Abstract
Study Objectives:
First-line therapy for patients with moderate to severe obstructive sleep apnea (OSA) is positive airway pressure (PAP). Although PAP is a highly efficacious treatment, adherence to PAP is still a substantial clinical problem. The objective of this study was to determine whether PAP adherence can be improved with a telemedicine monitoring system.
Design:
A nonblinded, single-center, randomized controlled trial that compared standard PAP treatment versus PAP treatment and a telemedicine monitoring system
Setting:
University sleep disorders program in British Columbia, Canada
Patients:
Adult patients (≥ 19 yr of age) with moderate to severe OSA (apnea hypopnea index (AHI) ≥ 15 events/hr determined by polysomnography) prescribed PAP
Interventions:
Patients were randomized to either standard care with an autotitrating PAP machine or an autotitrating PAP machine that transmitted physiologic information (i.e., adherence, air leak, residual AHI) daily to a website that could be reviewed. If problems were identified from information from the website, the patient was contacted by telephone as necessary.
Measurements:
PAP adherence after 3 mo, subjective sleep quality, and side effects
Results:
Seventy-five patients were enrolled; 39 were randomized to telemedicine and 36 to standard care. The mean age ± standard deviation (SD) was 53.5 ± 11.2 yr, mean AHI was 41.6 ± 22.1 events/hr, and 80% of patients were male. After 3 mo, mean PAP adherence was significantly greater in the telemedicine arm (191 min per day) versus the standard arm (105 min per day; mean difference = 87 min, 95% confidence interval (CI): 25-148 min, P = 0.006, unpaired t test). On days when PAP was used, mean adherence was 321 min in the telemedicine arm and 207 min in the standard arm (difference = 113 min, 95% CI: 62-164 min, P < 0.0001). Significant independent predictors of adherence included age, baseline Epworth Sleepiness Scale score, and use of telemedicine. On average, an additional 67 min of technician time was spent on patients in the telemedicine arm compared with the standard arm (P = 0.0001).
Conclusions:
PAP adherence can be improved with the use of a web-based telemedicine system at the initiation of treatment.
Citation:
Fox N; Hirsch-Allen AJ; Goodfellow E; Wenner J; Fleetham J; Ryan CF; Kwiatkowska M; Ayas NT. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. SLEEP 2012;35(4):477-481.
Keywords: Obstructive sleep apnea, telemedicine, remote monitoring, adherence, positive airway pressure
INTRODUCTION
Obstructive sleep apnea (OSA) is a common disease characterized by recurrent collapse of the upper airway during sleep, leading to nocturnal hypoxemia, sleep fragmentation, and daytime hypersomnolence. Moreover, untreated OSA is associated with numerous adverse health and safety consequences including stroke, heart failure, cardiovascular disease, and motor vehicle crashes.1
First-line therapy for moderate to severe OSA is a positive airway pressure (PAP) machine, a portable device attached to the patient with a mask and plastic tubing that establishes positive pressure in the upper airway during sleep.2 Although PAP is highly effective in resolving upper airway collapse, a major clinical challenge is maximizing adherence with therapy. Many patients discontinue or do not use the device substantially. This is of clinical importance as increased adherence is associated with a reduced risk of motor vehicle crashes, improved cardiovascular outcomes, increased alertness, and improved quality of life.3–5 Optimizing adherence is thus an important aspect of patient management.
Adherence to PAP therapy is influenced by many factors, including severity of the disorder, side effects, therapeutic response, claustrophobia, patient's perception of disease seriousness, family support, and cost. Increased air leak with auto-PAP therapy is associated with reduced adherence,6 and general management with interventions such as heated humidification, mask optimization, and topical nasal therapy improves adherence.7 Adherence can also be significantly improved by a comprehensive support program and timely interventions by health professionals. This suggests that technical innovations that permit close monitoring of physiologic variables (such as air leak) during therapy and rapid troubleshooting of potential problems may improve adherence to PAP therapy.8
Telemedicine can be defined as “the use of information and communication technology to deliver health services, expertise and information over distance, geographic, time, social and cultural barriers.”9 Current technology enables PAP machines to monitor applied pressures, air leaks, apnea hypopnea index (AHI), and objective adherence, and to send this information by modem to the patient's healthcare provider on a daily basis. This system should allow early detection of problems with appropriate interventions thereby improving early experience with continuous positive airway pressure (CPAP), and potentially improving adherence. The primary purpose of this study was to determine whether such a telemedicine monitoring system could improve 3-mo PAP adherence in patients with moderate to severe OSA.
