Abstract
Background
Evidence for an effect of work stressors on common mental disorders (CMD) has increased over the past decade. However, studies have not considered whether the effects of work stressors on CMD remain after taking co-occurring non-work stressors into account.
Method
Data were from the 2007 Adult Psychiatric Morbidity Survey, a national population survey of participants ⩾16 years living in private households in England. This paper analyses data from employed working age participants (N=3383: 1804 males; 1579 females). ICD-10 diagnoses for depressive episode, generalized anxiety disorder, obsessive compulsive disorder, agoraphobia, social phobia, panic or mixed anxiety and depression in the past week were derived using a structured diagnostic interview. Questionnaires assessed self-reported work stressors and non-work stressors.
Results
The effects of work stressors on CMD were not explained by co-existing non-work stressors. We found independent effects of work and non-work stressors on CMD. Job stress, whether conceptualized as job strain or effort–reward imbalance, together with lower levels of social support at work, recent stressful life events, domestic violence, caring responsibilities, lower levels of non-work social support, debt and poor housing quality were all independently associated with CMD. Social support at home and debt did not influence the effect of work stressors on CMD.
Conclusions
Non-work stressors do not appear to make people more susceptible to work stressors; both contribute to CMD. Tackling workplace stress is likely to benefit employee psychological health even if the employee's home life is stressful but interventions incorporating non-work stressors may also be effective.
Keywords: Common mental disorders, life events, non-work stressors, social support, work stressors
Introduction
In the UK, the recent Black report put the prevention of illness and the promotion of well-being and health at the heart of its vision for the working population (Black, 2008). Prospective evidence for an effect of psychosocial work stress on common mental disorders (CMDs) has increased over the past decade (Stansfeld & Candy, 2006; Siegrist, 2008), with studies assessing psychosocial work stress, characterized by job strain (Karasek, 1979; Johnson & Hall, 1988) and effort–reward imbalance (ERI) (Siegrist, 1996) showing effects on anxiety and mood disorders (de Lange et al. 2003; Stansfeld & Candy, 2006; Netterstrom et al. 2008; Siegrist, 2008). Job strain and ERI are postulated to influence CMD via an imbalance between job demands and control (Karasek, 1979; Johnson & Hall, 1988) and job efforts and rewards (Siegrist, 1996), respectively. However, while associations have been established between psychosocial work stressors and CMD, other factors such as recent life events (Melchior et al. 2007), prior psychological ill health (Hammen, 2005; Clark et al. 2007a), childhood adversity (Rodgers, 1990; Clark et al. 2010), caring responsibilities (Weich et al. 2001; Pinquart & Sorensen, 2003), socioeconomic status (Lorant et al. 2003), domestic abuse (Al-Modallal et al. 2008), housing quality (Weich et al. 2002; Clark et al. 2007b), work-to-family conflict (Lennon & Rosenfield, 1992; Allen et al. 2000) and social support (Stansfeld et al. 1997b; Fuhrer et al. 1999) also show robust associations with CMD, indicating that psychological disorders have a multi-factorial causation (Hammen, 2005).
To date, only a few studies of psychosocial work stress and CMD have included non-work stressors. These studies suggest an independent effect of both work stressors and non-work stressors on depression and psychiatric sickness absence (Phelan et al. 1991; Stansfeld et al. 1997a, 1998; Weinberg & Creed, 2000; Cole et al. 2002; Griffin et al. 2002; Artazcoz et al. 2004; Wang, 2006; Melchior et al. 2007) but have poorly conceptualized and weakly measured non-work stressors, with studies tending to focus on only one type of non-work stressor. To better inform interventions for managing stress in the workplace, associations between work stressors and a range of different types of non-work stressors need exploring in general population samples. It is not known if interventions that focus solely on work stressors will be as effective in tackling CMD as interventions addressing both types of stressors.
We conducted analyses of the 2007 Adult Psychiatric Morbidity Survey (APMS) to determine the contribution of stressors in the workplace to psychological ill health compared with stressors from non-work domains in a general population sample. First, we examined the individual associations of CMD with a range of work stressors and non-work stressors (recent life events, caring responsibilities, domestic abuse, financial difficulties, poor housing quality and non-work social support). Interactions with gender were examined as the impact of stressors on CMDs differs for women and men, as do effects for non-work stressors (Kendler et al. 2001; Stansfeld & Candy, 2006; Oldehinkel & Bouma, 2010). Second, we determined the relative contribution of work stressors and non-work stressors to CMD by assessing whether any significant associations between work stressors and CMD were explained by adjustment for the non-work stressors. Finally, we examined whether non-work stressors such as social support (Phelan et al. 1991; Stansfeld et al. 1997b) and life events (Melchior et al. 2007) could also moderate effects of work stressors on CMD.
Method
Setting and participants
The 2007 APMS is a stratified probability sample survey conducted between October 2006 and December 2007 among adults aged ⩾16 years living in private households in England (McManus et al. 2009). The response rate was 57% (n=7461); 30% refused and 13% were uncontactable (McManus et al. 2009). These analyses selected working age participants (males 16–65 years, females 16–60 years, based on retirement age for each gender) who were employees and had provided complete data on all of the work and non-work stressors (N=3383: 1804 males; 1579 females). The sample included those on short-term sickness absence but excluded those on longer-term sickness absence. Employment status was self-reported.
The survey had a multi-stage, stratified random probability sampling design, using the small users Postcode Address File as a sampling frame. Approximately 14 500 addresses were selected. Interviewers visited the addresses and one eligible occupant aged ⩾16 years was randomly selected. Ethical approval for the APMS was awarded by the Royal Free Multi Regional Ethical Committee (Ref: 06/Q0501/71) (McManus et al. 2009). The survey involved a 90-min computer-assisted personal interview (CAPI), which assessed CMD, current work and non-work stressors and sociodemographic factors using standardized, validated self-report measures.
