Abstract
Background:
The number of patients requiring in-patient rehabilitation services following acute stroke is unknown.
Methods:
All consecutive patients admitted with a diagnosis of stroke to eight community hospitals in southwestern Ontario from May 2008 to December 2009 were screened for in-patient rehabilitation eligibility using the Stroke Rehabilitation Candidacy Screening Tool.
Results:
Three hundred ninety-six patients were included, of which 147 (37.1%) were identified as candidates for in-patient rehabilitation. Of these patients, 111 (75%) were discharged to an in-patient rehabilitation unit. The most frequently documented reason that candidates were not transferred was lack of an available bed (n=19). Two hundred forty-nine (62.9%) patients were not considered candidates. The majority (80%) of these patients had experienced either mildly or severely disabling stroke and went home or directly to long-term care upon discharge.
Conclusion:
The reported estimate of 37% who required in-patient rehabilitation services is important for the purposes of planning and allocation of healthcare resources.
Abstract
Contexte :
On ne connaît pas bien le nombre de patients qui ont besoin de services de réadaptation après un accident cérébrovasculaire aigu.
Méthode :
Tous les patients admis suite à un diagnostic d'accident cérébrovasculaire dans huit hôpitaux communautaires du sud-ouest ontarien entre mai 2008 et décembre 2009 ont été soumis au protocole de dépistage pour les candidats à la réadaptation après un accident cérébrovasculaire (Stroke Rehabilitation Candidacy Screening Tool).
Résultats :
Trois cent quatre-vingt-seize patients ont été considérés. Parmi eux, 147 (37,1 %) ont été désignés comme candidats à la réadaptation. De ces patients, 111 (75 %) ont été dirigés vers une unité de réadaptation pour patients hospitalisés. La raison la plus évoquée pour ne pas y diriger un patient était le manque de lits disponibles (n=19). Deux cent quarante-neuf (62,9 %) patients n'ont pas été désignés candidats. La majorité (80 %) de ces patients avaient subit un accident cérébrovasculaire causant une invalidité de moyenne à sévère et ont reçu leur congé ou sont allés directement aux soins de longue durée.
Conclusion :
La proportion estimée de 37 pour cent des patients ayant besoin de services de réadaptation pour patients hospitalisés est importante pour la panification et la répartition des ressources en santé.
While it has been established that organized in-patient rehabilitation provides the greatest opportunity for recovery following stroke (Stroke Unit Trialists' Collaboration 2007), there is no universally accepted, standardized set of criteria available to healthcare providers to assess in-patient rehabilitation candidacy (Wade 2003). However, because stroke represents a significant societal burden, it is important to choose potential candidates wisely to ensure that limited healthcare resources are allocated appropriately. While many patients may benefit from intensive rehabilitation, it is not cost-effective to offer in-patient rehabilitative care to those least likely to demonstrate substantial improvement with treatment, or those left with little or no residual disability whose needs can be met instead within outpatient or home-based programs.
Studies of consecutive, unselected patients admitted to an acute care hospital with a diagnosis of stroke have reported that 9.5% to 44% are discharged to in-patient rehabilitation units/programs (Lai et al. 1998; Mayo et al. 1989; Rundek et al. 2000; Schlegel et al. 2003; Mahler et al. 2008; Treger et al. 2008). This wide range may be due to differences in service availability and delivery, as well as methods of remuneration among different regions or countries, and may, in part, reflect restrictions on services or patients' ability or willingness to pay for services. As a result, discharge to a stroke rehabilitation unit is not an accurate indicator of appropriate candidacy and should not be considered a suitable proxy.
Although the need for an estimate of the percentage of patients who require in-patient rehabilitation following stroke should be apparent to those charged with the task of planning and administering these services, to date, one does not exist. As a result, it is unknown whether the current level of rehabilitation service provision is sufficient to meet the need. There is evidence to suggest that it does not and that demand exceeds capacity. Across Canada (2007– 2008), 23% of stroke patients spent at least one day in alternative level of care (ALC) status, indicating that the patient no longer required the intensity of medical care available in an acute care facility (CIHI 2009). Waiting for access to a rehabilitation bed was cited as a reason that 19% of patients remained in acute care for longer than necessary.
To the best of our knowledge, there are no published reports in which persons with stroke were assessed for in-patient rehabilitation candidacy during their stay in acute care and followed to determine their eventual discharge destination. The objectives of this study were to identify appropriate candidates for admission to in-patient rehabilitation using a standardized screening method, and to establish what percentage of the identified candidates were discharged to an in-patient rehabilitation unit.
Methods
From May 1, 2008 to December 31, 2009, all patients admitted consecutively to eight community hospitals in the southwestern region of Ontario with a diagnosis of acute stroke (International Classification of Diseases [ICD]-10 codes 160–169) and who were discharged alive from their acute stay admission were included. Institutions were categorized based on the annual number of admissions for stroke, as low (<33), medium (33–99) or high (≥100). Two offered limited, non-specialized rehabilitation in general adult rehabilitation beds, while the remaining institutions transferred patients for in-patient rehabilitation to a regional 30-bed stroke rehabilitation unit in a freestanding rehabilitation hospital. The cost of all in-patient rehabilitation services was covered by the publicly funded healthcare system.