METHODS
We performed a single-center, randomized controlled trial of a telemedicine system versus standard care in patients with moderate to severe OSA. Patients were randomized to either standard care or telemedicine (1:1 ratio) using sequential numbered envelopes prepared by one of the authors (JW). The study was approved by the Clinical Research Ethics Board at the University of British Columbia. The study was registered prior to patient enrolment (ClinicalTrials.gov Identifier: NCT00561860).
Patients
Patients were recruited from adult (≥ 19 yr of age) patients with moderate to severe OSA (AHI ≥ 15 events/hr by polysomnography (PSG) using the Chicago scoring criteria for the determination of apneas and hypopneas, according to the American Academy of Sleep Medicine)10 diagnosed at the Sleep Disorders Program who were seen by one of three respirologists (JF, CFR, NTA) at the University of British Columbia (UBC) between April 8, 2008 to June 1, 2010. Patients with OSA who were prescribed PAP therapy by their regular sleep physician and who were willing to accept a trial of therapy were potentially eligible for the trial.
Patients were excluded from participating if they were unable or unwilling to provide informed consent, had active cardiopulmonary or psychiatric disease, had been previously treated for OSA, did not have a telephone line in their bedroom (necessary to transmit information by the modem), or could not return for follow-up visits.
Protocol
All patients were oriented to PAP during a 20-min session and fitted with a nasal or oronasal mask by the PAP coordinator from our clinic, who is a trained respiratory therapist with many years of experience with patients with sleep apnea. All patients were provided with a REMstar® Pro nasal CPAP device (Phillips Respironics Inc., Murrysville, PA). These types of machines are commonly used to treat patients with OSA. The autotitrating machine monitors patient airflow and adjusts pressure automatically to eliminate sleep apnea. Specifically, the machines were set to autotitrate at pressures between 6 and 16 cm H2O; this setting reflects our current clinical practice to allow for an adequate range of pressures. Patients were also provided with the telephone number of the PAP coordinator who could be contacted if any problems or questions arose.
Patients were then randomized to either standard care or telemedicine follow-up.
Standard care
Patients were contacted after 2 days to ask about progress and adherence, and to troubleshoot any problems with the machine. After 4-6 wk of therapy, patients returned to the clinic to see the PAP coordinator and their doctor, and information was downloaded from their machines. This information included a variety of physiologic variables, including PAP adherence, applied PAP pressure, mask leak, and residual respiratory events. Any problems with treatment were addressed at this time. After 8 wk, patients came to the research coordinator who downloaded the machine information. After 3 mo of treatment, information was downloaded from the machine and patients saw their sleep specialist. An Epworth Sleepiness Scale score and a variety of survey questions concerning side effects and sleep quality were completed (see next paragraphs).
Telemedicine
Identical to the standard pathway, all patients were oriented to CPAP, fitted with a mask, and given an autotitrating machine. A modem was attached to the PAP device (EncoreAnywhere®, Philips Respironics Inc.), and patients were instructed in its use by the research coordinator. The modem was programmed to send physiologic information directly to a web-based database across the telephone line each morning (PAP adherence, applied PAP pressure, mask leak, and residual respiratory events).
Patients were contacted by the research coordinator after 2 days to ask about progress and compliance, and to troubleshoot any problems with the machine. The research coordinator at UBC reviewed the downloaded information every weekday morning except holidays and contacted the patient if any of the following were present: mask leak > 40 L/min for greater than 30% of the night, < 4 hr of use for two consecutive nights, machine measured AHI > 10 events/hr, and 90th percentile of pressure > 16 cm H2O. The research coordinator called the patient and inquired about symptoms such as dry mouth, mask issues, discomfort with the device, or any other problems. If the only issue was low adherence due to lack of motivation, the research coordinator encouraged the patient to use PAP. Otherwise, the research coordinator would discuss the case with the PAP coordinator (the same person who helped care for the patient in the standard arm) and arrange for the patient to talk with or visit the PAP coordinator, depending on the responses from the patient and the physiologic data. Specific interventions to improve compliance that would be standard in our clinic (e.g., a different mask, chin strap, modifications of pressure settings, modifications of humidifier settings, saline nasal sprays) would then be prescribed.