Measures
Common mental disorder
CMD was measured in the survey using a structured diagnostic interview – the Revised Clinical Interview Schedule, which assesses the prevalence of ICD-10 diagnoses of common depressive and anxiety disorders in the past 7 days (Lewis et al. 1992). CMD was defined as any diagnosis of depressive episode, generalized anxiety disorder, obsessive compulsive disorder, agoraphobia, social phobia, panic or mixed anxiety and depression.
Work stressors
ERI occurs when job efforts are high and rewards are low (Siegrist, 1996). Over-commitment, an individual's need for approval and esteem at work, can also exacerbate the effects of ERI on psychological health (Siegrist, 1996). ERI was measured using items from the ERI questionnaire (Siegrist et al. 2009) assessing the work environment in the past year. Effort was measured by three items assessing the demands of the work environment, e.g. having many interruptions and disturbances. Rewards were assessed using eight items covering job security, promotion prospects, respect and esteem. Over-commitment was assessed using six items assessing attitude to work. Reliability for these scales was good; Cronbach's α=0.79 for effort, 0.72 for reward and 0.80 for over-commitment.
The job demand-control model (JDC) (Karasek, 1979) proposes that job strain arises when high job demands are combined with low job control. The job demand-control-support model (JCDS) (Johnson & Hall, 1988) further accounts for the potential for social support at work to moderate the effect of high job demands on psychological health. JDC and JDCS were measured using questions adapted from the Whitehall II study (Karasek, 1979; North et al. 1996), assessing the work environment in the past year. Due to time constraints, demands were assessed using the questions measuring effort from the ERI model. Job control was measured using two items assessing the extent to which employees have control over their work. Social support in the workplace was assessed using four items, e.g. were colleagues willing to listen to their work-related problems? Reliability for these scales was good; Cronbach's α=0.73 for control and 0.79 for social support at work. The ERI+over-commitment model and the JDCS questions are listed in full in the Appendix.
For both the ERI and the JDC/JDCS measures scores for each individual measure (effort/demands, rewards, over-commitment, control, workplace social support) were summed and divided into tertiles – high, mid, low. As in previous papers, analyses compare the high tertile for effort/demands and over-commitment with the mid- and low tertiles and the low tertile for rewards, control and social support with the mid- and high tertiles (Stansfeld et al. 1998; de Jonge et al. 2000), The high and low tertiles for the effort and reward measures were then used to allocate respondents into four categories assessing ERI: high effort/low reward (ERI); high effort/high reward; low effort/low reward; low effort/high reward. The tertiles for demands and control were used to allocate respondents into four categories assessing job strain: high demands/low control (job strain); high demands/high control; low demands/low control; low demands/high control.
Three further work-related stressors were assessed using the list of threatening experiences (LTE) (Brugha et al. 1985) measure of life events in the past 6 months. These were being made redundant, looking for work for >1 month and experiencing violence at work.
Non-work stressors
Recent life events, caring responsibilities, non-work social support, financial strain and housing quality were assessed using CAPI. Non-work life events in the past 6 months were assessed using the LTE (Brugha et al. 1985), e.g. separation/divorce and financial difficulties.
Caring responsibilities were assessed using a dichotomous measure (no/yes) of whether the participant undertook caring responsibilities: n=584 reported caring for 0–10 h per week; n=212 reported >10 h per week. Debt was indicated by whether the household had become behind with payments for any of a range of bills and loans in the past year (Jenkins et al. 2008).
Non-work social support was assessed using the Interview Measure of Social Relationships (Brugha et al. 1987, 2003), a standardized validated measure. Scores on the items are summed and categorized as good support (score=21), mid-support (score 18–20) and low support (score <18).
Housing quality was assessed by a dichotomous measure based on whether there was mould in the respondent's home over the past year. This variable indicates poor housing quality in the UK as it is a marker of an energy-inefficient home and also indicates fuel-related poverty (Harris et al. 2010).
Domestic violence and abuse was assessed using computer-assisted self-interview to encourage full disclosure. A dichotomous variable contrasting the absence of domestic abuse with any report of domestic abuse was created from reports of whether in the past year a previous or current partner had hit them, slapped/pinned them down, threatened them with a weapon, threatened to kill them or used a weapon on them.
Sociodemographic factors
The analyses use measures of age, gender, tenure (home owned/mortgaged versus rented/other) and marital status (married; single; separated/divorced/widowed/other) (McManus et al. 2009).
Analysis
The prevalence of each work and non-work stressor for the sample and for those reporting CMD was established. Preliminary logistic regression analyses assessed associations between the individual work and non-work stressor measures and CMD, adjusted for gender, marital status, age and tenure. For job strain and ERI, subsequent adjustments were made for social support at work and over-commitment, respectively, to assess the full work stress models.
A multivariate regression model assessing the adjusted odds for CMD was then run, combining the JDCS work stressors and the non-work stressors. This model was adjusted for all the JDCS work and non-work stressors, which had been significantly associated with CMD in the preliminary regression analyses, as well as age, gender, tenure and marital status. The potential moderators of gender, non-work social support and financial difficulties were examined using multiplicative interaction terms (Zammit et al. 2010a, b). This process was repeated for a multivariable regression model combining the ERI+over-commitment work stressors and the non-work stressors.
Analyses were conducted in SPSS Version 16.0 (SPSS Inc., USA) using the complex samples analysis function taking weighting and survey design into account.
Results
Descriptives for the sample
The mean age was 38 years; 53% were male; 52% were married, 13% cohabiting, 27% single, 5% divorced and 3% widowed/separated; 16% owned their home, 57% were buying with a mortgage, 24% rented and 3% lived in the house for free.
Of the sample, 14.4% had a CMD defined as one or more of the following diagnoses: depressive episode; generalized anxiety disorder; mixed anxiety disorder; social phobia; agoraphobia; panic or obsessive compulsive disorder.
Prevalence of work stressors and associations with CMD
Nearly 12% of the sample reported job strain. Table 1 shows the associations of the JDC and the JDCS models with CMD, adjusted for gender, age, marital status and tenure. After adjustment for social support at work, job strain (high demands/low control) was associated with a three-fold increase in odds for CMD and an active job (high demands/high control) was associated with nearly double the odds. Low and mid-levels of social support at work were also significantly associated with increased odds of CMD.
