Abstract
Objective In view of mobile phone exposure being classified as a possible human carcinogen by the International Agency for Research on Cancer (IARC), we determined the compatibility of two recent reports of glioma risk (forming the basis of the IARC’s classification) with observed incidence trends in the United States.
Design Comparison of observed rates with projected rates of glioma incidence for 1997-2008. We estimated projected rates by combining relative risks reported in the 2010 Interphone study and a 2011 Swedish study by Hardell and colleagues with rates adjusted for age, registry, and sex; data for mobile phone use; and various latency periods.
Setting US population based data for glioma incidence in 1992-2008, from 12 registries in the Surveillance, Epidemiology, and End Results (SEER) programme (Atlanta, Detroit, Los Angeles, San Francisco, San Jose-Monterey, Seattle, rural Georgia, Connecticut, Hawaii, Iowa, New Mexico, and Utah).
Participants Data for 24 813 non-Hispanic white people diagnosed with glioma at age 18 years or older.
Results Age specific incidence rates of glioma remained generally constant in 1992-2008 (−0.02% change per year, 95% confidence interval −0.28% to 0.25%), a period coinciding with a substantial increase in mobile phone use from close to 0% to almost 100% of the US population. If phone use was associated with glioma risk, we expected glioma incidence rates to be higher than those observed, even with a latency period of 10 years and low relative risks (1.5). Based on relative risks of glioma by tumour latency and cumulative hours of phone use in the Swedish study, predicted rates should have been at least 40% higher than observed rates in 2008. However, predicted glioma rates based on the small proportion of highly exposed people in the Interphone study could be consistent with the observed data. Results remained valid if we used either non-regular users or low users of mobile phones as the baseline category, and if we constrained relative risks to be more than 1.
Conclusions Raised risks of glioma with mobile phone use, as reported by one (Swedish) study forming the basis of the IARC’s re-evaluation of mobile phone exposure, are not consistent with observed incidence trends in US population data, although the US data could be consistent with the modest excess risks in the Interphone study.
Introduction
The association between microwave radiation exposure from mobile phone use and tumour development in the brain and central nervous system has been much investigated, yet remains controversial. Although many large and well conducted studies have found little evidence to support such a link,1 2 3 4 5 a few studies have observed modest to large increases in relative risk,6 7 8 9 10 11 generally of glioma but with some reports of acoustic neuroma.9 11 Results have been generally negative for an association between phone use and risk of meningioma.12 The International Agency for Research on Cancer (IARC) has recently re-evaluated the risk of tumour development in the brain and central nervous system from mobile phone use, and rated this type of exposure as a possible human carcinogen (grade 2B).12 This declaration was based mainly on the results of two epidemiological studies: the Interphone study4 and a recent Swedish study by Hardell and colleagues.10
Temporal trends in brain tumour incidence could add valuable data to the results of analytical epidemiological studies assessing exposures that have changed over time, such as the use of mobile phones. A large study in the United States13 assessed trends in brain cancer incidence in 1973-2006, and observed general reductions in incidence rates in 1992-2006. Compared with the marked increase in ownership and use of mobile phones in the US over this same period, the reductions did not support the notion that phone use causes brain cancer. In a study of brain cancer incidence in Scandinavia in 1974-2004, researchers observed gradually rising rates that did not correspond with the substantial increase in mobile phone use in the late 1990s,14 again implying no strong association.
A study in the United Kingdom observed no changes over the period 1998-2007 in the total incidence of brain cancer overall, nor for any sex or age group.15 Although researchers saw an increasing trend in cancer of the temporal lobe, this trend had begun in the late 1970s, with no change in rate in recent years; therefore, these results were unlikely to support the carcinogenic effect of mobile phone exposure.16 A similar survey of glioma incidence rates in Swedish adults in 1970-2009 yielded no evidence of changing rates over time for various age groups.17 However, none of these studies13 14 15 17 assessed the potential effect of latency or possible variation in excess relative risk with the cumulative duration of phone use on trends in brain cancer incidence.
In this study, we compared the observed patterns for glioma incidence trends in the US in 1992-2008 with projected incidence rates for the same period based on relative risks reported by the two epidemiological studies forming the basis of the IARC Working Group classification.4 10 Our comparisons considered hypothesised latency periods, anatomical sites, and glioma grades, and we also took account of changes in mobile phone use during this period.
Methods
Data collection
We used incidence data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) programme that compiles information from a series of population based cancer registries throughout the US.18 Because incidence rates vary by race and origin, and the population composition has changed over time, we focused our analysis on non-Hispanic white people (although subsidiary analysis was conducted of other ethnic groups). Hispanicity as well as race has been recorded since 1992 among residents of the areas in the 12 SEER registries used in this analysis (Atlanta, Detroit, Los Angeles, San Francisco, San Jose-Monterey, Seattle, rural Georgia, Connecticut, Hawaii, Iowa, New Mexico, and Utah).19
Primary site and histological type of the cancers were coded according to the International Classification of Diseases, 3rd edition (ICD-3), from 1992 onwards.20 We selected all 28 850 diagnoses of brain cancer (ICD-3 topography codes C71.0-C71.9, behaviour 3, excluding brain lymphomas) in non-Hispanic white people in 1992-2008. We focused on glioma (ICD-3 morphology codes 9380-9480), but also looked at astrocytoma (9400-9421, 9424, 9440-9442),21 a subgroup of gliomas that was assessed in detail in the Swedish study, although the study did not specify their exact codes.10 Most studies of brain cancer have focused on glioma in relation to mobile phone use2 3 4 6 9 10 (web appendix, table A1). Clinically, glioma is the most common category of brain cancer, and among those with the worst prognosis. Survival at five years is less than 50% for adults, and only 2.9% for glioblastoma, the most common histological subtype.22 These survival rates fall substantially with increasing age,18 although some patients with low grade glioma have had rates approaching 60%.23
We analysed data for 27 457 cases of glioma. Since most studies of mobile phone use and glioma have concentrated on adults,2 3 4 7 10 we concentrated on the 24 813 people diagnosed with glioma at age 18 years or older (table 1). We further categorised gliomas by primary anatomical site and grade, based on the World Health Organization’s brain tumour classification.24 We considered astrocytoma separately. We also did summary cross tabulations of the numbers of glioma and the underlying population by age, sex, and SEER registry (web appendix, tables A2 and A3).
