Abstract
Severe autonomic failure occurs in about 1 in 1000 people. Such patients are remarkable for the striking and sometimes paradoxical responses they manifest to a variety of physiologic and pharmacologic stimuli. Orthostatic hypotension is often the finding most commonly noted by physicians, but a myriad of additional and less well-understood findings also occur. These include supine hypertension, altered drug sensitivity, hyperresponsiveness of blood pressure to hypo/hyperventilation, sleep apnea and other neurological disturbances are also frequently encountered.
In this article we will review the clinical pathophysiology that underlies autonomic failure, with a particular emphasis on those aspects most relevant to the care of such patients in the perioperative settings. Strategies used by clinicians to diagnose and treat these patients, and the impact of these interventions on the pre-operative, intra-operative, and post-operative care that these patients undergo is a crucial element in the optimized management of care in these patients.
Introduction
Severe autonomic failure occurs in about 1 in 1000 people 1.;2. Such patients are remarkable for the striking and sometimes paradoxical responses they manifest to a variety of physiologic and pharmacologic stimuli. Autonomic failure may be secondary to other diseases, such as diabetes mellitus, amyloidosis, or bronchogenic carcinoma; or be due to a primary autonomic disorder such as multiple system atrophy (MSA; Shy-Drager syndrome) or pure autonomic failure.
Here we will review the pathophysiology that underlies autonomic failure, with a particular emphasis on those aspects most relevant to the care of such patients in the perioperative and intraoperative settings. We will also discuss strategies that can be used to manage the symptoms of autonomic failure.
Proper functioning of the autonomic nervous system requires that both afferent and efferent limbs are intact. Afferent neurons detect changes in blood pressure, temperature, and the myriad of other vital processes controlled by the autonomic nervous system, and communicate these changes centrally; whereas the efferent neurons engage effector systems to perturb or restore homeostasis. Dysfunction of the afferent limb is typically associated with labile hypertension, as seen in baroreflex failure, particularly in the postoperative period after endarterectomy or other neck surgeries affecting the carotid sinus nerve3. Abnormalities of central autonomic pathways such as in patients with MSA, of efferent effector systems as in patients with pure autonomic failure, patients with deficiency of dopamine beta hydroxylase, or any combination thereof can all lead to clinical autonomic failure and disabling orthostatic hypotension.
Some of the most severely affected individuals have pure autonomic failure or multiple system atrophy. Such patients often have both extremely low blood pressures upright and extremely high blood pressures supine. Patients with MSA are perhaps the most vulnerable of all such patients to the complex and interacting responses to drugs and perturbations that occur during anesthesia.
Preoperative Evaluation of Autonomic Dysfunction
Common Features Associated with Autonomic Dysfunction
Orthostatic hypotension is the core feature of autonomic failure. Orthostatic hypotension is defined as a fall in blood pressure of 20/10 mmHg on standing for 3 minutes. This definition is meant to capture initial or mild cases. Symptomatic orthostatic hypotension is more commonly encountered in subjects with falls in blood pressure that may range from this figure to the severest cases where the fall in blood pressure may be 100/50 mmHg. The most common symptoms of orthostatic hypotension are lightheadedness, dimming/tunneling of vision, and discomfort in the head (typically occipital), neck, shoulders, and sometimes the chest. It can be accompanied by various neurological features in the case of MSA and Parkinson’s disease. Table 1 summarizes some of the seemingly trivial stimuli that can cause major blood pressure changes in autonomic failure. Other common clinical manifestations of autonomic failure include postprandial hypotension, urinary bladder dysfunction with urinary retention, decreased gastrointestinal motility (sometimes with severe constipation), and erectile dysfunction. Supine hypertension affects more than half of patients with autonomic failure; it induces pressure natriuresis, worsening orthostatic hypotension and often complicates management. Supine hypertension is characterized by an increase in peripheral vascular resistance. This is due to the residual sympathetic tone in patients with MSA, but the cause is not clear in patients with pure autonomic failure who have similarly increased vascular resistance despite very low levels of plasma norepinephrine and renin activity4;5. Due to absent or decreased baseline efferent neural traffic, autonomic failure patients may also manifest denervation hypersensitivity to norepinephrine. Denervation hypersensitivity results in hyper-responsiveness of vascular smooth muscles to the chemical mediator that normally activates it (in this case, norepinephrine), due in part to up-regulation of adrenergic receptors secondary to the low levels of plasma norepinephrine in autonomic failure 6;7.
Table 1.
Commonplace Stimuli that can Cause Blood Pressure Changes in Autonomic Failure
| Lowers blood pressure | Raises blood pressure |
|---|---|
| Standing | Lying supine |
| Food | Water ingestion |
| Hyperventilation | Hypoventilation |
| Straining (Valsalva) | Abdominal binding |
| Fever and heat | Coffee |
| Dehydration | Water immersion |
| Exercise | Head-down tilt |
Basic Evaluation of Patients with Autonomic Dysfunction
Basic evaluation of patients includes obtaining a detailed clinical history and examination, measurement of blood pressure and heart rate while supine, and again after one and three minutes of standing. A seated blood pressure can sometimes be useful for those patients who cannot stand for even 1 minute. More detailed autonomic function testing is usually performed in specialized centers, using multiples methods such as the following:
Orthostatic & tilt-table testing; blood pressure and heart rate are measured twice in the supine position. The patient then is instructed to stand for 5 minutes. Blood pressure and heart rate are again determined at 1, 3, and 5 minute of upright. In most cases of autonomic failure there may be little or no increase in heart rate even though the blood pressure may drop more than 50 mmHg on the upright position. Results from the tilt-table test in general are analogous but not identical to the orthostatic test. Although the tilt-table test offers little diagnostic advantage over carefully done upright hemodynamic data, many investigators use tilt because of its convenience and safety for the patient8.
The Valsalva maneuver is performed by blowing through a closed mouthpiece with a tiny leakage (16 gauge hole) to maintain 15 mmHg for about 15 seconds. It tests several components of the baroreflex arc. The cardiovascular response has been subdivided into four phases. During phase I, there is a transient increase in stroke volume and blood pressure secondary to the sudden increase in intrathoracic pressure being transmitted to the aorta. In phase II, as continued strained expiration is maintained, venous return is reduced and cardiac output falls. This produces a fall in blood pressure with reflex tachycardia. With the release of raised intrathoracic pressure, blood pressure abruptly falls during phase III. During phase IV, there is a marked rise in blood pressure that exceeds basal levels. This blood pressure overshoot is the result of both an increase in cardiac output and peripheral vascular resistance. In autonomic failure patients, the normal tachycardia in phase II is blunted or absent. The phase IV blood pressure overshoot seen in normal people also fails to occur in autonomic failure patients8.
The cold pressor test evaluates efferent sympathetic function. It is carried out by placing the hand in a basin filled with half ice and half water for about 1 minute. The normal average response is an increment of 20 mmHg in systolic blood pressure in response The blood pressure rise is blunted in patients with autonomic failure8.
Deep breathing evaluates the vagal function on heart rate modulation during slow inhalation for 5 seconds and exhalation for 5 seconds over 90 seconds. The sinus arrhythmia ratio of the longest to the shortest interval is attenuated in those with autonomic failure8.