Table 1.
Odds ratios showing the associations of job strain, effort–reward imbalance and work-related recent life events on common mental disorder adjusted for age, gender, tenure and marital status
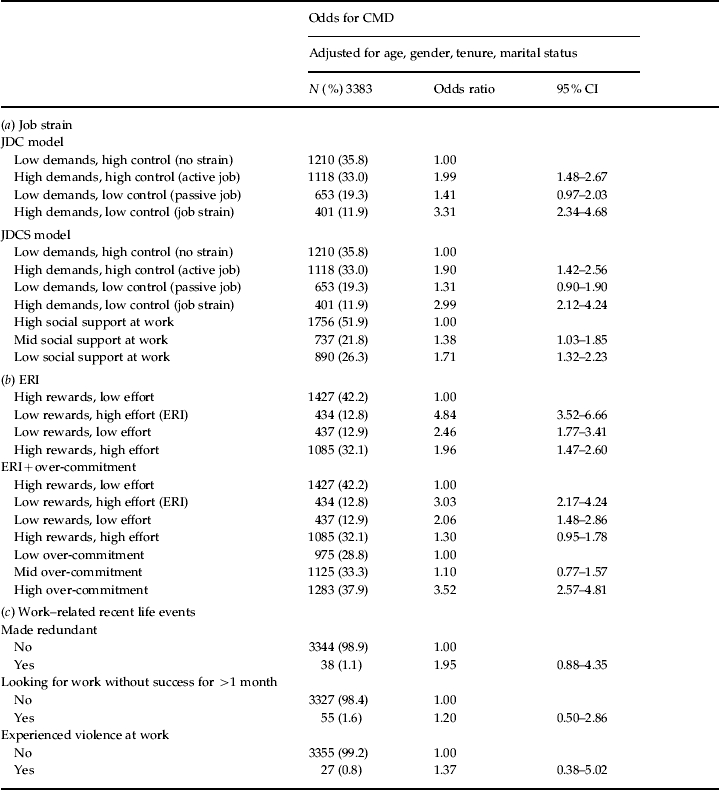
CMD, Common mental disorder; JDC, job demand-control; JDCS, job demand-control-support; ERI, effort–reward imbalance.
Nearly 13% of the sample reported ERI. Table 1 also shows the associations of the ERI and the ERI+over-commitment models with CMD adjusted for gender, age, marital status and tenure. After adjustment for over-commitment, ERI (low rewards/high effort) was associated with a three-fold increase in odds for CMD and low reward with low effort was associated with double the odds. High over-commitment was associated with a 3.5-fold increase in odds for CMD.
No significant associations were observed between the work-related life events in the past 6 months – being made redundant, looking for work without success or violence at work – and CMD. No gender interactions were observed between the work stressors and CMD, with the exception of being made redundant in the past 6 months (p=0.047). After stratification there was a significant effect of being made redundant on CMD for females [odds ratio (OR) 4.32, 95% CI 1.39–13.46] but not for males (OR 0.60, 95% CI 0.14–2.65) but these analyses were underpowered, with only 23 males and 15 females reporting redundancy in the past 6 months.
Prevalence of non-work stressors and associations with CMD
Table 2 shows the associations between the individual non-work stressors and CMD. In total, 18% of the sample reported experiencing at least one of the non-work life events in the past 6 months, which was associated with a 1.5-fold increase in odds for CMD. The serious illness/injury/assault of a close relative was associated with a 2.2-fold increase in odds for CMD, separation and divorce with nearly a 2.4-fold increase in odds, a major financial crisis with a 3.9-fold increase in odds and problems with the police with a 6.8-fold increase in odds. Domestic violence, caring responsibilities, low non-work social support, mould in the home and being in debt were also associated with increased odds for CMD (odds range=1.84–3.59).
Table 2.
Odds ratios showing the associations of non-work stressors (recent life events, caring responsibilities, domestic violence, non-work social support, housing quality and financial strain) on common mental disorder adjusted for age, gender, tenure and marital status
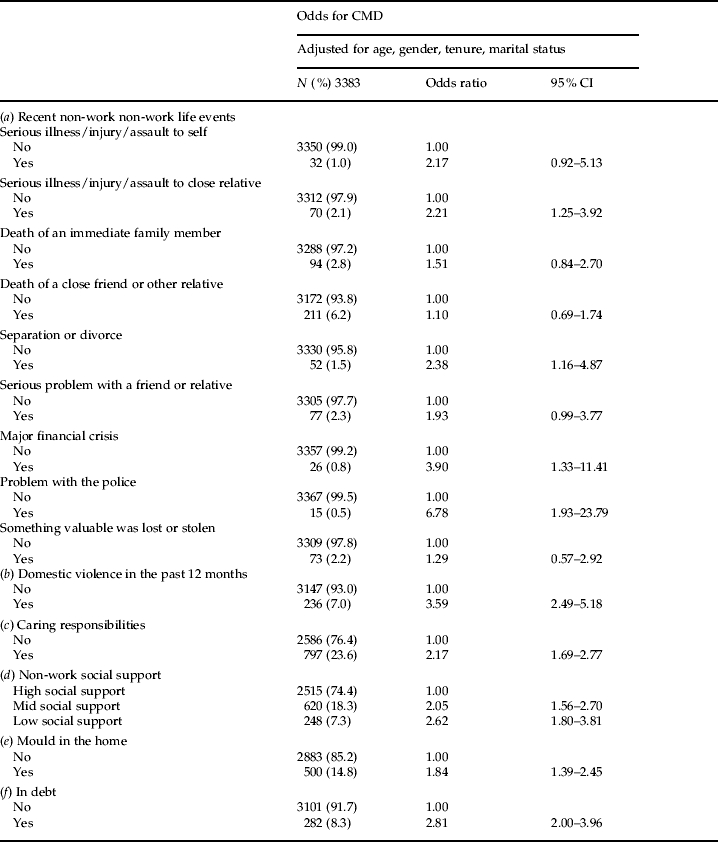
CMD, Common mental disorder.
