Abstract
This study examines racial disparities in Child Protective Services (CPS) reporting at delivery in a county with universal screening for alcohol/drug use in prenatal care. It also explores two mechanisms through which universal screening could reduce reporting disparities: Equitable Surveillance and Effective Treatment. Equitable Surveillance is premised on the assumptions that identification of drug use through screening in prenatal care leads to CPS reporting at delivery and that Black women are screened more than White women, which leads to disproportionate reporting of Black newborns. Universal screening would correct this by ensuring that prenatal providers screen and therefore also report White women to CPS, thereby reducing disparities. Effective Treatment is premised on the idea that identification of drug use through screening in prenatal care leads women to receive treatment during pregnancy, which thereby reduces CPS reporting at delivery. Universal screening would lead to prenatal providers screening more Black women and thereby to more Black women receiving treatment prenatally. The increase in treatment receipt during pregnancy would then decrease the number of Black newborns reported to CPS at delivery, thereby reducing disparities. County data were used to compare the racial/ethnic distribution of women and newborns in three points in the system (identification in prenatal care, treatment entry during pregnancy, and reporting to CPS at delivery related to maternal alcohol/drug use) and explore pathways to treatment. Despite Black women having alcohol/drug use identified by prenatal care providers at similar rates to White women and entering treatment more than expected, Black newborns were 4 times more likely than White newborns to be reported to CPS at delivery. This contradicts the premise of Effective Treatment. By default, findings were more consistent with Equitable Surveillance than Effective Treatment. Providers and policy makers should not assume that universal screening in prenatal
Keywords: Screening, Pregnancy, Substance-related disorders, Disparities, Child Welfare
Introduction
With few exceptions, 1 there is a growing consensus that universal screening for alcohol and illicit drug use should be the standard of care in prenatal care. 2-7 However, little is known about what universal screening accomplishes either in terms of health outcomes (e.g., cessation of alcohol and/or drug use; pregnancy outcomes) or child welfare (e.g., child maltreatment; Child Protective Services (CPS) reporting). Recent systematic reviews conducted by the United States Preventive Services Task Force (USPSTF) found that research evaluating the effectiveness of universal screening during pregnancy on health outcomes was inconclusive for alcohol and did not exist for other drugs. 8,9 Studies on alcohol not included in the USPSTF review have been similarly inconclusive. 10-12 The exceptions are the few studies of Kaiser Permanente’s universal screening program, which focuses on both alcohol and drugs. These studies found improved pregnancy outcomes for women identified through universal screening who received at least one treatment visit. 3,13
No research has been published about the relationship between universal screening in prenatal care and CPS reporting at delivery. This lack of research is significant because the relationship between screening and reporting is not obvious. On one hand, universal screening in prenatal care could increase CPS reports by placing women under increased surveillance for CPS reporting at delivery. Increased surveillance was the intent of a previous prenatal drug screening program. 14,15 Because current policy requires CPS reporting for prenatal exposure to illicit drugs, 16 increased surveillance is also plausible today. On the other hand, universal screening in prenatal care could decrease CPS reports by supporting women to reduce their alcohol and/or drug use prior to delivery and therefore reduce the need for CPS reports.
Agencies and organizations promoting universal screening in prenatal care also argue that it will reduce racial disparities in CPS reporting at delivery. 17-19 Disparities are a concern as Black children are more likely than other children to be reported to CPS both in general and in relation to maternal drug use during pregnancy. 20,21 There is growing attention to prenatal alcohol and drug use among Hispanic/Latina women and concern that, in general, reports of Hispanic/Latina children to CPS are rising. 20,22-23 However, the bulk of the research and concern about racial disparities in reporting relating to alcohol and drug use during pregnancy has focused on White- Black disparities. 14,18,21,26 Yet, no published research has assessed the impact of universal screening in prenatal care on racial disparities in CPS reporting at delivery or explored the mechanisms through which universal screening in prenatal care could reduce these disparities.
Individuals and organizations suggesting that universal screening will reduce disparities rarely make explicit the logic that connects universal screening and CPS reporting disparities. Instead, they 17,19 often cite Chasnoff et al.’s Pinellas County study. 18 In the Pinellas County study, Chasnoff et al. found that while White and Black pregnant women attending their first prenatal care visit used alcohol and drugs at similar rates, Black women were 10 times more likely than White women to be reported to health authorities at delivery. Although the study was not about universal screening in prenatal care, in the discussion section, Chasnoff et al. speculate that these reporting disparities exist because prenatal care providers mostly screen, and therefore mostly identify Black women. Chasnoff et al. propose that universal screening in prenatal care will solve this reporting disparity. Their logic of how this will work is unstated, but can be reasoned as follows: Universal screening leads prenatal providers to identify more White women as alcohol and/or drug users during prenatal care; identifying more White women in prenatal care will lead providers to report more White women to CPS at delivery; reporting more White women at delivery will, therefore, reduce White-Black reporting disparities. While they do not use these terms, the authors essentially argue that screening for alcohol and drug use in prenatal care functions as surveillance for CPS reporting at delivery. The goal of universal screening, as proposed by Chasnoff et al. 18 is thus to make the surveillance for CPS reporting more equitable. Hereafter, this mechanism will be referred to as Equitable Surveillance. [See Figure 1].
Figure 1.