After 4-6 wk of therapy, patients returned to the clinic to see their regular doctor and information was reviewed (including CPAP pressure, mask leak, residual respiratory events, and compliance). Any problems with treatment were also addressed at this time.
After 3 mo of treatment patients came to see their sleep specialist, who reviewed the data received via the modem. Surveys and Epworth Sleepiness Scale score (ESS) were completed (same as the standard group).
Surveys
At the end of 3 mo, patients were administered the ESS. This is a validated commonly used survey that assesses the degree of subjective daytime sleepiness. Scores range from 0 to 24, with a higher score indicating greater sleepiness. Patients were also asked to complete a variety of questions according to a visual analog scale. There was one question that assessed subjective sleep quality: “Overall, how satisfied were you with your quality of sleep on CPAP over the past mo? Place a mark on the line”. Patients were asked to mark a point on the line ranging from 0 (extremely dissatisfied) to 10 (extremely satisfied). Seven additional questions elicited information about side effects including frequency of awakenings, discomfort with the device, difficulty exhaling, mask leaks, dry mouth, nasal congestion, and difficulty falling asleep. These questions had a visual analog scale for every question, in which patients were asked to assess a score between 0 to 10, with a higher score representing a more favorable response.
Time spent with patients
We also recorded the amount of time our research coordinator or PAP coordinator spent with patients. Amount of time spent was written in a daily log sheet. This included time spent fitting masks, problem solving, talking with patients on the phone, meeting with patients, and reviewing downloaded or transmitted information.
Statistical analysis
The primary outcome was PAP adherence after 3 mo (min used per day), using an intention-to-treat approach (unpaired 2-tailed t-test). A variety of secondary outcomes were analyzed, including time spent with the patient, ESS, sleep quality, side effects, and adherence on days PAP was used. A multivariate linear regression analysis was also done to assess independent predictors of PAP adherence. SAS 9.2 (Cary, NC) was used for the analyses.
RESULTS
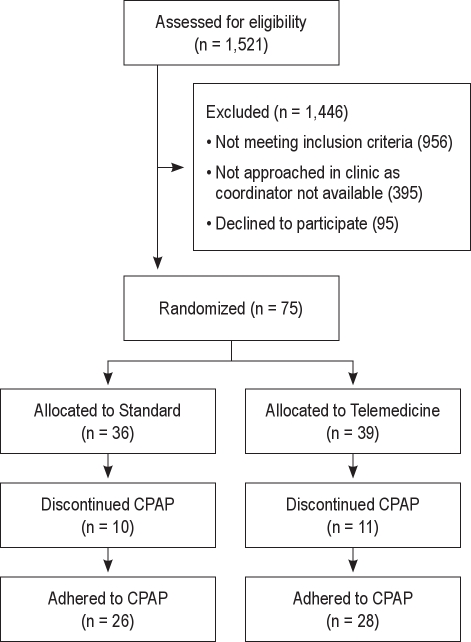
Over this time period, 1,521 patients were seen by these physicians. A flow chart of patient recruitment is shown in Figure 1. A total of 75 patients were enrolled in the study. Their mean age (± SD) was 53.5 ± 11.2 yr, and mean AHI was 41.6 ± 22.1 events/hr. Most of the patients were males. Patient characteristics are shown in Table 1. There was no significant difference in age, BMI, AHI, or ESS in the groups.
Figure 1.
Telemedicine study flow diagram.
Table 1.
Baseline characteristicsa
| Standard | Telemedicine | |
|---|---|---|
| Number of patients | 36 | 39 |
| % male | 77.8 | 82.0 |
| Mean age | 55.2 ± 11.5 | 52.0 ± 10.8 |
| Mean BMI | 32.6 ± 6.2 | 31.9 ± 5.0 |
| Mean AHI | 39.5 ± 19.6 | 44.3 ± 24.8 |
| Mean ESS | 9.7 ± 4.7 | 9.9 ± 5.0 |
Results are given as means ± SD.