No gender interactions were observed between the non-work stressors and CMD, with the exception of being in trouble with the police (p=0.018): due to low power, only 10 males and five females reported this life event, preventing stratification by gender to further explore this finding.
Multivariable models of work and non-work stressors
JDCS
Table 3 shows the multivariate regression model, giving the adjusted odds for CMD for the JDCS work stressor measures and the non-work stressors, adjusted for age, gender, marital status and tenure. In this fully adjusted model, both work and non-work stressors were significantly associated with CMD. Job strain remained associated with nearly a three-fold increase in odds for CMD and an active job (high demands/high control) with nearly double the odds for CMD. Low and mid-levels of social support at work also remained associated with CMD. A serious illness/injury/assault to a close relative in the past 6 months, domestic violence in the past year, caring responsibilities, low and mid-levels of non-work social support, mould in the home and debt were associated with increased odds for CMD, with odds ranging from 1.59 to 2.79.
Table 3.
Adjusted odds ratios showing associations of job-demand-control-support and non-work stressors on common mental disorder
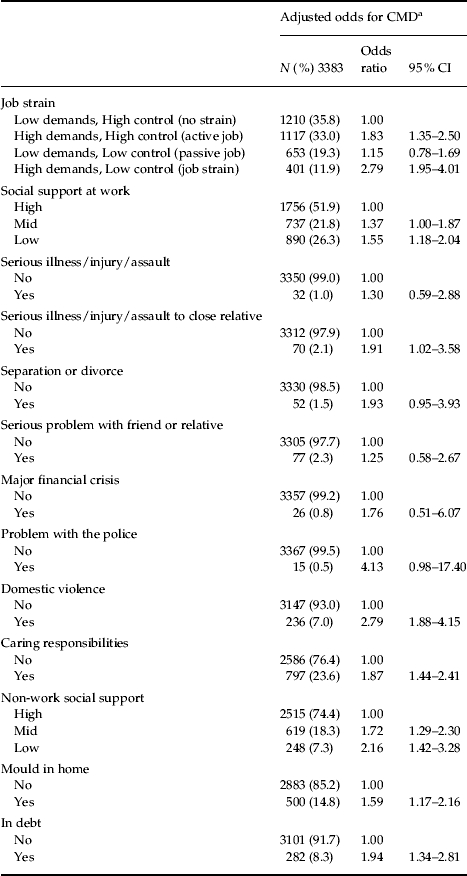
CMD, Common mental disorder.
Adjusted odds ratios are derived from a model adjusting for age, gender, tenure, marital status, job strain, social support at work, serious illness/injury/assault to self, serious illness/injury/assault to close relative, separation or divorce, serious problem with a friend or relative, major financial crisis, problem with the police, domestic violence, caring responsibilities, non-work social support, mould in the home and being in debt.
ERI model
Table 4 shows the multivariate regression model, giving the adjusted odds for CMD for the ERI+over-commitment work stressor measures and the non-work stressors, adjusted for age, gender, marital status and tenure. In this fully adjusted model, both work and non-work stressors were significantly associated with CMD. ERI (low rewards/high effort) remained associated with nearly a three-fold increase in odds for CMD and low rewards/low effort with a 1.6-fold increase in odds for CMD. High over-commitment was associated with a 3.4-fold increase in odds for CMD. A serious illness/injury/assault to a close relative in the past 6 months, domestic violence, caring responsibilities, low and mid-levels of non-work social support, mould in the home and debt also remained associated with increased odds for CMD, with odds ranging from 1.59 to 2.50.
Table 4.
Adjusted odds ratios showing associations of effort–reward imbalance+over-commitment and non-work stressors on common mental disorder
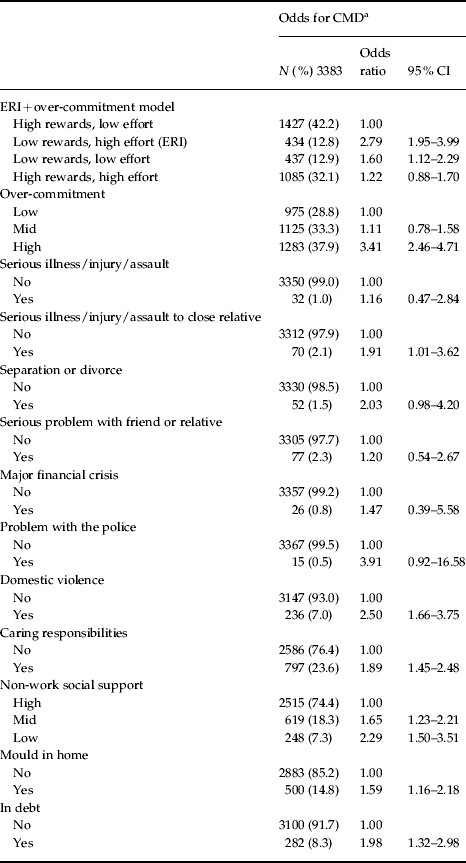
CMD, Common mental disorder; ERI, effort–reward imbalance.
Adjusted odds ratios are derived from a model adjusting for age, gender, tenure, marital status, job strain, over-commitment, serious illness/injury/assault to self, serious illness/injury/assault to close relative, separation or divorce, serious problem with a friend or relative, major financial crisis, problem with the police, domestic violence, caring responsibilities, non-work social support, mould in the home and being in debt.
Moderators of the effect of work stress on CMD
There was no significant interaction between JDC or ERI and non-work social support (p=0.435 and p=0.475). There was also no significant interaction between ERI and over-commitment (p=0.887) or between JDC or ERI and being in debt (p=0.318 and p=0.427).
Discussion
Main findings
In a representative general population sample, we found independent effects of work and non-work stressors on CMD. Job stress, whether conceptualized as job strain or ERI, together with lower levels of social support at work, recent stressful life events, domestic violence, caring responsibilities, lower levels of non-work social support, debt and poor housing quality were all independently associated with CMD. Effects of work stressors on CMD were not explained by co-existing non-work stressors. There were no gender differences in the associations observed between the stressors and CMD. Non-work social support and debt did not moderate the effect of work stressors on CMD.
