
Computing effect sizes for primary and secondary analyses
We first generated within-group effect sizes for ABMT and control groups. We then generated one effect size per experiment to index the differential effect on anxiety between the two experimental groups. Although some studies collected data on a range of symptoms, our primary goal was to estimate effects on anxiety. As a result, the principal analysis used only anxiety measures. For studies using more than one anxiety scale, effect sizes were computed per scale and averaged. Additional analyses examined effects for specific scales. Cohen’s q (38) (pp. 109-143) indexed effect sizes.
Standard software [Meta-Analysis Programs, Version 5.3 (39) and DSTAT (40)] was used. The q statistic is not a simple function of the difference between two effect sizes (d) because the same difference between effect sizes can result in different outcomes, depending on where along the d scale this difference occurs. To address this potential problem, the effect size d can be converted to an r statistic. Then, the r statistic can be transformed using Fisher’s z (z = ½ loge + [1r/1-r]) to generate the q statistic, which is the difference between Fisher z’s across the experimental and control groups. Cohen applies Fisher’s z because intervals along the scale remain equal. As such, differences of the same magnitude can be detected, regardless of the sizes of the z statistic in the experimental and control groups. According to Cohen (38) (pp. 109-143), q reflects an effect size index comparable to the “d family” of effects, and it can be converted to d by transforming q to r, and then back to d. Given the frequent reliance in other meta-analyses on this “d-family” of effect sizes, the unbiased estimator d (Hedge’s d) was used to index the between-group effect size of ABMT vs. control on anxiety and other symptoms. This d index was selected because it corrects for the bias in estimation of population effect size (41). Positive d values indicate greater improvement of outcome measures in ABMT compared to control. To estimate the overall effect size across studies, the weighted grand mean score was used for the ABMT and control groups.
To evaluate the file-drawer problem, we calculated a fail-safe N for all effect-size subsets, thereby estimating the number of unpublished studies with effect sizes of zero needed to reduce the aggregated effect below significance (42). A fail-safe N was not computed for effect-size aggregations producing non-significant results.
The overall effect size of changes in attention bias between pre- and post-ABMT was estimated in the same way as changes in anxiety-related scales. Attention bias towards negative stimuli is usually given as the subtraction of mean response latencies to targets in the location of neutral stimuli from that of negative stimuli. Of 12 studies, two did not measure change in attention bias (24, 32). From the remaining 10, we obtained data from 7 studies, either through published results or correspondence with authors. We also computed Spearman’s correlations to examine association between changes in attention bias and changes in anxiety pre- to post ABMT.
Our secondary goal was to test for effects of moderators on anxiety score changes as well as attention bias changes. These effects were estimated using two procedures. First, for categorical measures including the subject characteristics, training-target stimulus, stimulus location; stressor exposure; and outcome measures, weighted mean effect sizes were generated from different levels of a moderator and then compared with Qb tests (40). The Qb statistic is a between-group homogeneity test derived from Hedges and Olkin (41) that is analogous to a two-category pair-wise comparison. Second, moderation by continuous measures including the extent of training, age, and sex was tested using weighted least-squares analysis (effects weighted by sample size). For such analysis, the adjustment to the standard error recommended by Hedges (43) was applied, and 95% confidence intervals for the standardized regression coefficients were constructed. All tests are two-tailed with alpha set at 0.05.
Results
Thirty-nine effect sizes were computed using the 12 data sets from the 10 published reports. Study characteristics and 39 effect sizes per scale or assessment point are provided in Table 1. Based on these effect sizes, we generated one averaged effect size for each study and then estimated the overall effect size across studies as well as potential effects of categorical moderator variables. As a result, each of the 12 studies only contributed one effect size to these main analyses. These results appear in Table 2.
Table 2.
