Abstract
Introduction
Among ischemic stroke patients arriving within the treatment window, rapidly improving symptoms or having a mild deficit (i.e. too good to treat)is a common reason for exclusion. Several studies have reported poor outcomes in this group. We addressed the question of early neurological deterioration in too good to treat patients in a larger prospective cohort study.
Methods
Admission and discharge information were collected prospectively in acute stroke patients who presented to the emergency room within three-hours from onset. The primary outcome measure was change in the NIHSS from baseline to discharge. Secondary outcomes were discharge NIHSS>4, not being discharged home, and discharge modified Rankin scale.
Results
Of 355patients who presented within three-hours, 127 (35.8%) had too good to treat listed as the only reason for not receiving thrombolysis, with median admission NIHSS = 1 (range = 0 to 19). At discharge seven(5.5%) showed a worsening of NIHSS ≥1 and 9 (7.1 %) had an NIHSS > 4. When excluding prior stroke (remaining n= 97), discharge status was even more benign: only five (5.2%) had a discharge NIHSS > 4 and two (2.1%) patients were not discharged home.
Conclusion
We found that a small proportion of patients deemed too good to treat will have early neurological deterioration, in contrast to other studies. Decisions about whether to treat mild stroke patients depend on the outcome measure chosen, particularly when considering discharge disposition among patients who have had prior stroke. The decision to thrombolyze may ultimately rest on the nature of the presentation and deficit.
Introduction
The only Food and Drug Administration-approved treatment for acute ischemic stroke is intravenous (IV) tissue plasminogen activator (tPA)1. Thrombolysis with IV tPA improves outcomes and is associated with reasonably low complication rates2–4. Despite these results, few patients actually receive IV tPA5. Up to 18% of patients have been estimated to not receive IV tPA when they are in fact eligible6.
Several reasons have been identified for the low rates of thrombolysis, the most common being arrival outside of the appropriate time window7. Approximately 1/3 of stroke patients who arrive within the three-hour treatment window are excluded from thrombolysis because they are deemed too good to treat (TGT) by treating physicians6–9, while close to 50% of stroke admissions involve those with a national institutes of health stroke scale (NIHSS) ≤ 510. In the National Institute of Neurological Disorders and Stroke rt-PA study 13% of the screened patients were not randomized due to being TGT2, and only 58 with an NIHSS ≤ 5 were randomized11, providing little clinical trial guidance on how to treat these patients. The wisdom of this exclusion has been questioned, however, because of the potential for early neurological deterioration in this group. We used a prospective cohort to examine this question in a multi-ethnic, urban population.
Methods
Our data were drawn from the Specialized Program of Translational Research in Acute Stroke (SPOTRIAS) grant at Columbia University Medical Center. Demographic, social, and clinical information from hospitalized stroke patients was collected by review of the medical record and interviews with the patients and entered into a registry. We collected data, including admission and discharge National Institutes of Health Stroke Scale (NIHSS), on all patients who presented to the emergency room within 12 h from stroke onset and who either consented to participate in the registry or were included by means of an institutional review board (IRB)-approved waiver of consent. Our analysis was limited to those with final diagnosisof ischemic stroke or transient ischemic attack (TIA)admitted between December 1, 2004 and November 30,2008. We analyzed outcomes for those who were deemed TGT based on an explicit statement by the treating neurologist in the emergency room. our institution did not have standardized criteria for defining TGT, but relied on the clinical judgment and experience of the stroke neurologist. Rapid improvement was defined based on change while in the emergency room. Patients with prior stroke were not excluded if a clear determination of the patient’s baseline could be made by the neurologist in the emergency room. Clinical information obtained in all patients included stroke subtype using TOAST criteria12, medical co-morbidities (hypertension, diabetes, dyslipidemia, prior stroke or myocardial infarction), radiological findings, initial and discharge NIHSS, and discharge disposition. We did not routinely obtain vascular imaging in the emergency room. Our primary outcome measure was a decline in the NIHSS (discharge NIHSS minus admission NIHSS), which has been commonly examined in other studies of TGT patients, and is implicated as the principal reason for poor neurological outcomes13–15.
