Abstract
Purpose
Nowadays, endoscopic techniques are widely used in surgical procedures. Retroperitoneoscopy has been an extremely valuable tool for a wide variety of urologic disorders, whereas, it has limited use in orthopedic procedures.
Methods
We performed retroperitoneoscopic drainage (in combination with medical treatment) of complicated psoas abscess on 12 patients with tuberculous spondylitis. All the procedures were done under general anesthesia and in the lateral decubitus position. Psoas abscess was evacuated during procedure, and postoperatively, drainage was continued through a large silastic tube. The definitive diagnosis and the treatment were made based on the results of culture-antibiogram and PCR testing.
Results
Complete clinical and radiologic remission was observed in all patients in 3–6 months. The complication was not observed in any case postoperatively.
Conclusions
Retroperitoneoscopic drainage of psoas abscesses gains advantages in terms of rapid recovery, minimal invasiveness, absence of radiation, and shorter hospital stay. This procedure can be used not only for cold abscesses but also for other pathologies of lumbar vertebral area.
Keywords: Retroperitoneoscopy, Tuberculous spondylitis, Psoas abscess
Introduction
Patients with tuberculous spondylitis (including cold abscess) can usually be treated with drug therapy alone [1], nevertheless, open surgical techniques are indicated under circumstances such as ineffective drug treatment or drug resistant tuberculosis, neurological deficit, spinal instability, complicated abscess formation, and discitis [2–5]. Endoscopic or image-guided spinal abscess drainages have superior advantages over the traditional surgical techniques [6]. Transpedicular abscess drainage can be also done in appropriate cases [7].
Retroperitoneoscopy is a reliable and widespread method for treating urological problems [8]. The fascia of the psoas muscle with posterior perirenal fascia is anatomically placed in the retroperitoneal space [9], so we had thought that retroperitoneoscopic drainage can be used instead of open surgical drainage for psoas abscesses. To our knowledge, only two publications regarding endoscopic drainage of psoas abscess were reported in the English literature [10, 11].
We report a series of 12 cases of complicated tuberculous psoas abscesses that were drained by retroperitoneoscopic technique from August 2007 to August 2010.
Materials and methods
All patients were evaluated by plain radiographs and MRI, preoperatively. Abscess location and the depth of invasion of abscess were determined by MRI. Before procedure, a general surgeon had evaluated all the patients to rule out an intraabdominal pathology causing psoas abscess. Definitive diagnosis was done microbiologically [by both culture and polymerase chain reaction (PCR)].
Patients with loss of excessive vertebral height or vertebral destruction were excluded from this study. These patients had undergone other major surgeries such as spinal fusion with/without instrumentation, laminectomy, and spinal cord decompression.
All the patients were discharged from the hospital with anti-tuberculosis medication. Postoperatively, patients were followed at intervals of 3 months. The loss of vertebral height, alignment of vertebra and its destruction were evaluated by roentgenograms. Recovery monitoring was performed by erythrocyte sedimentation rate, C-reactive protein level, and neurological status.
Technique
All the procedures were done in the lateral decubitus position under general anesthesia. Access to the retroperitoneal space was obtained with the open technique through a 1.5-cm subcostal incision under the extremity of the 12th rib and muscle divulsion up to the aponeurosis of the transverse muscle, which was then opened, and the fascia transversalis, identifying the prerenal fat. The creation of a working space in the retroperitoneum was performed by a balloon. A Hasson trocar was inserted in this space and fixed to the musculature with a purse-string suture in order to avoid air leakage and development of subcutaneous emphysema, and CO2 insufflation was performed until reaching 12-mmHg tension. We used 0° optics and, when needed, the working space was completed using the optics under visualization. Two additional trocars were placed with the finger guidence; a 5-mm trocar on the hemiclavicular line just above the iliac spine and caudally to the optics port, and a 5- or 10-mm trocar posterior to the optics at the posterior axillary line, forming a triangle. When the psoas muscle and abscess become visible, a 2-cm incision was made in the fascia overlying the muscle, and pus was removed by suction and abscess cavity was irrigated with saline solution, after collecting 10 mL for microbial culture. A large silastic drain was placed into the abscess cavity and removed on second or third day, postoperatively.