Tests of categorical models of study characteristics in anxiety score changes a
| Categorical variables and relevant contrasts | k | N | d+ b | (95% CI) | Fail-safe N | Qw | Qb |
|---|---|---|---|---|---|---|---|
| All within study effect sizes averaged | |||||||
| 12 | 467 | 0.61 *** | (0.42-0.81) | 53.99 | 91.28 *** | ||
| Type of Participants | |||||||
| 1. Patient | 3 | 113 | 0.78 *** | (0.38-1.20) | 15.04 | 25.58 *** | |
| 2. Healthy subjects | 9 | 384 | 0.48 *** | (0.27-0.70) | 39.32 | 70.57 *** | |
| a. High anxious | 7 | 284 | 0.62 *** | (0.36-0.87) | 38.92 | 61.95 *** | |
| b. Non-High anxious | 2 | 70 | 0.36 n.s. | (-0.29-1.02) | 1.64 | 1.87 n.s. | |
| Contrast 1 (1 vs. 2) | 0.94 n.s. | ||||||
| Contrast 2 (2a vs. 2b) | 0.93 n.s. | ||||||
| Contrast 3 (1 vs. 2a) | 0.49 n.s. | ||||||
| Contrast 4 (1 vs. 2b) | 1.86 n.s. | ||||||
| Contrast 5 (1+2a vs. 2b) | 1.38 n.s. | ||||||
| Type of Outcome Measures | |||||||
| 1 Self-reported anxiety (state) c | 10 | 408 | 0.41 *** | (0.21-0.61) | 12.27 | 28.06 *** | |
| 2 Spielberger State Anxiety | 6 | 276 | 0.41 *** | (0.17-0.65) | 6.37 | 14.72 * | |
| 3 Self-reported anxiety (trait) = Spielberger Trait Anxiety | 7 | 236 | 1.06 *** | (0.75-1.37) | 73.49 | 97.20 *** | |
| 4 Social anxiety d | 4 | 219 | 0.33 ** | (0.06-0.60) | 2.55 | 3.21 n.s. | |
| 5 Generalized anxiety e | 2 | 53 | 0.93 *** | (0.36-1.50) | 7.28 | 0.93 n.s. | |
| 6 Self-reported anxiety f | 12 | 467 | 0.59 *** | (0.39- 0.77) | 58.79 | 107.33 *** | |
| 7 Self-reported depression g | 4 | 137 | 0.90 *** | (0.55-1.26) | 13.89 | 7.11 n.s. | |
| 8 Self-reported measures h | 12 | 467 | 0.63 *** | (0.44-0.83) | 55.95 | 91.75 *** | |
| 9 Clinician-assessed anxiety i | 3 | 113 | 0.92 *** | (0.53-1.32) | 12.73 | 8.54 * | |
| 10 Clinician-assessed depression j | 2 | 77 | 0.51 * | (0.06-0.97) | 3.12 | 0.10 n.s. | |
| 11 Clinician-asessed measures k | 3 | 113 | 0.95 *** | (0.55-1.35) | 12.48 | 6.98 * | |
| 12 All anxiety measures | 12 | 467 | 0.61 *** | (0.42-0.81) | 53.99 | 91.28 *** | |
| 13 All depression measures | 4 | 137 | 0.85 *** | (0.50-1.21) | 13.15 | 4.92 n.s. | |
| Contrast (2 vs. 3) l | 13.35 *** | ||||||
| Contrast (4 vs. 5) | 3.51 n.s. | ||||||
| Contrast (12 vs. 13) m | 1.83 n.s. | ||||||
| Type of Training Target Stimulus | |||||||
| 1. Face | 7 | 315 | 0.37 ** | (0.14-0.60) | 9.79 | 34.37 *** | |
| 2. Word | 5 | 152 | 1.29 *** | (0.92-1.67) | 45.79 | 38.71 *** | |
| Contrast 1 (1 vs. 2) | 18.19 *** | ||||||
| Type of Stimulus Location | |||||||
| 1. Top-Bottom | 8 | 343 | 0.79 *** | (0.56-1.03) | 55.50 | 78.48 *** | |
| 2. Left-Right | 4 | 124 | 0.21 n.s. | (-0.14-0.57) | 0.04 | 4.74 n.s. | |
| Contrast 1 (1 vs. 2) | 8.06 ** | ||||||
| Assessment followed by stressor exposure after Attention Bias Modification Treatment | |||||||
| 3 | 187 | 0.77 *** | (0.47-1.07) | 8.05 | 4.01 n.s. | ||
k, number of effect sizes; d+, effect sizes weighted by the reciprocal of their variances; CI, confidence interval; fail-safe n, the number studies with an effect size of “.00” needed to attenuate the average effect size below significance; Qw, test of within-category homogeneity; Qb, test of between-category homogeneity analogous to a pairwise comparison; other abbreviations as in Table 1.
Hedge’s d. Definition of categories for d: no effect (0 –.2), low effect (.2–.5), medium effect (.5–.8), and high effect (> .8).
Significant at p < .001.
Self-reported anxiety (state): STAI-S, BSPS, LSAS, SPAI, FNES, PSWQ, WDQ, HRSA, SPS, SIAS, SPQ.
