Abstract
Objectives
To evaluate the biomechanical effect of the X-Stop device on the intervertebral foramen (IVF) and segmental spinal canal length (SSCL), as well as the intervertebral disc space at the implanted and the adjacent segments in patients with lumbar spinal stenosis (LSS).
Materials and methods
Eight elderly patients with LSS, scheduled for X-stop implantation, were CT or MRI scanned to construct 3D vertebral models (L2–S1). Before and after the surgery, each patient was also imaged using a dual-fluoroscopic image system during weight-bearing standing and maximum extension–flexion. The positions of the vertebrae were then determined using an established 2D–3D model matching method.
Results
The data revealed that the postoperative IVF area was significantly increased by 32.9% (or 32 mm2) (p < 0.05) and the IVF width was increased by 24.4% (or 1.1 mm, p = 0.06) during extension, but with minimal change in standing and flexion. The IVF heights were significantly (p < 0.05) increased at standing by 1.2 mm and extension by 1.8 mm, but not at flexion. The SSCL were significantly (p < 0.05) increased at extension by 1.2 mm, but not at standing and flexion. Anterior disc space of the implanted level was significantly decreased from 8.0 to 6.6 mm during standing.
Conclusion
The X-Stop implantation efficiently enlarged the IVF area in the elderly patients with LSS at the operated level with little biomechanical effect immediately on the superior and inferior adjacent levels. However, it reduced the anterior disc space at the implanted level.
Keywords: Lumbar spinal stenosis, Biomechanical effect, Intervertebral foramen, Segmental spinal canal length, Intervertebral disc space
Introduction
Lumbar spinal stenosis (LSS) is a chronic degenerative process leading to narrowing of the spine central canal or intervertebral foramen. In symptomatic patients, the neural impingement is typically exacerbated by extension and relieved by flexion [1, 2]. The gold standard of surgical treatment is laminectomy with or without fusion, where elderly patients may be at higher risk of increased mortality resulting from prolonged anesthesia [3–6]. Recently, interspinous process (ISP) distraction devices, such as the X-Stop, have been applied; these devices can be mini-invasively inserted between the interspinous processes at the stenotic segment and placed in slight flexion, limiting extension and thus indirectly decompressing the IVF and spinal canal [7, 8].
Although there are data reporting promising clinical outcomes in elderly patients with LSS after X-stop surgeries [9–11], the few studies that have reported on the biomechanical effect of X-Stop implantation on the intervertebral foramen (IVF) dimensions (including area, height and width) have used in vitro experiment or in vivo 2-dimensional (2D) image techniques [9, 12–14].
Recently, we investigated the ISP gap changes in patients after implantation of X-Stop devices [15] using a combined 3D modeling and dual-fluoroscopic image system (DFIS) technique [16]. In this study, we investigated the in vivo changes of the IVF dimensions, spinal canal length and intervertebral disc heights after X-Stop implantation in these patients. We hypothesized that X-Stop implantation would enlarge the IVF area and elongate the spinal canal length, but also reduce the intervertebral disc height at the implantation level. Further, we hypothesized that X-Stop implantation will not significantly affect the biomechanics of the superior and inferior adjacent levels.
Materials and methods
Subject recruitment
Ten LSS patients scheduled for X-Stop implantation (Table 1) were recruited with approval of the authors’ institutional review board (IRB). Written consent was obtained from all subjects before testing. The inclusion criteria included: age over 50 years, leg, buttock, or groin pain with or without back pain that was relieved by flexion. The subjects must be able to stand for at least 20 min (duration of dual-fluoroscopic imaging). The exclusion criteria included: presence of active infection in the lumbar spine, cauda equina syndrome, previous lumbar surgery at the stenotic level, spondylolisthesis grade 2 or more (according to Meyerding classification) and moderate or severe scoliosis deformity (Cobb angle ≥ 25º).
Table 1.
Patient demographics
| No. | Sex | Age | BMI (kg/m2) | Symptoms | Diagnosis | Implanted level | Follow-up (months) |
|---|---|---|---|---|---|---|---|
| 1 | F | 74 | 22.4 | LBP& R,NIC | LSS | L4/5 | 3 |
| 2 | F | 86 | 19.1 | LBP& R,NIC | LSS | L4/5 | 5 |
| 3 | M | 78 | 27.5 | LBP& R,NIC | LSS | L3/4,L4/5 | 12 |
| 4 | M | 81 | 21.1 | LBP& NIC | LSS | L4/5 | 10 |
| 5 | M | 66 | 39.4 | LBP& R,NIC | LSS | L4/5,L5/S1 | 8 |
| 6 | F | 84 | 31.2 | LBP& NIC | LSS | L4/5 | 3 |
| 7 | M | 76 | 26.6 | LBP& R,NIC | LSS | L3/4 | 8 |
| 8 | F | 85 | 27 | LBP& NIC | LSS | L4/5 | 10 |
| Mean | NA | 78.8 | 26.8 | NA | NA | NA | 7.4 |
LBP low back pain, R radiated pain, NIC neural intermittent claudiation, LSS lumbar spinal stenosis, NA not applicable
Two patients who failed to complete the study were excluded from the final analysis: one patient opted out of surgery, and another refused the follow up visit. In the eight patients who finished this study, six patients had a single-level implantation and two patients received implantation at two levels (with 2 implantations at L3–4, 7 at L4–5, and 1 at L5–S1). The average follow-up time was 7.4 months (Table 1).
3-D vertebral modeling and image matching technique
Lumbar segments of seven of the enrolled patients were CT scanned (Light-Speed Pro16, GE, Waukesha, WI, USA) using high-resolution axial cuts images in the supine position. Images were obtained with a thickness of 0.625 mm and a gap of 0.625 mm, and with a resolution of 512 × 512 pixels. One patient was MRI scanned using a 3 T scanner (MAGNETOM® Trio, Siemens, Erlangen, Germany) with a spine surface coil and a T2-weighted fat suppressed spoiled gradient recalled (SPGR) sequence. Parallel sagittal images were obtained with a thickness of 1 mm without gap, with a resolution of 512 × 512 pixels. The CT and MRI images of the spinal segments were imported into a solid modeling software (Rhinoceros® version 4.0, Robert McNeel & Associates, Seattle, WA, USA) to construct 3D anatomical vertebral models of L2, L3, L4, L5 and S1 using an established, validated protocol [16, 17]. Both the CT and MRI techniques can yield accurate vertebral 3D models that can be used interchangeably [16].
Prior to X-Stop implantation and at the finial follow-up visit, the lumbar spines of the subjects were imaged using a dual orthogonal fluoroscopic image system (BV Pulsera, Phillips, Bot hell, WA, USA) at weight-bearing postures of the torso: upright standing, maximum extension and maximum flexion (Fig. 1). The positions of the lumbar vertebrae were then reproduced in the solid modeling software using the 3D models of the vertebrae and the dual-fluoroscopic images using an established protocol [16, 17]. The 3D models of the vertebrae were independently translated and rotated in 6 degree of freedom (6 DOF) until their projection outlines matched the osseous contours captured on the two calibrated fluoroscopic images (Fig. 2). Our previous study [16] validated the current noninvasive image matching method and found that the mean accuracy was less than 0.2 mm and the repeatability in reproducing the in vivo human spine kinematics was less than 0.3 mm in translation and less than 0.7° in orientation.
Fig. 1.