Table 1.
Numbers of malignant glioma cases and person-years at risk in study population
| Endpoint | ICD-3 topography code | ICD-3 morphology code | Number of cases |
|---|---|---|---|
| All glioma | — | 9380-9480 | 24 813 |
| Astrocytoma | — | 9400, 9401, 9410, 9411, 9420, 9421, 9424, 9440-9442 | 19 920 |
| Primary anatomical site | |||
| Temporal lobe | C71.2 | — | 5147 |
| Other specified site | C71.0, C71.1, C71.3-71.7 | — | 13 457 |
| Poorly specified site | C71.8, C71.9 | — | 6209 |
| WHO classification | |||
| Low grade | — | 9391, 9393, 9400, 9410, 9411, 9420, 9421, 9424, 9450 | 4821 |
| High grade | — | 9390, 9392, 9401, 9423, 9430, 9440-9442, 9451, 9470-9474 | 17 459 |
| Grade unspecified | — | 9380-9383, 9394, 9460, 9480 | 2533 |
| Total person-years at risk | — | — | 295 348 464 |
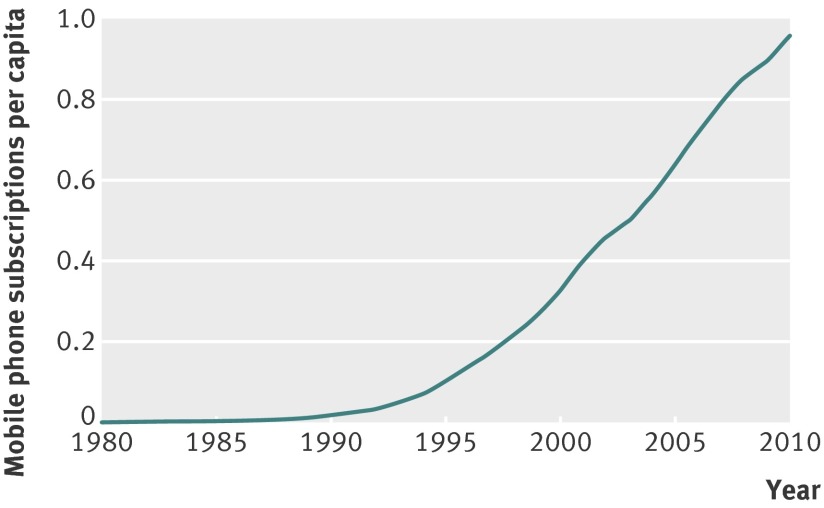
We downloaded data for mobile phone subscriptions per year in the US in 1985-2010 from the Cellular Telecommunications International Association’s website.25 Minimum latency periods of up to 10 years are thought to apply for mobile phone exposure4 10; therefore, we assessed subscriptions from 1982 onwards, for evaluation of glioma incidence from 1992 up to 2008. We estimated data for 1982-4 by log linear regression, with the assumption that the number of subscriptions per year was approximately C exp[α year] (where C and α are parameters determined by the regression). More specifically, we fitted a model via ordinary least squares to log[number of subscriptions per year], using subscriptions data for 1985-90. We estimated the number of subscriptions per capita for each year by dividing the number of subscriptions by the total US population in that year (fig 1).26
Fig 1 Mobile phone subscriptions per capita in the US, by year25
Statistical methods
Substantial mobile phone use only began in the mid-1990s (fig 1), and preliminary Poisson model fitting did not suggest that glioma rates in the 1990s varied greatly. Therefore, we fitted a model that estimated glioma rates in 1992-6 (assumed to be constant and largely independent of mobile phone use) and then in separate years from 1997 to 2008, adjusted for age group, specific SEER registry, and sex. We used model fitted rates to estimate observed rates, rather than crude rates, to avoid the introduction of errors from changes in the underlying population distribution (by age, sex, and registry). Model observed rates of glioma were estimated using men aged 60-64 years from the Los Angeles SEER registry as the baseline categories (web appendix, model A1), but the entire dataset (all ages ≥18 years, sexes, registries) was used to estimate these rates using this model. The reason for using these baseline categories is given in the web appendix. We fitted the model by Poisson maximum likelihood27 using Epicure (web appendix).28
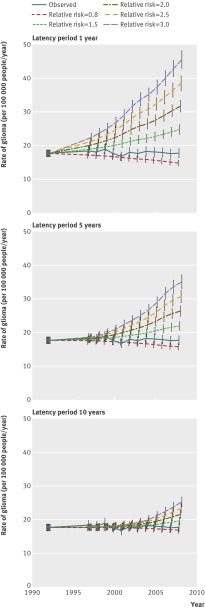
We calculated predicted risks of glioma with (ever versus never) mobile phone use in 1997-2008 by combining the estimated rates of glioma in 1992-6, the number of phone subscriptions per capita, and various assumed relative risks associated with ever using a phone and latency periods (fig 2). In figure 2, we also included a line corresponding to a relative risk of 0.8 (approximately corresponding to what was observed in the Interphone study).4
Fig 2 Observed and projected rates (95% CI) of malignant glioma in non-Hispanic white people, by latency period and various assumed levels of relative risk associated with ever using a phone
We further estimated the predicted rates by combining the number of mobile phone subscriptions with the relative risks by latency period and cumulative hours of phone use estimated in the Swedish study10 and Interphone study4 (web appendix, model A2). We assumed that the cumulative hours of phone use in the US population had the same distribution as that in the control groups in each study, as shown in tables 2-4 .
Table 2.
Relative risk of glioma (and astrocytoma) from the Swedish study10
| Latency period (years before reference date)* | Cumulative duration of mobile phone use (h) | |
|---|---|---|
| ≤74 h | >74 h | |
| 1-4 | ||
| Relative risk | 1.3 (1.3) | 1.0 (1.1) |
| Controls | 368 (368) | 203 (203) |
| 5-9 | ||
| Relative risk | 1.4 (1.5) | 1.2 (1.3) |
| Controls | 104 (104) | 182 (182) |
| ≥10 | ||
| Relative risk | 2.2 (2.7) | 2.7 (3.1) |
| Controls | 10 (10) | 96 (96) |
*The Swedish study described latency periods as “>1-5”, “>5-10”, and “>10” years. Although we used periods of 1-4, 5-9, and ≥10 years, very similar results were obtained if we interpreted periods as 2-5, 6-10, and ≥11 years (as would be possible if latency was interpreted to be an integral variable).