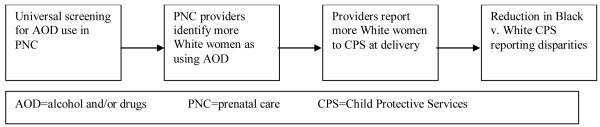
Equitable surveillance mechanism
Others have promoted universal screening as a way to provide effective treatment by identifying pregnant women who need alcohol and/or drug treatment earlier in pregnancy and then providing the needed treatment prior to delivery. 17 This second mechanism through which universal screening in prenatal care could reduce CPS reporting disparities at delivery will be referred to as Effective Treatment. The premise of Effective Treatment is that identifying pregnant women who need treatment and then providing treatment during the prenatal period will reduce CPS reporting at delivery. It is expected that this will especially benefit Black women who are assumed to not receive needed treatment. The logic can be reasoned as follows: universal screening leads prenatal care providers to identify all women who need treatment for alcohol and/or drug use; prenatal care providers will refer women to treatment during pregnancy; women who have their alcohol and/or drug use identified by a prenatal care provider through universal screening will enter treatment based on these referrals; and treatment will be effective. Following this reasoning, fewer women will be using alcohol and/or drugs at delivery; and providers therefore will report fewer women to CPS at delivery. The Effective Treatment mechanism also assumes that there are no racial differences in either treatment entry or treatment effectiveness once women are identified in prenatal care. [See Figure 2]. Importantly, some previous research does not support the idea that identification and referral by health care providers necessarily leads people to enter treatment, 1,24 thus contradicting a key assumption of the Effective Treatment mechanism: that identification in prenatal care leads women to enter treatment during pregnancy.
Figure 2.
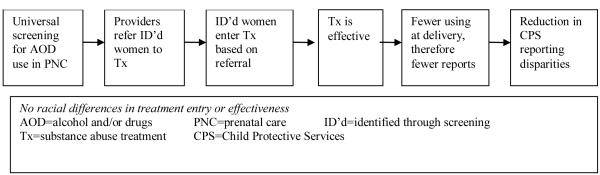
Effective treatment mechanism
Research is needed to determine whether universal screening functions as support for women, whether it functions intentionally or unintentionally as surveillance for CPS reporting, or whether it functions as both support and surveillance. This has clear implications for the ethics of prenatal screening. It also has practical implications, because the perception that identification of drug use in prenatal care leads to CPS reporting is a reason some women who use alcohol and drugs delay entry to prenatal care and skip prenatal appointments. 25 Research is also needed to understand the relationship between universal screening and CPS reporting disparities, including mechanisms underlying this relationship. Understanding these mechanisms will help determine whether screening functions as surveillance or support and provide guidance to policymakers to inform resource allocation. Studying the relationship between prenatal screening, treatment, and CPS would not be possible in a research setting, as identification of prenatal drug use in research settings is reportable only in cases of suspicion of child abuse/neglect. 27 In research settings, drug use, in and of itself, is not an indicator of child abuse/neglect. This makes this research question nearly impossible to study in research settings.
To begin exploring the relationship between universal screening in prenatal care and CPS reporting disparities at delivery, this study seeks to determine:
whether racial disparities in CPS reporting at delivery related to maternal alcohol and/or drug use are present in a county with universal screening in most public prenatal care sites and the major private prenatal care site; and
whether administrative and planning data relating to identification of alcohol and drug use in prenatal care, substance abuse treatment entry during pregnancy, and CPS reporting at delivery from the county are consistent with either the Equitable Surveillance or Effective Treatment mechanism.
Methods
Study setting
This study uses data collected for administrative, planning, and quality assurance purposes between 2001 and 2007 by government agencies in a California county located northeast of San Francisco. There are approximately one million people in the county. 28 Prenatal care providers in the county who participate in the Comprehensive Perinatal Services Program (CPSP), which serves pregnant women with Medi-Cal 29 (California’s Medicaid program), have been conducting universal screening since the early 1990s using paper screens and supplemental urine tests. 30 The main private provider site in the county also conducts universal screening. 3,13 The CPSP handbook recommends that providers offer women they identify as using alcohol and drugs health education and referrals to supportive services, including substance abuse treatment. 29
The county is racially/ethnically diverse, with a population that is 51% White, 9% Black, 22% Hispanic/Latino, and 13% Asian/Pacific Islander (API). 28 In 2006, there were 13,565 births, a birth rate of roughly 13.6 per 1000 population, slightly lower than the national average of 14.3. 31 8% of births were to White, 32% to Black, 51% to Hispanic/Latina, and 10% were to API women. 25% of births were to women with Medi-Cal. 32 Fewer than 10% of White women, approximate 33% of Black women, 50% of Hispanic/Latina women, and 10% of API women delivered with Medi-Cal. 32
Data Sources and Study Variables
This exploratory mixed methods 33 study used four non-integrated data sources to understand the system that identifies and responds to alcohol and drug use during pregnancy in the county. The components of the system examined in this study include prenatal health care, speciality substance abuse treatment, and CPS. Data sources include: 1) the Medi-Cal Perinatal Outcomes Project (MCPOP) database, 2) Alcohol and Other Drugs Services (AODS) Treatment (Treatment Entry) administrative data, 3) CPS (CPS Reporting) Administrative Data, 4) Barriers to Prenatal Care Data (B2C).
Medi-Cal Perinatal Outcomes Project (MCPOP)
De-identified data from MCPOP were extracted for all women residing in the county who had their first prenatal care visit between 2001-2003. MCPOP data were collected through medical chart abstractions conducted by health care providers at participating CPSP sites. The 2001-2003 database includes 8449 distinct pregnancies, of which 427 are second or third pregnancies of women already in the database. MCPOP data were no longer collected after 2003.