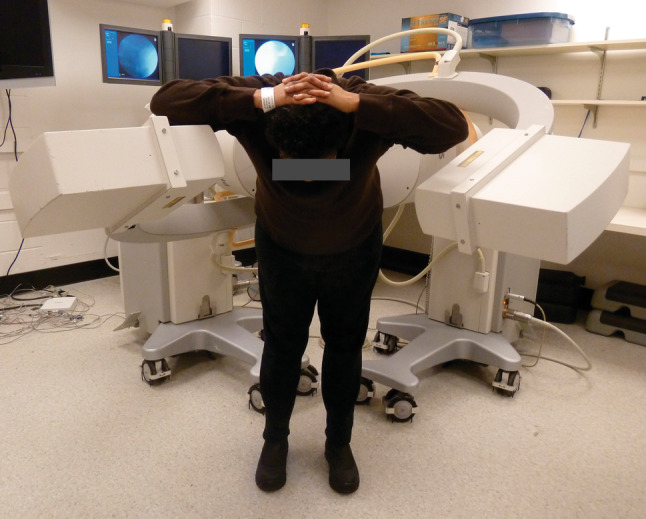
Experimental setup of the dual-fluoroscopic system (DFIS) for capture of the lumbar spine positions in vivo
Fig. 2.
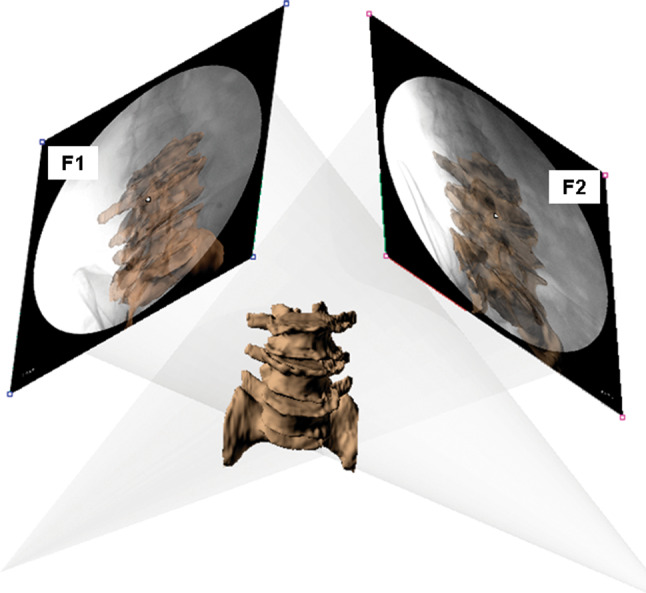
The in vivo positions of the lumbar vertebrae reproduced in solid modeling software using the 3D models of the vertebrae and the fluoroscopic images
Morphometric measurements
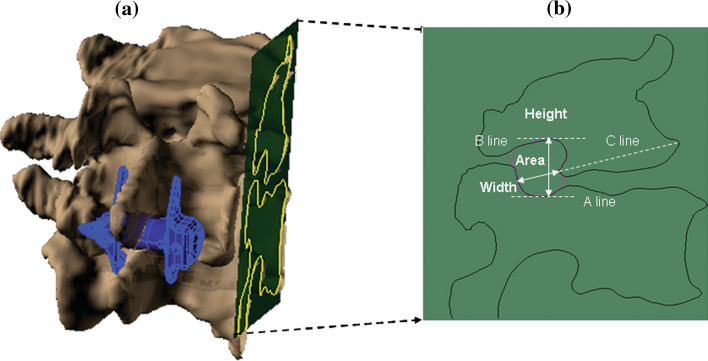
The authors have carefully examined the morphology of the vertebrae and excluded the osteophytes in the measurements. After the 3D vertebral models were built, osteophytes were identified and marked by a clinical spine doctor (the First author). Measurements were performed in a consistent way using the marked 3D models in the solid modeling software. In this way, osteophytes will not affect the quantitative kinematics measurements. The IVF dimensions (area, height and width) of 3D mesh models were measured on a pedicle cutting plane (Fig. 3a). Based on the geometry of the pedicle, we set the pedicle cutting plane passing the pedicle centers of the cranio-caudal pedicles and the long axis of the caudal pedicle, which also corresponded to the narrowest cross-section area of the intervertebral foramen [18]. We used the intersection line of the pedicle plane and the 3D mesh vertebral models as an IVF bony outline to measure the IVF dimensions (area, width, height). The area of IVF was drawn anatomically according to the IVF bony outline. The IVF height was measured from the longest distance between cranio-caudal pedicles, which was also perpendicular to the upper endplate of the caudal vertebrae. The width of IVF was measured on the line which was through both the posterior-inferior corner and the anterior-inferior corner of the cranial vertebrae (Fig. 3b). The pedicle cutting plane was only created once at standing preoperative position. After that, they were grouped with the corresponding segments to ensure consistency in measurements under various torso positions both pre–post operatively.
Fig. 3.
a Pedicle plane for measurement of the IVF dimensions b IVF dimensions (area, height and width) in the pedicle plane. Lines A and B are parallel with the upper endplate of the caudal segment; line C is through both the posterior-inferior corner and the anterior-inferior corner of the cranial vertebrae
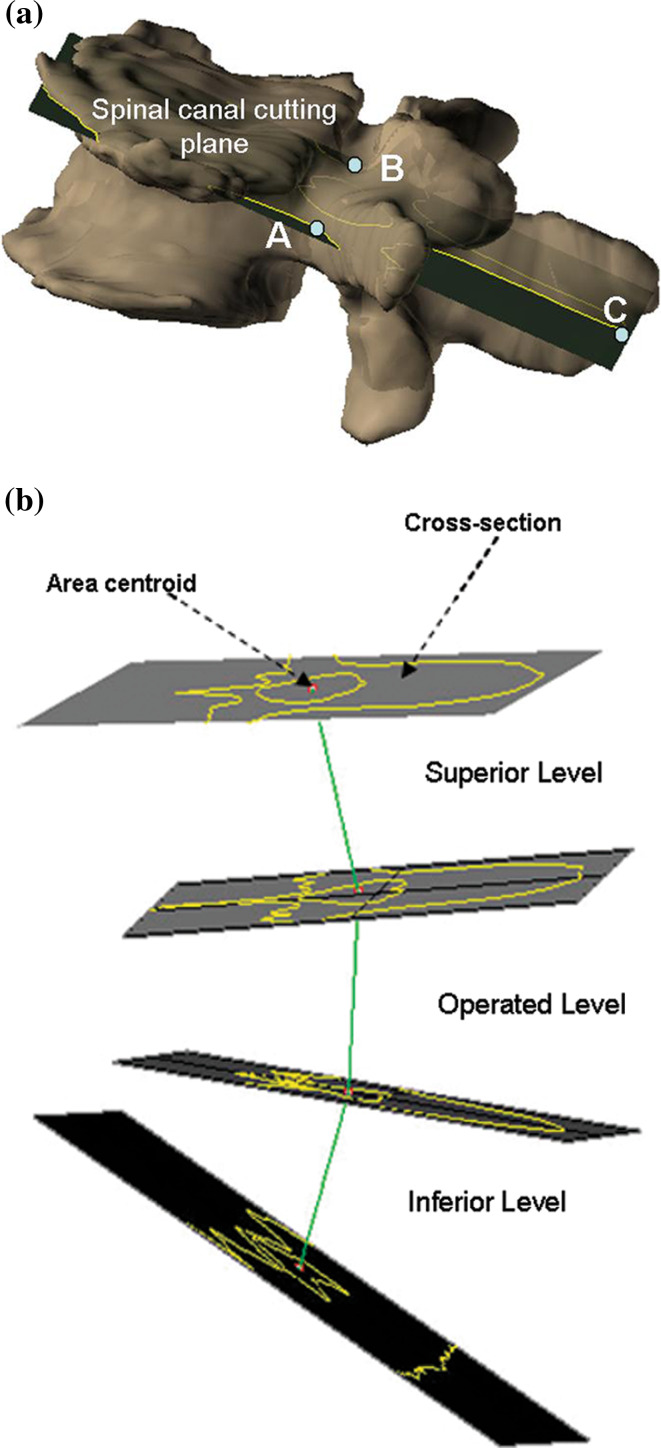
To determine the spinal canal across-section, we made a spinal canal cutting plane through the bilateral pedicles’ centers and the middle point of the posterior edge of the spinous process (Fig. 4a). We used the intersection line of the spinal canal cutting plane and the 3D mesh vertebral model as bony outline of the spinal canal axis cross-section (Fig. 4b). The segmental spinal canal length (SSCL) was the distance between cranio-caudal area centroids of the spinal canal axis cross-sections.