Strengths and limitations
Due to the cross-sectional nature of this study, we are unable to assess causality between the work and non-work stressors and CMD. The analyses may overestimate the associations and need replicating with prospective data. Further limitations include: the reliance on self-reports of stressors and CMD; lack of examination of differential diagnoses of depression and anxiety because of the high prevalence of anxiety and/or co-morbid anxiety disorders; the possibility that poor psychological health may result in negative ratings of job characteristics (de Lange et al. 2003); a lack of assessment of personal vulnerability for psychological disorders (Weinberg & Creed, 2000); the use of the ERI model effort items to assess demands for the JDC model, which weakens the JDC model assessment; underpowered analyses for individual recent life events; the possibility that the non-work social support measure may reflect social support provided by work colleagues; lack of information about the number of roles within and outside the household; a lack of objective assessment of work characteristics and psychological health. Our sample excludes people with long-term sickness absence, which may influence the strength of associations observed. Our healthy worker sample may be more resilient than the general population.
This study is larger than the previous UK study, which sampled 64 healthcare workers (Weinberg & Creed, 2000). Other strengths include: the generalizability of the findings from this representative sample, encompassing a broad range of occupations; the assessment of an extensive range of work and non-work stressors; and measures of non-work stressors, which are not limited to life events.
Work stressors
Job strain and ERI were strongly associated with CMD even after adjustment for non-work stressors, confirming previous prospective studies (Stansfeld & Candy, 2006; Siegrist, 2008). Given the cross-sectional data, our findings may overestimate the strength of the associations. However, high job demands coupled with high job control and high efforts coupled with high demands also significantly increased the odds for CMD. High control and high rewards were not protective for psychological health, as would be predicted (Karasek, 1979; Siegrist, 1996). Previous findings could be accounted for by sampling issues, as most studies use occupational samples. However, our findings may reflect that demands and efforts are more damaging for psychological health than for physical health, irrespective of levels of control and effort. In addition, jobs may have become more demanding in recent years, leading to less of a protective effect from control and rewards. Furthermore, the meaning of control may have changed in recent years as technological advances have eroded and altered the boundaries between work and home. Further research examining the moderating effect of control and rewards on the effect of high job demands/efforts on CMD in population samples is required before firmer conclusions can be drawn.
The effect sizes for the work stressors were little attenuated after adjustment for a wide range of non-work stressors, confirming their independent effect on CMD. One exception, where the attenuation was slightly larger, was for those with low reward/low effort jobs. Non-work stressors may play a slightly greater role in the aetiology of CMD for those with low reward/low effort jobs. This could reflect differences in resources or skills to cope with exposure to stressors and potential selection into low reward/low effort jobs for individuals with social disadvantage or previous CMD (Stansfeld et al. 2008).
Our study confirms previous findings that high levels of work social support are protective of psychological health (Stansfeld et al. 1997a; Stansfeld & Candy, 2006). The current study found no association between the work-related life events of being made redundant, looking for work or violence at work and CMD, which may reflect the lack of power for these analyses, as we would expect these events to be associated with CMD (Montgomery et al. 1999). Our analyses examined individuals who experienced redundancy or unemployment but who found employment again quickly, which is likely to have had a counteracting positive effect on mental health. These associations are likely to differ in a sample including individuals who did not find employment again so quickly. Over-commitment, a measure of excessive striving, showed the strongest association with CMD in the current study and is associated with alterations in the hypothalamic-pituitary-adrenal axis system (Wirtz et al. 2010) and stress responses in the sympathetic nervous system (Wirtz et al. 2008). Over-commitment may capture elements of over-investment at work or work–life imbalance. However, over-commitment is also a measure of personality that may reflect low self-esteem; over-commitment could be influencing CMD independently of work characteristics. Over-commitment may prove to be an important aspect to be targeted in occupational interventions for psychological health and should be a focus of future research.
Non-work stressors
This study examines a broad array of non-work stressors, finding independent associations of domestic violence, caring responsibilities, mould in the home and being in debt with CMD, supporting previous findings (Weich et al. 2002; Lorant et al. 2003; Clark et al. 2007b; Al-Modallal et al. 2008). While the individual measures of recent life events were significantly associated with CMD, these associations were mediated by the other measures of work and non-work stressors. After adjustment, there remained only a significant association for serious illness/injury/assault of a close relative. In terms of implications for models of stress in the workplace, an employee with one or more of these stressors is at increased risk for poor psychological health, which could influence sickness absence.
Overall, the current survey found a lower prevalence and subsequently weaker associations between the life events and CMD than the previous APMS 2000 survey (Jordanova et al. 2007). While some of the associations between the life events with CMD were similar for the two surveys, e.g. relationship breakdown, associations for most life events were weaker and often non-significant in the APMS 2007 compared with the APMS 2000, e.g. death of a partner or close relative and problems with friends/relatives. The studies share a similar methodology and it is unclear why the findings differ over the 7-year period. The years preceding 2007 may have been beneficial for mental health in the UK but the difference could represent under-reporting of life events in the current survey. Whether similar differences in the prevalence of life events are observed over this period in other panel studies should be examined. The low prevalence for events such as financial crisis, problems with the police and separation/divorce raise the possibility of type II errors. This seems likely given that the effect sizes for these life events in the multivariate models are similar to those for other life events that reach statistical significance.
Independent effects
Our study confirms previous findings of independent effects of work and non-work stressors on CMD (Phelan et al. 1991; Griffin et al. 2002), albeit using a broader range and multiple measures of work and non-work stressors. Non-work stressors do not appear to make a person more susceptible to work-related stressors. Weinberg & Creed (2000) found independent effects of work and non-work stressors on CMD in a small UK healthcare sample, which we replicate in a representative population sample. They found that lack of management support and conflict of work role were independently associated with CMD, while using theoretically based measures, we found effects for job strain and ERI. Taken together, the evidence supports the suggestion that models of stress in the workplace need to incorporate stress outside of the workplace, together with social support (Phelan et al. 1991). Moreover, the findings suggest that it is beneficial for employers to tackle workplace stress even if the employee's home life is stressful. The independent effects of work and non-work stressors imply that, potentially, gains can be made from improving the work environment alone.
