Abstract
Three cases of transient proximal small bowel angioedema induced by intravenous administration of nonionic iodinated contrast media (CM) are presented. Computed tomography (CT) images in the venous phase displayed the proximal small bowel with circumferential thickening of the wall including the duodenum and proximal segment of the jejunum. The bowel wall was normal in non-enhanced images, and normal or inconspicuous in arterial phase enhanced images. In one of the three cases, the bowel wall was thickened in venous phase but disappeared in the 40 s delayed phase images. No filling defect was seen in the lumen of the superior mesenteric artery and vein. No peritoneal effusion or mesentery abnormality was found. Each of these patients reported only mild abdominal discomfort and recovered without specific treatment within a short time. Only one patient suffered mild diarrhea after scanning which had resolved by the following day. The transient anaphylactic small bowel angioedema due to intravenous iodinated contrast media was easily diagnosed based on its characteristic CT findings and clinical symptoms. Differential diagnosis may include inflammatory and ischemic bowel disease, as well as neoplasms. A three-phase CT protocol and good understanding of this disorder are fundamentally important in the diagnosis of this condition. The supposed etiology behind the transient anaphylactic reaction to intravenous administration of iodinated CM in small bowel is similar to other CM-induced hypersensitive immediate reactions. The predilection location of transient anaphylactic bowel angioedema is the small intestine, particularly the proximal segment. A speculated cause may be the richer supply of vessels in the small intestine, ample mucous folds and loose connective tissue in the duodenum and the jejunum.
Keywords: Bowel angioedema, Bowel thickening, Computed tomography, Contrast media, Small bowel anaphylaxis
INTRODUCTION
Anaphylactic reactions to intravenous nonionic iodinated contrast media (CM) range from mild flushing to severe cardiopulmonary arrest and occur in about 1% of patients[1,2]. Such anaphylactic reactions can occur in the gastrointestinal tract presenting as bowel angioedema. To our knowledge, only four cases of small bowel angioedema and one case of colon angioedema were previously reported in the literature[3-5]. Here we report three cases of proximal small bowel angioedema and discuss their computed tomography (CT) findings, clinical features and outcomes.
CASE REPORT
Case one
A 55 year-old man with upper abdominal pain for one month was referred for an upper abdominal multi-phase contrast-enhanced CT examination. The patient drank 400 mL of iso-osmotic mannitol solution 30 min before the study and 100 mL just before the scan. After a conventional plain CT scan, a total of 90 mL nonionic iodinated CM (370 mgI/mL, Ultravist, Bayer Schering Pharma) was administered intravenously at a rate of 3 mL/s using an automated injector. The patient suffered mild abdominal discomfort during the examination and mild diarrhea after scanning. No dermal rash or other disorders were reported. These symptoms had resolved by the following day.
CT images in the venous phase displayed the proximal small bowel with circumferential thickening of the wall of a long segment (Figure 1A), including the descending, horizontal and ascending duodenum. However, the bowel wall was normal in the non-enhanced (Figure 1B) and arterial phase (Figure 1C) images. The fat around the bowel was clear. No filling defect was seen in the lumen of the superior mesenteric artery and vein. No peritoneal effusion or other abnormality was found. Therefore, the patient was clinically diagnosed with bowel angioedema, and follow-up was recommended.
Figure 1.