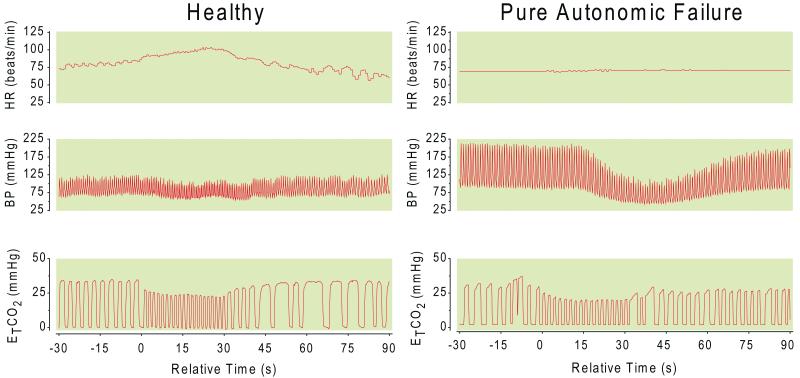
Hyperventilation tests the sympathetic response during deep and rapid one breath per second) breathing for 30 seconds to counteract the hypocapnea-induced systemic vasodilation. A significant fall in blood pressure indicates autonomic failure 8 (Figure 1).
Figure 1.
The effect of hyperventilation on a normal subject (panel B) and an autonomic failure patient (panel A). In response to hyperventilation the compensatory heart rate (channel 1) response is blunted despite the greater fall of blood pressure (channel 2) in autonomic failure patient compared to a control subject. The muscle sympathetic nerve activity (channel 3) is also diminished in autonomic failure compared to control.The frequency of respiratory rate (channel 4) is increased with hyperventilation. Channels from top to bottom, channel1= heart rate (HR; beats/minute), channel 2= blood pressure (BP; mmHg), channel 3= muscle sympathetic nerve activity (MSNA; burst/minute), channel 4= respiratory rate (resp.; breaths/minute).
Thermoregulatory Sweat Test and the Quantitative Sudomotor Axon Reflex Test both determine the sweat gland function and the integrity of efferent cholinergic sympathetic nervous system function. Sweating abnormalities are common in autonomic disorders; large areas of anhidrosis are found in patients with autonomic neuropathy due to various causes8.
Autonomic function testing can be especially important in asymptomatic patients with autonomic failure. Autonomic function testing can help to determine the severity and extent of the autonomic impairment, and hence aid in the anticipation of potential complications during anesthesia and surgery.
Clinical Features of Specific Autonomic Disorders
Table 2 lists some of the common causes of autonomic failure9,4,5. Although various causes of autonomic failure share common clinical features, the pathology is quite different and distinct in individual disorders. Some of the most severe forms of autonomic impairment are the neurodegenerative disorders commonly known as synucleinopathies4;10. They are characterized by aggregates of alpha-synuclein protein in the cytoplasm of neurons or glia. This group includes multiple system atrophy, and Lewy Body Disease (central autonomic failure). A related neurodegenerative disorder with isolated autonomic involvement is pure autonomic failure (peripheral autonomic failure). Parkinson’s Disease in certain cases has peripheral autonomic damage in additional to the central extrapyramidal disease. Distinction of multiple system atrophy in its earliest autonomic manifestation can be very difficult and is not currently always possible. Pharmacologically, patients with central autonomic failure (e.g. MSA) can sometimes be distinguished from peripheral autonomic failure (e.g. pure autonomic failure) by their response to imaging studies such as cardiac metaiodobenzylguanidine (MIBG) scan and olfactory function (usually normal in MSA, but abnormal in Parkinson’s Disease). Sometimes direct (norepinephrine or phenylephrine) and indirect (tyramine, that causes norepinephrine release from sympathetic neurons) sympathomimetics may also help. In peripheral autonomic failure, tyramine infusion produces only a small increase in blood pressure (due to peripheral neuronal damage), whereas norepinephrine infusion elicits an exaggerated pressor response (due to denervation hypersensitivity). Patients with central autonomic failure have a normal pressor response to tyramine and a lesser degree of denervation hypersensitivity11-15. Autonomic failure with profound orthostatic hypotension is the clinical hallmark of the rather rare pure autonomic failure. This is in contrast to MSA in which patients develop multiple neurological features, including Parkinsonism, cerebellar dysfunction and pyramidal signs. MSA is differentiated from Parkinson’s disease by the asymmetric resting tremor, the poor response to levodopa and the rapidly progressive nature of disease. Lewy Body Disease is defined by the coexistent Parkinsonism and progressive cognitive decline frequently accompanied by spontaneous recurrent visual hallucinations. Diabetic autonomic neuropathy complicates long-standing diabetes and has been linked to increased cardiovascular mortality. Apart from the common features of autonomic failure and widespread organ impairment, diabetic neuropathy is characterized by resting tachycardia and large fluctuations in blood glucose9.
Table 2.
Major Causes of Autonomic Failure
| Autonomic Synucleinopathies: |
| Multiple System Atrophy |
| A central nervous system cause of autonomic failure (with orthostatic hypotension) that may mimic some motor features of Parkinson’s Disease but is associated with a more rapid and dramatic course. |
| Parkinson’s Disease |
| A primary motor disease that can sometimes be associated with a peripheral autonomic neuropathy and orthostatic hypotension |
| Dementia with Lewy Bodies |
| A rapidly progressive dementia that is associated with a peripheral autonomic neuropathy and orthostatic hypotension. |
| Pure Autonomic Failure |
| A peripheral autonomic failure that occurs in older patients and can exist in isolation without motor neurological disorders. |
|
|
| Other Major Autonomic Disorders |
|
|
| Autoimmune Ganglionic Neuropathy |
| A form of autonomic failure caused by a loss of function antibody targeting of the alpha 3 subunit of the nicotinic receptor in autonomic ganglia. |
| Diabetic Autonomic Neuropathy |
| A peripheral autonomic neuropathy that can cause orthostatic hypotension, often in the setting of multiple other diabetic complications. |
| Familial Dysautonomia |
| An autosomal recessive developmental autonomic disease seen most commonly in Ashkenazi Jews. |
| Dopamine Beta Hydroxylase Deficiency |
| A rare genetic loss of the enzyme that is needed to convert dopamine to norepinephrine, so the patients lack both norepinephrine and epinephrine. |
| Amyloidosis |
| Amyloid protein deposition on autonomic neurons can cause autonomic failure with severe hypotension. |
| Drug-Induced Autonomic Dysfunction |
| Autonomic failure mimicked by drugs such as ganglionic blockers. |
| Spinal Cord Injury |
| Typically seen with cervical and thoracic spinal cord transections. |
Anesthetic Considerations for Patients with Autonomic Failure
Pre-operative knowledge of autonomic failure is of considerable importance in these patients. Pre-operative blood pressure is usually assessed in the seated position and is typically normal in patients with autonomic failure; supine and upright blood pressures, which would expose autonomic dysfunction, are not routinely determined. Ideally, blood pressure should be measured in the supine position and repeated after 1, 3, and 5 minutes of standing.