Gender
Our study confirms those that find no gender differences in the effects of psychosocial work stress on psychological health (Netterstrom et al. 2008) The contrast with studies that suggest gender differences (Artazcoz et al. 2004; Chandola et al. 2004) may reflect the occupational homogeneity of those studies compared to the current study. The independent contribution of work and non-work stressors to CMD is compatible with other studies that have concluded that gender differences in rates of CMD are not explained by the number or type of social roles occupied by men and women (Weich et al. 1998, 2001). Our findings suggest that it may not be multiple roles that are important for CMD, but the strain experienced within each domain per se.
Moderators of work stress effects on psychological health
We found no support for hypothesized effects of non-work social support, debt and over-commitment as moderators of effects of work stressors on CMD. Other studies have also failed to demonstrate interactions between life events or family stressors or non-work social support and work stressors (Griffin et al. 2002; Wang, 2006; Melchior et al. 2007). Our findings, taken together with the independent effect of non-work and work stressors on CMD, are supportive of the additive burden model (Dohrenwend & Dohrenwend, 1981), which suggests that each stressor contributes uniquely and independently to CMD.
Conclusions
In terms of the prevention of illness, interventions for managing stress in the workplace have been focused on changing job conditions, teaching people skills to help them cope with job conditions and treating those experiencing high levels of distress (Briner, 1997). However, evidence for the effectiveness of interventions to improve workers' health and reduce sickness absence is limited (BOHRF, 2005; Nieuwenhuijsen et al. 2008). It has also been suggested that the early detection of psychological disorders is important (Weinberg & Creed, 2000) and we reiterate the suggestion that existing models of work stress be developed to incorporate non-work stressors. Interventions incorporating non-work stressors may be successful, as non-work stressors can trigger sickness absence. This is of vital importance given, in recent years, the increasing likelihood because of an increase in dual-career couples and working mothers, that employees have substantial household responsibilities as well as work responsibilities (Allen et al. 2000). It would also be useful for future research to examine which factors predict sickness absence for those with CMD. The development of schemes that incorporate non-work stressors and an assessment of their effectiveness for the prevention of psychological ill health remains the next challenge. However, the findings of this study also suggest that schemes that tackle workplace stress alone may also be effective in improving employee psychological health.
Acknowledgements
The Adult Psychiatric Morbidity Survey 2007 was commissioned by The NHS Information Centre for Health and Social Care with funding from the Department of Health. This secondary analysis was funded by a grant from the Health and Safety Executive and the Department for Work & Pensions. Ethical approval for APMS 2007 was obtained from the Royal Free Hospital and Medical School Research Ethics Committee (reference number 06/Q0501/71).
Appendix
ERI+over-commitment model
Job effort
I have constant time pressures due to heavy workload.
I have many interruptions and disturbances in my job.
Over the past few years, my job has become more and more demanding.
Job rewards
I receive the respect I deserve from my line manager.
Considering all my efforts and achievements, I receive the respect and prestige I deserve from my colleagues.
Considering all my efforts and achievements, I receive the respect and prestige I deserve from my clients.
Considering all my efforts and achievements, I receive the respect and prestige I deserve from my customers.
I have experienced or expect to experience an undesirable change in my work situation.
My job security is poor.
My job promotion prospects are poor.
Considering all my efforts and achievements, my work prospects are adequate.
Over-commitment
I get easily overwhelmed by time pressures at work.
As soon as I get up in the morning I start thinking about work problems.
When I get home I can easily relax and switch off work.
People too close to me say I sacrifice too much for my job.
Work rarely lets me go, it is still on my mind when I go to bed.
If I postpone something that I was supposed to do today I'll have trouble sleeping at night.
Job demand control social support model
Job control
Do you have a choice in deciding how you go about your work?
Do you have a choice in deciding what you do at work?
Job demands
The same eight items listed under Job effort for the ERI+over-commitment model.
Social support in the workplace
Do you get help and support from your colleagues?
Are your colleagues willing to listen to your work-related problems?
Do you get help and support from your line manager?
Is your line manager willing to listen to your work-related problems?
Questions answered using a 4-point Likert scale (1=strongly agree; 2=agree; 3=disagree; 4=strongly disagree; or 1=often; 2=sometimes; 3=seldom; 4=never/almost never).