Secondary outcomes were:
discharge to other than home 15
NIHSS > 4at discharge.
We also looked for variables to explain differences in outcomes with in our TGT cohort. Continuous variables were compared using a 2-sidedt-test. Univariate analyses for categorical outcomes were carried out using a chi-squared statistic. Odds ratios (OR) were calculated for each of the outcomes of interest to compare the poor and good outcomes within the TGT patients. All analyses were carried out with SAS version 9.1 (Cary, N.C.). The study was approved by the CUMC IRB.
Results
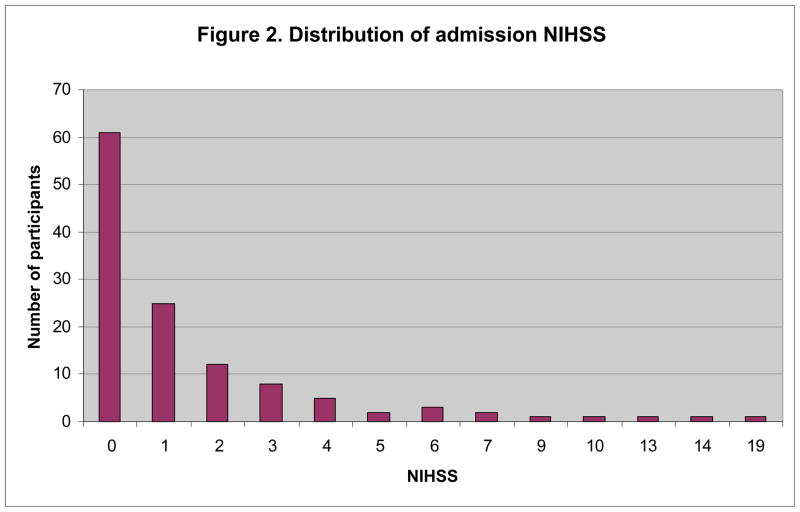
Of 355 patients who presented to the ED within three-hours from symptom onset, 127 had TGT as their only exclusion for thrombolysis; of those deemed TGT 48 (38%) had a final diagnosis of ischemic stroke, and 79 (62%) had a final diagnosis of TIA. Other reasons for exclusion from treatment included not being able to initiate treatment within three-hours (n = 103), seizure at onset (n = 4), prior intracerebral hemorrhage (n = 4), and the coagulation profile indicating an international normalized ratio of > 1.7 (n = 2); the remaining patients had more than one reason for being excluded. Table 1 outlines baseline demographic features of the TGT sample. The mean age was 64.8 ± 16.1, and 65 were women. Hispanics comprised most of our sample (n = 68, 53.5%), followed by whites (n =29, 22.8%), and blacks (n =23, 18.1%), with seven patients having other or missing race-ethnicity. Of the 127TGT patients, 30(23.6%)had a prior ischemic stroke. The mean NIHSS among those TGT at arrival was 1.6 ± 2.9, median NIHSS was 1, with a maximal score of 19; 61 patients (49.6%) had an NIHSS of 0 on admission. The patients with an NIHSS of 13, 14, and 19 had a prior stroke and dementia, which accounted for the high score, though TGT was the sole criterion used by the stroke neurologist for not treating. The distribution of admission NIHSS scores for the sample is illustrated in Figure 1.
Table 1.
Baseline demographics of the too good to treat sample
| Mean or number (SD or proportion) for total sample (n = 127) | |
|---|---|
| Age | 64.8 (16.1) |
| Women | 63 (49.6%) |
| Race-ethnicity | |
| Hispanic | 66 (53.5%) |
| White | 28 (22.8%) |
| Black | 23 (18.1%) |
| Missing/other | 10 (5.5%, 7 missing, 3 others) |
| Prior ischemic stroke | 30 (23.6%) |
| Mean NIHSS on admission (Median) | 1.6 (1) |
Figure 1.