AHI, apnea hypopnea index; BMI, body mass index; ESS, Epworth Sleepiness Scale Score.
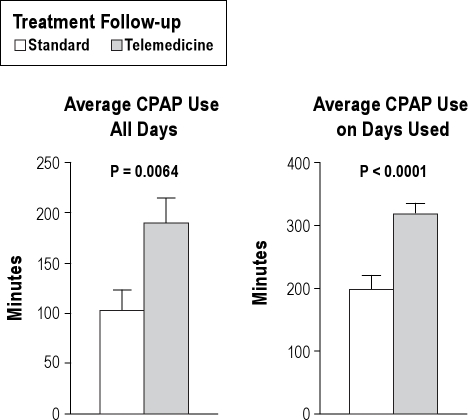
Overall, adherence to PAP was significantly greater in the telemedicine arm than in the standard arm (Table 2 and Figure 2). Specifically, patients in the telemedicine arm used PAP a mean of 191 min/day versus 105 min/day in the standard arm (mean difference = 87 min, 95% CI: 25-148 min, P = 0.006). Furthermore, on nights PAP was used, time used was much greater in the telemedicine arm (321 min/day) than in the standard arm (207 min/day) with a mean difference of 113 min/day (95% CI: 62-164 min, P < 0.0001). There was no significant difference in the percentage of nights PAP was used (46% versus 56% in the standard versus telemedicine arm). Mean AHI on treatment and change in ESS was similar in both groups.
Table 2.
Results of standard and telemedicine groupsa
| Standard | Telemedicine | P value | |
|---|---|---|---|
| Mean % days used | 45.9 ± 38.0 | 55.9 ± 40.0 | 0.19 |
| Mean adherence (min per day) | 105 ± 118 | 191 ± 147 | 0.006 |
| Mean adherence on nights PAP used (min per day) | 207 ± 106 | 321 ± 80 | < 0.0001 |
| Mean decrease in ESS | 0.7 ± 5.2 | 1.6 ± 5.1 | 0.49 |
| Mean AHI on treatment | 6.6 ± 4.8 | 4.7 ± 3.8 | 0.12 |
| Mean amount of time spent with patients (min over 3 mo) | 143 ± 48 | 210 ± 42 | < 0.0001 |
Results are given as means ± SD.
AHI, apnea hypopnea index; ESS, Epworth Sleepiness Scale Score; PAP, positive airway pressure.
Figure 2.
CPAP usage.
Patients with a greater ESS had improved CPAP compliance; however, significant differences still persisted between the standard and telemedicine arms. For instance, in patients with an ESS ≥ 11 (38 patients total), PAP adherence was 153 ± 122 min/day in the standard arm and 225 ± 137 min/day in the telemedicine arm (P = 0.035).
In univariate analyses, significant predictors of PAP adherence included increased age (P = 0.03), increased baseline ESS (P = 0.04), and use of telemedicine (P = 0.006). Sex and AHI were not significant predictors (P > 0.7). We then constructed a multivariate model using baseline ESS, age, and telemedicine use. All three variables were independently associated with daily adherence (Table 4).
Table 4.
Independent predictors of positive airway pressure adherencea
| Parameter Estimate (daily min of use) | P value | |
|---|---|---|
| Baseline ESS | 7.24* | 0.004 |
| Age | 3.96** | 0.02 |
| Telemedicine | 104.8 | 0.0007 |
A multivariate linear regression model was done to assess the independent effects of each of these three variables. ESS, Epworth Sleepiness Scale Score.
Increase in daily positive airway pressure (PAP) use for every 1-yr increase in ESS score.
Increase in daily PAP use for every 1-yr increase in age.
More time was spent with patients in the telemedicine arm. Over 3 mo, an average of 210 ± 42 min was spent with each patient in the telemedicine arm compared with 143 ± 48 min spent with patients in the standard arm (P < 0.0001) (Table 2). In other words, on average, an additional hour was spent with these patients over the 3-mo trial.
Results of the sleep quality and side effects surveys are shown in Table 3. Although side effects in general appeared to be less severe in patients in the telemedicine arm, none other than mouth dryness was statistically significant. Similarly, there was no significant difference in sleep quality.