Results
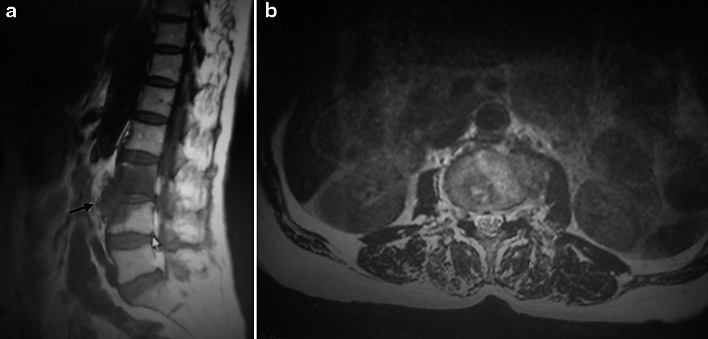
Patient characteristics and demographics are shown in Table 1. Prospectively, we performed a retroperitoneoscopic procedure in 12 patients. A patient with excessive hip flexion contracture complicated by psoas abscess has healed fully after retroperitoneoscopic drainage, and flexion contracture of the hip was rapidly improved with postoperative skin traction for 2–3 days (case 1) (Fig. 1a, b).
Table 1.
Patient characteristics and demographics
| Initials of patients | Age (years) | Sex | Side | Localization of abscess | Complication | Recovery |
|---|---|---|---|---|---|---|
| 1. E.S. | 21 | F | Left | Retroperitoneum | Flexion contracture of hip | Full |
| 2. H.K. | 25 | F | Right | Retroperitoneum, groin area and posterior of knee | Sepsis | Full |
| 3. E.K. | 68 | F | Left | Retroperitoneum | L3–L4 discitis, left sciatalgica | Full |
| 4. E.Ç. | 15 | F | Left | Retroperitoneum | L3 discitis | Full |
| 5. A.S. | 24 | M | Right | Retroperitoneum, and Petit triangle | Right sciatalgica | Full |
| 6. M.T. | 74 | F | Left | Retroperitoneum | Epidural abscess | Full |
| 7. A.L. | 63 | F | Left | Retroperitoneum | Left sciatalgica | Full |
| 8. S.T. | 51 | M | Right | Retroperitoneum and groin | Flexion contracture of hip | Full |
| 9. M.S. | 28 | F | Left | Retroperitoneum | L2 discitis | Full |
| 10. O.T. | 27 | F | Right | Retroperitoneum | Persistant low back pain | Full |
| 11. E.B. | 41 | M | Left | Retroperitoneum | L2 discitis | Full |
| 12. Z.A. | 49 | F | Left | Retroperitoneum | Epidural abscess | Full |
F female, M male
Fig. 1.
a Sagittal MR image, a large psoas abscess, definitive diagnosis was made microbiologically. b At same patient, axial MRI image demonstrating a left cold psoas abscess
The rubber tube put into the operation site was removed after 2–3 days in all patients, except for one case with sepsis. This patient had also a sizeable abscess along the ipsilateral groin and popliteal fossa, and retroperitoneoscopic drainage was simultaneously performed with groin drainage by mini-incision anterior approach (case 2) (Fig. 2). In this patient, septic shock have dramatically improved at postoperative second day. A week later we removed her drainage tube.
Fig. 2.
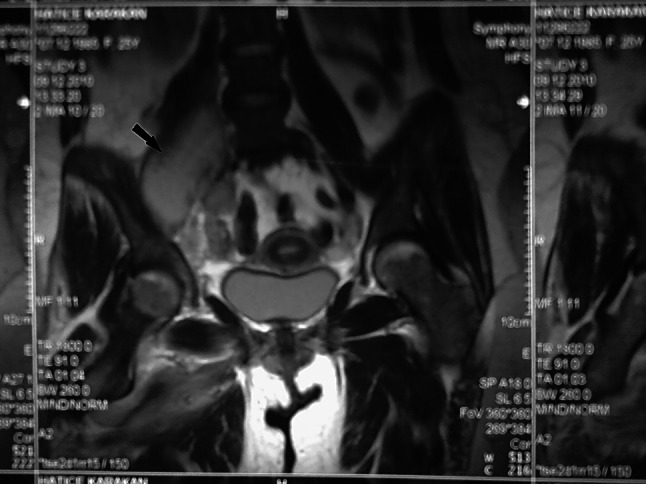
Coronal MRI of the vertebra. A right large cold psoas abscess
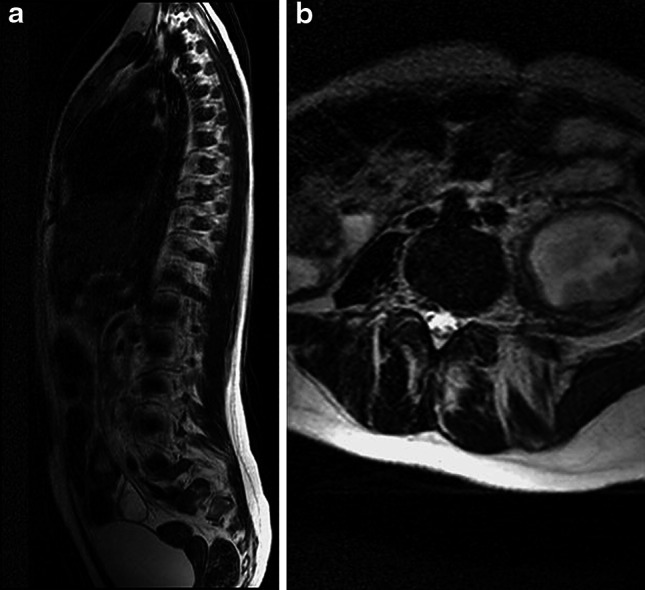
In a patient that admitted to our clinic after failed needle aspiration, we successfully drained the abscess by retroperitoneoscopic procedure and achieved successful result (case 3) (Fig. 3a, b).