Distribution of admission NIHSS in all of the too good to treat patients (n = 127)
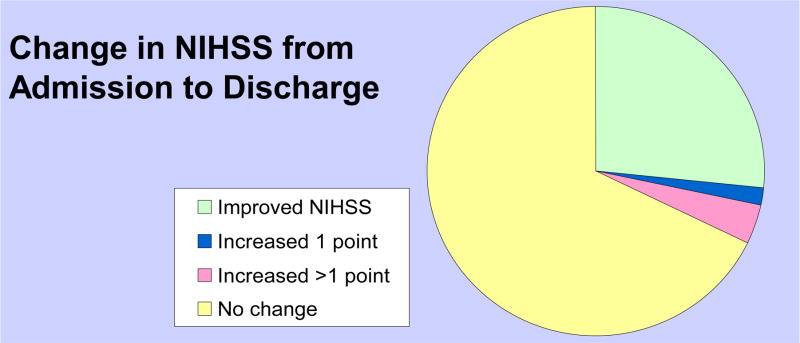
Comparing admission to discharge NIHSS, 86 patients had no change in their NIHSS, two had an increase of 1 point, and five(3.9%) had an increase greater than 1 point (two with a 7 point increase, one with 2 point and one with 6 point increase, one death); the other 34 had an improvement in their NIHSS (Figure 2). Ten (7.9 %) had an NIHSS > 4at discharge. A total of 13 patients (10.2 %) were discharged to somewhere other than home, nine to acute rehabilitation, three to sub-acute facilities, and one who died due to hemorrhagic transformation with subsequent withdrawal of care (patient with prior stroke)(Table 2). Among those with a final diagnosis of TIA 75 (95.8%) were discharged home, compared to those with ischemic stroke (n = 37, 77.1%).
Figure 2.
Change in NIHSS from Admission to Discharge in the Too Good To Treat Patients (n = 127)
No change in NIHSS: 86 (67.7%)
One point increase in NIHSS: 2 (1.6%)
More than one point increase in NIHSS: 5 (3.9%)
Improvement in NIHSS: 34 (26.8%)
Table 2.
Secondary outcomes in the too good to treat patients
| Outcome | TGT (n=127) | No prior stroke (n=97) | |
|---|---|---|---|
| Discharge disposition | Home | 114 (89.8 %) | 94 (97.0%) |
| Acute Rehabilitation | 9 (7.1 %) | 1 (1.0%) | |
| Sub-acute Rehabilitation | 3 (2.4 %) | 1 (1.0%) | |
| Death | 1 (0.7%) | 1 (1.0%) | |
| NIHSS at discharge | 0–1 | 102 (80.3%) | 86 (88.7 %) |
| 2–4 | 15 (11.8 %) | 6 (6.2 %) | |
| 5–10 | 6 (4.7 %) | 3 (3.1%) | |
| 11–42 | 4 (3.2 %) | 2 (2.0%) | |
We carried out analyses excluding patients with prior stroke to explore if outcomes based only on discharge status were driven by patients with a prior neurological deficit since there was a trend towards poor outcomes in this group(Table 2). All had been living at home before their admission. Only two (2.1%) were discharged to other than home: one to an acute rehabilitation facility, and one to a nursing home. Five of the patients had an admission NIHSS of > 4.
During this time period we treated 18 patients with an NIHSS of 0–5, of whom 11were discharged home (61.1%), one died due to multi-organ system failure and sepsis, and eight (44.4%) had an NIHSS > 2 (five with an NIHSS of 3, one with an NIHSS of 4, two with an NIHSS of 5). There were no symptomatic hemorrhages in this group.
In univariate analysis, most of the collected demographic or clinical variables were not associated with the primary outcome, including stroke subtype, baseline NIHSS, serum glucose, gender, and race-ethnicity. Among the secondary outcomes age at baseline was the only predictor of not being discharged to home within the TGT sample (OR 1.05, 95% CI 1.01–1.1). Multi-variable models were not carried out because of the small number of outcomes.