Table 3.
Relative risk of glioma from the Interphone study4
| Latency period (years before reference date) | Cumulative duration of mobile phone use (h) | |||||
|---|---|---|---|---|---|---|
| Never use | <5 | 5-114.9 | 115-359.9 | 360-1639.9 | ≥1640 | |
| 1-4 | ||||||
| Relative risk | 1.00 | 0.68 | 0.82 | 0.74 | 0.75 | 3.77 |
| Controls | 1078 | 182 | 533 | 154 | 95 | 8 |
| 5-9 | ||||||
| Relative risk | — | 0.86 | 0.86 | 0.71 | 0.72 | 1.28 |
| Controls | — | 13 | 208 | 192 | 204 | 73 |
| ≥10 | ||||||
| Relative risk | — | 1.13 | 0.63 | 0.89 | 0.91 | 1.34 |
| Controls | — | 2 | 25 | 42 | 90 | 73 |
Table 4.
Relative risk* of glioma from appendix 2 of the Interphone study4
| Relative risk | No of controls | |
|---|---|---|
| Time since start of regular use of mobile phone (years) | ||
| 1-1.9 | 1 | 159 |
| 2-4 | 1.68 | 451 |
| 5-9 | 1.54 | 491 |
| 10+ | 2.18 | 150 |
| Cumulative time spent on mobile phone call (h) | ||
| <5 | 1 | 114 |
| 5.0-12.9 | 0.88 | 124 |
| 13-30.9 | 1.37 | 118 |
| 31-60.9 | 1.13 | 126 |
| 61-114.9 | 1.06 | 135 |
| 115-199.9 | 1.13 | 119 |
| 200-359.9 | 1.00 | 138 |
| 360-734.9 | 1.17 | 139 |
| 735-1639.9 | 1.09 | 125 |
| 1640+ | 1.82 | 113 |
| Cumulative number of calls | ||
| <150 | 1 | 102 |
| 150-349 | 0.95 | 123 |
| 350-749 | 0.85 | 148 |
| 750-1399 | 1.19 | 111 |
| 1400-2549 | 1.10 | 134 |
| 2550-4149 | 1.19 | 124 |
| 4150-6799 | 1.02 | 122 |
| 6800-12 799 | 1.13 | 147 |
| 12 800-26 999 | 1.49 | 120 |
| 27 000+ | 1.31 | 120 |
*Relative to low use categories of mobile phone users.
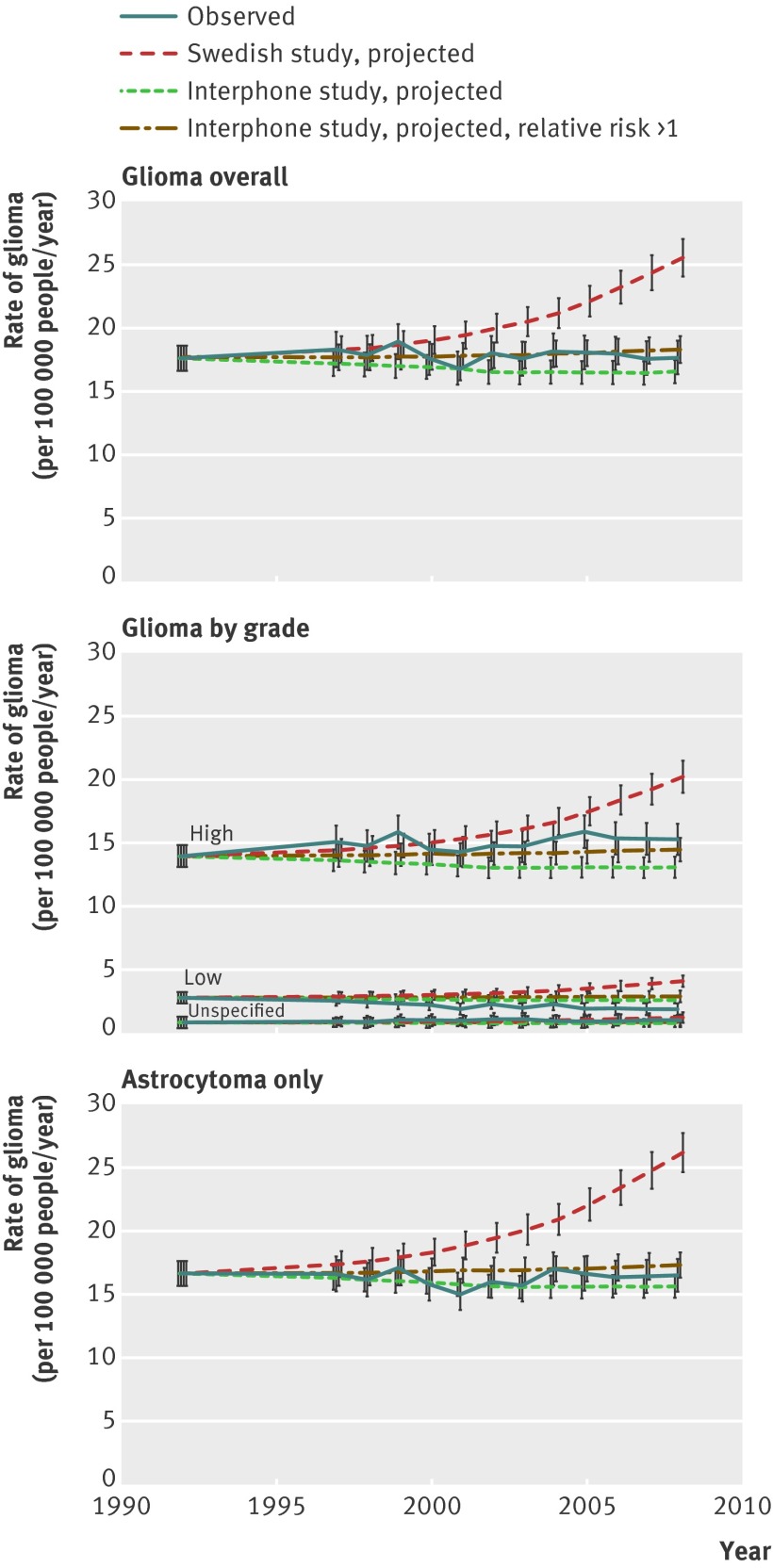
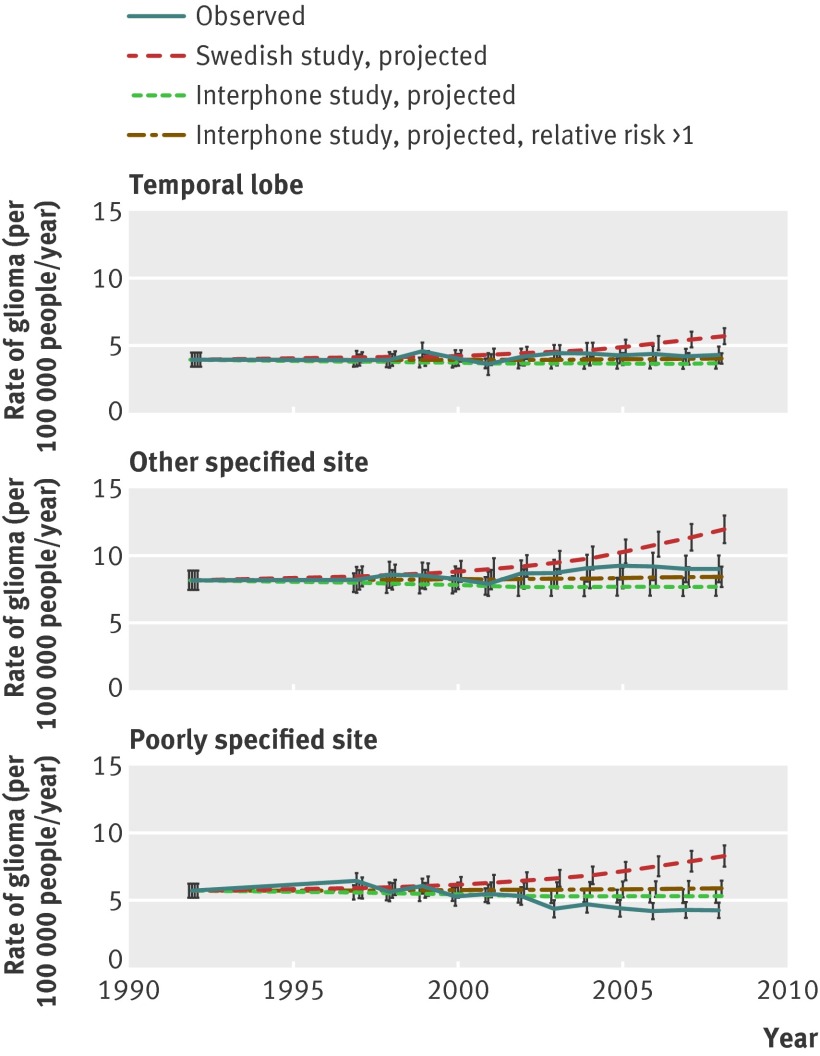
We compared these projected rates of glioma for each year from 1997 onwards, with the corresponding “observed” rates predicted by the model (that had adjusted for age, registry, and sex) (figs 3 and 4, tables 5). We also used predicted data from appendix 2 of the Interphone study4 (tables 4 and 6), which calculated risks relative to low use categories of mobile phone users (rather than the non-regular users used in the main analysis). We did this additional analysis to minimise potential bias that had been indicated by the J shaped dose-response curve in the Interphone study.4 However, when predicting the risk of US glioma incidence in table 6, we assumed that these relative risks were relative to the group of non-users of mobile phones. Because many relative risks of exposed people, compared with non-exposed people, were less than 1 in the Interphone study4 (implying an unexpected protective effect of phone use), we also estimated rates assuming that Interphone study risks were 1 or more (thus setting all relative risks less than 1 to 1), which assumes no protective effects in any category. The reporting of our study conforms to the STROBE statement29 (web appendix, table A4).