Fig. 3.
a Sagittal MRI of the vertebral column. Discitis and osteomyelitis at L3 to L4 and paravertebral cold abscess. Indistinctness of the psoas muscle margin and enlarged psoas muscle and preserved vertebral height. b Axial MRI of the same patient. A large cold psoas abscess. Definitive diagnosis was made microbiologically
After treatment, all patients were became free of disease at a mean follow-up of 6 months. After 1–3 months the patients’ clinical symptoms resolved, C-reactive protein (CRP) and sedimentation rate decreased to normal values. The periodic roentgenograms did not revealed any loss of height or destruction of vertebral bodies.
Discussion
The primary therapy of spinal tuberculous abscesses is done with appropriate anti-tuberculous drugs. If the treatment is neglected, serious complications can occur such as discitis [12], epidural abscess [13, 14], fatal outcome [15, 16], fistulization of the adjacent organs [17–19], and pediatric spondylolisthesis [20].
For a long time we had performed the open surgical treatment for psoas abscesses and we had achieved successful results. With the popularity of endoscopic procedures, 2 years ago, we initiated the retroperitoneoscopic procedure for only psoas abscesses in the tuberculous spondylitis.
We have successfully treated the 12 patients with retroperitoneoscopy. In only one patient, we performed open drainage for groin area in addition to retroperitoneoscopy and gained to successful result.
We also applied this technique in a patient after failed simple needle aspiration performed in another hospital, and the patient recovered fully. Based on our experience, in tuberculous spondylitis, abscesses can be purulent with high density. Therefore, the width of the mouth of the used instrument for drainage should be large, and diameter of our used instrument was 5 mm.
In previous published articles, about retroperitoneoscopic procedures, various complications and failed attempts have been reported [3, 10, 21, 22]. In a series of 600 urological cases, the authors have reported complication rates of 5.3% including bleeding or hematoma, and conversion rates to open surgery of 4.6% [3]. In a orthopedic series of 20 cases, the three cases with bleeding and one case with peritoneum penetration has been reported [10]. However, with increasing experience the complication rates decrease [22].
We did not meet any complication in our cases, intraoperatively. Each of the patients was examined roentgenographically at least 6 months postoperatively, and there was no complication such as loss of height or destruction of the vertebral body.
Although the CT-guided drainage was reported to be used successfully in the drainage of psoas abscesses, the risk of high dose of radiation should be kept in mind [23].
We only used this technique for drainage of complicated lumbar psoas abscesses and we achieved the successful results.
Conclusion
Retroperitoneoscopic drainage of psoas abscesses gains advantages in terms of rapid recovery, minimally invasiveness, absence of radiation, and shorter hospital stay. We think that retroperitoneoscopic drainage of psoas abscess is a safe method in patients with tuberculous lomber spondylitis. In addition, we think that retroperitoneoscopic procedure can be used not only for cold abscesses, but also for other pathologies of lumbar vertebral area.
Conflict of interest
None.