Fig. 4.
a spinal canal cutting plane was through the centers of the left and right pedicles (point A and B) as well as the middle point of the posterior edge of the spinous process (point C). b Segmental spinal canal length (SSCL) was determined between the area centroids of the cranial-caudal spinal canal cross-sections at the operated level and the superior-inferior adjacent levels
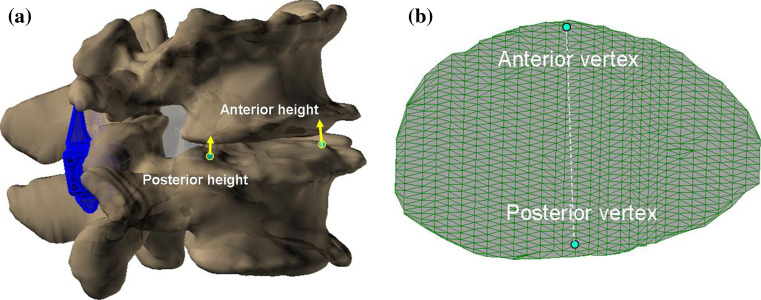
Anterior and posterior disc heights of the implanted level and the adjacent levels on standing, extension and flexion postures before and after X-Stop surgery were calculated using evenly distributed mesh vertices on the upper and lower endplates (approximately 800 points per endplate). We chose anterior and posterior vertex points at the lower endplates for each disc excluding the osteophyte (Fig. 5a). Using the iterative closest point method [19, 20], anterior disc height was determined at anterior vertex and posterior disc height was determined at posterior vertex of the endplate (Fig. 5b).
Fig. 5.
a Using the iterative closest point method, the anterior and posterior disc heights were measured. b Anterior and posterior representative locations on endplate surface composed with evenly distributed mesh vertices
Statistical analysis
Two-way repeated measures analysis of variance (ANOVA) was used to detect significant differences in all biomechanical measurements. The area, width, height of IVF and the SSCL as well as disc heights at different levels (implanted level, superior level and inferior level) were the dependent variables and the X-Stop operation and different postures (standing, extension and flexion) were the independent variables. When a statistically significant difference was detected, a post hoc Newman–Keuls test was performed. Level of statistical significance was set at p < 0.05. The statistical analysis was performed using Statistica v. 8.0 (Statsoft, Tulsa, OK, USA).
Results
Intervertebral foramen dimensions
The IVF dimensions for the both left and right sides were described in the Appendix 1. To assess the effect of X-Stop implantation on the IVF, the measurements of IVF dimensions (area, width, height) at the left and right sides were averaged to calculate the mean values.
At the implanted level, in extension, the mean IVF area of both sides was significantly increased by 32.9% (or 32 mm2, p = 0.002). However, the IVF area was not significantly (p > 0.05) increased in standing and flexion. At the superior and inferior adjacent levels, the preoperative and postoperative IVF areas were not significantly (p > 0.05) different in standing, extension and flexion (Table 2).
Table 2.
Effect of X-Stop implantation on the IVF dimensions during various postures (mm)
| NF areas | NF heights | NF widths | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Stand | Extension | Flexion | Stand | Extension | Flexion | Stand | Extension | Flexion | |
| Proximal | |||||||||
| Pre-Op | 141 ± 39 | 133 ± 30 | 147 ± 35 | 15.6 ± 2.5 | 16.2 ± 2.1 | 16.7 ± 2.2 | 8.2 ± 3.7 | 7.8 ± 3.3 | 8.2 ± 3.2 |
| Post-Op | 137 ± 29 | 137 ± 31 | 148 ± 29 | 15.6 ± 2.0 | 16.2 ± 2.4 | 16.7 ± 1.9 | 8.2 ± 3.3 | 8.6 ± 3.6 | 8.4 ± 2.9 |
| p value | 0.479 | 0.445 | 0.854 | 0.949 | 0.938 | 0.902 | 0.990 | 0.744 | 0.946 |
| Operated | |||||||||
| Pre-Op | 144 ± 19 | 129 ± 39 | 168 ± 44 | 14.4 ± 2.5 | 14.0 ± 2.8 | 15.7 ± 3.6 | 9.5 ± 2.0 | 8.8 ± 3.1 | 10.5 ± 3.0 |
| Post-Op | 158 ± 30 | 161 ± 27 | 167 ± 37 | 15.5 ± 2.8 | 15.8 ± 2.3 | 16.1 ± 3.4 | 9.9 ± 2.7 | 10.7 ± 3.2 | 10.1 ± 2.6 |
| p value | 0.073 | 0.002 | 0.903 | 0.012 | 0.035 | 0.571 | 0.554 | 0.061 | 0.558 |
| Distal | |||||||||
| Pre-Op | 122 ± 39 | 116 ± 24 | 115 ± 30 | 1.3.0 ± 3.3 | 13.5 ± 2.9 | 12.7 ± 3.7 | 8.8 ± 3.8 | 8.2 ± 3.0 | 9.1 ± 3.3 |
| Post-Op | 115 ± 37 | 115 ± 31 | 110 ± 23 | 12.9 ± 3.9 | 13.0 ± 2.8 | 12.2 ± 2.3 | 8.3 ± 3.4 | 8.2 ± 3.0 | 8.6 ± 3.1 |
| p value | 0.607 | 0.997 | 0.712 | 0.994 | 0.722 | 0.456 | 0.568 | 0.990 | 0.641 |
The values represent mean. Statistical significance is set at p < 0.05 in bold and italics fonts
Pre-Op pre-operative, Post-Op postoperative
At the implanted level, the mean IVF height of both sides was significantly increased by 8.2% (or 1.2 mm, p = 0.012) and 13.9% (or 1.8 mm, p = 0.035) in standing and extension, respectively, after the surgery. At the superior and inferior adjacent levels, the preoperative and postoperative IVF heights were not significantly (p > 0.05) different in standing, extension and flexion (Table 2).
At the implanted level, the mean IVF width of the both sides was increased by 24.4% (or 1.1 mm, p = 0.061) but not in standing and flexion (p > 0.05). At the superior and inferior adjacent levels, the preoperative and postoperative IVF areas were not significantly (p > 0.05) different in standing, extension and flexion (Table 2).
Segmental spinal canal length
Postoperatively, at the implanted level, the mean SSCL was significantly increased by 1.2 mm in extension (p = 0.002); and also increased by 1.1 mm in standing (p = 0.071), but not in flexion (p = 0.903). At the superior and inferior adjacent levels, the preoperative and postoperative SSCL were not significantly (p > 0.05) different in standing, extension and flexion (Table 3).
Table 3.
Effect of X-Stop implantation on the SSCL (segmental spinal canal length) (mm)
| Proximal level | Operated level | Distal level | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Stand | Extension | Flexion | Stand | Extension | Flexion | Stand | Extension | Flexion | |
| Pre-Op | 31.9 | 31.3 | 32.5 | 28.7 | 28.7 | 29.4 | 23.8 | 23.5 | 22.8 |
| Post-Op | 31.6 | 31.5 | 32.1 | 29.8 | 29.8 | 30.3 | 23 | 22.8 | 22.5 |
| Difference | −0.4 | 0.3 | −0.4 | 1.1 | 1.2 | 0.9 | −0.8 | −0.6 | −0.4 |
| p value | 0.363 | 0.514 | 0.374 | 0.073 | 0.002 | 0.903 | 0.337 | 0.621 | 0.764 |
The values represent mean. Statistical significance is set at p < 0.05 and is used bold and italics fonts
Pre-Op pre-operative, Post-Op postoperative
Anterior and posterior disc heights measurement
At the implanted level, postoperative anterior disc height was decreased from 8.0 to 6.6 mm (p = 0.037) in standing, from 8.1 to 7.4 mm (p = 0.387) in extension and from 7.6 to 6.8 mm (p = 0.176) in flexion. The postoperative posterior disc height was not significantly changed in standing (p = 0.752), extension (p = 0.973) and flexion (p = 0.699). At the superior and inferior adjacent levels, in standing, extension and flexion, the preoperative and postoperative anterior disc height and posterior disc height were not significantly different (p > 0.05; Table 4).