Fig 3 Observed and projected rates (95% CI) of malignant glioma in non-Hispanic white people, by histological type and WHO grade of glioma, using the relative risks, periods of latency, and cumulative hours of phone use from the Swedish study10 and Interphone study4
Fig 4 Observed and projected rates (95% CI) of malignant glioma in non-Hispanic white people, by tumour location, using the relative risks, periods of latency, and cumulative hours of phone use from the Swedish study10 and Interphone study4
Table 5.
Comparison of observed rates of glioma in non-Hispanic white people in 2008 with projected rates for 2008 based on relative risks, periods of latency, and cumulative hours of phone use from the Swedish study (table 2)10 and Interphone study (table 3)4
| Endpoint | 2008 observed rate | Swedish study | Interphone study | Interphone study, relative risk>1 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Projected 2008 rate | Difference from 2008 observed rate (%) | Projected 2008 rate | Difference from 2008 observed rate (%) | Projected 2008 rate | Difference from 2008 observed rate (%) | ||||
| All glioma | 17.7 (16.5 to 19.0) | 25.5 (24.2 to 27.0) | 44.5 | 16.5 (15.6 to 17.5) | −6.5 | 18.2 (17.3 to 19.3) | 3.2 | ||
| Astrocytoma | 16.5 (15.3 to 17.8) | 26.1 (24.7 to 27.7) | 58.3 | 15.6 (14.8 to 16.6) | −5.4 | 17.3 (16.3 to 18.3) | 4.4 | ||
| Primary anatomical site | |||||||||
| Temporal lobe | 4.3 (3.8 to 4.9) | 5.6 (5.1 to 6.3) | 30.6 | 3.7 (3.3 to 4.1) | −15.5 | 4.0 (3.6 to 4.5) | −6.8 | ||
| Other specified location | 9.0 (8.1 to 10.1) | 11.9 (10.9 to 13.0) | 31.7 | 7.7 (7.1 to 8.4) | −14.7 | 8.5 (7.8 to 9.2) | −5.9 | ||
| Poorly specified location | 4.2 (3.7 to 4.8) | 8.2 (7.5 to 9.1) | 95.2 | 5.3 (4.8 to 5.9) | 26.3 | 5.9 (5.3 to 6.5) | 39.4 | ||
| WHO classification | |||||||||
| Low grade | 1.9 (1.6 to 2.2) | 4.0 (3.6 to 4.5) | 116.2 | 2.6 (2.3 to 2.9) | 39.9 | 2.9 (2.6 to 3.2) | 54.4 | ||
| High grade | 15.2 (14.0 to 16.5) | 20.2 (18.9 to 21.4) | 32.5 | 13.0 (12.3 to 13.9) | −14.2 | 14.4 (13.5 to 15.3) | −5.4 | ||
| Grade unspecified | 1.0 (0.8 to 1.2) | 1.2 (1.1 to 1.4) | 22.7 | 0.8 (0.7 to 0.9) | −20.6 | 0.9 (0.8 to 1.0) | −12.4 | ||
Data are rate (95% confidence interval) per 100 000 people per year unless stated otherwise.