References
- 1.Wimmer C, Ogon M, Sterzinger W, Landauer F, Stöckl BJ. Conservative treatment of tuberculous spondylitis: a long-term follow-up study. J Spinal Disord. 1997;10:417–419. doi: 10.1097/00002517-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg (Br) 2010;92:905–913. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 3.Lifeso RM, Weaver P, Harder EH. Tuberculous spondylitis in adults. J Bone Joint Surg (Am) 1985;67:1405–1413. [PubMed] [Google Scholar]
- 4.Janssens JP, de Haller R. Spinal tuberculosis in a developed country. A review of 26 cases with special emphasis on abscesses and neurologic complications. Clin Orthop. 1990;257:67–75. [PubMed] [Google Scholar]
- 5.Ng AW, Chu WC, Ng BK, Li AM. Extensive paraspinal abscess complicating tuberculous spondylitis in an adolescent with Pott kyphosis. Clin Imaging. 2005;29:359–361. doi: 10.1016/j.clinimag.2005.01.025. [DOI] [PubMed] [Google Scholar]
- 6.Powell MF, DiNobile D, Reddy AS. C-arm fluoroscopic cone beam CT for guidance of minimally invasive spine interventions. Pain Physician. 2010;13:51–59. [PubMed] [Google Scholar]
- 7.Arora S, Kumar R, Batra S, Nath R (2010) Transpedicular drainage of presacral abscess and posterior decompression of acute cauda equina syndrome in caries spine: a case series of 3 patients. J Spinal Disord Tech 24(3):26–30 [DOI] [PubMed]
- 8.Liapis D, de la Taille A, Ploussard G, Robert G, Bastien L, Hoznek A, Vordos D, Abbou C, Salomon L. Analysis of complications from 600 retroperitoneoscopic procedures of the upper urinary tract during the last 10 years. World J Urol. 2008;26:523–530. doi: 10.1007/s00345-008-0319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burkill GJC, Healy JC. Anatomy of the retroperitoneum. Imaging. 2000;12:10–20. [Google Scholar]
- 10.Atkin G, Qurashi K, Isla A. Laparoscopic drainage of bilateral tuberculous psoas abscesses. Surg Laparosc Endosc Percutan Tech. 2005;15:380–382. doi: 10.1097/01.sle.0000191590.92108.c4. [DOI] [PubMed] [Google Scholar]
- 11.Katara AN, Shah RS, Bhandarkar DS, Unadkat RJ. Retroperitoneoscopic drainage of a psoas abscess. J Pediatr Surg. 2004;39:e4–e5. doi: 10.1016/j.jpedsurg.2004.05.033. [DOI] [PubMed] [Google Scholar]
- 12.Mulleman D, Mammou S, Griffoul I, Avimadje A, Goupille P. Characteristics of patients with spinal tuberculosis in a French teaching hospital. Joint Bone Spine. 2006;73:424–427. doi: 10.1016/j.jbspin.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Buyukbebeci O, Karakurum G, Guleç A, Erbagci A. Tuberculous osteomyelitis of the lumbosacral region: a spinal epidural abscess with presacral extension. Arch Orthop Trauma Surg. 2004;124:346–348. doi: 10.1007/s00402-004-0660-y. [DOI] [PubMed] [Google Scholar]
- 14.Pareyson D, Savoiardo M, D’Incerti L, Sghirlanzoni A. Spinal epidural abscess complicating tuberculous spondylitis. Ital J Neurol Sci. 1995;16:321–325. doi: 10.1007/BF02249108. [DOI] [PubMed] [Google Scholar]
- 15.Kanaan IU, Ellis M, Safi T, Al Kawi MZ, Coates R. Craniocervical junction tuberculosis: a rare but dangerous disease. Surg Neurol. 1999;51:21–26. doi: 10.1016/S0090-3019(97)00294-2. [DOI] [PubMed] [Google Scholar]
- 16.Dahl T, Lange C, Ødegård A, Bergh K, Osen SS, Myhre HO. Ruptured abdominal aortic aneurysm secondary to tuberculous spondylitis. Int Angiol. 2005;24:98–101. [PubMed] [Google Scholar]
- 17.Yau AC, Hodgson AR. Penetration of the lung by the paravertebral abscess in tuberculosis of the spine. J Bone Joint Surg (Am) 1968;50:243–254. doi: 10.2106/00004623-196850020-00003. [DOI] [PubMed] [Google Scholar]
- 18.Blumenthal DH, Morin ME, Tan A, Li YP. Intestinal penetration by tuberculous psoas abscess. AJR Am J Roentgenol. 1981;136(5):995–997. doi: 10.2214/ajr.136.5.995. [DOI] [PubMed] [Google Scholar]
- 19.Johnson AD, Mcintosh WJ. Tuberculous fistula between the 5th lumbar vertebra and the colon presenting as a left thigh abscess. Br J Surg. 1978;65:186–187. doi: 10.1002/bjs.1800650313. [DOI] [PubMed] [Google Scholar]
- 20.Kirkman MA, Sridhar K. Posterior listhesis of a lumbar vertebra in spinal tuberculosis. Eur Spine J. 2010;20:1–5. doi: 10.1007/s00586-010-1524-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blaser A, Rosset P. Fatal carbon dioxide embolism as an unreported complication of retroperitoneoscopy. Surg Endosc. 1999;13:713–714. doi: 10.1007/s004649901079. [DOI] [PubMed] [Google Scholar]
- 22.Teber D, Tefekli A, Eskicorapci S, Gözem AS, Bujosevic S, Sugiono M, Stock C, Rassweiler JJ (2006) Retroperitoneoscopy: a versatile access for many urologic indications. European urology 5(suppl):975–982
- 23.Cantasdemir M, Kara B, Cebi D, Selcuk ND, Numan F. Computed tomography-guided percutaneous catheter drainage of primary and secondary iliopsoas abscesses. Clin Radiol. 2003;58(10):811–815. doi: 10.1016/S0009-9260(03)00274-5. [DOI] [PubMed] [Google Scholar]