Significant at p < .05.
Social anxiety includes Amir et al. (21): GSP, Klumpp and Amir (24): mild level social anxiety by LSAS, Amir et al. (19): high level social anxiety by LSAS, and Li et al. (26): social interaction anxiety by SIAS.
Significant at p < .01.
Generalized anxiety includes Amir et al. (20): GAD and Hazen et al. (18): pathological worry by PSWQ.
Self-reported anxiety combines the self-reported anxiety (state) and the self-reported anxiety (trait).
Self-reported depression: BDI or BDI-II.
Self-reported measures includes all self-reported measures whether they are for assessing anxiety or depression.
Clinician assessed anxiety includes: BSPS, LSAS, HRSA.
Clinician assessed depression: HAM-D.
Clinician assessed measures: BSPS, LSAS, HRSA, HAM-D.
In the Qb comparison between STAI-S and STAI-T, two sets of data from Amir et al. (20) and See et al. (29), which have effect sizes on both measures, were excluded because Qb analysis does not allow an overlap of data from the same sample across groups.
In the Qb comparison between All anxiety measures and All depression measures, four studies that have effect sizes on both [Amir et al. (20); Schmidt et al. (32); Hazen et al. (18); Amir et al. (21)] were excluded because of the reason that Qb analysis does not allow an overlap of data from the same sample across groups.
The primary analysis revealed a significant benefit of ABMT on anxiety measures, with a medium effect size (d = 0.61, p < 0.001, 95% CI = 0.42-0.81). This result also was supported by a relatively large fail-safe N = 54. Figure 2 shows standard differences in means and confidence intervals per study. This figure suggests the presence of three possible outliers with particularly large effects (28, 32). When the three studies are removed, the overall effect size is reduced but remains medium, d = 0.36 (k = 9, N = 372, p < 0.001, 95% CI = 0.15-0.57; Qw = 12.52, p = 0.13) with a fail safe N = 7.
Figure 2.
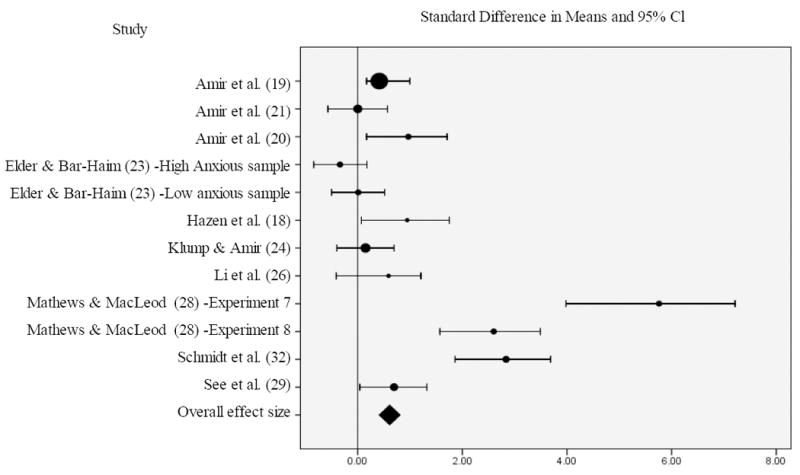
Size of round circle reflects sample size
Secondary analyses examined potential moderators (Table 2). When participants were divided into patients and healthy subjects, d was 0.78 (p < 0.001, 95% CI = 0.38-1.20) in patients, a medium to large effect size, and 0.48 in non-patients (p < 0.001; 95% CI=.27-.70). Nevertheless, Qb is non-significant. In the three studies employing stress exposure after ABMT, d was 0.77 (p < 0.001, 95% CI = 0.47-1.07), indicating a buffering effect of ABMT against stressor exposure. The d on trait-anxiety scales was significantly higher than that on state-anxiety scales (d = 1.06, p < 0.001, 95% CI = 0.75-1.37 vs. d = 0.41, p < 0.001, 95% CI = 0.17-0.65); Qb = 13.35, p < 0.001).
In categorical models, ABMT training procedures emerged as moderators. Here, studies using verbal target stimuli (words) generated a larger effect than those using face stimuli (d = 1.29, p < 0.001, 95% CI = 0.92-1.67 vs. d = 0.37, p < 0.005, 95% CI = 0.14-0.60; Qb = 18.19, p <.001). Similarly, studies using target stimuli presented in a top-bottom formation yielded a significant effect size, while those presented in a side-by-side formation did not (d = 0.79, p < 0.001, 95% CI = 0.56-1.03 vs. d = 0.21, p = 0.12, 95% Cl = -0.14-0.57; Qb = 8.06, p < 0.01). For continuous models, regression analysis considered age, sex, and extent of training; no moderators predicted ABMT effect on anxiety.