The following variables were extracted and constructed based on a larger set of variables in MCPOP. Main study variables included current drug use (any current or past month illicit drug use); current alcohol use (any current or past month alcohol use); and race/ethnicity (White, Black, Hispanic/Latina/Latin American, Asian, Pacific Islander, Native American, Other, Unknown; both Asian and Pacific Islander and Other and Unknown race/ethnicity were combined). Women with current alcohol and/or drug use were considered “identified” as alcohol and/or drugs users by prenatal care providers. To understand demographic, psychological, social, and pregnancy-related health characteristics of the study sample, the following characteristics were examined: parity (first time mothers versus all others); prenatal care utilization (broken appointments, entry after 12 weeks); insurance status at entry (Presumptive Eligibility Insurance – immediate, temporary Medi-Cal for prenatal care pending formal MediCal application - versus all other); partner status (married or living with a partner versus not); proxies for socioeconomic status - illiteracy, less than 12 years education, financial difficulties; current homelessness; partner/family violence (current and prior to past year); mental health problems (current or history of depression and psychiatric problems, suicidal ideation and suicide attempts); tobacco use and secondhand exposure; history of preterm delivery; prior demise of an infant before the infant’s first birthday; spontaneous abortion; current CPS involvement; current incarceration/probation/parole; and maternal age at entry to care. Other than maternal age, which is continuous, and race/ethnicity, which is categorical, all variables unless otherwise specified are dichotomous. In addition, a psychosocial risk scale was created using the variables described above. The scale includes eight risk categories (late/missed prenatal care; instability – Presumptive Eligibility insurance, partner status, homelessness; socioeconomic status; partner violence current; partner/family violence past; mental health problems; criminal justice/CPS involvement; previous poor pregnancy outcome) based loosely on those used by local health care providers and the local CPS agency. A score of 0–8 was created for each person based on the number of categories in which providers identified risk.
Alcohol and Other Drugs Services Treatment Entry Data (Treatment Entry)
Treatment entry data include the number of pregnant women by race/ethnicity who entered publicly-funded substance abuse treatment in the county between 2001-2003 and 2005-2007, and treatment referral source (including referrals from health care providers, CPS, self-referral, criminal justice, and other service providers) for the first treatment episode in a calendar year.
CPS Administrative Data (CPS Reporting)
CPS Reporting data include race/ethnicity of newborns (infants less than 7 days old) reported to CPS between 2005-2007, where maternal alcohol and/or drug use was noted as a factor in the report. Tracking of maternal substance use as a factor in reports was not routine prior to 2005.
Barriers to Prenatal Care (B2C) Data
B2C data consist of semi-structured interviews (n=20) and two focus groups (n=18) conducted between September–December 2006 about barriers to prenatal care for pregnant women using alcohol and drugs. 25,34 Participants were recruited from publicly-funded substance abuse treatment programs, a home visiting program, and the county Women, Infants, and Children (WIC) program. Participants consisted of a racially/ethnically diverse group of pregnant and parenting women with current alcohol and/or drug use or a history of substance abuse. The race/ethnicity distribution of participants was as follows: 42% White, 18% Black, 26% Hispanic/Latina, 3% API, and 11% mixed race. Participants were primarily polysubstance users, with methamphetamine as the most common primary substance. A little more than one half (55%) had graduated from high school or received a General Equivalency Diploma. Interview and focus group guides queried women’s thoughts about and experiences with prenatal care; barriers and facilitators to prenatal care for women who use alcohol and drugs; and what the health department and prenatal providers might do to motivate women who use alcohol and drugs to enter prenatal care earlier. More detail about study methods and participant characteristics is available in previously published studies. 25,34
Analysis
Databases were not integrated, thus multivariate analysis was not possible. To describe characteristics of the study population, two-by-two Chi-square tests and ANOVAs were used as appropriate to determine racial/ethnic differences in identification in prenatal care and in demographic, psychological, social, and pregnancy-related health characteristics of women in MCPOP. Chi-square tests used Fisher’s exact tests for small cell sizes.
To determine whether different racial/ethnic groups were over- or under-represented at different points in the system, the distributions of women by race/ethnicity at identification in prenatal care, substance abuse treatment entry during pregnancy, and CPS reporting relating to maternal alcohol and/or drug use at delivery were compared. Two-by-four Chi-square tests of homogeneity were used to compare racial/ethnic differences in the distribution of women identified as alcohol and/or drug users in prenatal care to the racial/ethnic distribution of women entering treatment and the distribution of women reported to CPS. API and Other/Native American were combined for this analysis to ensure adequate cell sizes. Among women identified as using alcohol and/or drugs through prenatal screening, there were no statistically significant differences in demographic, psychological, social, and pregnancy-related health characteristics between API and Other/Native American women, suggesting that combining the groups for analysis is appropriate. Two-by-two Chi-square tests were then used to determine whether the proportion of each racial/ethnic group in treatment was greater or less than the proportion of those identified and whether the proportion of those reported to CPS was greater or less than the proportion of those identified. To compensate for data limitations and for comparability with previous research, 18 CPS reporting disparities were also calculated by comparing the percentage of newborns by race/ethnicity reported to CPS related to maternal alcohol and/or drug use to the percentage of newborns by race/ethnicity born to all women in the county. Two-by-two Chi-square tests were used to test if reporting percentages differed from what would be expected if all newborns were equally likely to be reported.
Because of the gap between identification (2001-2003) and reporting data (2005-2007), treatment entry data from both time periods was used to check if there were any differences in the racial/ethnic distribution of treatment entry between 2001-2003 and 2005-2007. Tests of homogeneity showed that distributions did not differ between these two time periods. Thus, because identification data are from 2001-2003 and comparisons in the analysis are to identification data, 2001-2003 treatment entry data are used.