General Pre & Post Operative Treatment Strategies for Autonomic Failure
General management must focus on ensuring hemodynamic stability perioperatively with adequate hydration, maintenance of euvolemia, and optimization of pharmacologic treatment. Simple maneuvers such as raising or lowering the head of the bed have proven to be helpful in ameliorating orthostatic symptoms for patients with autonomic failure in the outpatient setting. Hypotension during anesthesia is readily responsive to small doses of the α1-adrenoreceptoragonist phenylephrine, especially in pure autonomic failure patients16-18.
Supine hypertension is particularly responsive to transdermal nitrates, although short-acting intravenous vasodilators/venodilators such as sodium nitroprusside or intravenous nitroglycerin may be better choice in extreme elevation of blood pressure to avoid profound hypotension. In one case report, the use of hydralazine for supine hypertension resulted in severe hypotension, that was corrected by vasopressin 19. Other agents that can be used judiciously for supine hypertension include intravenous dexmedetomidine and nicardipine20,21;22. Prolonged post-operative bed-rest and inactivity should be avoided, since they will worsen the already tenuous tolerance to standing.
Drugs used in the treatment of autonomic failure
Fludrocortisone
Fludrocortisone is a mineralocorticoid, which causes sodium retention and enhances the sensitivity of blood vessels to circulating catecholamines23. Most patients will need to gain about 1-2 kg of fluid in order to have the full benefit of this agent. Some of the benefit of fludrocortisone may be due to the support which increased interstitial fluid provides to the vasculature. Fluid overload is not generally a problem for patients with autonomic failure who are taking fludrocortisone. With more than 0.3 mg per day, some patients will experience a small amount of glucocorticoid effect, which might have unfavorable long-term consequences if they remain on the agent for many years. Fludrocortisone use can cause hypokalemia in up to 50% of patients, and hypomagnesemia in perhaps 10%. Chronically, blood volume is often supported with the use of fludrocortisone, a mineralocorticoid agonist that promotes renal sodium reabsorption. At higher doses, > 0.3 mg/qd, fludrocortisone can result in suppression of the hypothalamic-pituitary axis 2. Even though these higher doses of fludrocortisone rarely provide added benefit, they are often used. Thus, the risk of adrenal insufficiency from fludrocortisone therapy must be considered preoperatively in these patients.
Fludrocortisone may be useful in the 1-2 weeks before an elective procedure to optimize the volume status of a patient with profound autonomic failure 23. In the face of these weight changes, one might expect that fluid overload and pulmonary edema would commonly occur in autonomic failure patients taking fludrocortisones. In practice this is rarely seen, perhaps because weight gain beyond 2 kg is avoided, and also because seated or upright posture provides rapid relief if mild symptoms of shortness of breath begin to occur.
Midodrine
Midodrine is a prodrug that acts by stimulating alpha-1 adrenoreceptors to constrict blood vessels and raise blood pressure. The pressor effect of midodrine comes on within about 30 minutes and wanes after 4 or 5 hours. Other than excessive hypertension due to denervation hypersensitivity, the most troublesome side effect of midodrine is gooseflesh (chill bumps). This is due to the drug’s alpha-1 effect to cause hair to stand on end. Some patients experience this as a numbness or “strange” sensation in the scalp or neck. Midodrine may be a very useful agent for management of orthostatic hypotension in the perioperative period in patients with autonomic failure, although there are reports of excessive rise in the supine blood pressure of a patient taking midodrine preoperatively. In the latter case report the supine hypertension was corrected quickly with the reverse Trendelenburg position. In patients with preexisting supine hypertension, it might be safe to hold the drug perioperatively to avoid excessive rise in supine blood pressure24.
Pyridostigmine
Pyridostigmine is sometimes beneficial in autonomic disorders. Early studies showed that blood pressure was raised by anticholinesterase drugs whether they crossed the blood-brain barrier (physostigmine) or not (neostigmine) in autonomic failure patients. Pyridostigmine is now the most widely used drug of this class for this purpose. The drug has long been used for the treatment of myasthenia gravis by preventing the destruction of acetylcholine by acetylcholinesterase. Inhibition of acetylcholinesterase enhances sympathetic ganglionic neurotransmission particularly in the standing position, with lesser increase in supine blood pressure compared to other pressor25. The overall effect of pyridostigmine is a modest increase in upright blood pressure in patients with orthostatic hypotension. However, occasionally other aspects of autonomic failure such as constipation, urinary bladder dysfunction, and dryness of secretions may also be improved by this agent. This agent may be useful in the postoperative period for management of the symptoms of autonomic failure. However, the effect of an acetylcholinesterase inhibitor in the operating room may lead to unpredictably decreased or altered efficacy of neuromuscular blocking drugs. In addition, the beneficial effects of pyridostigmine in patients with autonomic failure, while notable, are not dramatic, and the medication can be held safely in most cases. Therefore, discontinuation of pyridostigmine in the preoperative period should be considered in patients with autonomic failure25.
Octreotide
Octreotide is a somatostatin analogue, which has significant effects on gastrointestinal hormones and the gastrointestinal tract. The pressor action of octreotide is probably mediated via splanchnic vasoconstriction and elevation of systemic vascular resistance, although an effect of augmenting cardiac output has also been reported26;27. At quite low subcutaneous doses, 12.5-25 mcg, it often elicits an increase in blood pressure in patients with autonomic impairment, sometimes with very little in the way of side effects. Following administration subcutaneously, drug effects appear within a few minutes and last for few hours. Almost all patients experience some increase in blood pressure if they have baseline autonomic impairment, but occasional patients experience increases in systolic blood pressure of 40 mmHg or more. Administration of the long-acting somatostatin analogue was associated with severe hypertension in one case report of diabetic autonomic neuropathy28. Excessively high doses may cause nausea or altered gastrointestinal motility. Gastrointestinal side effects are particularly prominent in patients with diabetes mellitus who can rarely tolerate octreotide for this reason26;29.
Atomoxetine
This drug inhibits the reuptake of norepinephrine by the norepinephrine transporter producing an increase in norepinephrine at the synapses of peripheral sympathetic neurons. In central autonomic failure (MSA), patients lack central modulation of sympathetic activity, and this translates into an increase in blood pressure even at pediatric doses of atomoxetine. Therefore it can be used to treat orthostatic hypotension very effectively in patients with central autonomic failure. Of note, this medication does not produce any increase in heart rate in patients with central autonomic failure despite its effect on blood pressure. In people with peripheral autonomic failure, the effect on blood pressure is minimal. The concomitant use of atomoxetine with a monoamine oxidase inhibitor may elicit especially large blood pressure elevations, but should only be undertaken with careful observation. Neuroleptic malignant syndrome also remains a theoretical possibility with these drug combinations and should be grounds for extreme caution30.
Acarbose
Patients with severe postprandial hypotension may benefit from the use of acarbose with meal ingestion. This alpha-glucosidase inhibitor is commonly used to treat postprandial hyperglycemia in type II diabetes mellitus because it decreases the absorption of glucose in the small intestine. This effect seems to blunt the secretion of some gut peptides that act as vasodilators and might be responsible for the hypotensive effect of meals. Patients may complain of abdominal cramps, or of unusual or foul-smelling stools. This is likely due to an increased production of butyrate by gut bacteria. Acarbose usually attenuates postprandial hypotension by 20 mmHg and accelerates the blood pressure recovery to baseline values31. Obviously, acarbose has no benefit for postprandial hypotension when patients nil per os perioperatively.