Table 6.
Projected rates of glioma for 2008, based on relative risks from appendix 2 of the Interphone study (table 4)4
| Projected rates | Interphone study, appendix 2 | Interphone study, appendix 2, relative risk>1 | ||
|---|---|---|---|---|
| Projected 2008 rate | Difference from 2008 observed rate (%)* | Projected 2008 rate | Difference from 2008 observed rate (%)* | |
| Time since start of regular use (years) | 19.5 (18.4 to 20.6) | 10.3 | 19.5 (18.4 to 20.6) | 10.3 |
| Mobile phone use (h) | ||||
| 1 year latency | 20.1 (19.0 to 21.2) | 13.4 | 20.2 (19.1 to 21.4) | 14.5 |
| 5 year latency | 19.2 (18.1 to 20.3) | 8.4 | 19.3 (18.2 to 20.4) | 9.0 |
| 10 year latency | 18.3 (17.3 to 19.4) | 3.5 | 18.4 (17.4 to 19.4) | 3.8 |
| Mobile phone calls (no) | ||||
| 1 year latency | 19.4 (18.4 to 20.6) | 9.9 | 19.8 (18.7 to 20.9) | 11.9 |
| 5 year latency | 18.8 (17.8 to 19.9) | 6.2 | 19.0 (18.0 to 20.1) | 7.4 |
| 10 year latency | 18.1 (17.2 to 19.2) | 2.6 | 18.2 (17.2 to 19.3) | 3.1 |
Data are rates (95% confidence interval) per 100 000 people per year unless stated otherwise.
*Compared with observed 2008 rate of 17.7 (16.5 to 19.0).
Results
Glioma rates were generally stable from 1992 to 2008 (figs 2-4, table 5), changing by about −0.02% per year (95% confidence interval −0.28% to 0.25%) over this period (table 7). The only marked exceptions were gliomas of low grade and those with a poorly specified anatomical location, which showed decreased rates (−3.02% per year (−3.49 to −2.54) and −2.35% per year (−2.81 to −1.89), respectively), and gliomas of the temporal lobe and other specified sites, which showed modest increases in rates (0.73% per year (0.23 to 1.23) and 0.79% per year (0.40 to 1.19), respectively) (figs 3 and 4, tables 5 and 7). However, we saw no acceleration in the rate of gliomas at the temporal lobe (P=0.279) or at other specified sites (P=0.090) before 1996 compared with after 1996 (results not shown). Equally, we saw no evidence to indicate a decrease in glioma risk by about 20% (that is, a relative risk of 0.8), which had been indicated by the Interphone study for regular users of mobile phones.
Table 7.
Trends in SEER glioma rates for non-Hispanic white people over the period 1992-2008
| Endpoint | Rate (% per year, 95% CI) |
|---|---|
| Glioma | −0.02 (−0.28 to 0.25) |
| Astrocytoma | −0.21 (−0.50 to 0.07) |
| Primary anatomical site | |
| Temporal lobe | 0.73 (0.23 to 1.23) |
| Other specified location | 0.79 (0.40 to 1.19) |
| Poorly specified location | −2.35 (−2.81 to −1.89) |
| WHO classification | |
| Low grade | −3.02 (−3.49 to −2.54) |
| High grade | 0.64 (0.33 to 0.95) |
| Grade unspecified | 1.21 (0.63 to 1.79) |
The result of assuming a true association of mobile phone use greatly increased the expected glioma rates. Even with a lag of 10 years and the smallest assumed relative risk more than 1 that was associated with ever using a phone (that is, a relative risk of 1.5), the underlying glioma rate estimated by age, registry, and sex was predicted to increase from 17.7 per 100 000 people per year (95% confidence interval 16.7 to 18.7) in 1992-6 to 19.5 per 100 000 people per year (18.5 to 20.7) in 2008, an increase of 10.7% (fig 2). With greater relative risks or shorter lag periods, this increase became much larger. In general, glioma rates were predicted to increase by at least 20% with a short latency period (≤5 years) or large relative risks (≥2.0) (fig 2).
Predicted rates were substantially more than observed rates if we applied the relative risks of the Swedish study10 to the 1992-6 baseline rates (and took account of the distribution by latency periods and cumulative phone use reported), and if we accounted for the increasing per capita prevalence of mobile phone use (figs 3-4, table 5). For example, the observed rate for glioma in 2008 was 17.7 per 100 000 people per year (95% confidence interval 16.5 to 19.0), whereas the projected rate in that year, assuming that the Swedish study’s relative risks associated with mobile phone use apply, was 44.5% higher than the observed rate (25.5 per 100 000 people per year (24.2 to 27.0)), and clearly inconsistent with it. In general, the model predicted the same or greater effects for astrocytoma only (fig 3, table 5), various grades of glioma (fig 3, table 4), and different anatomical sites (fig 4, table 5). Results were similar if we used the Swedish study’s “ever versus never use” data10 rather than the data taking account of cumulative hours of phone use (results not shown).
However, if we used the relative risks from the Interphone study,4 the expected incidence rate of glioma in 2008 changed to 16.5 per 100 000 people per year (95% confidence interval 15.6 to 17.5), compared with the observed rate of 17.7 per 100 000 people per year, or 18.2 per 100 000 people per year (95% confidence interval 17.3 to 19.3) if we restricted excess risks to be positive (that is, relative risk ≥1) (fig 3, table 5). The confidence intervals around the glioma rates implied that the observed trends were consistent with those predicted by the Interphone study; we observed the same effect if we used the relative risks taken from appendix 2 of the Interphone study4 (table 6). We saw similar results for specific groups aged 40 to 69 years (web appendix, table A5 and fig A1). Results were also similar for different categories of sex, or race (web appendix, tables A6-A10) and differing baseline periods (1992-5 or 1992-7; results not shown).