Whether women who entered treatment during pregnancy in the county entered based on a referral from a health care provider (a premise of Effective Treatment) was determined by triangulating qualitative B2C data relating to women’s pathways to treatment 35 with treatment referral source data from the AODS Treatment Entry database. Qualitative B2C data were analyzed through transcription, thematic coding, individual case studies, and typologies. 35,36
Results
Sample description
Prenatal care providers identified 6% of pregnant women in MCPOP as current alcohol and/or drug users [Table 1]. The percentage of women identified varied by race/ethnicity. More White (14%) than Hispanic/Latina (2%) and Asian/Pacific Islander (3%) women were identified as alcohol and/or drug users (p<.001). White versus Hispanic/Latina differences persisted when the comparison group of Hispanic/Latina women was restricted to women speaking English, of whom 8% were identified. There were no differences in the percentage of White and Black women identified. Prenatal providers identified fewer women as current alcohol users (1.5%) than as current drug users (5.2%), with fewer than 1% identified as using alcohol only. Compared to White women, providers identified fewer Hispanic/Latina and API women as illicit drug and as alcohol users.
Table 1.
Racial/ethnic differences in characteristics of women in MCPOP
| White (n=1590) % |
Black (n=918) % |
Hispanic/ Latina (n=5078) % |
Asian/ Pacific Islander (n=640) % |
Native American (n=40) % |
Other (n=183) % |
Total (n=8449) % |
|
|---|---|---|---|---|---|---|---|
| Alcohol and/or drug user | 14 | 14 | 2*** | 3*** | 20 | 14 | 6 |
| Illicit drugs | 12 | 13 | 2*** | 3*** | 18 | 10 | 5 |
| Alcohol | 4 | 3 | 1*** | 2** | 5 | 4 | 2 |
| Illicit drug only ° | 10 | 11 | 2 | 2 | 15 | 10 | 4 |
| Alcohol only ° | 2 | 1 | <1 | <1 | 3 | 4 | 1 |
| Illicit drugs and alcohol ° | 2 | 1 | <1 | 1 | 3 | 0 | 1 |
| First time mothers | 36 | 35 | 34 | 37 | 35 | 39 | 35 |
| Broken prenatal care appts. | 9 | 20*** | 8 | 11 | 10 | 8 | 10 |
| Prenatal care after 1st trim | 49 | 48 | 43*** | 54* | 58 | 47 | 46 |
| Presumptive eligibility ins. | 11 | 5*** | 10 | 5*** | 10 | 12 | 9 |
| Living with partner | 57 | 32*** | 74*** | 67*** | 43 | 39*** | 65 |
| Illiteracy | 1 | 2 | 4*** | 3** | 0 | 1 | 3 |
| Less than12 years education | 31 | 31 | 64*** | 22*** | 43 | 43*** | 50 |
| Financial difficulties | 37 | 33 * | 27 *** | 28 *** | 25 | 19 *** | 30 |
| Homelessness | 6 | 6 | 1*** | 1*** | 5 | 2* | 2 |
| Partner violence, current | 10 | 9 | 5*** | 5*** | 8 | 4* | 6 |
| Fam/partner violence, past | 38 | 27*** | 18*** | 11*** | 30 | 20*** | 23 |
| Mental health problems | 36 | 30** | 20*** | 18*** | 33 | 22*** | 24 |
| Current tobacco use | 39 | 23*** | 4*** | 11*** | 20* | 23*** | 14 |
| Secondhand tobacco exp. | 23 | 17*** | 5*** | 11*** | 13 | 14** | 10 |
| History preterm delivery§ | 9 | 14** | 5*** | 6 | 8 | 5* | 7 |
| Prior infant demise§ | 3 | 7** | 3 | 4 | 0 | 1* | 4 |
| Hx spontaneous abortion | 47 | 47 | 33*** | 39*** | 45 | 48 | 38 |
| Current probation/parole | 4 | 4 | <1*** | <1*** | 0 | 2 | 1 |
| Current CPS involvement§ | 4 | 2 | <1*** | 1** | 4 | 1* | 1 |
|
| |||||||
| mean | mean | mean | mean | mean | mean | mean | |
|
| |||||||
| Maternal age∞ | 26.11 | 25.02*** | 25.51*** | 27.4*** | 25.13 | 25.57*** | 25.71 |
p<.05, compared to White, by Chi-square, Fisher’s exact, and ANOVAs.
p<.01, compared to White, by Chi-square, Fisher’s exact, and ANOVAs.
p<.001, compared to White, by Chi-square, Fisher’s exact, and ANOVAs.
Maternal age only calculated for >=12 & <=50,
denominator is only non-First time mothers,
statistical tests not conducted
Overall, women in MCPOP also faced many social, psychological, and pregnancy-related health challenges [Table 1]. About half started prenatal care after their first trimester; half had neither graduated from high school nor obtained a GED; 23% had a history of family/partner violence; 24% had current or past mental health problems; 1% were involved with CPS and 1% were incarcerated or on probation or parole. Racial/ethnic groups differed in prenatal care utilization, socioeconomic status, social and psychological risk factors, and previous pregnancy outcomes. Neither White nor Black women were consistently advantaged or disadvantaged. White women appear less advantaged overall as compared to Hispanic/Latina and API women.
Women identified as using alcohol and/or drugs in MCPOP faced many additional challenges [Table 2]. Similar to all women in MCPOP, about half of those identified entered prenatal care after their first trimester and a similar percentage had neither graduated high school nor received a GED. More women who had alcohol and/or drug use identified vs. those not identified faced these additional challenges. Close to half had past partner/family violence and a similar percentage had past or current mental health problems; more than 10% were homeless; close to 10% were CPS involved; and 7% were on probation or parole. Although many of the racial/ethnic differences that existed among all women disappeared among identified women, some differences remained. Hispanic/Latina women were slightly younger, had lower tobacco use and exposure, and had less education. Fewer White than Black women had a history of broken appointments and more White than Black women lived with a partner, entered prenatal care with Presumptive Eligibility insurance, and used tobacco. Two new differences emerged among identified women. A higher proportion of White women had a history of spontaneous abortion and were first time mothers compared to Black women. Fewer API/Other women had financial difficulties, past family/partner violence, mental health problems, or tobacco use. There were no racial/ethnic differences in the number of categories of risk women faced (data not shown).