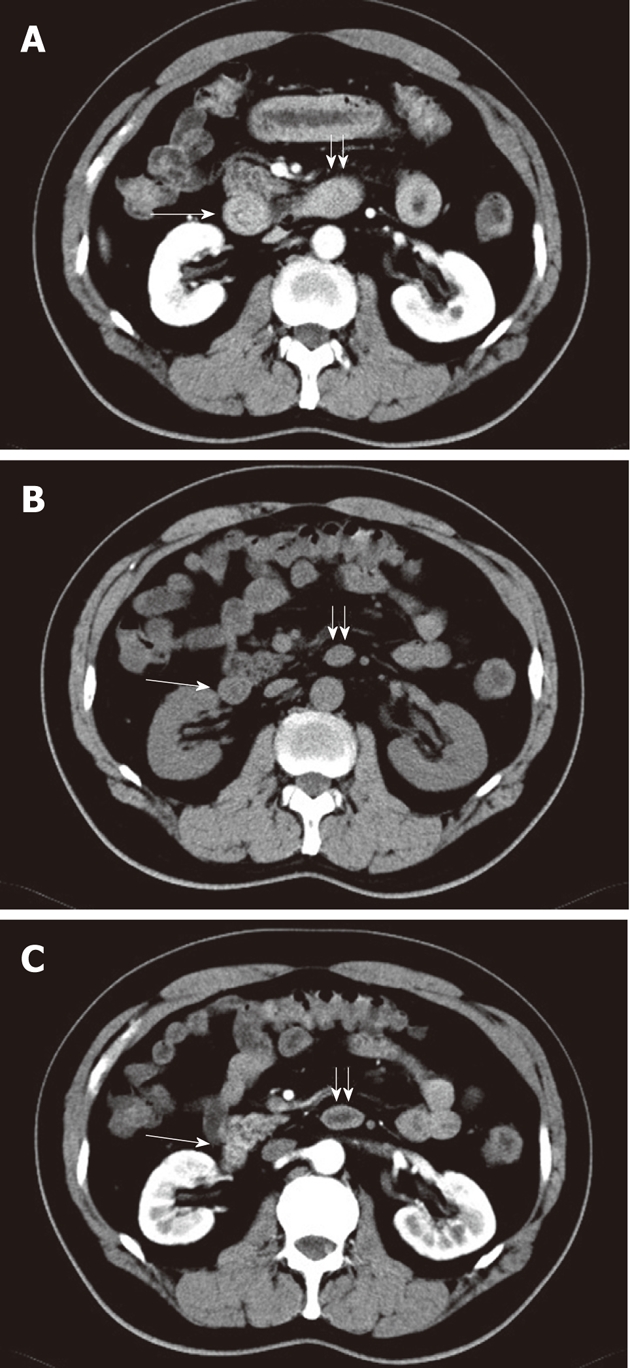
A 55-year-old man. A: Circumferential thickening of the proximal small bowel in a long segment including the descending duodenum (long arrow) and horizontal duodenum (double short arrows) in venous phase image; B and C: This bowel segment appears normal in unenhanced image (B) and arterial phase image (C).
Four months later, the patient received a repeat abdominal enhanced CT scan using another nonionic CM (370 mgI/mL, Iopamidol Injection, Bracco Diagnostics). The proximal small bowel was normal.
Case two
A 46 year-old man with multiple colon polyps was referred for a complete abdominal contrast-enhanced CT exam. Prior to the CT scan, 1000 mL oral iso-osmotic mannitol solution was administered to distend the alimentary duct within one hour. The protocol for administering iodinated CM was the same as that in the first case, however, the CM (370 mgI/mL, Iopamidol Injection, Bracco Diagnostics) was different. The patient complained of mild abdominal discomfort after the CT examination. Symptoms resolved about thirty minutes later.
In non-enhanced CT images, no abnormality in the small bowel was found. The proximal segment of the small bowel showed slight thickening in arterial phase (Figure 2A) and marked circumferential thickening in venous phase (Figure 2B) CT images. The affected segment included the descending, horizontal and ascending duodenum. However, no extraluminal, mesenteric, or peritoneal pathological process was found.
Figure 2.