Discussion
The results of this study suggest that, if the effects of mobile phones on malignant glioma risk are substantial, then the incidence rates in the US population would be far higher than those observed over most of the study period in 1992-2008 (fig 2). Although we cannot rule out modest increases in glioma incidence since 1992, increases of 20% or more that might occur if the latency period was short (≤5 years) or relative risk was large (≥2.0) were inconsistent with the observed SEER data. Using the relative risks from the Swedish study10 and accounting for the substantial increase in phone use in 1992-2008, our alternative analysis predicted that glioma rates should be about 44% higher than the observed incidence rates for 2008.
However, if we used the relative risks from the Interphone study,4 the increase in mobile phone use in 1992-2008 predicted a modest reduction in glioma incidence of about 7% (or an increase of about 3% if assuming relative risks ≥1); these results were consistent with the observed rate. However, we did not find evidence supporting the overall reduction of about 19% when comparing ever use and never use groups, as implied by the Interphone study (fig 2). The J shaped dose-response curve in the Interphone study, of which this 19% reduction is one indicator, has been used to argue for possible participation bias, implying that risks ought to be estimated relative to the lowest use group, rather than to non-users (that is, using the results from appendix 2 of the study).4 The findings based on appendix 2 of the Interphone study were consistent with observed glioma trends (tables 5 and 6).
Without data indicating substantial effects of mobile phone exposure on incidence rates of brain cancer,1 2 3 4 5 it is not possible to accurately estimate the minimum latency period. Ionising radiation is generally assumed to have a minimum latency period of 2-5 years.30 31 The induction of cancer is thought to occur largely by the initiation of DNA lesions.32 In particular, clinical evidence has shown clonal DNA mutations in brain tumours,33 34 35 36 implying that DNA damage could be the initiating event. Ionising radiation, which is known to induce brain cancer,30 is thought to do so by initiating large scale chromosomal damage resulting from DNA breakage and rearrangement.32
Since microwave radiation produced by mobile phones is non-ionising and therefore not strong enough to cause DNA lesions directly, it probably acts later in the carcinogenic process. This effect implies that the minimum latency period for radiation produced by mobile phones is probably shorter than that for ionising radiation (that is, <5 years). However, since the cause of brain cancer is still unclear, we could not definitively state a minimum latency period, and therefore considered several periods between 1 and 10 years, similar to other studies.4 10 The Swedish study10 suggested a minimum latency period of at least 10 years (table 2; web appendix, table A1). This result is puzzling, because the study used data for people diagnosed in 1997-2003, and mobile phone use in Sweden only began to be appreciable only in the mid to late 1990s.14 17
Several scientific groups have reviewed the experimental in vivo and in vitro data available for microwave exposure from mobile phone use.12 37 No compelling data have suggested that microwave exposure can increase the risk of any type of cancer, or raise rates of somatic or germ cell mutation.37 In particular, a study of 480 Fischer rats did not find any excess risk of glioma or astrocytoma in those exposed to 835.62 MHz or 847.74 MHz of microwave radiation.38 However, the study’s statistical power for astrocytoma was probably low, because the 160 controls had a 1% prevalence.
Strengths and limitations of the study
This study used population based incidence data from the well regarded SEER programme. The SEER data’s high quality was evidenced by the completeness of case ascertainment and the accurate classification of cancer sites and histological types. However, the appropriate exposure measure for brain cancer is still unclear in relation to mobile phone use. A widely used method is to use an “ever versus never use” comparison.1 2 3 4 5 6 7 8 9 Metrics based on the duration of mobile phone use have also been used—that is, the number of minutes per day of operation, duration of use (in years), or cumulative period of use (in hours).1 2 4 7 8 10 We used a model based on an “ever versus never use” comparison (fig 2) and another based on the cumulative hours of mobile phone use (figs 3 and 4, table 4). (Our definition of “ever use” was based on the ownership of a phone, whereas the Interphone study defined “ever use” as an average of at least one phone call per week for six months or more, based on interview data from individuals.4) We used both models in conjunction with data for phone subscriptions gathered for the US as a whole,25 to assess the effect of mobile phone use on glioma incidence.
Subscription data may have slightly underestimated the proportion of people who were mobile phone users, because people might have used a phone without being a subscriber. More likely, the data could have overestimated the proportion, because some individuals might have had multiple subscriptions. The number of subscribers in 2011 exceeded the US population by about 2%,25 implying that the estimate was unlikely to be substantially in error downwards, and we suspect also upwards. The area covered by the SEER registries might not have represented the US as a whole in its ownership and use of mobile phones. Furthermore, the age distribution of users might not have matched that of the underlying SEER population, although the two cannot be very different towards the end of the period considered when ownership approached 100% of the population.
The second model used was slightly more sophisticated, and used estimates of relative risk for specific classes of latency periods and cumulative hours of phone use reported by the Swedish study10 and Interphone study.4 We used both models to predict cancer rates (particularly for the period 1997-2008), with data for mobile phone ownership. A critical assumption of both models was that the underlying cancer rates (in the absence of phone use) remained constant at the levels determined for the period 1992-6, when use was relatively modest. However, for low grade tumours and those of poorly specified anatomical location, incidence seemed to decrease in 1992-2008 (figs 3 and 4), so this assumption might not have been valid for these endpoints. The reduction in tumours with poorly specified sites might have indicated improvements in diagnosis during this period, which would therefore lead to increased rates of gliomas at the temporal lobe and at other specified sites. The fact that the rate of increase did not change substantially after 1996 for gliomas at the temporal lobe and at other specified sites suggests that phone use was not a contributing factor.
The generally flat trend in incidence could have masked an increasing glioma risk associated with mobile phone use that had been counterbalanced by a fall in incidence due to reductions in other hypothetical exposures associated with excess risk of glioma. However, the increase in phone use during the study period would probably not have cancelled out the overall reduction in glioma rates due to speculative other contributing factors. Finally, risks of glioma in small susceptible subgroups might not have been detectable in aggregate population risks.
We focused on non-Hispanic white people, because black and Hispanic white people are known to have lower rates of brain tumours13 and also make up variable proportions of the underlying SEER population, as seen with the rapidly increasing proportion of Hispanic white people in the largest SEER registry (Los Angeles). However, analyses in additional ethnic groups have produced similar results (web appendix, tables A6-A8).