As with analyses treating anxiety symptoms as an outcome, analyses estimating the effect of ABMT on attention bias also yielded a significant effect, in this instance with a large overall effect size (d = 1.16, p < 0.001, 95% CI = 0.82-1.50). Table 3 presents results from categorical moderator analyses. Similar to the result for anxiety symptoms, studies using words generated a significant effect while those using face stimuli did not (d = 2.68, p < 0.001, 95% CI = 2.13-3.23 vs. d = 0.30, p = 0.08; Qb = 46.32, p <.001). Also, studies using target stimuli presented in a top-bottom formation yielded a larger effect than those presented in a side-by-side formation (d = 2.22, p <.001, 95% CI = 1.65-2.80 vs. d = 0.62, p < 0.01, 95% CI = 0.20-1.04; Qb = 19.37, p <.001). Finally, for continuous moderators, number of sessions significantly predicted ABMT’s effect on attention bias (β = 1.18, t = 37.33, p<0.05, 95% Cl = 0.54-1.10). Moreover, the correlation between magnitude of attention bias change and anxiety change across studies was large, though of trend level significance, r = 0.75, p = 0.052.
Table 3.
Tests of categorical models of study characteristics in attention bias changes
| Categorical variables and relevant contrasts | k | N | d+ a | (95% CI) | Fail-safe N | Qw | Qb |
|---|---|---|---|---|---|---|---|
| All within study effect sizes averaged | |||||||
| 7 | 207 | 1.16 *** | (0.82-1.50) | 78.11 | 98.95 *** | ||
| Type of Participants | |||||||
| 1. Patient | 0 | - | - | - | - | - | - |
| 2. Healthy subjects | 7 | 207 | 1.16 *** | (0.82-1.50) | 78.11 | 98.95 *** | |
| a. High anxious | 5 | 137 | 1.27 *** | (0.88-1.67) | 36.48 | 29.81 *** | |
| b. Non-High anxious | 2 | 70 | 0.84 *** | (0.16-1.51) | 43.16 | 65.40 *** | |
| Contrast 1 (2a vs. 2b) | 0.87 n.s. | ||||||
| Type of Training Target Stimulus | |||||||
| 1. Face | 3 | 84 | 0.30 n.s. | (-0.13-0.74) | 1.57 | 1.70 n.s. | |
| 2. Word | 4 | 123 | 2.68 *** | (2.13-3.23) | 77.53 | 50.94 *** | |
| Contrast 1 (1 vs. 2) | 46.32 *** | ||||||
| Type of Stimulus Location | |||||||
| 1. Top-Bottom | 3 | 83 | 2.22 *** | (1.65-2.80) | 34.03 | 12.48 ** | |
| 2. Left-Right | 4 | 124 | 0.62 ** | (0.20-1.04) | 44.99 | 67.10 *** | |
| Contrast 1 (1 vs. 2) | 19.37 *** |
Significant at P <.05.
Significant at P <.01.
Significant at P <.001.
n.s. =Not significant
Symbol: - = Not calculated.
Note: k = number of effect sizes; d+ = effect sizes weighted by the reciprocal of their variances; CI = confidence interval; fail-safe N = the number studies with an effect size of “.00” needed to attenuate the average effect size below significance. Qw = test of withih-category homogeneity; Qb = test of between-category homogeneity analogous to a pairwise comparison
Discussion
This review of 12 RCTs in 467 participants finds a statistically-significant medium effect of ABMT on anxiety with a relatively large fail-safe calculation. Thus, a significant beneficial effect still would be present even if 54 unpublished studies had produced null results. Given the early stage of research on ABMT, no head-to-head trials compare ABMT with established interventions. Indeed, the effect of ABMT on anxiety appears smaller than for SSRIs and CBT, which typically produce large effects (6-10).