Droxidopa (L-DOPS, L-dihydroxyphenylserine)
Droxidopa is the treatment of choice for dopamine β-hydroxylase deficiency, a rare congenital form of severe orthostatic hypotension caused by complete absence of the enzyme required for the conversion of dopamine to norepinephrine which results in absence of both norepinephrine and epinephrine. Droxidopa is converted in one step into norepinephrine by dopa decardoxylase, an enzyme that is present in most tissues and sympathetic nerves. Droxidopa administration produces a moderate increase in blood pressure and a sustained dramatic relief of orthostatic symptoms32;33.
Drug Interactions with Autonomic Failure
Liver blood flow in human subjects is relatively posture dependent. In healthy subjects liver blood flow is only reduced 5% in the seated posture as compared to the supine posture. In patients with autonomic failure, the liver blood flow can decrease as much as 30% with upright posture. A consequence of this is that a hepatically cleared drug like lidocaine, may display plasma levels that are dramatically posture and blood pressure dependent. When patients with orthostatic hypotension are receiving intravenous lidocaine, the plasma drug levels are almost twice as high when they are seated vs. supine, and this change in posture can occasionally result in a toxic seizure despite an unchanged infusion rate34.
The response to various cardiovascular vasodepressor drugs also may be exaggerated, while the response to other vasoactive agents is unpredictable13;14.Tyramine infusion results in a slight increase in blood pressure in pure autonomic failure and normal pressor response in MSA, whereas norepinephrine infusion elicits an exaggerated pressor response in pure autonomic failure11-15. Ephedrine is another sympathomimetic agent with lesser effect on blood pressure increase due to mixed stimulation of α1, β1 and β2 adrenergic receptors 35. In addition to blood pressure effect, there is a concurrent increase in mean heart rate mediated by β1-receptors stimulation36. Due to its mechanism of action that includes release of norepinephrine from the postganglionic neurons, this agent might only be effective in patients with residual sympathetic activity and capacity to release norepinephrine. Clonidine has a paradoxical action in the severest cases of pure autonomic failure, instead of the typical central sympatholytic effect and blood pressure reduction. The stimulation of the postsynaptic α2-adrenergic and possibly some α1-adrenergic receptors may predominate over the presynaptic receptors on the norepinephrine-depleted neurons. Therefore, doses above 0.2 mg clonidine can occasionally increase blood pressure significantly37. Table 3 lists the responses to some drugs in autonomic failure patients.
Table 3.
Drugs with Unusual Effects in Autonomic Failure
| Drugs | Effects |
|---|---|
| Pressor effect | |
| Phenylephrine | Markedly increases blood pressure (even eye drops) 14 |
| Norepinephrine | Markedly Increases blood pressure |
| Vasopressin | Markedly Increases blood pressure 63 |
| Atomoxetine | Excessive pressor effect (~25 mmHg) in MSA but not pure autonomic failure |
| Octreotide | Low dose (12.5mg) may increase blood pressure for several hours |
| Saline | Increases blood pressure |
| Oxymetazoline | Increases blood pressure |
| NSAID (indomethacin) | Increases blood pressure by 5-30 mmHg64 |
| Ephedrine | Increases blood pressure 35 |
| Clonidine | High dose (> 0.4 mg) paradoxically increases rather than lowers blood pressure 65. |
|
| |
| Depressor effect | |
| Salbutamol/terbutaline | Can reduce supine systolic blood pressure up to 50%66 |
| Insulin IV | Decreases blood pressure Tizanidine Depressor first, then pressor (overshoot) when drug levels are gone |
| Propranolol | Usually little effect on blood pressure |
| Narcotics/Barbiturates | Depressor |
| Atropine | Large IV dose (3mg) may transiently decrease blood pressure because of the drug’s small α-1 antagonist effect, especially if α agonist is being administered. |
| Dexmedetomidine | Blood pressure fall may not always occur |
| Dopamine | May be depressor |
| Nitrates | Depressor effect, with significant blood pressure drop |
|
| |
| Chronotropic effect | |
| Isoproterenol | 6 fold β-1 hypersensitivity and 17 fold β-2 hypersensitivity66 |
| Epinephrine | Increases heart rate more than blood pressure -may be depressor |
| Pindolol | Increases HR 5-20 beats/min with mild elevation of blood pressure |
|
| |
| Miscellaneous effect | |
| Lidocaine | Toxic levels and seizures if plasma levels increase with posture change |
HR, heart rate; MSA, multiple system atrophy; NSAID, non-steroidal anti-inflammatory drug.
Special Considerations in Intraoperative Clinical Management
Airway Management
Several features related to the pathophysiology of autonomic failure may complicate airway management in the anesthetic care setting. Impaired gastrointestinal motility should be taken into consideration when approaching airway management. Rapid sequence induction should be considered. Patients with MSA have muscle rigidity similar to patients with Parkinson’s disease which may make intubation difficult. Vocal cord paralysis due to laryngeal muscle dysfunction38;39 may be seen in central autonomic disorders such as MSA. As with any structural or functional disorder involving the vocal cords or glottic apparatus, this can result in difficult endotracheal intubation. Oshima reported a transient deterioration in laryngeal function following anesthesia in a patient with MSA, resulting in complete glottic obstruction and sudden death40. The combination of impaired gastrointestinal motility and laryngeal dysfunction make aspiration a particular concern in these patients.
Apnea in autonomic failure patients, either due to upper airway obstruction (such as that seen in obstructive sleep apnea) or due to impaired central regulation of respiration, could be aggravated post-operatively. One author has postulated that the observed respiratory depression in autonomic failure was likely due to disordered central control of respiration during anesthesia rather than extreme respiratory center sensitivity to the anesthetic agent41. In addition to hypoxemia, apnea in these patients can have significant effects on blood pressure due to the resulting hypercapnea. The effect of hypercapnea on blood pressure should also be taken into consideration when titrating opioids or other respiratory depressants in the operating room and post-operatively40;42;43.
Gastrointestinal Function& Food Ingestion
Impaired gastrointestinal motility may impair gastric emptying. Autonomic failure patients should be treated as if they have a full stomach. Gastroparesis in autonomic failure can predispose to aspiration upon induction of anesthesia 44;45.Constipation, due to decreased gastrointestinal motility, and fecal incontinence are common in patients with autonomic failure, this may result in inadequate bowel preparation for colon surgery. Use of narcotics postoperatively may exacerbate the already sluggish intestinal motility and result in intestinal pseudo-obstruction and toxic megacolon. Additionally, distension of the rectosigmoid portion of the lower intestinal tract may worsen urinary retention. For these reasons, it may be prudent to minimize postoperative narcotics, though not at the expense of adequate pain control 46;47.
Food ingestion can induce profound hypotension even in the supine position in patients with autonomic failure, especially with carbohydrate-rich meals 48. While this is often not an issue preoperatively for elective procedures, it may be of particular concern in the recovery room for same-day procedures, as patients are often given food and drinks that are high in carbohydrates to assess their ability to tolerate oral intake prior to discharge. Conversely patients with supine hypertension may ingest food to attenuate the excessive blood pressure elevation.