Discussion
Our cohort is one of the first to examine the question of early neurological deterioration and outcomes in mildly affected or rapidly improving acute stroke patients who are not treated with IV tPA. We, like others, have found that a high proportion of patients are not treated with IV tPA because they are deemed TGT, and yet few have early neurological deterioration. In our cohort of TGT patients we found that in only three(2.4 %) was there an increase in NIHSS from admission to discharge, a better outcome than previous studies reporting neurological deterioration during the inpatient admission15. Overall 120 out of 127 (94%)of our patients had no change or an improvement in their NIHSS. Interestingly, when choosing static outcomes that describe patient status at a given time point (our secondary outcomes) 10%were discharged to other than home, and 7% had discharge NIHSS >4. We found that our relatively high proportion with a poor static outcomes(discharge to other than home) appeared to be largely driven by the patients with prior neurological deficits from previous strokes, whereas the impact of prior neurological deficits is accounted for in only one prior report 15.
Static discharge outcomes have been evaluated in several studies: two examined discharge to home as an outcome9, 15, and two others examined functional status14, 16. In the study from UCLA, 20% of TGT patients exhibited a poor functional outcome at discharge as defined by the mRS, though this study included patients eligible for endovascular therapy14. In a single center prospective database eleven of 41 considered TGT died or were not discharged home (27%), mostly due to persistent neurological deficits or clinical worsening15, while in another California based registry 34% of the TGT patients were not discharged home or able to walk9. One third of patients in another report who were excluded from IV tPA for being TGT subsequently died or were left dependent16. As in our study, being TGT was defined by the judgment of the physician. The few studies that have evaluated three-month outcomes report inconsistent results. In one report 25% of patients who were TGT had an unfavorable three-month outcome as measured by an mRS ≥ 213. In contrast to this study, Dutch investigators found that among 27 of 81 (33%) who were not given IV tPA because they were TGT, 24 out of 27 had an mRS of 0–1 with all 27 living independently at home17. In one study change in NIHSS was used as an outcome, patients with a greater than 4 point increase in the NIHSS worsened due to expansion of the infarct15. A recent report examining 760 patients with minor stroke examined both discharge and 90-day outcomes noted the best outcomes among patients with an NIHSS of ≤ 318.
Reasons for our differences with previously reported studies are difficult to pinpoint. Comparisons are challenging given the heterogeneity of TGT definitions, discharge outcomes, and timing of follow-up. One possibility for our better outcomes could have been that patients with large vessel occlusion, more severe syndrome at onset, or isolated motor symptoms, factors cited as predictive of a poor outcome 13–15, 18, were treated at our institution rather than having thrombolys is with held. On the other hand we did not routinely obtain vascular imaging in the emergency department, so the presence of a vascular occlusion is unlikely to be an explanation for more aggressive treatment. The definition of TGT is also variable across the studies, though an NIHSS ≤5 or treating physician judgment are the most commonly used definitions. Many of the previous studies were retrospective reviews of all patients and no prospective trial data exists as of yet.
Our study has some potential limitations. First, we could not follow most of the patients out to three-months and it is possible that our patients had a worse outcome at 90 days. We used discharge outcomes, which have been used by other investigators to indicate that TGT patients have poor outcomes14–16, and feel that our results are comparable from that perspective. Though a patient may have an improvement in the NIHSS, their functional status at 90 days may be unchanged. However, given that we observed very good early outcomes, we would expect that in the longer term our outcomes would be even more favorable in the TGT group. The latter is supported by a recent report including discharge and 90 day outcomes, which showed that the proportions of patients discharged to home was lower than the proportion with a mRS 0–2 at 90 days. Second, in our database we were not able to capture fluctuations in neurological deficits in the emergency room, or the presence of arterial occlusions on neuro-imaging, which have been associated with poorer outcomes within the TGT cohort in other studies, and therefore we could not describe these possible factors that have been reported to predict worsening within the TGT group. We included those who were ultimately diagnosed as TIA (i.e. symptoms completely resolved within 24 h), which had been previously excluded from prior reports13–16, which may have made our outcomes more benign. On the other hand we included these patients, as the stroke neurologist in the emergency room may not know at the time of treatment whether the patient would ultimately improve. In one prior report indicating good outcomes in patients who were TGT, the exclusion of patients with TIA was not mentioned17. During the period of study vascular imaging was rarely obtained in acute stroke patients prior to a decision about IV tPA, and as such we do not believe that the decision on whether to treat was influenced by this variable. Third, there could be a selection bias whereby the patients with mild stroke who were in fact treated were also the ones likely to have a poor outcome. In our database we only captured total scores in the NIHSS, and could therefore not categorize patients by their neurological syndrome, or presence of clinical characteristics relatively under-represented by the NIHSS such as hemi-neglect and aphasia, gait disturbance or isolated hand paresis. Some deficits may significantly affect a patient’s quality of life and employment, and they may have led the clinician to push ahead with treatment despite the low NIHSS. For example, a clinician may be more likely to thrombolyse an English teacher presenting with isolated aphasia than a retired engineer with left hemisensory loss.