In one sense, a difference in effect-size magnitude between ABMT and SSRIs or CBT may seem unsurprising. ABMT is a limited, focused intervention, in terms of clinician involvement. As a result, contributions to efficacy from staff contact, other non-specific factors, and expectancy are likely to be small in ABMT. In addition, SSRIs or CBT trials exclusively focused on clinical populations whereas the ABMT RCTs analyzed in the present report are mostly of nonclinical or subclinical populations. When isolating the ABMT RCTs conducted in clinical settings and with clinical samples (20, 21, 32), the effect sizes are comparable to those observed for CBT and SSRIs. Moreover, CBT often has been compared to conditions, such as wait-list control, which are poorly matched to the active treatment, in terms of non-specific treatment factors and expectancy (9, 10). The studies of ABMT typically involve tight experimental control in which all participants are exposed to the exact same cue stimuli, number of training/placebo trials, number of treatment sessions, and overall procedures. As a result, while the current data suggest that ABMT is probably inferior to SSRIs and CBT, they also suggest a possible applicability of ABMT to the overall management of anxiety.
The current analysis also showed a large effect size of ABMT in reducing threat-related attention bias, indicating that overall, the attention training protocols are effective. The correlation between effect sizes on attention bias change scores and on anxiety change scores was also large, suggesting that ABMT reduces anxiety via effects on attention bias. However, more studies are needed to reveal the mechanism underlying the effects of ABMT on anxiety.
Benefits of ABMT appear to emerge under various experimental conditions, in diverse samples, assessed with a variety of clinical response measures. This conclusion is supported by the analyses of heterogeneity in response (see Table 2). ABMT produced a greater effect on trait than state anxiety measures. This suggests that ABMT may target the more enduring aspects of anxiety. Similarly, procedural factors also predicted response: the nature of stimuli and their location moderated outcome. Specifically, studies that used a Top-Bottom stimulus presentation achieved better effects than those using a Side-by-Side presentation, as did studies that used words relative to pictures. Interestingly, extent of training moderated effects on attention bias but not anxiety symptoms. More work is needed to characterize the nature and robustness of these influences. In particular, given the relatively small number of studies, negative findings should be viewed particularly cautiously. However, research on ABMT as an evidence-based therapy remains immature, and well-controlled clinical RCTs are costly. As a result, future research may be shaped by results from these moderator analyses.
These data may shape therapeutics. If future RCTs yield positive results, ABMT and similar computer-based training regimens may be viable stand-alone treatments in patients who do not have access to CBT or SSRI treatment, or who are either are unwilling or incapable of undergoing such treatment. ABMT may also serve as a viable alternative for treatment of children with anxiety disorders. However, only three of the reviewed studies of ABMT were conducted in anxiety-disorder patients, and none examined children. While biased allocation of attention represents an important correlate of anxiety, it is only one of many cognitive biases (44); differences in attention bias between healthy and anxious subjects are only moderate in size (11); and a significant group of anxiety-disorder patients exhibit no biasing of attention. Adopting a personalized medicine approach, future ABMT studies might consider the magnitude and nature of patients’ biases before prescribing training protocols [see also (34)].
Future studies could also test the utility of ABMT as an adjunct to SSRIs or CBT, both of which show strong effects but fail to produce remission in many patients. While SSRIs or CBT target a broad array of biases, ABMT provides a more focused, targeted approach that might augment the impact of the other treatments on attention bias. Similarly, the finding in the current meta-analysis that verbal stimuli appear more powerful than pictures when attempting alter anxiety may implicate personalized information as a target for training. This, in turn, may provide targets for other computerized approaches, focused on various other biases to be altered by novel treatments in anxiety. Taken together, such views resonate with those emerging from neuroscience, emphasizing delineation of the unique substrates that underlie distinct forms of learning (45). In fact, beyond the clinical relevance of the findings reported in the current meta-analysis, the findings reported here also may usefully shape theoretical views on anxiety disorder pathophysiology and treatment.
In anxious patients, therapeutic goal-based learning may be achieved through deliberative teaching, verbal instruction, and guided experiences with threats. Each of these learning tasks is targeted by CBT. ABMT, on the other hand, represents a focused attempt to teach patients one specific skill, attention control. Available neuroscience literature suggests that attention control abilities reflect competencies in specific, dedicated neural architecture. Thus, brain imaging studies on individual differences in anxiety implicate perturbed subcortical engagement to threats presented relatively rapidly or outside the focus of attention (12-14). Prior work on other forms of learning, such as motor skill development, suggest that abilities moderated by subcortical pathways, such as habitual responses, may be most efficiently shaped through repeated exposures to specific, focused tasks, as occurs in ABMT, even without verbal instruction or deliberative teaching (8, 46). On the other hand, much like in motor learning (46), attention control also is likely to be shaped by multiple, convergent neural pathways. In the case of ABMT, available research implicates lateral expanses of prefrontal cortex in the control of attention (8). Consistent with these observational data, the only imaging study to examine the effect of ABMT found that training altered lateral frontal regions in healthy individuals, in tandem with attention biases (35). This suggests that both frontal-cortical and subcortical circuitry may be targeted by ABMT.