Excess risks of glioma associated with mobile phone use might not become apparent for at least 10 years. However, the latency periods used in our models were based on observations in the Interphone study4 and Swedish study.10 The Swedish study suggested an appreciable risk of glioma within 10 years of exposure.
Delays in cancer registration of glioma cases could have caused recent incidence rates to underestimate the true rates. Calculations based on SEER data have suggested that 2008 rates of brain cancer in white people, after adjustment for delay, might be about 4% higher than those initially reported.18
The choice of 1992-6 as the baseline period was arbitrary, and the interval was used because of the low level of mobile phone subscriptions (<15% of the US population) during this period. Results obtained using alternative baseline periods (1992-5 and 1992-7) were very similar.
We assumed that the patterns of mobile phone use (numbers of hours used by years of latency) were similar to the Swedish10 and the Interphone studies.4 To the best of our knowledge, analogous data for phone use do not exist for the US population. However, in view of the similar distribution of hours of use by latency period in the Swedish10 and Interphone studies4 (tables 2 and 3), we would not expect any patterns of use in the US population to be substantially different from those considered in these two studies.
Another weakness was that the estimated cumulative hours of use was for the period 1997-2003 for the Swedish study10 or 2000-4 for the Interphone study,4 while incidence trends in our analysis were predicted from 1997 to 2008. Owing to the additional four or five years of incidence included in our study, a substantially larger proportion of the mobile phone users would have reached the numbers of hours of phone use in the highest exposure categories of the Swedish10 and the Interphone studies,4 as well as longer latency periods. The cumulative hours of use among participants in the Interphone study were recorded mostly in 1980-2004, when mobile phone use was less common, more expensive, and less a part of daily life than it is in the more recent years of the present study. Use of the estimated cumulative hours of use from the Swedish10 and Interphone4 studies would have resulted in our underestimating the predicted change in the incidence trends. However, this would only appreciably affect our results if we assumed a minimum latency period shorter than 5 years.
In the Interphone study,4 participation bias had been postulated as an explanation for the overall reduced risk for glioma and meningioma. Assuming that the bias was uniform across all exposure groups, this could be eliminated by using the renormalising strategy as proposed in appendix 2 of the Interphone study.4 The relative risks used in our study were always assumed to be relative to non-users. But we also used groups with the lowest phone use as a baseline category (as in appendix 2 of the Interphone study), with the assumption that glioma rates in these groups were identical to those in non-users.
What is already known on this topic
The IARC recently re-evaluated brain tumour risks associated with mobile phone exposure and classified microwave radiation produced by mobiles phones as a possible human carcinogen, largely based on relative risks reported by two epidemiological studies, the 2010 Interphone study and a 2011 Swedish study by Hardell and colleagues
However, trends in brain cancer incidence have not mirrored the substantial increase in mobile phone use since the mid-1990s, and have generally remained constant
What this study adds
We compared projected rates with observed rates of glioma incidence by also considering the effect of detailed latency distribution and patterns of mobile phone use
Based on relative risks from the Swedish study, predicted rates of glioma were much higher than (and therefore statistically inconsistent with) observed rates. However, based on relative risks from the Interphone study, projected rates could be consistent with the observed data
Funding: This work was supported by the Intramural Research Program of the National Institutes of Health, and the National Cancer Institute, Division of Cancer Epidemiology and Genetics.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: funding support from the Intramural Research Program of the National Institutes of Health, and the National Cancer Institute, Division of Cancer Epidemiology and Genetics; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Data from the SEER registry have no personal identifying information and therefore ethical approval not required.
Contributors: MPL did the statistical analysis and is the data guarantor. All the authors contributed to the drafting of the manuscript, had full access to all the data (including statistical reports and tables) in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis.
Data sharing: The SEER data described in this study and web appendix are freely available on application to SEER (http://seer.cancer.gov/data/). The statistical codes used are available from the corresponding author.
Cite this as: BMJ 2012;344:e1147
Web Extra. Extra material supplied by the author
Web appendix: Statistical methods and supplementary data
References
- 1.Muscat JE, Malkin MG, Thompson S, Shore RE, Stellman SD, McRee D, et al. Handheld cellular telephone use and risk of brain cancer. JAMA 2000;284:3001-7. [DOI] [PubMed] [Google Scholar]
- 2.Inskip PD, Tarone RE, Hatch EE, Wilcosky TC, Shapiro WR, Selker RG, et al. Cellular-telephone use and brain tumors. N Engl J Med 2001;344:79-86. [DOI] [PubMed] [Google Scholar]
- 3.Schüz J, Jacobsen R, Olsen JH, Boice JD Jr, McLaughlin JK, Johansen C. Cellular telephone use and cancer risk: update of a nationwide Danish cohort. J Natl Cancer Inst 2006;98:1707-13. [DOI] [PubMed] [Google Scholar]
- 4.INTERPHONE Study Group. Brain tumour risk in relation to mobile telephone use: results of the INTERPHONE international case-control study. Int J Epidemiol 2010;39:675-94. [DOI] [PubMed] [Google Scholar]
- 5.Frei P, Poulsen AH, Johansen C, Olsen JH, Steding-Jessen M, Schüz J. Use of mobile phones and risk of brain tumours: update of Danish cohort study. BMJ 2011;343:d6387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Auvinen A, Hietanen M, Luukkonen R, Koskela RS. Brain tumors and salivary gland cancers among cellular telephone users. Epidemiology 2002;13:356-9. [DOI] [PubMed] [Google Scholar]