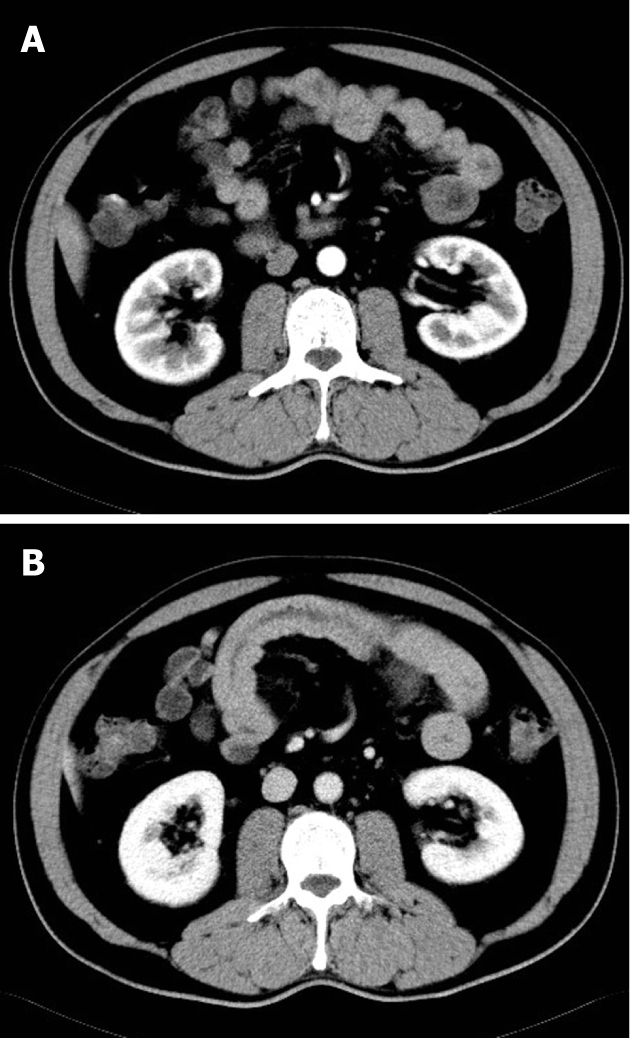
A 46-year-old man. A: The proximal bowel segment is slightly thickened in arterial phase image; B: The proximal bowel segment shows marked circumferential thickening in venous phase.
Case three
A 32-year-old woman with a mass in the right kidney was referred for a multi-phase abdominal enhanced CT exam. The examination protocol was the same as that in case one, except the CM was Omnipaque (350 mgI/mL, Iohexol Injection, GE Healthcare). An edematous proximal intestinal segment, including the second to fourth segment of the duodenum, was identified in venous phase CT images (Figure 3A). The intestinal wall was marked by circumferential thickening and the lumen was slightly dilated. Slight bowel edema was found in both arterial phase and 40-s delayed phase images (Figure 3B). However, the bowel segment was normal on the non-enhanced images (Figure 3C). Mild abdominal discomfort was the only symptom in this case and resolved spontaneously.
Figure 3.
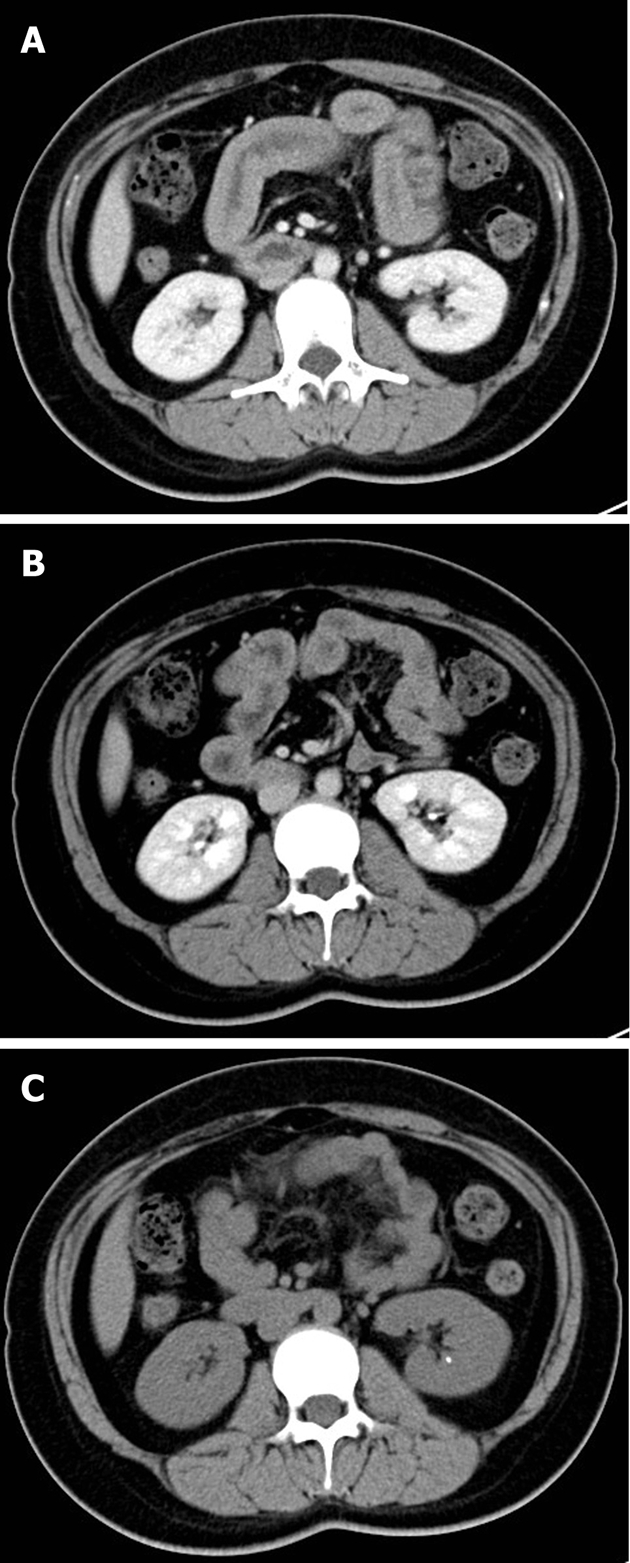
A 32-year-old woman. A: Venous phase image reveals an edematous proximal small bowel segment, including the descending and horizontal duodenum; B: The edematous wall resolved after the 40-s delayed image; C: This same bowel segment presented as normal on the unenhanced image.
DISCUSSION
Segmental bowel wall thickening is usually indicative of inflammatory bowel disease, mesenteric ischemia, or neoplastic disease. In the above-mentioned cases, thickening of the intestinal wall was most prominent on venous phase imaging. However, the bowel wall was normal in non-enhanced images and inconspicuous in arterial phase enhanced images. It is interesting that the bowel wall thickening disappeared in the 40-s delayed phase images in the third case. A rapid change in bowel wall thickening may be an exclusive characteristic of anaphylactic small intestinal angioedema due to intravenous iodinated contrast. Although bowel wall angioedema can appear slightly thickened at an initially enhanced CT and be markedly