Table 2.
Racial/ethnic differences in background characteristics of women identified as alcohol and/or drug users in MCPOP
| White n=226 % |
Black n=125 % |
Hispanic/Latina n=104 % |
Asian/Pacific Islander/Other n=53 % |
Total identified n=508 % |
|
|---|---|---|---|---|---|
| First time mothers | 36 | 24* | 32 | 28 | 32 |
| Broken prenatal care appointments. |
15 | 36*** | 11 | 6 | 18 |
| Prenatal care after first trim | 52 | 62 | 43 | 43 | 52 |
| Presumptive eligibility ins. | 23 | 8*** | 13* | 30 | 18 |
| Homelessness | 11 | 18 | 8 | 2* | 11 |
| Illiteracy | 1 | 3 | 2 | 0 | 2 |
| Less than12 years education | 51 | 48 | 63 | 64 | 54 |
| Financial difficulties | 46 | 49 | 37 | 21** | 42 |
| Living with partner | 48 | 30** | 41 | 57 | 43 |
| Partner violence, current | 15 | 20 | 13 | 13 | 16 |
| Fam/partner violence, past | 52 | 43 | 46 | 21*** | 45 |
| Mental health problems | 53 | 43 | 45 | 38* | 47 |
| Current tobacco use | 69 | 54** | 42*** | 53* | 58 |
| Secondhand tobacco exp. | 39 | 30 | 26* | 26 | 33 |
| History preterm delivery§ | 8 | 15 | 6 | 5 | 9 |
| Prior infant demise§ | 2 | 5 | 4 | 0 | 3 |
| History spontaneous abortion | 55 | 43* | 57 | 55 | 53 |
| Current probation/parole | 7 | 10 | 6 | 4 | 7 |
| Current CPS involvement§ | 11 | 8 | 7 | 3 | 9 |
|
| |||||
| mean | mean | mean | mean | mean | |
|
| |||||
| Maternal age∞ | 26.09 | 25.11 | 24.23* | 23.96* | 25.25 |
p<.05, compared to White, by Chi-square, Fisher’s exact, or ANOVA.
p<.01, compared to White, by Chi-square, Fisher’s exact, or ANOVA.
p<.001, compared to White, by Chi-square, Fisher’s exact, or ANOVA.
Maternal age only calculated for >=12 & <=50
denominator is only non-First time mothers
Comparison of racial/ethnic distributions of being identified, entering treatment, and reporting to CPS
Hispanic/Latina women comprise 20% of women identified as alcohol and/or drug users in MCPOP. Forty-four percent of identified women were White, 25% were Black, and 10% were Asian/Pacific Islander and Other race/ethnicity [Table 3, column 1]. Although prenatal providers identify a smaller percentage of Hispanic/Latina women as using alcohol and/or drugs, Hispanic/Latina women comprise a large percentage of identified because they comprise a large percentage of women giving birth in the county. Of women entering treatment during pregnancy, 52% were White, 33% were Black, 9% were Hispanic/Latina, and 6% were Asian/Pacific Islander and Other race/ethnicity [column 2]. This distribution differs from the distribution expected based on the percent of women identified as alcohol and/or drug users in prenatal care [column 1] (p<.001). White and Black women make up larger proportions of those entering treatment during pregnancy compared to those identified in prenatal care (52% v. 44%; p<.05 for White women; 33% v. 25%, p<.01 for Black women; significance tests not shown in Table). Hispanic/Latina and API/Other race/ethnicity women make up smaller proportions of those entering treatment than those identified (9% v. 20%, p<.001 for Hispanic/Latina women’ 3% v. 6%, p<.05 for API/Other race/ethnicity; significance tests not shown in Table).
Table 3.
Distributions of prenatal care visits, identified AOD use, treatment entry during pregnancy, and CPS reporting
| Column 1 | Column 2 | Column 3 | |
|---|---|---|---|
| Pregnant women identified as AOD users in MCPOP 2001-2003 n=508 % |
Pregnant women entering treatment 2001-2003 n=359 % *** |
Newborns reported to CPS related to maternal AOD use 2005-2007 n=307 % *** |
|
| White | 44 | 52 | 39 |
| Black | 25 | 33 | 40 |
| Hispanic/Latino | 20 | 9 | 11 |
| API/Other § | 10 | 6 | 9 |
includes both Native American and missing race; API and “Other” categories combined for analysis
p<.001, Two-by-four Chi-square tests of homogeneity compared to identified
Post-hoc analysis with 2X2 Chi2 tests compared the proportion of each group in columns 2 and 3 to that group in column 1
The distribution by race/ethnicity of newborns reported to CPS [Table 3, column 3] also differs from the distribution by race/ethnicity of women identified in prenatal care (p<.001). White and “Other” women make up similar proportions of those reported and identified (comparisons not statistically significant). Black women make up a larger proportion of those reported compared to those identified (p<.001). Hispanic/Latina women make up a smaller proportion of those reported than those identified (p<.001; significance test result not shown in Table).
The same pattern of disparities is present when the race/ethnicity of newborns reported to CPS related to maternal alcohol and/or drug use is compared to the race/ethnicity of all births in the county [Table 4]. Fewer than 1% of White, Hispanic/Latina, and API/Other newborns were reported, while 3.5% of Black newborns were reported, respectively. White newborns were 3.5 times and 2.5 times more likely than Hispanic/Latina and API/Other newborns to be reported (p<.001). Black newborns were 4.1 times more likely than White newborns to be reported (p<.001).