Table 4.
Effect of X-Stop implantation on the anterior & posterior disc heights (mm)
| Proximal level | Operated level | Distal level | ||||
|---|---|---|---|---|---|---|
| Anterior | Posterior | Anterior | Posterior | Anterior | Posterior | |
| Stand | ||||||
| Pre-op | 6.0 ± 2.8 | 2.7 ± 1.2 | 8.0 ± 2.5 | 4.4 ± 2.8 | 7.3 ± 3.4 | 2.4 ± 2.2 |
| Post-op | 6.4 ± 2.5 | 2.9 ± 1.8 | 6.6 ± 2.8 | 4.8 ± 2.2 | 7.0 ± 2.5 | 2.4 ± 1.0 |
| p value | 0.636 | 0.858 | 0.037 | 0.752 | 0.757 | 0.973 |
| Extension | ||||||
| Pre-op | 5.6 ± 2.4 | 2.2 ± 1.8 | 8.1 ± 2.5 | 4.8 ± 2.9 | 6.9 ± 2.0 | 2.2 ± 1.3 |
| Post-op | 6.1 ± 3.0 | 2.7 ± 2.3 | 7.4 ± 3.1 | 4.8 ± 3.1 | 7.6 ± 1.9 | 2.1 ± 1.5 |
| p value | 0.662 | 0.244 | 0.387 | 0.973 | 0.874 | 0.927 |
| Flexion | ||||||
| Pre-op | 6.7 ± 3.3 | 3.5 ± 1.6 | 7.6 ± 2.3 | 5.2 ± 2.6 | 7.0 ± 2.5 | 2.1 ± 1.0 |
| Post-op | 5.9 ± 2.8 | 2.8 ± 1.5 | 6.8 ± 2.2 | 5.4 ± 2.8 | 5.5 ± 2.1 | 1.9 ± 1.3 |
| p value | 0.474 | 0.251 | 0.176 | 0.699 | 0.162 | 0.731 |
The values are mean ± standard deviation and two-way repeated ANOVA is used. Statistical significance is set at p < 0.05
Pre-Op preoperative, Pre-Op postoperative
Discussion
Although interspinous spacers are becoming increasingly popular in surgical treatment of LSS, the proposed biomechanical effect of increasing space available for neural elements has not been documented under in vivo physiological conditions. This study investigated the effect of X-Stop implantation on patient lumbar spine biomechanics during weight-bearing functions. The data confirmed our initial hypothesis that the IVF mean areas and the SSCL were significantly (p < 0.05) increased during extension of the torso at the implanted segments, but not at the adjacent segments. At the operated level, the implantation caused reduction of the intervertebral disc height at anterior location, but not at the posterior location.
The results of this study compare favorably with the other available reports in the literature. Richards et al. [12] reported that the mean area of the bilateral IVF of the implanted level was increased by 25% (from 106 to 133 mm2) in extension after X-Stop implantation in eight cadaveric specimens using MRI technique. Lee et al. [6] reported that the cross-sectional area of IVF of the X-Stop at the implanted level was increased by 36.5% (or 22 mm2) using MRI in ten elderly LSS patients. Siddiqui et al. [14] also observed that the X-Stop implantation enlarged the IVF area in extension at single diseased (with 20% increase at left side) and at two diseased levels (with 20–32% increase) in 26 elderly LSS patients. In the current study, we measured the bony outline of IVF using 3D bony vertebral models. The IVF area of our study was bigger than the previous reports obtained using MRI technique since the soft tissue around the IVF was not included in our study. However, our data were similar with that measured by Schlegel et al. [21] using CT scan where the IVF area of 10 stenotic segments in 7 cadaver lumbar spines was reported as 166.2 mm2 (range 136–217 mm2).
Conversely, Nandakumar et al. [13] recently reported that IVF area of the implanted level was not significantly increased during all postures except for left cranial level for double-level surgeries in 48 X-Stop patients at average 2 years postoperatively using a positional MRI technique. Since our follow-up study was at an average of 7.4 months after surgery, it remains to be seen if the biomechanical efficiency of the surgery for IVF can still remain in the medium-long term after X-Stop surgeries.
There are only limited data on the changes in specific IVF dimensions such as width and height after X-Stop implantation. Richard et al. [12] reported that the mean width of the IVF area was increased significantly (preoperative 3.4 mm vs. postoperative 4.8 mm) in extension, but not for height in terms of IVF area in cadaveric specimens using MR images. Zucherman et al. [9] measured the changes of IVF height in LSS patients who underwent X-Stop surgery on plain radiographs, and reported that the mean IVF height was 23.2 mm in X-Stop patients and 22.5 mm in nonoperatively treated patients (p > 0.05) at an average 1-year follow-up. Two years postoperatively, the mean IVF height was 21.2 mm in X-Stop patients and 21.5 mm in nonoperatively treated patients (p > 0.05). Due to different study design and measurement method for IVF width and height, there were slight deviations for IVF height and width values compared with the previous studies [2, 9, 12, 18]. The data of this study showed that postoperatively only during extension of the torso, the mean width on left and right side IVF was increased by 24.4% (or 1.1 mm, p = 0.06). The postoperative IVF mean height was significantly (p < 0.05) increased by 8.2% (or 1.2 mm) during standing and 13.9% (or 1.8 mm) during extension, but not during flexion posture. The measurement of IVF width in this study was greater than other reports since we used 3D bony models to measure the IVF dimensions and did not take into account the disc bulging and thickness of ligament flavum. Furthermore, we measured the IVF width consistently on a line parallel to upper endplate of cranial vertebra rather than parallel with the disc reported by Richard et al. [12].
Our data showed that the SSCL at the X-Stop implanted level was significantly (p < 0.05) increased by 1.2 mm in extension after the X-Stop surgery, and increased by 1.1 mm in flexion (p = 0.073). The increase of SSCL contributes to stretching the infolded soft tissue, especially ligament flavum and enlarges the available space for spine cord [21, 22]. However, the clinical importance of the SSCL stretching is currently difficult to evaluate.
In general, we found that the anterior disc height was decreased and no significant change was detected at the posterior disc height in the implanted level, but the anterior and posterior disc heights of the superior and inferior adjacent segments were not significantly affected after implantation of the X-Stop devices. This was similar to the data of Siddiqui et al. [23] and Nandakumar et al. [13] reported that the anterior disc height of the X-Stop implanted level was significantly decreased, but without significant change in posterior disc height. Lee et al. [6] reported that the posterior disc height of the X-Stop implanted level was significantly (p < 0.05) increased from 5.93 to 7.68 mm in 10 elderly patients with LSS. We hypothesized that the natural progression of degeneration in patients with LSS probably affects the disc heights, except the mechanical factor of X-Stop implantation, which can explain the no significant increase at the posterior disc height while significant decrease at the anterior disc height. The increase of IVF area may attribute to both the increase of its height and width as well as the changes of its shape. We found that the IVF area was increased while the posterior disc height was not significantly changed. In this case, the increase was mainly caused by the distraction of the posterior element rather than the intervertebral disc, which supports the design purpose of the X-Stop device. Decrease of the anterior disc height with no significant change of the posterior disc height can induce a local kyphosis, which was also supported by the Lindsey et al. [8] who reported X-Stop implantation places the implanted segment at 2° slight flexion position.