edematous 4 h later, the majority of cases in the literature revealed that circumferential wall thickening of small bowel segments was found only at initial enhanced CT images[3,4]. In our cases, peak wall thickening appeared on the venous phase about 65 s after administration of intravenous contrast. Another feature of the CT findings in our cases was that there was no exudation, vascular engorgement, or lymphadenopathy around the thickened bowel segment, which is distinguishable from other pathological processes.
All three patients felt mild abdominal discomfort during scanning with contrast enhancement, but recovered after the CT examination without special treatment. Only one patient complained of mild diarrhea on the day of examination. Such symptoms may be caused by oral administration of iso-osmotic mannitol solution before examination for distending the stomach and small intestine[6]. Our findings, in accordance with previous reports, indicate that anaphylactic angioedema of the small bowel induced by iodinated CM was self-limiting and resolved quickly without additional intervention[4].
To our knowledge, there have only been 4 cases reported in the literature with iodinated CM-induced small bowel anaphylactic angioedema. The incidence of CM-induced bowel anaphylactic angioedema is very low compared with pruritus and mild urticaria in affected patients[1]. Due to high time resolution, CM-induced bowel anaphylactic angioedema may not be well displayed in CT images before or after the venous phase, about 65 s after administration of iodinated CM. A transient wall thickening without pathological CT findings around the bowel wall and/or obvious clinical symptoms may miss the diagnosis of CM-induced bowel anaphylactic angioedema. Occasionally, it may be misdiagnosed as inflammatory or ischemic bowel disease, especially if only the venous phase protocol is used for multi-detector CT enterography[7]. Based on the above-mentioned possibilities, we presume that such a condition may be clinically underestimated.