For various reasons, the review generates only tentative conclusions. Perhaps most importantly, the review is based in a relatively small number of studies, containing relatively few patients with anxiety disorders, performed by a limited number of research groups. Moreover, the available data, as illustrated by an asymmetrical funnel plot and variable effect sizes across the 12 experiments, suggest heterogeneity in treatment response and possibly some degree of outliers, though findings remained significant, albeit weakened, when the three findings with the strongest results were removed. Such patterns are not unusual in early research on promising novel treatments. Given the promising nature of these early results, the next few years may herald a growing series of RCTs evaluating ABMT as a treatment for anxiety disorders.
In closing, this meta-analysis indicates that ABMT shows promise as a novel treatment for anxiety disorders. These results emerge from an initial, small series of RCTs demonstrating greater benefits on anxiety from ABMT, relative to control-training regimens. Reflecting a translational approach, the ideas for ABMT emerge from a melding of cognitive and neuroscience theory over the past 20 years. These ideas generate novel procedures that may enhance currently available treatments focused on perturbed cognition. Given the role for perturbed cognition in many common, impairing psychiatric disorders, such an approach in the anxiety disorders may serve as a guide for developing other novel, learning based therapies in a range of conditions.
Figure 3.
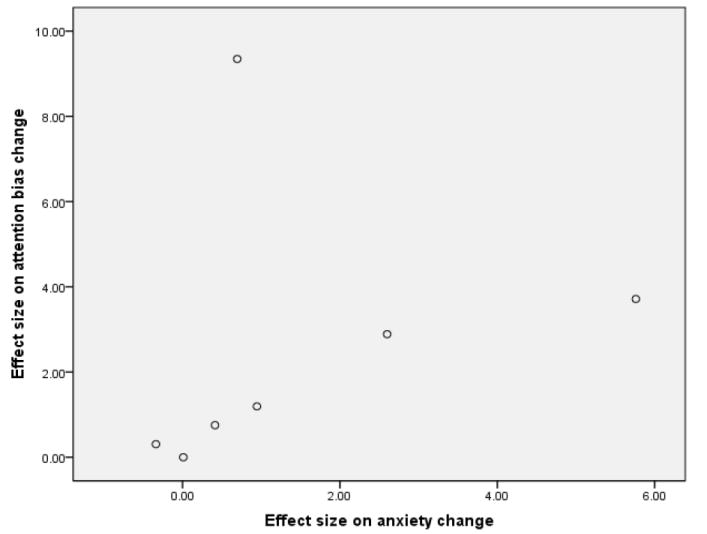
Spearman’s r = 0.75, p = 0.052.
Acknowledgments
Yuko Hakamata was a visiting fellow in the National Institute of Mental Health from 2009 to 2010. The stipend was supported by the Japan Society for the Promotion of Science. Sincere appreciation is extended to Dr. Yoshiharu Kim, Dr. Tetsuya Suhara, Dr. Haruhiko Shimoyama, Dr. Toshiya Inada, Dr. Yutaka Matsuoka, Dr. Masatoshi Inagaki, Dr. Kiyoto Kasai, Dr. Robert B. Innis, and Dr. Danny Pine for their help and support in this matter.
Footnotes
Dandeneau et al (36, 37) trained biased attention in healthy individuals using a visual search task. This procedure has also produced a promising effect in reducing anxiety. However, this procedure is quite distinct from a modified dot-probe task and thus we decided not to include these results in the meta-analyses.