The consequence of treating patients with mild deficits has also been examined extensively in the literature. Prior reports suggest an acceptable safety profile in these patients. A single center clinical observation study in 19 patients who were categorized as TGT but received IV tPA anyway indicated that none had clinical worsening or hemorrhage 19. Another group found that among 32 patients with mild stroke treated with IV tPA, 94% had a favorable outcome, as measured by an mRS 0–1 at three-months, with one asymptomatic hemorrhage and no symptomatic hemorrhages20. The safety of IV tPA in stroke mimics has been similarly established.21
Given how common TGT is as a reason for not administering IV tPA, and that outcomes among these patients are still in question, further studies are warranted. We would argue that early neurological worsening should be considered in any of these studies. Furthermore, this measure is not confounded by prior neurological deficits. How these patients should be treated may ultimately be answered by a randomized clinical trial across multiple populations. Such a study would need to account for patients with prior stroke and those who may ultimately be diagnosed with TIA. The data to date, including our own, cannot yet answer whether these patients should be treated. Given the heterogeneity of the impact of a mild stroke scale on functional outcomes future studies should also include other 90 day measures beyond the mRSto detect more subtle benefits. Until such trial, the decision on whether to thrombolyse TGT patients may rest on a clinical impression of how likely the patient is to be disabled by their mild neurological deficit.
Acknowledgments
This study was funded by the Specialized Program of Translational Research in Acute Stroke (SPOTRIAS) initiative at Columbia University Medical Center, NINDS P50 NS049060.
Footnotes
Conflict of interest None declared.
References
- 1.A systems approach to immediate evaluation and management of hyperacute stroke. Experience at eight centers and implications for community practice and patient care. The National Institute of Neurological Disorders and Stroke (NINDS) rt-PA Stroke Study Group. Stroke. 1997;28:1530–40. doi: 10.1161/01.str.28.8.1530. [DOI] [PubMed] [Google Scholar]
- 2.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. NEJM. 1995;333:1581–87. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 3.Albers GW, Bates VE, Clark WM, Bell R, Verro P, Hamilton SA. Intravenous tissue-type plasminogen activator for treatment of acute stroke: the Standard Treatment with Alteplase to Reverse Stroke (STARS) study. JAMA. 2000;283:1145–50. doi: 10.1001/jama.283.9.1145. [DOI] [PubMed] [Google Scholar]
- 4.Tanne D, Bates VE, Verro P, et al. Initial clinical experience with IV tissue plasminogen activator for acute ischemic stroke: a multicenter survey. The t-PA Stroke SurveyGroup. Neurol. 1999;53:424–7. doi: 10.1212/wnl.53.2.424. [DOI] [PubMed] [Google Scholar]
- 5.Schumacher HC, Bateman BT, Boden-Albala B, et al. Use of thrombolysis in acute ischemic stroke: analysis of the Nationwide Inpatient Sample 1999 to 2004. AnnEmerg Med. 2007;50:99–107. doi: 10.1016/j.annemergmed.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 6.Cocho D, Belvis R, Marti-Fabregas J, et al. Reasons for exclusion from thrombolytic therapy following acute ischemicstroke. Neurol. 2005;64:719–20. doi: 10.1212/01.WNL.0000152041.20486.2F. [DOI] [PubMed] [Google Scholar]