Table 4.
Percent of all newborns in the county reported to CPS related to maternal AOD use 2005-2007
| Newborns reported n (%) |
Total births n |
|
|---|---|---|
| White | 121(0.84) | 14355 |
| Black | 124 (3.46) *** | 3582 |
| Hispanic/Latino | 35 (0.24) *** | 14485 |
| Asian/Pacific Islander | 27(0.34) *** | 7771 |
p<.05, Chi-square test compared to White
p<.01, Chi-square test compared to White
p<.001, Chi-square test compared to White
Treatment referral sources
Three main pathways to treatment in the perinatal period were identified: 1) identification by prenatal care providers leads to treatment entry during pregnancy; 2) CPS removes baby at delivery and then women enter treatment; and 3) self-referral by women to correct behavior they perceive as having led to previous CPS reports.
While the theme of referral to treatment by prenatal providers was present, few women reported entering treatment during pregnancy based on a provider referral. Most entered treatment only after they delivered and were reported to CPS.
“My son was almost 3 days old when I left the hospital… I went directly to court, the… next day I went to treatment.”
Some women who entered treatment after being reported to CPS indicated they had been referred by a prenatal provider, but did not accept the referral at that time.
“My doctor actually suggested the place that I’m going to for my day care right now…If I had listened to my doctor before I had my baby, I would’ve had my baby with me now instead of not having her and having to wait until I could get into [residential treatment program for CPS involved women] before I can get her back.”
Other women reported that prenatal providers did not discuss treatment with them at all. They received referrals only after they delivered and had babies removed by CPS.
“She never once gave me a referral to any kind of programs whatsoever…all the days I went to test, and, they never once referred me to a drug program, not once gave me any kind of information, didn’t even attempt to, but she gave me a referral to quit smoking, twice, as a matter of fact. And, then, once I got into [delivery hospital] and had my baby, they wanted to take her from me. Right then and there.”
Finally, some women self-referred. A common theme among women who self-referred was previous removal of a child by CPS. They described efforts in their current pregnancy such as entering treatment and attending prenatal care as attempts to avoid being reported to CPS again and to reunify with previously removed children.
“CPS…put a lot of stress on my life [with my last child] and I’m just glad that I came into the program finally to get this drug addiction off my shoulders. I’m happy that I won’t be going through that with this baby.”
This pattern of few women entering based on referrals from health care providers is supported by AODS treatment entry data. Fewer than 10% of women in the AODS Treatment Entry database (6% in 2001-2003 and 8% in 2005-2007) entered treatment during pregnancy based on a referral from a health care provider. Many more “self-referred” (38% in 2001-2003 and 23% in 2005-2007). Some (9%) also entered based on a referral from CPS (only 2006-2007 data available for this referral source). Others entered based on referrals from criminal justice and other service providers.
Discussion
This study examined the relationship between universal screening for alcohol and/or drug use in prenatal care and racial disparities in CPS reporting. Compared to Chasnoff et al.’s study, conducted in a county without universal screening where there was a 10-fold difference in CPS reporting between Whites and Blacks, 18 data from this study show much smaller reporting disparities (approximately a 4-fold difference). It is possible that the smaller disparities are due to factors other than universal screening in prenatal care.
However, if the reduced disparities are due to universal screening in prenatal care, the study findings shed light on possible underlying mechanisms. Findings are less consistent with Effective Treatment than Equitable Surveillance. First, providers identify similar percentages of White and Black women in prenatal care and identify more White than Hispanic/Latina women. However, the racial/ethnic distribution of women entering treatment differs from the distribution of those identified in prenatal care. White and Black women enter treatment more than expected and Hispanic/Latina women enter treatment less than expected. If entering treatment during pregnancy reduces the need for CPS reports at delivery (Effective Treatment), rates of CPS reporting among White and Black women should be lower than among Hispanic/Latina women. However, this study shows that rates of CPS reporting of White newborns are lower than Black newborns and higher than Hispanic/Latina newborns. Thus, over-representation in treatment appears positively associated with over-representation in CPS reports. It is possible that the treatment that Black women receive reduces what would otherwise be an even higher CPS reporting rate. However, both administrative and qualitative data indicate that any possible reduction in CPS reporting due to treatment receipt during pregnancy is unlikely to be due to screening in prenatal care as data indicate that providers are not a main source of treatment referrals. It is possible that providers offer referrals and women do not follow up on them. Regardless, the data strongly suggest that a basic building block of Effective Treatment – that screening leads to treatment – is not in place. Additionally, the idea that effective treatment will simultaneously reduce CPS reporting and reduce CPS reporting disparities may be problematic. Research into reducing health disparities suggests that it is difficult to simultaneously improve population-level outcomes and reduce disparities at the same time. 37 Because Effective Treatment is not supported and reporting disparities are smaller in this county compared to Chasnoff et al.’s study, 18 an alternative explanation is needed. A plausible alternative is Equitable Surveillance. More research is needed to confirm this explanation.