Table 3.
Side effects and overall sleep qualitya
| Standard | Telemedicine | P value | |
|---|---|---|---|
| Side effects | |||
| Woken up frequently | 5.50 ± 2.5 | 5.79 ± 2.6 | 0.69 |
| CPAP discomfort | 4.41 ± 3.2 | 5.19 ± 2.8 | 0.34 |
| Difficulty exhaling | 4.80 ± 3.5 | 5.79 ± 3.0 | 0.27 |
| Mask leaks | 4.24 ± 3.0 | 5.08 ± 2.8 | 0.29 |
| Dry mouth | 4.16 ± 2.6 | 5.81 ± 2.3 | 0.01 |
| Nasal congestion | 5.88 ± 2.7 | 6.83 ± 2.4 | 0.16 |
| Difficulty falling asleep | 5.72 ± 3.5 | 6.22 ± 2.8 | 0.55 |
| Overall sleep quality | 5.13 ± 3.5 | 6.40 ± 2.7 | 0.13 |
Scores ranged from 0 to 10 with a larger number representing a more favorable response. Results are given as mean ± SD.
CPAP, continuous positive airway pressure.
DISCUSSION
In our single-center, randomized controlled trial, telemedicine monitoring improved PAP adherence at 3 mo in patients with moderate to severe OSA.
Telemedicine has been used in previous studies to promote and reinforce CPAP therapy; the results have been mixed. Taylor and colleagues randomized 114 patients to either a telehealth (intervention) arm or traditional care.11 In the intervention arm, a cognitive behavioral intervention was applied. Questions related to CPAP use and quality of sleep were sent to patients electronically. The patients' responses were monitored by a sleep medicine practitioner, and the patient telephoned if necessary. Adherence was not significantly different between the traditional and intervention groups (4.22 versus 4.29 hr per night; P = 0.87). Failure to show benefit may have been due to difficulties in contacting patients (sometimes delayed several days). Furthermore, the intervention only provided self-reported data to the healthcare provider; objective compliance and detailed physiologic information (as was used in our study) may have been more effective.
In a relatively small study, Smith and colleagues randomized 19 patients who were nonadherent with CPAP for 3 mo to either a telemedicine intervention or placebo.12 Both groups were scheduled for telehealth sessions with a nurse (14 30-min sessions over 12 wk) using a video teleconferencing system in the patient's home. The intervention group received specific advice about CPAP, whereas the placebo group had advice focused on a neutral health topic (i.e., vitamins). Although the numbers of patients were small, by the end of the study there was a significantly greater rate of adherence (90% versus 44%, P = 0.033) in the intervention group compared with the placebo group. In a small study by DeMolles et al., a computer telephone system in addition to usual care was used in 15 patients and compared to usual care only in another 15 patients.13 The group using the telehealth system had better CPAP adherence by the end of the study that trended to significance (4.4 versus 2.9 hr/night, P = 0.08).
Sparrow and colleagues report on the use of a telehealth intervention to improve CPAP adherence in a relatively large randomized controlled study (250 patients with sleep apnea).14 In the intervention arm, an automated telephone-linked communication (TLC) system was tailored to promote CPAP use and designed around the concepts of motivational interviewing. Every wk for the first month and every month thereafter, patients would telephone the system and report perceptions and experiences with OSA and CPAP (including compliance) over the previous week. Tailored feedback and counselling were provided by telephone to motivate patients to use CPAP. The control arm received general health information through the TLC system. At 12 months, median CPAP use was significantly greater in the intervention arm (2.98 hr/night versus 0.99 hr/night).
The potential mechanisms by which telemedicine improved adherence in our study is open to speculation. One possibility is that prompt attention to problems might have resulted in improved side effects. Consistent with this concept is the reduction in side effect complaints shown in the visual analog scales. However, the overall effect was fairly modest suggesting that other factors may also have been important. Another possibility is that the patients in the telemedicine arm, due to the daily monitoring, might have had a greater sense of accountability and were more motivated to not disappoint their healthcare providers (an extension of the Hawthorne effect). Future studies designed to ascertain how much of the effect is contributed from the monitoring of the physiologic variables, and how much from the prompt interventions (such as mask change, intranasal saline, steroid spray etc.) would be useful.