- 7.Bambauer KZ, Johnston SC, Bambauer DE, Zivin JA. Reasons why few patients with acute stroke receive tissue plasminogen activator. ArchNeurol. 2006;63:661–4. doi: 10.1001/archneur.63.5.661. [DOI] [PubMed] [Google Scholar]
- 8.Kleindorfer D, Kissela B, Schneider A, et al. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: a population-based study. Stroke. 2004;35:e27–9. doi: 10.1161/01.STR.0000109767.11426.17. [DOI] [PubMed] [Google Scholar]
- 9.Hills NK, Johnston SC. Why are eligible thrombolysis candidates left untreated? Am J Prev Med. 2006;31:S210–16. doi: 10.1016/j.amepre.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Kleindorfer D, Broderick J, Khoury J, et al. The unchanging incidence and case-fatality of stroke in the 1990s: a population-based study. Stroke. 2006;37:2473–8. doi: 10.1161/01.STR.0000242766.65550.92. [DOI] [PubMed] [Google Scholar]
- 11.Khatri P, Kleindorfer DO, Yeatts SD, et al. Strokes With Minor Symptoms. An Exploratory Analysis of the National Institute of Neurological Disorders and Stroke Recombinant Tissue Plasminogen Activator Trials. Stroke. 2010;41:2581–6. doi: 10.1161/STROKEAHA.110.593632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adams HP, Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 13.Nedeltchev K, Schwegler B, Haefeli T, et al. Outcome of stroke with mild or rapidly improving symptoms. Stroke. 2007;38:2531–5. doi: 10.1161/STROKEAHA.107.482554. [DOI] [PubMed] [Google Scholar]
- 14.Rajajee V, Kidwell C, Starkman S, et al. Early MRI and outcomes of untreated patients with mild or improving ischemic stroke. Neurol. 2006;67:980–4. doi: 10.1212/01.wnl.0000237520.88777.71. [DOI] [PubMed] [Google Scholar]
- 15.Smith EE, Abdullah AR, Petkovska I, Rosenthal E, Koroshetz WJ, Schwamm LH. Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke. Stroke. 2005;36:2497–9. doi: 10.1161/01.STR.0000185798.78817.f3. [DOI] [PubMed] [Google Scholar]
- 16.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurol. 2001;56:1015–20. doi: 10.1212/wnl.56.8.1015. [DOI] [PubMed] [Google Scholar]
- 17.van den Berg JS, de Jong G. Why ischemic stroke patients do not receive thrombolytic treatment: resultsfrom a general hospital. Acta Neurol Scand. 2009;120:157–60. doi: 10.1111/j.1600-0404.2008.01140.x. [DOI] [PubMed] [Google Scholar]
- 18.Fischer U, Baumgartner A, Arnold M, et al. What is a minor stroke? Stroke. 2010;41:661–6. doi: 10.1161/STROKEAHA.109.572883. [DOI] [PubMed] [Google Scholar]
- 19.Baumann CR, Baumgartner RW, Gandjour J, von Budingen HC, Siegel AM, Georgiadis D. Good outcomes in ischemic stroke patients treated with intravenous thrombolysis despite regressing neurological symptoms. Stroke. 2006;37:1332–3. doi: 10.1161/01.STR.0000217272.38455.a2. [DOI] [PubMed] [Google Scholar]
- 20.Kohrmann M, Nowe T, Huttner HB, et al. Safety and outcome after thrombolysis in stroke patients with mild symptoms. CerebrovascDis. 2009;27:160–6. doi: 10.1159/000185607. [DOI] [PubMed] [Google Scholar]
- 21.Chernyshev OY, Martin-Schild S, Albright KC, et al. Safety of tPA in stroke mimics and neuroimaging-negative cerebral ischemia. Neurol. 2010;74:1340–5. doi: 10.1212/WNL.0b013e3181dad5a6. [DOI] [PMC free article] [PubMed] [Google Scholar]