There are several limitations in this study that should be noted. First, we measured the bony dimensions of IVF before and after X-Stop implantation, thus yielding greater dimensions of IVF compared to the previous studies using MRI-based techniques. Soft tissue structures (such as unfolding ligament flavum, buckling disc and hypertrophy of the facet capsule) can further contribute to LSS. However, the changes of the bony dimensions were in line with the effectiveness of decompression after X-Stop implantation. Second, relatively small sample size was included in this current study due to the limited patient availability that met our inclusion criteria. Thus, we did not consider the distraction to be an independent variable and sub-divide the subjects into smaller groups. To minimize the influences of the distraction parameters and placing of the implant, all the patients involved in the study were recruited from a single surgeon who did the surgeries in a consistent way. In addition, the p values obtained in this study may possibly represent a small and selected subset of a potentially large group of p values. Thus, the complete data of each individual were included in Appendix 2 for the readers.
In summary, this study quantified the in vivo changes in the IVF dimensions, SSCL as well as the intervertebral disc space in elderly patients with LSS using CT/MRI and DFIS techniques. The results showed that the X-Stop device decompressed the IVF in extension without significant disturbance of the adjacent levels, but the effectiveness in the treatment of the stenosis should be clinically confirmed. At the implanted level, we observed approximately 1 mm of lengthening of the spinal canal segment, and significantly reduced anterior disc height on standing. Medium- to long-term follow up data are necessary to determine whether this relatively new treatment retains its efficacy over time.
Acknowledgments
This study was partially supported by a research grant of Medtronic Inc, NIH (R21AR057989) and China Scholarship Council (2009637094).
Conflict of interest
None.
Appendix (1): NF dimensions at left and right sides
The intervertebral foramen (IVF) dimensions (area, height and width) of the left and right sides at implanted and adjacent levels were quantified (Tables 5, 6, 7). At the implanted level, the postoperative IVF area was significantly (p < 0.05) increased by 46.0% (or 34.9 mm2) for left side and 13.1% (or 17.5 mm2) for right side during extension, yet not in standing and flexion (Table 5). The IVF width was significantly increased by 32.2% significantly (or 1.7 mm) for left side and increased by 3.0% (or 0.3 mm, p = 0.08), yet not significantly for right side (Table 6). The IVF heights were significantly (p < 0.05) increased by 16.2% (or 2.1 mm) for left side during extension, 13.1% (or 1.8 mm) during standing and 16.0% (or 1.9 mm) for right side, but not in flexion (Table 7).
Table 5.
Effect of X-Stop implantation on the IVF area at the left and right sides
| Left side | Right side | |||||
|---|---|---|---|---|---|---|
| Stand | Extension | Flexion | Stand | Extension | Flexion | |
| Superior level | ||||||
| Pre-Op | 135 ± 40 | 132 ± 39 | 139 ± 35 | 148 ± 61 | 134 ± 42 | 154 ± 57 |
| Post-Op | 133 ± 36 | 132 ± 36 | 145 ± 40 | 142 ± 42 | 142 ± 40 | 150 ± 46 |
| p value | 0.731 | 0.975 | 0.241 | 0.587 | 0.225 | 0.577 |
| Operated level | ||||||
| Pre-Op | 141 ± 33 | 123 ± 46 | 162 ± 53 | 147 ± 33 | 135 ± 41 | 174 ± 51 |
| Post-Op | 151 ± 47 | 161 ± 41 | 154 ± 44 | 164 ± 40 | 162 ± 31 | 179 ± 45 |
| p value | 0.340 | 0.021 | 0.638 | 0.082 | 0.007 | 0.564 |
| Inferior level | ||||||
| Pre-Op | 122 ± 55 | 124 ± 33 | 121 ± 41 | 121 ± 33 | 108 ± 27 | 109 ± 31 |
| Post-Op | 122 ± 56 | 119 ± 37 | 116 ± 34 | 108 ± 25 | 110 ± 35 | 103 ± 32 |
| p value | 0.971 | 0.300 | 0.538 | 0.160 | 0.888 | 0.471 |
The values represent mean ± standard deviation. Statistical significance is set at p < 0.05 in bold and italic fonts
Pre-Op preoperative, Post-Op postoperative
Table 6.
Effect of X-Stop implantation on the IVF height at the left and right sides
| Left side | Right side | |||||
|---|---|---|---|---|---|---|
| Stand | Extension | Flexion | Stand | Extension | Flexion | |
| Superior level | ||||||
| Pre-Op | 15.6 ± 2.8 | 16.4 ± 3.3 | 16.5 ± 2.6 | 15.6 ± 4.0 | 16.0 ± 2.5 | 16.8 ± 2.7 |
| Post-Op | 15.4 ± 2.7 | 16.1 ± 3.7 | 17.0 ± 2.6 | 15.9 ± 3.0 | 16.3 ± 2.5 | 16.4 ± 2.9 |
| p value | 0.698 | 0.621 | 0.269 | 0.678 | 0.551 | 0.237 |
| Operated level | ||||||
| Pre-Op | 14.6 ± 3.9 | 13.8 ± 3.0 | 15.7 ± 4.2 | 14.1 ± 2.8 | 14.3 ± 3.7 | 15.8 ± 4.3 |
| Post-Op | 15.3 ± 4.0 | 15.7 ± 3.0 | 15.9 ± 3.8 | 16.0 ± 3.3 | 16.1 ± 3.0 | 16.3 ± 4.1 |
| p value | 0.252 | 0.020 | 0.770 | 0.007 | 0.007 | 0.398 |
| Inferior level | ||||||
| Pre-Op | 13.1 ± 5.1 | 14.0 ± 4.3 | 13.1 ± 5.1 | 12.8 ± 2.8 | 13.0 ± 2.7 | 12.2 ± 3.1 |
| Post-Op | 12.7 ± 2.8 | 13.3 ± 4.5 | 12.7 ± 2.8 | 12.7 ± 2.5 | 12.7 ± 1.6 | 11.6 ± 2.9 |
| p value | 0.970 | 0.138 | 0.684 | 0.825 | 0.736 | 0.436 |
The values represent mean ± standard deviation. Statistical significance is set at p < 0.05 in bold and italic fonts
Pre-Op preoperative, Post-Op postoperative
Table 7.
Effect of X-Stop implantation on the IVF width at the left and right sides
| Left side | Right side | |||||
|---|---|---|---|---|---|---|
| Stand | Extension | Flexion | Stand | Extension | Flexion | |
| Superior level | ||||||
| Pre-Op | 7.5 ± 4.3 | 7.8 ± 3.4 | 8.3 ± 3.8 | 8.9 ± 3.9 | 7.9 ± 3.6 | 8.2 ± 3.5 |
| Post-Op | 7.7 ± 4.2 | 8.2 ± 3.9 | 8.3 ± 3.7 | 8.7 ± 2.9 | 8.9 ± 3.8 | 8.5 ± 3.0 |
| p value | 0.626 | 0.639 | 0.987 | 0.864 | 0.130 | 0.464 |
| Operated level | ||||||
| Pre-Op | 9.3 ± 3.0 | 8.5 ± 3.5 | 10.3 ± 3.3 | 9.8 ± 2.3 | 9.0 ± 3.2 | 10.7 ± 3.1 |
| Post-Op | 9.6 ± 3.5 | 10.6 ± 4.5 | 10.0 ± 3.6 | 10.2 ± 3.0 | 10.8 ± 2.4 | 10.2 ± 2.2 |
| p value | 0.534 | 0.038 | 0.734 | 0.422 | 0.247 | 0.552 |
| Inferior level | ||||||
| Pre-Op | 9.1 ± 4.4 | 8.8 ± 2.8 | 8.6 ± 3.6 | 8.4 ± 4.1 | 7.7 ± 3.6 | 9.6 ± 3.6 |
| Post-Op | 8.8 ± 3.6 | 8.8 ± 3.1 | 8.1 ± 3.0 | 7.8 ± 3.7 | 7.7 ± 4.1 | 9.1 ± 3.8 |
| p value | 0.626 | 0.909 | 0.554 | 0.386 | 0.984 | 0.574 |
The values represent mean ± standard deviation. Statistical significance is set at p < 0.05 in bold and italic fonts
Pre-Op preoperative, Post-Op postoperative
Appendix (2): individual measurements
Table 8.