In addition, more research is needed to explore other explanations for the persistence of racial disparities in CPS reporting. It is plausible that underlying racial/ethnic differences in psychological, social, and pregnancy-related health characteristics that may be evidence of structural racism may also be related to reporting disparities. However, data on racial/ethnic differences in these characteristics among women identified as using alcohol and/or drugs in prenatal care do not suggest that any one racial/ethnic group of alcohol and/or drug users (with the exception of API/Other race/ethnicity women) in this sample is consistently advantaged or disadvantaged. More research is needed to determine if this is the case in other racially/ethnically diverse samples of low-income women using alcohol and/or drugs during pregnancy. However, in this case, it is unlikely that underlying racial/ethnic differences in background characteristics among pregnant women who had alcohol and/or drug use identified by prenatal care providers explain the reporting disparities. Further, provider bias in reporting of women who have drug use identified may also be a factor. For example, previous research suggests that providers may report fewer White than Black women among women using drugs at delivery. 21 Some of this may reflect bias towards Black women using drugs, 21 but it also may reflect bias towards crack-cocaine use, a substance that White women use less than Black women. 38
The results should be considered in light of some limitations. First, data provide a snapshot of a complicated system and leaves out critical components, such as data on women who deliver with no prenatal care or who are seen by private providers who do not screen, both of which may contribute to CPS reporting disparities. Second, while the main private provider in the county conducts universal screening, 3,13 their identification and treatment data are not included in this study. Because White women make up a larger proportion than Black and Hispanic/Latina women of those delivering with private insurance, if the identification data from the private provider were included, White women would comprise an even larger proportion of women identified and Black women would comprise a smaller proportion than they do in the MCPOP database. The CPS reporting data would not change. Thus, the comparison of the racial distributions of identification data (including the data from the private provider) and reporting data would be expected to show an even greater over-representation of Black women among those reported to CPS than among those identified through screening in prenatal care. Third, there were demographic changes between 2001 and 2006. These changes could plausibly influence shifts between 2001-2003 and 2005-2007. The number of Hispanic/Latina women delivering increased 1.5 times, while the numbers of White and Black women delivering both decreased by 5%. Because of the similarity in shifts for White and Black women, this change is unlikely to have influenced White versus Black comparisons, which are the central findings. Finally, it is not possible to determine if the lack of women entering treatment based on a referral from a health care provider is due to providers not making referrals or women not accepting or following up on referrals. Research is needed to determine which of these is the case, as they would require different interventions. Regardless of the source of the lack of entry based on provider referrals, the study findings suggest that screening does not necessarily lead to treatment.
This study also has a number of strengths. While there are limitations to each data source, using multiple data sources to triangulate 33 findings and multiple methods to calculate CPS reporting disparities adds weight to results. The magnitude of disparities also gives credence to the key finding that universal screening alone does not eliminate reporting disparities. Additionally, while not generalizable to all forms of universal screening, this study raises important questions about the implications of conducting universal screening in real-world prenatal care settings. Also, this study demonstrates that counties can combine multiple data sources to get a basic picture of the system that identifies and responds to alcohol and drug use during pregnancy while also highlighting specific data needs that can support future data collection efforts.
Implications for behavioral health
This study suggests that it is incorrect to assume that universal screening in prenatal care leads to treatment for pregnant women providers identify as alcohol and drug users. It is also incorrect to assume that universal screening alone eliminates CPS reporting disparities. A stated goal of screening in prenatal care is to increase the likelihood that women who use alcohol and drugs receive support, including during pregnancy. If this is the goal, practitioners and policymakers need to supplement screening to ensure that women (especially Black women) who have alcohol and/or drug use identified are referred to and actually receive effective treatment as well as services to meet other co-existing challenges such as homelessness and domestic violence. Ensuring that women receive treatment and services during pregnancy is a necessary pre-condition for screening to function as support and not primarily as surveillance.
Acknowledgements
This project was supported by a March of Dimes Community Award and NIAAA Graduate Training on Alcohol Problems, T32 AA07240. This manuscript was a chapter in Sarah Roberts’ dissertation. Cheri Pies provided helpful comments on this paper.
References
- 1.USPSTF Screening for Illicit Drug Use: U.S. Preventive Services Task Force Recommendation Statement. 2008 http://www.ahrq.gov/clinic/uspstf08/druguse/drugrs.pdf.
- 2.USPSTF Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse Recommendation Statement. 2004 doi: 10.7326/0003-4819-140-7-200404060-00016. http://www.ahrq.gov/clinic/3rduspstf/alcohol/alcomisrs.pdf. [DOI] [PubMed]
- 3.Goler NC, Armstrong MA, Taillac CJ, et al. Substance abuse treatment linked with prenatal visits improves perinatal outcomes: a new standard. Journal of Perinatology. 2008;28(9):597–603. doi: 10.1038/jp.2008.70. [DOI] [PubMed] [Google Scholar]
- 4.ACOG ACOG Committee Opinion No. 422: at-risk drinking and illicit drug use: ethical issues in obstetric and gynecologic practice. Obstetrics and Gynecology. 2008;112(6):1449–1460. doi: 10.1097/AOG.0b013e318192499b. [DOI] [PubMed] [Google Scholar]