Blood Pressure & Volume Control
While orthostatic hypotension may not be evident in the operating room, the interventions associated with anesthetic management disturb cardiovascular equilibrium even in healthy individuals. The maintenance of baroreflex control of the circulation serves as a crucial counter-regulatory mechanism in the face of surgical blood loss. Anesthetic agents can suppress the residual capacity to release catecholamines and can induce diminished baroreflex gain, which further compromises the pressor response during surgery18;49-52. The magnitude of these changes can be greatly enhanced in patients with efferent baroreflex impairment due to their inability to buffer changes in blood pressure. Furthermore, denervation hypersensitivity makes the pressor response to norepinephrine and its analogues very unpredictable.
In addition, a seeming paradox (but evidently part of the pathophysiology of dysautonomia) is that ~50% of our patients also have supine hypertension, often with systolic blood pressure >200 mmHg. These elevated pressures occur in spite of extremely low levels of both plasma norepinephrine and plasma renin activity53. Even minor physical and pharmacological perturbations in these patients may [increase or decrease] blood pressure and/or cardiac output to dangerous levels.
The loss of cardiovascular reflexes in autonomic failure can complicate anesthesia and predispose patients to life threatening changes in blood pressure54. The volume status of the patient is one of the most important factors in determining hemodynamic stability in autonomic failure patients. Consequently, acute changes in blood volume (such as may be seen with rapid saline infusion or with rapid blood loss) can result in a substantial rise or fall in blood pressure. A relatively fixed heart rate in response to cardiovascular stimuli is characteristic in these patients. Bradycardia in patients with autonomic failure may not respond to atropine (since vagal tone is already diminished in these patients), and alternatives such as isoproterenol or a temporary pacemaker can be life-saving. Supine hypertension is present in more than half of autonomic failure patients. While it may complicate surgery when patients are supine, it usually responds to changing position (reverse Trendelenburg) or judicious use of anti-hypertensive agents such as transdermal or intravenous nitroglycerin without causing unwanted hypotension. Prone position during surgery as an alternative to the traditional supine one is known to obstruct venous return and may result in hypotension55. Supine hypertension has been noted to be especially prominent in patients taking midodrine. Omitting midodrine or other acute pressor agents the day of the surgery should be considered24.
Ventilatory Management
The inability of patients with autonomic failure to increase cardiac output through sympathetic activation makes them exquisitely sensitive to the effects of positive pressure ventilation on venous return and cardiac output. Similarly, these patients may be less tolerant of the pneuomoperitoneum associated with laparascopic procedures. Using smaller tidal volumes and volume loading to control hypotension would be appropriate management.
In patients with autonomic failure, hyperventilation and the resulting decrease in blood carbon dioxide levels causes a rapid fall in blood pressure, sometimes ≥40 mmHg within 60 seconds42. Conversely, hypercapnea (such as can be seen with hypoventilation or increased dead space ventilation) can rapidly raise blood pressure 20 mmHg or more43. In fact, some autonomic failure patients are able to increase their tolerance of upright posture by increasing dead space ventilation as by breathing through a length of tubing 56. These observations imply that blood pressure in patients with autonomic failure can at least partially be modulated by manipulation of minute ventilation.
Response to Infection
Patients with severe autonomic failure respond to infection with an acute fall in blood pressure and a greatly reduced functional capacity of standing and ambulation. Such infections are most commonly in the urinary tract or the lungs. If a patient with autonomic failure experiences greater than usual blood pressure lability, new-onset recurrent syncope, or an acute decrease in performance status, a search should be undertaken for occult infection, with emphasis on evaluation for urinary tract infection or aspiration pneumonia. Suspicion for urinary tract infection should be especially high because urinary bladder dysfunction and chronic urinary retention is part of autonomic failure.
Temperature regulation
Patients with autonomic failure often lose the ability to sweat. Early on in the clinical course, this can be patchy, and paradoxically present as apparent “increased sweating” in less involved areas such as the head and neck. Impaired perspiration can lead to an inability to dissipate heat adequately. When patients are exposed to hot weather, this may be a problem. This could also contribute to a persistent high fever postoperatively. This increase in body temperature can cause a fall in blood pressure that is accompanied by a feeling of extreme fatigue. The patient may only be able to tolerate this temperature for a few minutes. Contemporary operating rooms have carefully controlled temperatures, but with aggressive warming measures (e.g., heavy bedding of the patient with blankets, use of convective air warmers, and heated IV fluids) temperature elevation may sometimes occur and lead to thermally induced hypotension. Conversely, the inability of patients with autonomic failure to vasoconstrict in response to a cool environment may result in excessive heat loss and hypothermia57. The lack of thermoregulatory vasoconstriction is specially reported in diabetic neuropathy patients, it predisposes patients to intraoperative hypothermia, excessive blood loss and postoperative infections 58.
Afferent Baroreflex Failure
Multiple clinical disorders can result in baroreflex failure such as accidental trauma, trauma either from unilateral or bilateral carotid endarterectomyor additional surgical therapy for pathology in the relevant anatomic areas, local tumor growth (carotid body tumor), and brain stem stroke are all recognized causes of baroreflex failure. Radiation therapy of head and neck carcinoma may also have the side effect of damage to cranial nerves, although this can occur months to years after the irradiation3.
Acute baroreflex failure clinically resembles pheochromocytoma more than it does autonomic failure, and excursions of systolic blood pressure to 320 mmHg or more is sometimes seen during stress. The blood pressure in these individuals is sensitive not only to usual perturbations of pain, anxiety, anger, and stress, but also to what would for others be a minor stress, such as exposure to bright light, sudden noise, or the appearance of the physician at the patient’s door. The headache accompanying these large elevations in blood pressure sometimes places patients in a position to develop their own intuitive biofeedback-based mechanisms to lower blood pressure. Some sensitive patients find that sunglasses can prevent headaches due to exposure to sunlight.
When baroreflex impairment is due to disturbance of transmission up the vagal and glossopharyngeal nerves, there may also be complete loss of parasympathetic function. This results from the close physical relation of the afferent baroreflex nerves in the vagus and glossopharyngeal nerves, and efferent vagal nerves. However, certain individuals have intact efferent parasympathetic control so that stress can be fully appreciated and expressed in terms of both blood pressure and heart rate3;59. In this disorder, selective baroreflex failure, blood pressure and heart rate may fall quite low during sedation or sleep, sometimes with sinus arrest for several seconds, and pacemaker placement may become necessary.
Choice of Anesthesia in Autonomic Failure
Currently, there are no systemic studies that looked at the preference of general versus regional anesthesia in autonomic failure patients. Most of the information is based upon individual case reports. Dose requirement of local anesthetic for adequate level of anesthesia was reported to be higher in autonomic failure patients 49;60, although this finding has not been consistent in all case reports 61. Marked hypotension can complicate spinal anesthesia in autonomic failure; it is usually preventable by adequate perioperative fluid replacement 16;62. Postural hypotension may develop during placement of the spinal anesthesia in the sitting position 60, which requires special attention. Bevan has concluded that the choice between regional and general anesthesia is less important than adequate volume replacement and hemodynamic monitoring16. Table 4 summarizes the preoperative intraoperative and postoperative aspects of dysautonomias and anesthesia.
Table 4.