- 7.Hardell L, Mild KH, Carlberg M. Case-control study on the use of cellular and cordless phones and the risk for malignant brain tumours. Int J Radiat Biol 2002;78:931-6. [DOI] [PubMed] [Google Scholar]
- 8.Hardell L, Carlberg M, Mild KH. Case-control study of the association between the use of cellular and cordless telephones and malignant brain tumors diagnosed during 2000-2003. Environ Res 2006;100:232-41. [DOI] [PubMed] [Google Scholar]
- 9.Hardell L, Carlberg M. Mobile phones, cordless phones and the risk for brain tumours. Int J Oncol 2009;35:5-17. [DOI] [PubMed] [Google Scholar]
- 10.Hardell L, Carlberg M, Hansson MK. Pooled analysis of case-control studies on malignant brain tumours and the use of mobile and cordless phones including living and deceased subjects. Int J Oncol 2011;38:1465-74. [DOI] [PubMed] [Google Scholar]
- 11.Sato Y, Akiba S, Kubo O, Yamaguchi N. A case-case study of mobile phone use and acoustic neuroma risk in Japan. Bioelectromagnetics 2011;32:85-93. [DOI] [PubMed] [Google Scholar]
- 12.Baan R, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L et al. Carcinogenicity of radiofrequency electromagnetic fields. Lancet Oncol 2011;12:624-6. [DOI] [PubMed] [Google Scholar]
- 13.Inskip PD, Hoover RN, Devesa SS. Brain cancer incidence trends in relation to cellular telephone use in the United States. Neuro Oncol 2010;12:1147-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deltour I, Johansen C, Auvinen A, Feychting M, Klaeboe L, Schüz J. Time trends in brain tumor incidence rates in Denmark, Finland, Norway, and Sweden, 1974-2003. J Natl Cancer Inst 2009;101:1721-4. [DOI] [PubMed] [Google Scholar]
- 15.De Vocht F, Burstyn I, Cherrie JW. Time trends (1998-2007) in brain cancer incidence rates in relation to mobile phone use in England. Bioelectromagnetics 2011;32:334-9. [DOI] [PubMed] [Google Scholar]
- 16.De Vocht F, Burstyn I, Cherrie JW. Authors’ reply to Kundi’s comments on de Vocht et al. “Time trends (1998-2007) in brain cancer incidence rates in relation to mobile phone use in England.” Bioelectromagnetics 2011;32:675-6. [DOI] [PubMed] [Google Scholar]
- 17.Ahlbom A, Feychting M. Mobile telephones and brain tumours. BMJ 2011;343:d6605. [DOI] [PubMed] [Google Scholar]
- 18.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W et al. SEER cancer statistics review, 1975-2008. National Cancer Institute, 2011.
- 19.Surveillance, Epidemiology, and End Results (SEER) Program. SEER*stat database: incidence—SEER 13 regs research data. National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, 2011.
- 20.Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International classification of diseases for oncology. 3rd ed (ICD-O-3). World Health Organization, 2000.
- 21.Central Brain Tumor Registry of the United States (CBTRUS). CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2004-2006. Central Brain Tumor Registry of the United States, 2010.
- 22.Ries LAG, Young JL Jr, Keel GE, Eisner MP, Lin YD, Horner MJD. Cancer survival among adults: US SEER program, 1988-2001. Patient and tumor characteristics. SEER Survival Monograph. Publication 07-6215. SEER, 2007.
- 23.Claus EB, Black PM. Survival rates and patterns of care for patients diagnosed with supratentorial low-grade gliomas. Cancer 2006;106:1358-63. [DOI] [PubMed] [Google Scholar]
- 24.Louis DN, Ohgaki H, Wiestler OD, Cavanee WK. WHO classification of tumours of the central nervous system. International Agency for Research on Cancer, 2007.
- 25.Cellular Telephone Industry Association (CTIA). CTIA semi-annual wireless industry survey. 2011. http://files.ctia.org/pdf/CTIA_Survey_MY_2011_Graphics.pdf.
- 26.US Census Bureau. Population estimates. 2011. www.census.gov/popest/eval-estimates/eval-est.html.
- 27.McCullagh P, Nelder JA. Generalized linear models. 2nd ed. Monographs on statistics and applied probability 37. Chapman and Hall/CRC, 1989.
- 28.Preston DL, Lubin JH, Pierce DA, McConney ME. Epicure release 2.10. Hirosoft International, 1998.
- 29.Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). UNSCEAR 2006 report. Annex A. Epidemiological studies of radiation and cancer. United Nations, 2008.
- 31.United States National Research Council, Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health risks from exposure to low levels of ionizing radiation: BEIR VII—phase 2. National Academy Press, 2006. [PubMed]
- 32.Little MP, Wakeford R, Tawn EJ, Bouffler SD, Berrington de Gonzalez A. Risks associated with low doses and low dose rates of ionizing radiation: why linearity may be (almost) the best we can do. Radiology 2009;251:6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sidransky D, Mikkelsen T, Schwechheimer K, Rosenblum ML, Cavanee W, Vogelstein B. Clonal expansion of p53 mutant cells is associated with brain tumour progression. Nature 1992;355:846-7. [DOI] [PubMed] [Google Scholar]
- 34.Zhu JJ, Maruyama T, Jacoby LB, Herman JG, Gusella JF, Black PM, et al. Clonal analysis of a case of multiple meningiomas using multiple molecular genetic approaches: pathology case report. Neurosurgery 1999;45:409-16. [DOI] [PubMed] [Google Scholar]
- 35.Busque L, Zhu J, DeHart D, Griffith B, Willman C, Carroll R, et al. An expression based clonality assay at the human androgen receptor locus (HUMARA) on chromosome X. Nucleic Acids Res 1994;22:697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tada M, Iggo RD, Ishii N, Shinohe Y, Sakuma S, Estreicher A, et al. Clonality and stability of the p53 gene in human astrocytic tumor cells: quantitative analysis of p53 gene mutations by yeast functional assay. Int J Cancer 1996;67:447-50. [DOI] [PubMed] [Google Scholar]
- 37.Advisory Group on Non-ionising Radiation. Health effects from radiofrequency electromagnetic fields. Report of an advisory group on non-ionising radiation. Documents of the NRPB. National Radiological Protection Board, 2003.
- 38.La Regina M, Moros EG, Pickard WF, Straube WL, Baty J, Roti Roti JL. The effect of chronic exposure to 835.62 MHz FDMA or 847.74 MHz CDMA radiofrequency radiation on the incidence of spontaneous tumors in rats. Radiat Res 2003;160:143-51. [DOI] [PubMed] [Google Scholar]
- 39.Hardell L, Carlberg M, Hansson MK. Re-analysis of risk for glioma in relation to mobile telephone use: comparison with the results of the Interphone international case-control study. Int J Epidemiol 2011;40:1126-8. [DOI] [PubMed] [Google Scholar]
- 40.Johansen C, Boice J Jr, McLaughlin J, Olsen J. Cellular telephones and cancer—a nationwide cohort study in Denmark. J Natl Cancer Inst 2001;93:203-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Statistical methods and supplementary data