- 5.Washington State Department of Health . Substance Abuse During Pregnancy: Guidelines for Screening. Revised Edition 2008 2008. [Google Scholar]
- 6.Perinatal Substance Use: A Guide for Hospitals and Health Care Providers. Virginia Departments of Health, Social Services, and Mental Health, Mental Retardation, and Substance Abuse Services; 2007. [Google Scholar]
- 7.Littaua R, Ramstrom K, Jocson M. Local MCAH Jurisdiction Survey on Prenatal Substance Use Screening Data. Maternal, Child and Adolescent Health/Office of Family Planning Branch, California Department of Health Services; 2006. [Google Scholar]
- 8.Whitlock EP, Green CA, Polen MR. Behavioral Counseling Interventions in Primary Care to Reduce Risky/Harmful Alcohol Use. AHRQ; Portland: 2004. [PubMed] [Google Scholar]
- 9.Polen M, Whitlock E, Wisdom J, et al. Screening in Primary Care Settings for Illicit Drug Use: Staged Systematic Review for the United States Preventive Services Task Force. Agency for Healthcare Research and Quality; Rockville, MD.: 2008. AHRQ Publication No. 08-05108-EF-s. [PubMed] [Google Scholar]
- 10.Chang G, McNamara TK, Orav EJ, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstetrics and Gynecology. 2005;105(5 Pt 1):991–998. doi: 10.1097/01.AOG.0000157109.05453.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang G, Wilkins-Haug L, Berman S, et al. Brief intervention for alcohol use in pregnancy: a randomized trial. Addiction. 1999;94(10):1499–1508. doi: 10.1046/j.1360-0443.1999.941014996.x. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor MJ, Whaley SE. Brief intervention for alcohol use by pregnant women. American Journal of Public Health. 2007;97(2):252–258. doi: 10.2105/AJPH.2005.077222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Armstrong MA, Osejo V Gonzales, Lieberman L, et al. Perinatal substance abuse intervention in obstetric clinics decreases adverse neonatal outcomes. Journal of Perinatology. 2003;23(1):3–9. doi: 10.1038/sj.jp.7210847. [DOI] [PubMed] [Google Scholar]
- 14.Roberts DE. Killing the black body: race, reproduction, and the meaning of liberty. Vintage; New York: 1999. [DOI] [PubMed] [Google Scholar]
- 15.Ferguson v. City of Charleston, S.C. p. 308. 380(Unites States Court of Appeals, Fourth Circuit 2002)
- 16.U.S.C.A. 2007;42 Section 5106a. [Google Scholar]
- 17.ACOG ACOG Committee Opinion. Number 294, May 2004. At-risk drinking and illicit drug use: ethical issues in obstetric and gynecologic practice. Obstetrics and Gynecology. 2004;103(5 Pt 1):1021–1031. [PubMed] [Google Scholar]
- 18.Chasnoff IJ, Landress HJ, Barrett ME. The prevalence of illicit-drug or alcohol use during pregnancy and discrepancies in mandatory reporting in Pinellas County, Florida. New England Journal of Medicine. 1990;322(17):1202–1206. doi: 10.1056/NEJM199004263221706. [DOI] [PubMed] [Google Scholar]
- 19.Chasnoff IJ. Fetal Alcohol Spectrum Disorders Seminar for County MCAH Teams and Partners. Sacramento, CA: 2007. [Google Scholar]
- 20.Hill R. An Analysis Of Racial/Ethnic Disproportionality and Disparity at the National, State, and County Levels. Casey-CSSP Alliance for Racial Equity in Child Welfare; 2007. [Google Scholar]
- 21.Neuspiel DR, Zingman TM, Templeton VH, et al. Custody of cocaine-exposed newborns: determinants of discharge decisions. American Journal of Public Health. 1993;83(12):1726–1729. doi: 10.2105/ajph.83.12.1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chambers CD, Hughes S, Meltzer SB, et al. Alcohol consumption among low-income pregnant Latinas. Alcoholism, Clinical and Experimental Research. 2005;29(11):2022–8. doi: 10.1097/01.alc.0000187160.18672.f9. [DOI] [PubMed] [Google Scholar]
- 23.Vega WA, Kolody B, Hwang J, et al. Perinatal drug use among immigrant and native-born Latinas. Substance Use and Misuse. 1997;32(1):43–62. doi: 10.3109/10826089709027296. [DOI] [PubMed] [Google Scholar]
- 24.Weisner C, Matzger H. A prospective study of the factors influencing entry to alcohol and drug treatment. Journal of Behavioral Health Services Research. 2002;29(2):126–137. doi: 10.1007/BF02287699. [DOI] [PubMed] [Google Scholar]
- 25.Roberts SC, Nuru-Jeter A. Women’s perspectives on screening for alcohol and drug use in prenatal care. Womens Health Issues. 2010 May-Jun;20(3):193–200. doi: 10.1016/j.whi.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacMahon JR. Perinatal Substance Abuse: The impact of reporting infants to Child Protective Services. Pediatrics. 1997;100(5) doi: 10.1542/peds.100.5.e1. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen D, Smith LM, Lagasse LL, et al. Intrauterine growth of infants exposed to prenatal methamphetamine: results from the infant development, environment, and lifestyle study. The Journal of Pediatrics. 2010;157(2):337–339. doi: 10.1016/j.jpeds.2010.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Community Survey. 2006.
- 29.CDPH Comprehensive Perinatal Services Program. 2008 http://www.cdph.ca.gov/PROGRAMS/CPSP/Pages/default.aspx.
- 30.PSAP Findings from a small pilot study of health care providers in Contra Costa County. 2006.
- 31.Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary Data for 2007. National Vital Statistics Reports. 2009;57(23) [PubMed] [Google Scholar]
- 32.Demioz L. California Department of Health Services, Birth Statistical Master File, 2006. Contra Costa Health Services; 2006. Contra Costa County Births 2000-2006. [Google Scholar]
- 33.Creswell JPC, VL . Designing and Conducting Mixed Methods Research. Sage Publications; Thousand Oaks: 2007. [Google Scholar]
- 34.Roberts SC, Pies C. Complex calculations: How drug use during pregnancy becomes a barrier to prenatal care. Matern Child Health Journal. 2011;15(3):333–41. doi: 10.1007/s10995-010-0594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Sage Publications; Thousand Oaks: 1994. [Google Scholar]
- 36.Patton MQ. Qualitative Research and Evaluation Methods. Sage Publications; Thousand Oaks: 2002. [Google Scholar]
- 37.Keppel K, Bilheimer L, Gurley L. Improving population health and reducing health care disparities. Health Affairs (Millwood) 2007;26(5):1281–1292. doi: 10.1377/hlthaff.26.5.1281. [DOI] [PubMed] [Google Scholar]
- 38.Lester BM, Andreozzi L, Appiah L. Substance use during pregnancy: time for policy to catch up with research. Harm Reduction Journal. 2004 Apr 20;1(1):5. doi: 10.1186/1477-7517-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