Summary of Anesthesia Implications
| Preoperative factors |
|
|
| Patients orthostatic hypotension with or without supine hypertension |
| Be aware of gastroparesis and aspiration risk |
| Be aware of blood volume status for the conduct of anesthesia |
| Be aware of slight anemia due to reduced erythropoiesis |
| Consider holding oral vasopressors to prevent drug interactions intraoperatively |
|
|
| Intraoperative factors |
|
|
| General versus regional anesthesia choice would be dependent on procedure type |
| Patients require adequate monitoring and constant vigilance |
| Hypothermia and hyperthermia are both risks with poor thermal regulation |
| Intubation may require rapid sequence with cricoid pressure |
| Patient positioning may have significant effects on vital signs |
| Nitroglycerine, prone positioning or reverse trendelenberg can be used for supine hypertension |
| Sudden blood volume changes may precipitate untoward blood pressure response (rapid infusions or rapid blood loss) |
| Pneumoperitoneum should be applied with extreme caution or avoided if possible |
| Vasopressors and Inotropes can have resistance or undue sensitivity (See Table 3.) |
| Abnormal electrolyte values affect responses to medications |
|
|
| Postoperative factors |
|
|
| Anticipate volume changes in the postoperative period and observe with a higher level of care |
| Orthostatic hypotension requires good blood volume and assistance with first ambulation |
| Abnormal electrolyte values affect responses to medications |
| Thermal regulation may be an issue in the recovery period |
| Ileus can be worsened by opiate use in the postoperative period |
| Restart home dysautonomia medications before discharge |
Summary
Autonomic failure patients are a special population with significantly perturbed homeostatic responses to normal physiological and environmental stresses. Postural hypotension is the chief and most disabling symptom, but other neurological disturbances are frequently encountered. Preoperative management of autonomic failure requires careful evaluation and control of blood volume. The absence of compensatory mechanisms exaggerates the response to vasoactive and cardiac depressant agents. The decision to withhold or continue medications perioperatively should be individualized and tailored for each patient.
Intraoperatively patients need careful and attentive monitoring and are at risk for hypertension or hypotension with volume stimuli and also with positioning. Temperature regulation can result in hyperthermia or hypothermia and should be controlled for during either event. Postoperatively, orthostatic hypotension control necessitates the use of volume expansion, postural training and occasionally vasoconstrictors. Patients should be placed on home medications for dysautonomia before discharge.
Acknowledgments
Supported by P01 HL056693 (DR), R01 HL071784 (DR), K23 RR020783 (SRR), the Vanderbilt CTSA (UL1 RR024975), and the Autonomic Diseases Clinical Research Consortium U54 NS065736 (DR), all from the National Institutes of Health, Bethesda MD, USA.
Footnotes
Conflicts: No conflicts of interest to disclose.
Attestation: Study design, data collection, data analysis, manuscript preparation
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Shibao C, Grijalva CG, Raj SR, Biaggioni I, Griffin MR. Orthostatic hypotension-related hospitalizations in the United States. Am.J.Med. 2007;120:975–80. doi: 10.1016/j.amjmed.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein DS, Holmes C, Frank SM, Dendi R, Cannon RO, III, Sharabi Y, Esler MD, Eisenhofer G. Cardiac sympathetic dysautonomia in chronic orthostatic intolerance syndromes. Circulation. 2002;106:2358–65. doi: 10.1161/01.cir.0000036015.54619.b6. [DOI] [PubMed] [Google Scholar]
- 3.Robertson D, Hollister AS, Biaggioni I, Netterville JL, Mosqueda-Garcia R, Robertson RM. The diagnosis and treatment of baroreflex failure. N.Engl.J.Med. 1993;329:1449–55. doi: 10.1056/NEJM199311113292003. [DOI] [PubMed] [Google Scholar]
- 4.Robertson D. The pathophysiology and diagnosis of orthostatic hypotension. Clin.Auton.Res. 2008;18(Suppl 1):2–7. doi: 10.1007/s10286-007-1004-0. [DOI] [PubMed] [Google Scholar]
- 5.Jordan J, Biaggioni I. Diagnosis and treatment of supine hypertension in autonomic failure patients with orthostatic hypotension. J Clin Hypertens (Greenwich) 2002;4:139–45. doi: 10.1111/j.1524-6175.2001.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones R, Vrbova G. Two factors responsible for the development of denervation hypersensitivity. J.Physiol. 1974;236:517–38. doi: 10.1113/jphysiol.1974.sp010450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies B, Sudera D, Sagnella G, Marchesi-Saviotti E, Mathias C, Bannister R, Sever P. Increased numbers of alpha receptors in sympathetic denervation supersensitivity in man. J.Clin.Invest. 1982;69:779–84. doi: 10.1172/JCI110516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson David, Biaggioni Italo. Disorders of the Autonomic Nervous System. 1st edn Harwood academic publishers; 1995. pp. 112–21. [Google Scholar]
- 9.Freeman R. Clinical practice. Neurogenic orthostatic hypotension. N.Engl.J.Med. 2008;358:615–24. doi: 10.1056/NEJMcp074189. [DOI] [PubMed] [Google Scholar]
- 10.Robertson D, Beck C, Gary T, Picklo M. Classification of autonomic disorders. Int Angiol. 1993;12:93–102. [PubMed] [Google Scholar]
- 11.Bannister R, Davies B, Holly E, Rosenthal T, Sever P. Defective cardiovascular reflexes and supersensitivity to sympathomimetic drugs in autonomic failure. Brain. 1979;102:163–76. doi: 10.1093/brain/102.1.163. [DOI] [PubMed] [Google Scholar]
- 12.Bevan DR, Monks PS, Calne DB. Cardiovascular reactions to anaesthesia during treatment with levodopa. Anaesthesia. 1973;28:29–31. doi: 10.1111/j.1365-2044.1973.tb00280.x. [DOI] [PubMed] [Google Scholar]
- 13.Davies B, Bannister R, Sever P, Wilcox C. Pressor Actions of Noradrenaline, Angiotensin-Ii and Saralasin in Chronic Autonomic Failure Treated with Fludrocortisone. Br J of Clin Pharmacol. 1979;8:253–60. doi: 10.1111/j.1365-2125.1979.tb01011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robertson D. Contraindication to the Use of Ocular Phenylephrine in Idiopathic Orthostatic Hypotension. Am J of Ophthalmol. 1979;87:819–22. doi: 10.1016/0002-9394(79)90361-1. [DOI] [PubMed] [Google Scholar]