Pre-Op and Post-Op IVF dimensions during upright standing (mm/mm2)
| No. | Height (a) | Height (b) | Width (a) | Width (b) | Area (a) | Area (b) |
|---|---|---|---|---|---|---|
| Proximal level | ||||||
| 1 | 13.0 | 14.2 | 6.8 | 7.5 | 99.6 | 116.3 |
| 2 | 15.4 | 15.1 | 12.5 | 10.6 | 179.9 | 165.6 |
| 3 | 14.7 | 14.6 | 4.7 | 3.7 | 145.0 | 120.9 |
| 4 | 18.4 | 18.0 | 3.3 | 4.4 | 117.7 | 113.2 |
| 5 | 16.7 | 18.3 | 8.8 | 8.9 | 156.0 | 154.0 |
| 6 | 14.1 | 15.2 | 5.0 | 6.5 | 92.3 | 104.7 |
| 7 | 19.7 | 17.0 | 12.5 | 11.0 | 205.5 | 185.8 |
| 8 | 12.7 | 12.5 | 11.6 | 13.2 | 134.3 | 139.2 |
| Operated level | ||||||
| 1 | 13.4 | 13.1 | 11.5 | 12.6 | 162.0 | 159.9 |
| 2 | 11.6 | 13.6 | 10.5 | 11.3 | 135.0 | 149.0 |
| 3 (Cranial) | 15.7 | 17.2 | 6.9 | 4.8 | 126.2 | 123.7 |
| 3 (Caudal) | 13.6 | 13.3 | 9.1 | 8.2 | 128.2 | 122.8 |
| 4 | 15.1 | 15.8 | 8.7 | 8.8 | 158.2 | 159.5 |
| 5 (Cranial) | 17.1 | 17.9 | 7.4 | 7.8 | 151.5 | 152.0 |
| 5 (Caudal) | 12.3 | 14.8 | 8.7 | 8.6 | 117.2 | 144.8 |
| 6 | 19.0 | 21.8 | 10.3 | 10.9 | 179.0 | 231.5 |
| 7 | 15.1 | 15.5 | 8.3 | 11.7 | 136.3 | 169.4 |
| 8 | 11.0 | 12.5 | 13.7 | 14.2 | 143.9 | 166.7 |
| Distal level | ||||||
| 1 | 11.5 | 14.3 | 12.8 | 11.8 | 142.1 | 141.9 |
| 2 | 14.7 | 13.3 | 6.4 | 6.3 | 116.4 | 113.2 |
| 3 | 13.7 | 13.7 | 7.0 | 6.1 | 92.5 | 90.5 |
| 4 | 10.3 | 10.3 | 3.7 | 4.0 | 70.2 | 70.5 |
| 6 | 10.0 | 9.1 | 10.4 | 9.7 | 96.2 | 96.1 |
| 7 | 19.3 | 20.3 | 6.9 | 6.9 | 185.1 | 182.5 |
| 8 | 11.7 | 9.6 | 14.4 | 13.3 | 148.7 | 110.8 |
Height (a) pre-operative IVF height, Height (b) post-operative IVF height, Width (a) pre-operative IVF width, Width(b) post-operative IVF width, Area(a) pre-operative IVF area, Area(b) post-operative IVF area
Table 9.
Pre-Op and Post-Op IVF dimensions during extension (mm/mm2)
| No. | Height (a) | Height (b) | Width (a) | Width (b) | Area (a) | Area (b) |
|---|---|---|---|---|---|---|
| Proximal level | ||||||
| 1 | 13.7 | 12.8 | 5.9 | 8.1 | 100.0 | 98.6 |
| 2 | 17.9 | 15.9 | 12.3 | 10.9 | 173.0 | 152.7 |
| 3 | 17.9 | 17.7 | 3.6 | 4.5 | 138.6 | 126.4 |
| 4 | 17.2 | 18.3 | 5.3 | 4.4 | 129.3 | 125.2 |
| 5 | 15.3 | 17.6 | 5.7 | 9.5 | 93.1 | 131.5 |
| 6 | 16.9 | 16.3 | 7.2 | 5.8 | 122.5 | 113.0 |
| 7 | 17.9 | 18.6 | 10.3 | 10.4 | 177.9 | 199.0 |
| 8 | 12.6 | 12.5 | 12.2 | 15.0 | 129.6 | 150.6 |
| Operated level | ||||||
| 1 | 14.4 | 14.1 | 11.4 | 13.2 | 171.7 | 181.0 |
| 2 | 12.1 | 13.8 | 9.1 | 11.8 | 129.6 | 164.1 |
| 3 (Cranial) | 14.2 | 17.8 | 4.0 | 5.8 | 89.1 | 137.0 |
| 3 (Caudal) | 11.9 | 14.4 | 3.1 | 9.4 | 57.9 | 126.9 |
| 4 | 12.4 | 15.2 | 9.5 | 8.9 | 111.3 | 146.0 |
| 5 (Cranial) | 16.7 | 18.1 | 6.9 | 7.5 | 126.9 | 128.5 |
| 5 (Caudal) | 11.2 | 15.2 | 11.3 | 11.7 | 119.5 | 163.6 |
| 6 | 14.1 | 16.2 | 9.9 | 10.8 | 139.4 | 162.9 |
| 7 | 20.5 | 20.3 | 10.5 | 10.8 | 196.7 | 203.0 |
| 8 | 12.8 | 13.1 | 12.3 | 17.2 | 147.3 | 197.6 |
| Distal level | ||||||
| 1 | 11.1 | 11.5 | 10.4 | 12.2 | 104.7 | 131.2 |
| 2 | 16.2 | 13.8 | 8.4 | 7.1 | 132.9 | 118.6 |
| 3 | 14.8 | 11.5 | 7.5 | 7.1 | 107.3 | 83.7 |
| 4 | 11.6 | 12.4 | 3.4 | 3.4 | 75.4 | 72.4 |
| 6 | 12.5 | 11.2 | 10.5 | 9.7 | 128.3 | 111.6 |
| 7 | 18.1 | 18.9 | 5.5 | 6.7 | 150.3 | 168.0 |
| 8 | 10.2 | 11.4 | 11.9 | 11.3 | 115.0 | 118.3 |
Height (a) pre-operative IVF height, Height (b) post-operative IVF height, Width (a) pre-operative IVF width, Width (b) means post-operative IVF width, Area (a) means pre-operative IVF area, Area (b) post-operative IVF area
Table 10.
Pre-Op and Post-Op IVF dimensions during different functional activities
| No. | Flexion | |||||
|---|---|---|---|---|---|---|
| Height (a) | Height (b) | Width (a) | Width (b) | Area (a) | Area (b) | |
| Proximal level | ||||||
| 1 | 15.1 | 14.7 | 7.5 | 7.4 | 120.8 | 117.9 |
| 2 | 17.2 | 16.7 | 12.3 | 13.1 | 189.6 | 185.9 |
| 3 | 16.6 | 16.0 | 5.1 | 5.6 | 127.0 | 127.6 |
| 4 | 19.3 | 19.2 | 6.2 | 5.1 | 133.8 | 148.6 |
| 5 | 16.2 | 17.3 | 5.7 | 7.3 | 119.1 | 136.3 |
| 6 | 17.7 | 17.1 | 5.4 | 6.5 | 134.5 | 136.9 |
| 7 | 19.0 | 19.1 | 11.2 | 11.3 | 212.1 | 199.0 |
| 8 | 12.5 | 13.6 | 12.3 | 10.8 | 136.4 | 128.9 |
| Operated level | ||||||
| 1 | 16.1 | 15.2 | 9.6 | 12.7 | 178.9 | 201.2 |
| 2 | 14.7 | 13.6 | 10.5 | 10.6 | 159.6 | 154.2 |
| 3 (Cranial) | 18.3 | 18.1 | 4.9 | 5.7 | 149.5 | 143.1 |
| 3 (Caudal) | 12.2 | 13.2 | 7.9 | 8.1 | 115.2 | 118.0 |
| 4 | 15.7 | 14.5 | 12.3 | 10.0 | 181.8 | 155.3 |
| 5 (Cranial) | 21.2 | 19.8 | 15.1 | 8.9 | 252.9 | 166.2 |
| 5 (Caudal) | 10.4 | 15.3 | 8.6 | 7.9 | 105.8 | 139.2 |
| 6 | 15.3 | 16.0 | 10.9 | 11.9 | 153.4 | 179.6 |
| 7 | 20.9 | 23.3 | 10.9 | 10.8 | 221.1 | 248.4 |
| 8 | 12.4 | 12.4 | 14.3 | 14.7 | 158.8 | 162.7 |
| Distal level | ||||||
| 1 | 10.4 | 11.9 | 12.4 | 10.2 | 114.1 | 116.5 |
| 2 | 14.6 | 14.9 | 5.8 | 7.9 | 110.7 | 122.8 |
| 3 | 15.1 | 12.7 | 9.0 | 8.7 | 136.5 | 105.2 |
| 4 | 10.5 | 10.4 | 3.7 | 2.9 | 69.4 | 67.9 |
| 6 | 9.0 | 10.2 | 11.8 | 11.9 | 104.3 | 123.0 |
| 7 | 19.2 | 15.3 | 8.9 | 7.1 | 165.8 | 136.8 |
| 8 | 9.9 | 9.7 | 11.7 | 11.5 | 103.9 | 95.1 |
Height (a) pre-operative IVF height, Height (b) post-operative IVF height, Width (a) pre-operative IVF width, Width (b) post-operative IVF width, Area (a) pre-operative IVF area, Area (b) post-operative IVF area
Table 11.