Financial Disclosures All authors report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Canino G, Shrout P, Rubio-Stipec M, Bird H, Bravo M, Ramirez R, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry. 2004;61:85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- 2.Kessler R, Chiu W, Demler O, Merikangas K, Walters E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberts R, Roberts C, Xing Y. Rates of DSM-IV psychiatric disorders among adolescents in a large metropolitan area. J Psychiatr Res. 2007;41:959–967. doi: 10.1016/j.jpsychires.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler R, Barber C, Beck A, Berglund P, Cleary P, McKenas D, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ) J Occup Environ Med. 2003;45:156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- 5.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 6.Ballenger J. Remission rates in patients with anxiety disorders treated with paroxetine. J Clin Psychiatry. 2004;65:1696–1707. doi: 10.4088/jcp.v65n1216. [DOI] [PubMed] [Google Scholar]
- 7.Cartwright-Hatton S, Roberts C, Chitsabesan P, Fothergill C, Harrington R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. Br J Clin Psychol. 2004;43:421–436. doi: 10.1348/0144665042388928. [DOI] [PubMed] [Google Scholar]
- 8.Pine D, Helfinstein S, Bar-Haim Y, Nelson E, Fox N. Challenges in developing novel treatments for childhood disorders: lessons from research on anxiety. Neuropsychopharmacology. 2009;34:213–228. doi: 10.1038/npp.2008.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Otto M, Smits J, Reese H. Cognitive-behavioral therapy for the treatment of anxiety disorders. J Clin Psychiatry. 2004;65(Suppl 5):34–41. [PubMed] [Google Scholar]
- 10.Arch J, Craske M. First-line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatr Clin North Am. 2009;32:525–547. doi: 10.1016/j.psc.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg M, van IJzendoorn M. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Rauch S, Whalen P, Shin L, McInerney S, Macklin M, Lasko N, et al. Exaggerated amygdala response to masked facial stimuli in posttraumatic stress disorder: a functional MRI study. Biol Psychiatry. 2000;47:769–776. doi: 10.1016/s0006-3223(00)00828-3. [DOI] [PubMed] [Google Scholar]
- 13.Felmingham K, Kemp A, Williams L, Falconer E, Olivieri G, Peduto A, et al. Dissociative responses to conscious and non-conscious fear impact underlying brain function in post-traumatic stress disorder. Psychol Med. 2008;38:1771–1780. doi: 10.1017/S0033291708002742. [DOI] [PubMed] [Google Scholar]
- 14.Dickie E, Armony J. Amygdala responses to unattended fearful faces: Interaction between sex and trait anxiety. Psychiatry Res. 2008;162:51–57. doi: 10.1016/j.pscychresns.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 15.MacLeod C. Training selective attention: a cognitive-experimental technique for reducing anxiety vulnerability? World Congress of Behavioral and Cognitive Therapies Abstracts. 1995:118. [Google Scholar]
- 16.MacLeod C, Rutherford E, Campbell L, Ebsworthy G, Holker L. Selective attention and emotional vulnerability: assessing the causal basis of their association through the experimental manipulation of attentional bias. J Abnorm Psychol. 2002;111:107–123. [PubMed] [Google Scholar]
- 17.Koster E, Fox E, MacLeod C. Introduction to the special section on cognitive bias modification in emotional disorders. J Abnorm Psychol. 2009;118:1–4. doi: 10.1037/a0014379. [DOI] [PubMed] [Google Scholar]
- 18.Hazen RA, Vasey MW, Schmidt NB. Attentional retraining: A randomized clinical trial for pathological worry. J Psychiatr Res. 2009;43:627–633. doi: 10.1016/j.jpsychires.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Amir N, Weber G, Beard C, Bomyea J, Taylor CT. The Effect of a Single-Session Attention Modification Program on Response to a Public-Speaking Challenge in Socially Anxious Individuals. J Abnorm Psychol. 2008;117:860–868. doi: 10.1037/a0013445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amir N, Beard C, Burns M, Bomyea J. Attention Modification Program in Individuals With Generalized Anxiety Disorder. J Abnorm Psychol. 2009;118:28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amir N, Beard C, Taylor C, Klumpp H, Elias J, Burns M, et al. Attention training in individuals with generalized social phobia: A randomized controlled trial. J Consult Clin Psychol. 2009;77:961–973. doi: 10.1037/a0016685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eldar S, Ricon T, Bar-Haim Y. Plasticity in attention: Implications for stress response in children. Behav Res Ther. 2008;46:450–461. doi: 10.1016/j.brat.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 23.Eldar S, Bar-Haim Y. Neural plasticity in response to attention training in anxiety. Psychol Med. 2009:1–11. doi: 10.1017/S0033291709990766. [DOI] [PubMed] [Google Scholar]