- 15.Ziegler MG, Lake CR, Kopin IJ. The sympathetic-nervous-system defect in primary orthostatic hypotension. N.Engl.J.Med. 1977;296:293–7. doi: 10.1056/NEJM197702102960601. [DOI] [PubMed] [Google Scholar]
- 16.Bevan DR. Shy-Drager syndrome. A review and a description of the anaesthetic management. Anaesthesia. 1979;34:866–73. doi: 10.1111/j.1365-2044.1979.tb08537.x. [DOI] [PubMed] [Google Scholar]
- 17.Osborne PJ, Lee LW. Idiopathic Orthostatic Hypotension, Midodrine, and Anesthesia. Can J of Anaes-Journal Canadien D Anesthesie. 1991;38:499–501. doi: 10.1007/BF03007588. [DOI] [PubMed] [Google Scholar]
- 18.Stirt JA, Frantz RA, Gunz EF, Conolly ME. Anesthesia, catecholamines, and hemodynamics in autonomic dysfunction. Anesth.Analg. 1982;61:701–4. [PubMed] [Google Scholar]
- 19.Vallejo R, DeSouza G, Lee J. Shy-Drager syndrome and severe unexplained intraoperative hypotension responsive to vasopressin. Anesth.Analg. 2002;95:50–2. doi: 10.1097/00000539-200207000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Yamasaki Y, Takahashi H, Miyabe M, Toyooka H. Anesthetic management of a patient with acute idiopathic pandysautonomia. Masui. 2004;53:1029–31. [PubMed] [Google Scholar]
- 21.Young TM, Asahina M, Watson L, Mathias CJ. Hemodynamic effects of clonidine in two contrasting models of autonomic failure: Multiple system atrophy and pure autonomic failure. Mov Disord. 2006;21:609–15. doi: 10.1002/mds.20755. [DOI] [PubMed] [Google Scholar]
- 22.Freshwater-Turner D, Udy A, Lipman J, Deans R, Stuart J, Boots R, Hegde R, McWhinney BC. Autonomic dysfunction in tetanus - what lessons can be learnt with specific reference to alpha-2 agonists. Anaesthesia. 2007;62:1066–70. doi: 10.1111/j.1365-2044.2007.05217.x. [DOI] [PubMed] [Google Scholar]
- 23.Hickler RB, Thompson GR, Fox LM, Hamlin JT., III Successful treatment of orthostatic hypotension with 9-alpha-fluorohydrocortisone. N.Engl.J.Med. 1959;261:788–91. doi: 10.1056/NEJM195910152611604. [DOI] [PubMed] [Google Scholar]
- 24.Chaimberg KH, Travis KW. Supine hypertension during general anesthesia in a patient taking midodrine. Anesth.Analg. 2002;95:1196–7. doi: 10.1097/00000539-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Singer W, Opfer-Gehrking TL, McPhee BR, Hilz MJ, Bharucha AE, Low PA. Acetylcholinesterase inhibition: A novel approach in the treatment of neurogenic orthostatic hypotension. J.Neurol.Neurosurg.Psychiatry. 2003;74:1294–8. doi: 10.1136/jnnp.74.9.1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoeldtke RD, Israel BC. Treatment of orthostatic hypotension with octreotide. J.Clin.Endocrinol.Metab. 1989;68:1051–9. doi: 10.1210/jcem-68-6-1051. [DOI] [PubMed] [Google Scholar]
- 27.Hoeldtke RD, Davis KM, Joseph J, Gonzales R, Panidis IP, Friedman AC. Hemodynamic effects of octreotide in patients with autonomic neuropathy. Circulation. 1991;84:168–76. doi: 10.1161/01.cir.84.1.168. [DOI] [PubMed] [Google Scholar]
- 28.Pop-Busui R, Chey W, Stevens MJ. Severe hypertension induced by the long-acting somatostatin analogue sandostatin LAR in a patient with diabetic autonomic neuropathy. J.Clin.Endocrinol.Metab. 2000;85:943–6. doi: 10.1210/jcem.85.3.6401. [DOI] [PubMed] [Google Scholar]
- 29.Armstrong E, Mathias CJ. The effects of the somatostatin analogue, octreotide, on postural hypotension, before and after food ingestion, in primary autonomic failure. Clin.Auton.Res. 1991;1:135–40. doi: 10.1007/BF01826210. [DOI] [PubMed] [Google Scholar]
- 30.Shibao C, Raj SR, Gamboa A, Diedrich A, Choi L, Black BK, Robertson D, Biaggioni I. Norepinephrine transporter blockade with atomoxetine induces hypertension in patients with impaired autonomic function. Hypertension. 2007;50:47–53. doi: 10.1161/HYPERTENSIONAHA.107.089961. [DOI] [PubMed] [Google Scholar]
- 31.Shibao C, Gamboa A, Diedrich A, Dossett C, Choi L, Farley G, Biaggioni I. Acarbose, an alpha-glucosidase inhibitor, attenuates postprandial hypotension in autonomic failure. Hypertension. 2007;50:54–61. doi: 10.1161/HYPERTENSIONAHA.107.091355. [DOI] [PubMed] [Google Scholar]
- 32.Robertson D, Haile V, Perry SE, Robertson RM, Phillips JA, III, Biaggioni I. Dopamine beta-hydroxylase deficiency. A genetic disorder of cardiovascular regulation. Hypertension. 1991;18:1–8. doi: 10.1161/01.hyp.18.1.1. [DOI] [PubMed] [Google Scholar]
- 33.Robertson D, Goldberg MR, Onrot J, Hollister AS, Wiley R, Thompson JG, Jr., Robertson RM. Isolated failure of autonomic noradrenergic neurotransmission. Evidence for impaired beta-hydroxylation of dopamine. N.Engl.J.Med. 1986;314:1494–7. doi: 10.1056/NEJM198606053142307. [DOI] [PubMed] [Google Scholar]
- 34.Feely J, Wade D, Mcallister CB, Wilkinson GR, Robertson D. Effect of Hypotension on Liver Blood-Flow and Lidocaine Disposition. N. Engl.J.Med. 1982;307:866–9. doi: 10.1056/NEJM198209303071406. [DOI] [PubMed] [Google Scholar]
- 35.Mathias CJ. Autonomic diseases: management. J.Neurol.Neurosurg.Psychiatry. 2003;74(Suppl 3):iii42–7. doi: 10.1136/jnnp.74.suppl_3.iii42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fouad-Tarazi FM, Okabe M, Goren H. Alpha sympathomimetic treatment of autonomic insufficiency with orthostatic hypotension. Am.J.Med. 1995;99:604–10. doi: 10.1016/s0002-9343(99)80246-0. [DOI] [PubMed] [Google Scholar]
- 37.Robertson D, Goldberg MR, Hollister AS, Wade D, Robertson RM. Clonidine raises blood pressure in severe idiopathic orthostatic hypotension. Am J Med. 1983;74:193–200. doi: 10.1016/0002-9343(83)90607-1. [DOI] [PubMed] [Google Scholar]
- 38.Drury PME, Williams EGN. Vocal Cord Paralysis in the Shy-Drager Syndrome - A Cause of Postoperative Respiratory Obstruction. Anaesthesia. 1991;46:466–8. doi: 10.1111/j.1365-2044.1991.tb11685.x. [DOI] [PubMed] [Google Scholar]
- 39.Williams A, Hanson D, Calne DB. Vocal Cord Paralysis in the Shy-Drager Syndrome. J Neurol Neurosurg and Psychiatry. 1979;42:151–3. doi: 10.1136/jnnp.42.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oshima Shigenori, Sugihara Kazuho, Wakayama Shigeharu. Aggravated sleep apnea after general anesthesia in a patient with Shy-Drager syndrome. J Anesth. 1994:484–6. doi: 10.1007/BF02514633. [DOI] [PubMed] [Google Scholar]