The exact etiology of the anaphylactic reactions to intravenous administration of iodinated CM is not completely understood. In our three cases, anaphylactic angioedema of the proximal small intestine was induced by different brands of nonionic iodinated CM. In case one, the patient was hypersensitive to one type of commercial product, but not to another type. The concentration of iodinated CM we used was relative high (350 or 370 mgI/mL). However, anaphylactic small bowel angioedema can also be induced by iodinated CM at lower concentrations (300 or 282 mgI/mL) according to the literature[4,5]. Thus, the relationship between anaphylactic small bowel angioedema and the concentration of iodine in the CM was not assured. We propose that transient anaphylactic small bowel angioedema shares the same underlying etiology as the other non-allergic CM-induced hypersensitive immediate reactions[8,9]. With regard to the reason why most cases (including ours) of transient anaphylactic bowel angioedema occur in the small intestine, particularly the proximal segment, the speculated cause may be the richer supply of vessels in the small intestine than in the colon, as well as the ample mucous folds and loose connective tissue in the jejunum.
In conclusion, transient anaphylactic small bowel angioedema due to intravenous iodinated contrast media is easily diagnosed based on its characteristic CT findings. However, the three-phase CT protocol and a good understanding of this disorder are fundamentally important.
Footnotes
Peer reviewer: Arthur J Segal, Professor, Rochester General Hospital, Department of Diagnostic Imaging, 1425 Portland Ave, Rochester, NY 14621, United States
S- Editor Gou SX L- Editor Webster JR E- Editor Xiong L
References
- 1.Wang CL, Cohan RH, Ellis JH, Caoili EM, Wang G, Francis IR. Frequency, outcome, and appropriateness of treatment of nonionic iodinated contrast media reactions. Am J Roentgenol. 2008;191:409–415. doi: 10.2214/AJR.07.3421. [DOI] [PubMed] [Google Scholar]
- 2.Mortelé KJ, Oliva MR, Ondategui S, Ros PR, Silverman SG. Universal use of nonionic iodinated contrast medium for CT: evaluation of safety in a large urban teaching hospital. Am J Roentgenol. 2005;184:31–34. doi: 10.2214/ajr.184.1.01840031. [DOI] [PubMed] [Google Scholar]
- 3.Polger M, Kuhlman JE, Hansen FC 3rd, Fishman EK. Computed tomography of angioedema of small bowel due to reaction to radiographic contrast medium. J Comput Assist Tomogr. 1998;12:1044–1046. doi: 10.1097/00004728-198811000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Kim SH, Cho JY, Lim HK. CT findings of isolated small bowel angioedema due to iodinated radiographic contrast medium reaction. Abdom Imaging. 1999;24:117–119. doi: 10.1007/s002619900457. [DOI] [PubMed] [Google Scholar]
- 5.Blake SP, McNicholas MM. Hypersensitivity to intravenous contrast material causing CT appearance of bowel wall thickening. Clin Radiol. 2004;59:638–640. doi: 10.1016/j.crad.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 6.Zhang LH, Zhang SZ, Hu HJ, Gao M, Zhang M, Cao Q, Zhang QW. Multi-detector CT enterography with iso-osmotic mannitol as oral contrast for detecting small bowel disease. World J Gastroenterol. 2005;11:2324–2329. doi: 10.3748/wjg.v11.i15.2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elsayes KM, Al-Hawary MM, Jagdish J, Ganesh HS, Platt JF. CT enterography: principles, trends, and interpretation of findings. Radiographics. 2010;30:1955–1970. doi: 10.1148/rg.307105052. [DOI] [PubMed] [Google Scholar]
- 8.Brockow K, Christiansen C, Kanny G, Clément O, Barbaud A, Bircher A, Dewachter P, Guéant JL, Rodriguez Guéant RM, Mouton-Faivre C, Ring J, Romano A, Sainte-Laudy J, Demoly P, Pichler WJ, ENDA, EAACI interest group on drug hypersensitivity. Management of hypersensitivity reactions to iodinated contrast media. Allergy. 2005;60:150–158. doi: 10.1111/j.1398-9995.2005.00745.x. [DOI] [PubMed] [Google Scholar]
- 9.Trcka J, Schmidt C, Seitz CS, Bröcker EB, Gross GE, Trautmann A. Anaphylaxis to iodinated contrast material: nonallergic hypersensitivity or IgE-mediated allergy? AJR Am J Roentgenol. 2008;190:666–670. doi: 10.2214/AJR.07.2872. [DOI] [PubMed] [Google Scholar]