Although adherence was improved, on average more time was required to manage patients in the telemedicine arm. However, the overall magnitude of this was fairly minor (1 hr per patient), and we believe would be justified by the improved adherence.
Limitations
We acknowledge that there are many limitations to our study. First, only patients with moderate to severe disease were included in our study and our results cannot be extrapolated to patients with less severe disease. Second, this is a single-center study with a relatively modest number of patients. Reproducing these findings in other centers and patient populations would be important to demonstrate generalizability. Third, adherence in the standard care arm was relatively low (1.75 hr/night). However, this is similar to the adherence reported by the study by Sparrow et al.11 and other studies in the literature. Our low adherence might also have been explained by our low baseline ESS scores, suggesting that our patients were not particularly sleepy. In support of this concept, adherence was much greater in both treatment arms when only patients with a baseline ESS of 11 or greater were included. Fourth, we did not have a sham telemedicine control group (i.e., patients with the telemedicine device that was not being monitored by the investigators). Inclusion of such a control arm might have allowed us to determine whether the increased adherence might have been due to the perception of monitoring by the patients, or the more prompt institution of clinical interventions. A future study should also take into consideration both the monitoring of physiologic data (such as leak and nasal congestion), and the respective intervention (such as mask change, intranasal saline, steroid spray, etc.), to determine whether it was the monitoring alone or the interventions which may have contributed to the positive findings.
CONCLUSIONS
In our single-center study, adherence with PAP was improved with a web-based telemedicine monitoring system. Although these findings must be verified in other centers, adoption of this type of system could result in substantially improved care of patients with OSA.
DISCLOSURE STATEMENT
This study was partially supported by a research grant from Phillips Respironics Inc. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Al Lawati NM, Patel SR, Ayas NT. Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Prog Cardiovasc Dis. 2009;51:285–93. doi: 10.1016/j.pcad.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society 2011 guideline update: diagnosis and treatment of sleep disordered breathing. Can Respir J. 2011 Jan-Feb;18:25–47. doi: 10.1155/2011/506189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.George CF. Sleep. 5: Driving and automobile crashes in patients with obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004;59:804–7. doi: 10.1136/thx.2003.007187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 5.Weaver TE, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007 Jun 1;30:711–9. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valentin A, Subramanian S, Quan SF, Berry RB, Parthasarathy S. Air leak is associated with poor adherence to autoPAP therapy. Sleep. 2011 Jun 1;34:801–6. doi: 10.5665/SLEEP.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously noncompliant with continuous positive airway pressure. J Clin Sleep Med. 2007 Dec 15;3:706–12. [PMC free article] [PubMed] [Google Scholar]
- 8.Zozula R, Rosen R. Compliance with continuous positive airway pressure therapy: assessing and improving treatment outcomes. Curr Opin Pulmonary Med. 2001;7:391–8. doi: 10.1097/00063198-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Reid J. A telemedicine primer: understanding the issues. Billings, MT.: Innovative Medical Communications; 1996. [Google Scholar]
- 10.AASM. Sleep related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in adults. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 11.Taylor Y, Eliasson A, Andrada T, Kristo D, Howard R. The role of telemedicine in CPAP compliance for patients with obstructive sleep apnea syndrome. Sleep Breathing. 2006;10:132–8. doi: 10.1007/s11325-006-0059-9. [DOI] [PubMed] [Google Scholar]
- 12.Smith CE, Dauz ER, Clements F, et al. Telehealth services to improve nonadherence: a placebo-controlled study. Telemed J E Health. 2006;12:289–96. doi: 10.1089/tmj.2006.12.289. [DOI] [PubMed] [Google Scholar]
- 13.DeMolles DA, Sparrow D, Gottlieb DJ, Friedman R. A pilot trial of a telecommunications system in sleep apnea management. Medical Care. 2004;42:764–9. doi: 10.1097/01.mlr.0000132353.99209.fe. [DOI] [PubMed] [Google Scholar]
- 14.Sparrow D, Aloia M, DeMolles DA, Gottlieb DJ. A telemedicine intervention to improve CPAP adherence: a RCT. Thorax. 2010;65:1061–6. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]