Declaration of Interest
S. M. and J. H. are employed by the National Centre for Social Research, the primary contractor for APMS 2007.
References
- Allen TD, Herst DE, Bruck CS, Sutton M. Consequences associated with work-to-family conflict: a review and agenda for future research. Journal of Occupational Health Psychology. 2000;5:278–308. doi: 10.1037//1076-8998.5.2.278. [DOI] [PubMed] [Google Scholar]
- Al-Modallal H, Peden A, Anderson D. Impact of physical abuse on adulthood depressive symptoms among women. Issues in Mental Health Nursing. 2008;29:299–314. doi: 10.1080/01612840701869791. [DOI] [PubMed] [Google Scholar]
- Artazcoz L, Artieda L, Borrell C, Cortes I, Benach J, Garcia V. Combining job and family demands and being healthy – what are the differences between men and women? European Journal of Public Health. 2004;14:43–48. doi: 10.1093/eurpub/14.1.43. [DOI] [PubMed] [Google Scholar]
- Black C. Working for a Healthier Tomorrow: Dame Carol Black's Review of the Health of Britain's Working Age Population. The Stationery Office; London: 2008. [Google Scholar]
- BOHRF. Workplace Interventions for People with Common Mental Health Problems: Evidence Review and Recommendations. British Occupational Health Research Foundation; London: 2005. [Google Scholar]
- Briner RB. Improving stress assessment: toward an evidence-based approach to organizational stress interventions. Journal of Psychosomatic Research. 1997;43:61–71. doi: 10.1016/s0022-3999(97)00010-x. [DOI] [PubMed] [Google Scholar]
- Brugha T, Bebbington P, Tennant C, Hurry J. The list of threatening experiences – a subset of 12 life event categories with considerable long-term contextual threat. Psychological Medicine. 1985;15:189–194. doi: 10.1017/s003329170002105x. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Morgan Z, Bebbington P, Jenkins R, Lewis G, Farrell M, Meltzer H. Social support networks and type of neurotic symptoms among adults in British households. Psychological Medicine. 2003;33:307–318. doi: 10.1017/s0033291702006505. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Sturt E, MacCarthy B, Potter J, Wykes T, Bebbington PE. The Interview Measure of Social Relationships: the description and evaluation of a survey instrument for assessing personal social resources. Social Psychiatry and Psychiatric Epidemiology. 1987;22:123–128. doi: 10.1007/BF00584017. [DOI] [PubMed] [Google Scholar]
- Chandola T, Martikainen P, Bartley M, Lahelma E, Marmot M, Michikazu S, Nasermoaddeli A, Kagamimori S. Does conflict between home and work explain the effect of multiple roles on mental health? A comparative study of Finland, Japan, and the UK. International Journal of Epidemiology. 2004;33:884–893. doi: 10.1093/ije/dyh155. [DOI] [PubMed] [Google Scholar]
- Clark C, Caldwell T, Power C, Stansfeld SA.. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45 year prospective epidemiologic study. Annals of Epidemiology. 2010;20:385–394. doi: 10.1016/j.annepidem.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Clark C Rodgers B Caldwell T Power C Stansfeld S 2007aChildhood and adulthood psychological ill health as predictors of midlife affective and anxiety disorders: the 1958 British Birth Cohort Archives of General Psychiatry 64668. [DOI] [PubMed] [Google Scholar]
- Clark C Stansfeld SA Candy B 2007bA systematic review on the effect of the physical environment on mental health Journal of Public Mental Health 614–27. [Google Scholar]
- Cole DC, Ibrahim S, Shannon HS, Scott FE, Eyles J. Work and life stressors and psychological distress in the Canadian working population: a structural equation modelling approach to analysis fo the 1994 National Population Health Survey. Chronic Diseases in Canada. 2002;23:2391–2399. [PubMed] [Google Scholar]
- de Jonge J, Bosma H, Peter R, Siegrist J. Job strain, effort-reward imbalance and employee wellbeing: a large-scale cross-sectional study. Social Science & Medicine. 2000;50:1317–1327. doi: 10.1016/s0277-9536(99)00388-3. [DOI] [PubMed] [Google Scholar]
- de Lange AH, Taris TW, Kompier MAJ, Houtman ILD, Bongers PM. “The very best of the millennium”: longitudinal research and the demand-control-(support) model. Journal of Occupational and Health Psychology. 2003;8:282–305. doi: 10.1037/1076-8998.8.4.282. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS, Dohrenwend BP. Dohrenwend B. S., Dohrenwend B. P. Stressful Life Events and Their Contexts. Prodist; New York: 1981. Life stress and illness: formulation of the issues; pp. 1–27. ), pp. [Google Scholar]
- Fuhrer R, Stansfeld SA, Chemali J, Shipley MJ. Gender, social relations and mental health: prospective findings from an occupational cohort (Whitehall II study) Social Science & Medicine. 1999;48:77–87. doi: 10.1016/s0277-9536(98)00290-1. [DOI] [PubMed] [Google Scholar]
- Griffin JM, Fuhrer R, Stansfeld SA, Marmot M. The importance of low control at work and home on depression and anxiety: do these effects vary by gender and social class? Social Science & Medicine. 2002;54:783–798. doi: 10.1016/s0277-9536(01)00109-5. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Harris J, Hall J, Meltzer H, Jenkins R, Oreszczyn T, McManus S. Health, mental health and housing conditions in England. National Centre for Social Research; London: 2010. [Google Scholar]
- Jenkins R, Bhugra D, Bebbington P, Brugha T, Farrell M, Coid J, Fryers T, Weich S, Singleton N, Meltzer H. Debt, income and mental disorder in the general population. Psychological Medicine. 2008;38:1485–1493. doi: 10.1017/S0033291707002516. [DOI] [PubMed] [Google Scholar]
- Johnson JV, Hall EM. Job strain, work place social support, and cardiovascular disease: a cross-sectional study of a random sample of the Swedish working population. American Journal of Public Health. 1988;78:1336–1342. doi: 10.2105/ajph.78.10.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordanova V, Stewart R, Goldberg D, Bebbington PE, Brugha T, Singleton N, Lindesay JE, Jenkins R, Prince M, Meltzer H. Age variation in life events and their relationship with common mental disorders in a national survey population. Social Psychiatry and Psychiatric Epidemiology. 2007;42:611–616. doi: 10.1007/s00127-007-0209-9. [DOI] [PubMed] [Google Scholar]
- Karasek RA. Job demands, job decision latitude, and mental strain – implications for job redesign. Administrative Science Quarterly. 1979;24:285–308. [Google Scholar]
- Kendler KS, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. American Journal of Psychiatry. 2001;158:587–593. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- Lennon MC, Rosenfield S. Women and mental-health – the interaction of job and family conditions. Journal of Health and Social Behavior. 1992;33:316–327. [PubMed] [Google Scholar]
- Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric-disorder in the community – a standardized assessment for use by lay interviewers. Psychological Medicine. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. American Journal of Epidemiology. 2003;157:98. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- McManus S, Meltzer H, Brugha T, Bebbington P, Jenkins R. Adult Psychiatric Morbidity in England 2007: Results of a Household Survey. The Health & Social Care Information Centre; Leeds: 2009. [Google Scholar]
- Melchior M, Berkman LF, Niedhammer I, Zins M, Goldberg M. The mental health effects of multiple work and family demands – a prospective study of psychiatric sickness absence in the French GAZEL study. Social Psychiatry and Psychiatric Epidemiology. 2007;42:573–582. doi: 10.1007/s00127-007-0203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery SM, Cook DG, Bartley MJ, Wadsworth MEJ. Unemployment pre-dates symptoms of depression and anxiety resulting in medical consultation in young men. International Journal of Epidemiology. 1999;28:95. doi: 10.1093/ije/28.1.95. [DOI] [PubMed] [Google Scholar]
- Netterstrom B, Conrad N, Bech P, Fink P, Olsen O, Rugulies R, Stansfeld S. The relation between work-related psychosocial factors and the development of depression. Epidemiologic Reviews. 2008;30:118–132. doi: 10.1093/epirev/mxn004. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuijsen K, Bultmann U, Neumeyer-Gromen A, Verhoeven AC, Verbeek JH, Feltz-Cornelis CM. Interventions to improve occupational health in depressed people. Cochrane Database of Systematic Reviews. 2008;16 doi: 10.1002/14651858.CD006237.pub2. , Art. No. CD006237. [DOI] [PubMed] [Google Scholar]
- North FM, Syme SL, Feeney A, Shipley M, Marmot M. Psychosocial work environment and sickness absence among British civil servants: The Whitehall II Study. American Journal of Public Health. 1996;86:332–340. doi: 10.2105/ajph.86.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldehinkel AJ, Bouma EMC. Sensitivity to depressogenic effect of stress and HPA-axis reactivity in adolescence: a review of gender differences. Neuroscience and Behavioural Review. 2010;35:1757–1770. doi: 10.1016/j.neubiorev.2010.10.013. [DOI] [PubMed] [Google Scholar]
- Phelan J, Schwartz JE, Bromet EJ, Dew MA, Parkinson DK, Schulberg HC, Dunn LO, Blane H, Curtis EC. Work stress, family stress and depression in professional and managerial employees. Psychological Medicine. 1991;21:999. doi: 10.1017/s0033291700029998. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical heatlh: a meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Rodgers B. Behaviour and personality in childhood as predictors of adult psychiatric disorder. Journal of Child Psychology and Psychiatry. 1990;31:393–414. doi: 10.1111/j.1469-7610.1990.tb01577.x. [DOI] [PubMed] [Google Scholar]
- Siegrist J. Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. European Archives of Psychiatry and Clinical Neuroscience. 2008;258:115–119. doi: 10.1007/s00406-008-5024-0. [DOI] [PubMed] [Google Scholar]
- Siegrist J, Wege N, Pühlhofer F, Wahrendorf M. A short generic measure of work stress in the era of globalization: effort-reward imbalance. International Archives of Occupational and Environmental Health. 2009;82:1005–1013. doi: 10.1007/s00420-008-0384-3. [DOI] [PubMed] [Google Scholar]
- Stansfeld S, Candy B. Psychosocial work environment and mental health – a meta-analytic review. Scandinavian Journal of Work Environment & Health. 2006;32:443–462. doi: 10.5271/sjweh.1050. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Bosma H, Hemingway H, Marmot MG. Psychosocial work characteristics and social support as predictors of SF-36 health functioning: The Whitehall II study. Psychosomatic Medicine. 1998;60:247–255. doi: 10.1097/00006842-199805000-00004. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Clark C, Caldwell T, Rodgers B, Power C. Psychosocial work characteristics and anxiety and depressive disorders in midlife: the effects of prior psychological distress. Occupational and Environmental Medicine. 2008;65:634–642. doi: 10.1136/oem.2007.036640. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA Fuhrer R Head J Ferrie J Shipley M 1997aWork and psychiatric disorder in the Whitehall II study Journal of Psychosomatic Research 4373–81. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA Rael EGS Head J Shipley M Marmot M 1997bSocial support and psychiatric sickness absence: a prospective study of British civil servants Psychological Medicine 2735–48. [DOI] [PubMed] [Google Scholar]
- Wang JL. Perceived work stress, imbalance between work and family/personal lives, and mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2006;41:541–548. doi: 10.1007/s00127-006-0058-y. [DOI] [PubMed] [Google Scholar]
- Weich S, Blanchard M, Prince M, Burton E, Erens B, Sproston K. Mental health and the built environment: cross-sectional survey of individual and contextual risk factors for depression. British Journal of Psychiatry. 2002;180:428–433. doi: 10.1192/bjp.180.5.428. [DOI] [PubMed] [Google Scholar]
- Weich S, Sloggett A, Lewis G. Social roles and gender difference in the prevalence of common mental disorders. British Journal of Psychiatry. 1998;173:489–493. doi: 10.1192/bjp.173.6.489. [DOI] [PubMed] [Google Scholar]
- Weich S, Sloggett A, Lewis G. Social roles and the gender difference in rates of the common mental disorders in Britain: a 7-year, population-based cohort study. Psychological Medicine. 2001;31:1055–1064. doi: 10.1017/s0033291701004263. [DOI] [PubMed] [Google Scholar]
- Weinberg A, Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet. 2000;355:533–537. doi: 10.1016/S0140-6736(99)07366-3. [DOI] [PubMed] [Google Scholar]
- Wirtz PH, Siegrist J, Emini L, Ehlert U. Higher overcommitment to work is associated with lower norepinephrine secretion before and after acute psychosocial stress in men. Psychoneuroendocrinology. 2008;33:92–99. doi: 10.1016/j.psyneuen.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Wirtz PH, Siegrist J, Schuhmacher A, Hoefels S, Maier W, Zobel AW.. Higher overcommitment to work is associated with higher plasma cortisol but not ACTH responses in the combined dexamethasone/CRH test in apparently healthy men and women. Psychoneuroendocrinology. 2010;35:536–543. doi: 10.1016/j.psyneuen.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Zammit S Lewis G Dalman C Allebeck P 2010aExamining interactions between risk factors for psychosis British Journal of Psychiatry 197207–211. [DOI] [PubMed] [Google Scholar]
- Zammit S Wiles N Lewis G 2010bThe study of gene environment interactions in psychiatry: limited gains at a substantial cost? Psychological Medicine 40711–716. [Google Scholar]