Pre-Op and Post-Op SSCL during different functional activities
| No. | Upright Standing | Extension | Flexion | |||
|---|---|---|---|---|---|---|
| SSCL (a) | SSCL (b) | SSCL (a) | SSCL (b) | SSCL (a) | SSCL (b) | |
| Proximal level | ||||||
| 1 | 24.3 | 24.6 | 23.3 | 23.2 | 24.9 | 24.7 |
| 2 | 30.1 | 29.0 | 29.5 | 28.8 | 29.7 | 29.0 |
| 3 | 33.8 | 32.2 | 31.0 | 31.8 | 33.2 | 33.3 |
| 4 | 38.0 | 37.3 | 36.5 | 37.9 | 38.7 | 38.4 |
| 5 | 39.0 | 40.2 | 39.7 | 39.7 | 40.4 | 39.1 |
| 6 | 31.4 | 32.7 | 32.6 | 31.8 | 34.5 | 33.2 |
| 7 | 33.4 | 30.8 | 31.7 | 32.7 | 32.9 | 32.4 |
| 8 | 25.6 | 25.6 | 25.9 | 26.5 | 25.7 | 27.0 |
| Operated level | ||||||
| 1 | 22.0 | 22.9 | 23.0 | 23.7 | 24.7 | 24.3 |
| 2 | 27.4 | 27.2 | 27.4 | 27.2 | 27.7 | 27.2 |
| 3 (Cranial) | 29.9 | 31.9 | 29.8 | 30.7 | 31.4 | 32.9 |
| 3 (Caudal) | 27.5 | 28.9 | 28.3 | 29.1 | 27.0 | 29.7 |
| 4 | 29.8 | 29.4 | 27.3 | 29.4 | 30.4 | 28.9 |
| 5 (Cranial) | 31.8 | 31.9 | 30.1 | 32.1 | 30.9 | 33.1 |
| 5 (Caudal) | 31.9 | 32.9 | 32.7 | 32.8 | 32.5 | 33.9 |
| 6 | 28.2 | 29.9 | 28.1 | 29.9 | 29.2 | 30.4 |
| 7 | 35.2 | 38.1 | 36.3 | 37.3 | 35.9 | 38.0 |
| 8 | 23.3 | 24.9 | 24.0 | 26.2 | 24.9 | 24.9 |
| Distal level | ||||||
| 1 | 21.8 | 22.3 | 20.4 | 20.9 | 19.7 | 20.0 |
| 2 | 20.0 | 19.6 | 20.5 | 20.1 | 20.9 | 20.6 |
| 3 | 24.6 | 22.3 | 22.8 | 20.3 | 22.3 | 19.9 |
| 4 | 29.0 | 27.8 | 29.8 | 27.8 | 28.9 | 28.5 |
| 6 | 18.8 | 18.9 | 21.0 | 20.7 | 18.3 | 21.5 |
| 7 | 29.5 | 30.3 | 29.2 | 29.8 | 30.3 | 27.2 |
| 8 | 22.9 | 20.1 | 20.7 | 20.2 | 19.7 | 19.7 |
SSCL(a) pre-operative segmental spinal canal length; SSCL(b) means post-operative segmental spinal canal length
Table 12.
Pre-Op and Post-Op disc space measurements during different functional activities
| No. | Upright Standing | Extension | Flexion | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ant (a) | Ant (b) | Pos (a) | Pos (b) | Ant (a) | Ant (b) | Pos (a) | Pos (b) | Ant (a) | Ant (b) | Pos (a) | Pos (b) | |
| Proximal level | ||||||||||||
| 1 | 3.6 | 5.3 | 1.4 | 2.9 | 5.8 | 5.0 | 1.5 | 1.6 | 6.1 | 5.7 | 3.4 | 2.8 |
| 2 | 5.5 | 5.7 | 3.9 | 3.3 | 4.1 | 6.8 | 3.2 | 3.3 | 4.6 | 4.3 | 3.0 | 3.6 |
| 3 | 9.4 | 8.0 | 3.8 | 1.6 | 7.1 | 7.9 | 0.4 | 0.5 | 8.6 | 5.1 | 1.9 | 1.0 |
| 4 | 10.2 | 10.0 | 2.3 | 1.3 | 8.1 | 10.6 | 0.8 | 2.1 | 11.0 | 9.7 | 3.1 | 2.1 |
| 5 | 5.2 | 9.5 | 4.4 | 6.7 | 6.6 | 8.3 | 5.2 | 5.5 | 8.1 | 9.0 | 6.6 | 5.5 |
| 6 | 7.1 | 5.3 | 1.1 | 1.6 | 7.5 | 5.7 | 2.1 | 1.2 | 9.8 | 6.4 | 3.9 | 2.8 |
| 7 | 2.0 | 3.1 | 1.7 | 1.7 | 0.9 | 1.0 | 0.3 | 0.4 | 0.9 | 0.8 | 1.3 | 0.9 |
| 8 | 4.9 | 4.5 | 3.0 | 4.2 | 4.4 | 3.9 | 3.9 | 6.7 | 4.7 | 6.1 | 4.6 | 3.5 |
| Operated level | ||||||||||||
| 1 | 4.1 | 0.9 | 3.5 | 5.1 | 4.1 | 1.3 | 5.0 | 4.8 | 4.7 | 2.3 | 5.0 | 5.9 |
| 2 | 5.7 | 4.1 | 9.6 | 8.5 | 9.4 | 6.1 | 10.9 | 9.5 | 6.2 | 6.3 | 10.1 | 10.8 |
| 3 (Cranial) | 8.5 | 8.1 | 1.7 | 3.9 | 10.1 | 8.4 | 3.1 | 2.6 | 11.6 | 8.8 | 4.0 | 4.1 |
| 3 (Caudal) | 9.8 | 9.1 | 1.1 | 1.8 | 8.9 | 9.8 | 3.2 | 0.8 | 11.6 | 8.6 | 3.6 | 0.8 |
| 4 | 9.1 | 8.0 | 5.4 | 2.9 | 9.5 | 8.1 | 2.0 | 2.1 | 6.7 | 6.0 | 6.0 | 3.3 |
| 5 (Cranial) | 10.7 | 8.9 | 5.3 | 6.0 | 10.2 | 12.8 | 5.5 | 6.3 | 7.3 | 9.6 | 5.9 | 7.2 |
| 5 (Caudal) | 11.5 | 8.7 | 5.4 | 4.6 | 10.2 | 8.0 | 6.9 | 4.2 | 8.1 | 7.8 | 5.8 | 5.2 |
| 6 | 7.9 | 7.8 | 3.5 | 6.2 | 4.6 | 6.1 | 3.4 | 5.4 | 6.6 | 7.4 | 2.9 | 6.1 |
| 7 | 7.6 | 6.8 | 1.1 | 2.4 | 8.9 | 8.5 | 1.3 | 2.4 | 6.3 | 5.7 | 0.7 | 2.6 |
| 8 | 4.7 | 3.7 | 7.6 | 7.1 | 4.7 | 4.4 | 6.6 | 9.9 | 6.6 | 5.2 | 7.9 | 7.6 |
| Distal level | ||||||||||||
| 1 | 8.8 | 7.9 | 3.5 | 3.4 | 6.5 | 6.9 | 2.6 | 3.2 | 5.2 | 7.4 | 2.3 | 1.9 |
| 2 | 2.8 | 5.2 | 1.2 | 3.3 | 3.2 | 4.8 | 1.9 | 2.1 | 4.6 | 3.1 | 2.2 | 2.2 |
| 3 | 9.8 | 11.1 | 1.1 | 1.8 | 8.9 | 9.8 | 3.2 | 0.8 | 11.6 | 8.6 | 3.6 | 0.8 |
| 4 | 4.4 | 4.2 | 0.7 | 1.2 | 5.6 | 7.5 | 0.7 | 0.4 | 4.8 | 3.3 | 0.7 | 1.1 |
| 6 | 6.1 | 4.6 | 2.2 | 1.5 | 7.0 | 9.6 | 1.0 | 3.5 | 7.0 | 5.8 | 1.0 | 4.5 |
| 7 | 6.2 | 8.1 | 1.0 | 1.9 | 7.9 | 6.1 | 1.3 | 0.7 | 7.6 | 3.9 | 2.0 | 0.9 |
| 8 | 12.7 | 8.1 | 7.0 | 3.7 | 8.9 | 8.5 | 4.5 | 4.0 | 8.2 | 6.3 | 3.0 | 1.9 |
Ant (a) pre-operative anterior disc height, Ant (b) post-operative anterior disc height, Pos(a) pre-operative posterior disc height, Pos(b) post-operative posterior disc height
References
- 1.Verbiest H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954;36-B:230–237. doi: 10.1302/0301-620X.36B2.230. [DOI] [PubMed] [Google Scholar]
- 2.Inufusa A, An HS, Lim TH, Hasegawa T, Haughton VM, Nowicki BH. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion–extension movement. Spine. 1996;21:2412–2420. doi: 10.1097/00007632-199611010-00002. [DOI] [PubMed] [Google Scholar]
- 3.Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:198–207. doi: 10.1097/01.blo.0000198722.70138.96. [DOI] [PubMed] [Google Scholar]