- 24.Klumpp H, Amir N. Examination of vigilance and disengagement of threat in social anxiety with a probe detection task. Anxiety Stress Coping. 2009;22:283–296. doi: 10.1080/10615800802449602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krebs G, Hirsch C, Mathews A. The effect of attention modification with explicit vs. minimal instructions on worry. Behav Res Ther. 2009 doi: 10.1016/j.brat.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 26.Li SW, Tan JQ, Qian MY, Liu XH. Continual training of attentional bias in social anxiety. Behav Res Ther. 2008;46:905–912. doi: 10.1016/j.brat.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 27.MacLeod C, Soong L, Rutherford E, Campbell L. Internet-delivered assessment and manipulation of anxiety-linked attentional bias: validation of a free-access attentional probe software package. Behav Res Methods. 2007;39:533–538. doi: 10.3758/bf03193023. [DOI] [PubMed] [Google Scholar]
- 28.Mathews A, MacLeod C. Induced processing biases have causal effects on anxiety. Cogn Emot. 2002;16:331–354. [Google Scholar]
- 29.See J, MacLeod C, Bridle R. The Reduction of Anxiety Vulnerability Through the Modification of Attentional Bias: A Real-World Study Using a Home-Based Cognitive Bias Modification Procedure. J Abnorm Psychol. 2009;118:65–75. doi: 10.1037/a0014377. [DOI] [PubMed] [Google Scholar]
- 30.Wadlinger H, Isaacowitz D. Looking happy: the experimental manipulation of a positive visual attention bias. Emotion. 2008;8:121–126. doi: 10.1037/1528-3542.8.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harris L, Menzies R. Changing attentional bias: Can it effect self-reported anxiety? Anxiety Stress Coping. 1998;11:167–179. [Google Scholar]
- 32.Schmidt NB, Richey JA, Buckner JD, Timpano KR. Attention Training for Generalized Social Anxiety Disorder. J Abnorm Psychol. 2009;118:5–14. doi: 10.1037/a0013643. [DOI] [PubMed] [Google Scholar]
- 33.MacLeod C, Soong LY, Rutherford EM, Campbell LW. Internet-delivered assessment and manipulation of anxiety-linked attentional bias: validation of a free-access attentional probe software package. Behav Res Methods. 2007;39:533–538. doi: 10.3758/bf03193023. [DOI] [PubMed] [Google Scholar]
- 34.Bar-Haim Y. Attention Bias Modification (ABM): A Novel Treatment for Anxiety Disorders. J Child Psychol Psychiatry. doi: 10.1111/j.1469-7610.2010.02251.x. in press. [DOI] [PubMed] [Google Scholar]
- 35.Browning M, Holmes E, Murphy S, Goodwin G, Harmer C. Lateral Prefrontal Cortex Mediates the Cognitive Modification of Attentional Bias. Biol Psychiatry. 2009 doi: 10.1016/j.biopsych.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dandeneau S, Baldwin M. The inhibition of socially rejecting information among people with high versus low self-esteem: the role of attentional bias and the effects of bias reduction training. J Soc Clin Psychol. 2004;23:584–602. [Google Scholar]
- 37.Dandeneau S, Baldwin M, Baccus J, Sakellaropoulo M, Pruessner J. Cutting stress off at the pass: reducing vigilance and responsiveness to social threat by manipulating attention. J Pers Soc Psychol. 2007;93:651–666. doi: 10.1037/0022-3514.93.4.651. [DOI] [PubMed] [Google Scholar]
- 38.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 39.Schwarzer R. Meta-analysis programs, version 5.3. Berlin, Germany: 1989. [Google Scholar]
- 40.Johnson B. DSTAT: software for the meta-analytic review of research literatures, version 1.11. Hillsdale, NJ: Lawrence Erlbaum Associates; 1989. [Google Scholar]
- 41.Hedge L, Olkin I. Statistical methods for meta-analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- 42.Rosenthal R. Comment: assumptions and procedures in the file drawer problem. Psychol Bull. 1979;86:638–641. [Google Scholar]
- 43.Hedge L. Fixed effects models. In: Cooper H, Hedge L, editors. The handbook of research synthesis. New York: Russel Sage Foundation; 1994. pp. 285–299. [Google Scholar]
- 44.Beck A, Clark D. An information processing model of anxiety: automatic and strategic processes. Behav Res Ther. 1997;35:49–58. doi: 10.1016/s0005-7967(96)00069-1. [DOI] [PubMed] [Google Scholar]
- 45.Yin H, Knowlton B. The role of the basal ganglia in habit formation. Nat Rev Neurosci. 2006;7:464–476. doi: 10.1038/nrn1919. [DOI] [PubMed] [Google Scholar]
- 46.Balleine B, O’Doherty J. Human and rodent homologies in action control: corticostriatal determinants of goal-directed and habitual action. Neuropsychopharmacology. 2010;35:48–69. doi: 10.1038/npp.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]