- 41.Sweeney BP, Jones S, Langford RM. Anaesthesia in dysautonomia: Further complications. Anaesthesia. 1985;40:783–6. doi: 10.1111/j.1365-2044.1985.tb11006.x. [DOI] [PubMed] [Google Scholar]
- 42.Burnum JF, Hickam JB, Stead EA. Hyperventilation in postural hypotension. Circulation. 1954;10:362–5. doi: 10.1161/01.cir.10.3.362. [DOI] [PubMed] [Google Scholar]
- 43.Burnum JF, Hickam JB, McIntosh H. The effect of hypocapnia on arterial blood pressure. Circulation. 1954;9:89–95. doi: 10.1161/01.cir.9.1.89. [DOI] [PubMed] [Google Scholar]
- 44.Maule S, Lombardo L, Rossi C, Crocella L, Masoero G, Della MP, Catalfamo E, Calvo C, Mecca F, Quadri R. Helicobacter pylori infection and gastric function in primary autonomic neuropathy. Clin.Auton.Res. 2002;12:193–6. doi: 10.1007/s10286-002-0030-1. [DOI] [PubMed] [Google Scholar]
- 45.Thomaides T, Karapanayiotides T, Zoukos Y, Haeropoulos C, Kerezoudi E, Demacopoulos N, Floodas G, Papageorgiou E, Armakola F, Thomopoulos Y, Zaloni I. Gastric emptying after semi-solid food in multiple system atrophy and Parkinson disease. J.Neurol. 2005;252:1055–9. doi: 10.1007/s00415-005-0815-y. [DOI] [PubMed] [Google Scholar]
- 46.Mabuchi N, Hirayama M, Koike Y, Watanabe H, Ito H, Kobayashi R, Hamada K, Sobue G. Progression and prognosis in pure autonomic failure (PAF): Comparison with multiple system atrophy. J.Neurol.Neurosurg.Psychiatry. 2005;76:947–52. doi: 10.1136/jnnp.2004.049023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stocchi F, Badiali D, Vacca L, D’Alba L, Bracci F, Ruggieri S, Torti M, Berardelli A, Corazziari E. Anorectal function in multiple system atrophy and Parkinson’s disease. Mov Disord. 2000;15:71–6. doi: 10.1002/1531-8257(200001)15:1<71::aid-mds1012>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 48.Mathias CJ, Holly E, Armstrong E, Shareef M, Bannister R. The influence of food on postural hypotension in three groups with chronic autonomic failure--clinical and therapeutic implications. J.Neurol.Neurosurg.Psychiatry. 1991;54:726–30. doi: 10.1136/jnnp.54.8.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cohen CA. Anesthetic management of a patient with the Shy-Drager syndrome. Anesthesiology. 1971;35:95–7. doi: 10.1097/00000542-197107000-00026. [DOI] [PubMed] [Google Scholar]
- 50.Cowie DA, Shoemaker JK, Gelb AW. Orthostatic hypotension occurs frequently in the first hour after anesthesia. Anesth.Analg. 2004;98:40–5. doi: 10.1213/01.ANE.0000093388.17298.90. [DOI] [PubMed] [Google Scholar]
- 51.Hutchinson RC, Sugden JC. Anaesthesia for Shy-Drager syndrome. Anaesthesia. 1984;39:1229–31. doi: 10.1111/j.1365-2044.1984.tb06437.x. [DOI] [PubMed] [Google Scholar]
- 52.Knuttgen D, Weidemann D, Doehn M. Diabetic autonomic neuropathy: Abnormal cardiovascular reactions under general anesthesia. Klin.Wochenschr. 1990;68:1168–72. doi: 10.1007/BF01815272. [DOI] [PubMed] [Google Scholar]
- 53.Shannon J, Jordan J, Costa F, Robertson RM, Biaggioni I. The hypertension of autonomic failure and its treatment. Hypertension. 1997;30:1062–7. doi: 10.1161/01.hyp.30.5.1062. [DOI] [PubMed] [Google Scholar]
- 54.Bannister R, Ardill L, Fentem P. Defective autonomic control of blood vessels in idiopathic orthostatic hypotension. Brain. 1967;90:725–46. doi: 10.1093/brain/90.4.725. [DOI] [PubMed] [Google Scholar]
- 55.Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br.J.Anaesth. 2008;100:165–83. doi: 10.1093/bja/aem380. [DOI] [PubMed] [Google Scholar]
- 56.Onrot J, Bernard GR, Biaggioni I, Hollister AS, Robertson D. Direct vasodilator effect of hyperventilation-induced hypocarbia in autonomic failure patients. Am.J.Med.Sci. 1991;301:305–9. doi: 10.1097/00000441-199105000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Robertson D, Biaggioni I. Primer On The Autonomic Nervous System. Third edition Vol. 56. Elsevier Academic Press; 2011. pp. 213–7. [Google Scholar]
- 58.Kitamura A, Hoshino T, Kon T, Ogawa R. Patients with diabetic neuropathy are at risk of a greater intraoperative reduction in core temperature. Anesthesiology. 2000;92:1311–8. doi: 10.1097/00000542-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 59.Ketch T, Biaggioni I, Robertson R, Robertson D. Four faces of baroreflex failure: Hypertensive crisis, volatile hypertension, orthostatic tachycardia, and malignant vagotonia. Circulation. 2002;105:2518–23. doi: 10.1161/01.cir.0000017186.52382.f4. [DOI] [PubMed] [Google Scholar]
- 60.Niquille M, Van Gessel E, Gamulin Z. Continuous spinal anesthesia for hip surgery in a patient with Shy-Drager syndrome. Anesth Analg. 1998;87:396–9. doi: 10.1097/00000539-199808000-00030. [DOI] [PubMed] [Google Scholar]
- 61.Malinovsky JM, Cozian A, Rivault O. Spinal anesthesia for transurethral prostatectomy in a patient with multiple system atrophy. Can J Anaesth-Journal Canadien D Anesthesie. 2003;50:962–3. doi: 10.1007/BF03018749. [DOI] [PubMed] [Google Scholar]
- 62.Gomesz FA, Montell M. Caudal anaesthesia in the Shy-Drager syndrome. Anaesthesia. 1992;47:1100. doi: 10.1111/j.1365-2044.1992.tb04230.x. [DOI] [PubMed] [Google Scholar]
- 63.Mohring J, Glanzer K, Maciel JA, Jr., Dusing R, Kramer HJ, Arbogast R, Koch-Weser J. Greatly enhanced pressor response to antidiuretic hormone in patients with impaired cardiovascular reflexes due to idiopathic orthostatic hypotension. J.Cardiovasc.Pharmacol. 1980;2:367–76. doi: 10.1097/00005344-198007000-00004. [DOI] [PubMed] [Google Scholar]
- 64.Goldberg MR, Robertson D, FitzGerald GA. Prostacyclin biosynthesis and platelet function in autonomic dysfunction. Neurology. 1985;35:120–3. doi: 10.1212/wnl.35.1.120. [DOI] [PubMed] [Google Scholar]
- 65.Robertson D, Goldberg MR, Hollister AS, Wade D, Robertson RM. Clonidine raises blood pressure in severe idiopathic orthostatic hypotension. Am.J.Med. 1983;74:193–200. doi: 10.1016/0002-9343(83)90607-1. [DOI] [PubMed] [Google Scholar]
- 66.Goldberg MR, Hollister AS, Carey EL, Tung CS, Robertson D. Vascular Beta-2-Adrenergic Hypersensitivity in Autonomic Dysfunction. Circulation. 1982;66:6. [Google Scholar]