- 4.Burnett MG, Stein SC, Bartels RH. Cost-effectiveness of current treatment strategies for lumbar spinal stenosis: nonsurgical care, laminectomy, and X-STOP. J Neurosurg Spine. 2010;13:39–46. doi: 10.3171/2010.3.SPINE09552. [DOI] [PubMed] [Google Scholar]
- 5.Juricek M, Rehak L, Horvath J, Tisovsky P. Quality of life after elective lumbar spinal fusions. Bratisl Lek Listy. 2010;111:290–295. [PubMed] [Google Scholar]
- 6.Lee J, Hida K, Seki T, Iwasaki Y, Minoru A. An interspinous process distractor (X STOP) for lumbar spinal stenosis in elderly patients: preliminary experiences in 10 consecutive cases. J Spinal Disord Tech. 2004;17:72–77. doi: 10.1097/00024720-200402000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Bono CM, Vaccaro AR. Interspinous process devices in the lumbar spine. J Spinal Disord Tech. 2007;20:255–261. doi: 10.1097/BSD.0b013e3180331352. [DOI] [PubMed] [Google Scholar]
- 8.Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003;28:2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 9.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio ST, Cauthen JC, Ozuna RM. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine. 2005;30:1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]
- 10.Kondrashov DG, Hannibal M, Hsu KY, Zucherman JF. Interspinous process decompression with the X-STOP device for lumbar spinal stenosis: a 4-year follow-up study. J Spinal Disord Tech. 2006;19:323–327. doi: 10.1097/01.bsd.0000211294.67508.3b. [DOI] [PubMed] [Google Scholar]
- 11.Kuchta J, Sobottke R, Eysel P, Simons P. Two-year results of interspinous spacer (X-Stop) implantation in 175 patients with neurologic intermittent claudication due to lumbar spinal stenosis. Eur Spine J. 2009;18:823–829. doi: 10.1007/s00586-009-0967-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richards JC, Majumdar S, Lindsey DP, Beaupre GS, Yerby SA. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine. 2005;30:744–749. doi: 10.1097/01.brs.0000157483.28505.e3. [DOI] [PubMed] [Google Scholar]
- 13.Nandakumar A, Clark NA, Peehal JP, Bilolikar N, Wardlaw D, Smith FW. The increase in dural sac area is maintained at 2 years after X-stop implantation for the treatment of spinal stenosis with no significant alteration in lumbar spine range of movement. Spine J. 2010;10:762–768. doi: 10.1016/j.spinee.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Siddiqui M, Karadimas E, Nicol M, Smith FW, Wardlaw D. Influence of X Stop on neural foramina and spinal canal area in spinal stenosis. Spine (Phila Pa 1976) 2006;31:2958–2962. doi: 10.1097/01.brs.0000247797.92847.7d. [DOI] [PubMed] [Google Scholar]
- 15.Wan Z, Wang S, Kozanek M, Passias PG, Xia Q, Mansfield FL, Wood KB, Li G (2011) Effect of X-Stop implantation on vertebral and interspinous process motion. In: 57th Annual Meeting of the Orthopaedic Research Soceity Long Beach, California
- 16.Wang S, Passias P, Li G, Wood K. Measurement of vertebral kinematics using noninvasive image matching method-validation and application. Spine. 2008;33:355–361. doi: 10.1097/BRS.0b013e3181715295. [DOI] [PubMed] [Google Scholar]
- 17.Li G, Wang S, Passias P, Xia Q, Wood K. Segmental in vivo vertebral motion during functional human lumbar spine activities. Eur Spine J. 2009;18:1013–1021. doi: 10.1007/s00586-009-0936-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fujiwara A, An HS, Lim TH, Haughton VM. Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine. 2001;26:876–882. doi: 10.1097/00007632-200104150-00010. [DOI] [PubMed] [Google Scholar]
- 19.Ge Y, Maurer CR, Fitzpatrick JM. Surface-based 3D image registration using the iterative closest point algorithm with a closest-point transform. Med Imaging Image Process. 1996;2710:358–367. [Google Scholar]
- 20.Wang S, Xia Q, Passias P, Wood K, Li G. Measurement of geometric deformation of lumbar intervertebral discs under in vivo weightbearing condition. J Biomech. 2009;42:705–711. doi: 10.1016/j.jbiomech.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Schlegel JD, Champine J, Taylor MS, Watson JT, Champine M, Schleusener RL, Savory KM. The role of distraction in improving the space available in the lumbar stenotic canal and foramen. Spine. 1994;19:2041–2047. doi: 10.1097/00007632-199409150-00004. [DOI] [PubMed] [Google Scholar]
- 22.Bayley JC, Yoo JU, Kruger DM, Schlegel J. The role of distraction in improving the space available for the cord in cervical spondylosis. Spine. 1995;20:771–775. doi: 10.1097/00007632-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Siddiqui M, Nicol M, Karadimas E, Smith F, Wardlaw D. The positional magnetic resonance imaging changes in the lumbar spine following insertion of a novel interspinous process distraction device. Spine. 2005;30:2677–2682. doi: 10.1097/01.brs.0000187878.79676.26. [DOI] [PubMed] [Google Scholar]