Patients were screened for potential eligibility for in-patient rehabilitation using the Stroke Rehabilitation Candidacy Screening Tool (see Appendix). The SRCST was developed based on a service provision model recommended by provincial standards of care that outlined factors to be considered in determining the need for in-patient rehabilitation. A regional task team of clinical experts formed to create a tool to standardize admission criteria that could be implemented across the southwestern region of Ontario. The SRCST was developed as a means to standardize the assessment procedure and included criteria that enabled patients the opportunity to pursue a wide range of rehabilitation goals. The screening tool was composed of two parts, candidacy and readiness. The candidacy criteria included ability to follow commands, presence of rehabilitation goals, demonstrated improvement over the period of acute hospitalization that were related to rehabilitation goals and willingness to participate in rehabilitation. Time over which improvement was demonstrated varied depending on the severity of the stroke, as assessed by the AlphaFIM® Instrument.
The AlphaFIM® portion of the screening tool was to be completed during the first three to five days following admission to acute care. The remaining portions of the candidacy criteria could be completed during the patient's stay on the acute unit as information became available. The AlphaFIM® Instrument is an abbreviated six-item version of the 18-item FIM® Instrument intended for use in the acute care setting (Stillman et al. 2009). The instrument includes four motor items (eating, grooming, bowel management and toilet transfer) and two cognitive items (verbal expression and memory). Each item was scored on a scale ranging from 1 (total assistance required) to 7 (complete independence), using pre-defined criteria. AlphaFIM® Software Release 2.0 was used to convert raw scores, ranging from 6 to 42, to projected total FIM® scores, ranging from 18 to 126. The AlphaFIM® Instrument was used as a proxy measure for stroke severity and to establish a time frame over which functional improvement was expected to be demonstrated. Scores were used to assign patients to categories based on stroke severity: mild (81–126), moderate (40–80) and severe (18–39).
If the SRCST screen was not completed during the hospital stay, the information associated with each item of the tool could also be retrieved by chart audit, ensuring that a determination of the in-patient rehabilitation candidacy for each patient in the cohort could be made. The one item that could not be scored retrospectively was the AlphaFIM® Instrument; therefore, the six-item modified Rankin Scale (mRS) was used as its proxy. Modified Rankin Scale scores range from 0 (no symptoms) to 5 (severe disability) (van Swieten et al. 1988). The mRS scores were also collected for all subjects, regardless of the availability of AlphaFIM® Instrument data as a measure of global function.
A patient was considered to be a rehabilitation candidate if he or she fulfilled all criteria for candidacy. Candidates were then followed to determine if and when readiness criteria were met. Readiness criteria included items relating to activity tolerance and medical stability. The ability to sit upright out of bed for a minimum of one hour, twice a day was evidence of tolerance. The following items were used to assess whether a patient was medically stable: etiology of the stroke explored and investigations either completed or in progress, secondary prevention completed or in progress, co-morbid medical conditions stable and life expectancy greater than six months (see Appendix). The inter-rater reliability of the screening tool has been established previously (Willems et al. 2009).
Specially trained personnel (occupational therapists, physical therapists, nurses and speech–language pathologists) completed the screening tool using direct observation of the patient and consultation with other members of the patient's care team. The resulting recommendations were available to the acute care team but were non-binding in that the receiving institution or unit could accept or reject any given patient. Discharge destination was established at a later date by chart review. Information was also collected on age, sex, length of hospital stay and days spent in ALC. Patients identified as ALC were those awaiting transfer to another service or facility. Information on rehabilitation services that were recommended or received following discharge from acute care was also recorded for eligible patients who were not transferred to an in-patient rehabilitation unit.
The characteristics and discharge destinations of all patients included in the cohort are presented descriptively. Continuous data are presented as means and standard deviation (±SD). Median and interquartile range (IQR) values are also presented for data relating to length of hospital stay (LOS). In order to determine whether the AlphaFIM® and mRS scores provided similar estimates of function, the correlation coefficient between AlphaFIM® scores and mRS ratings was calculated using Spearman's rho (two-tailed). A p-value of <0.05 was considered to be statistically significant. SPSS v. 19 was used for analyses.
Results
Data were collected on 396 patients (208 males, 188 females) from one high-volume, three medium-volume and four low-volume institutions. The mean age of patients in the cohort was 73 ± 12 years (range: 43–93 years). The mean and median lengths of stay in acute care were 11.4 (±15.2) and 7 (IQR=8) days, respectively. AlphaFIM® and mRS scores were obtained on 235 (59%) and 390 (98%) patients, respectively. There was a significant, inverse correlation between AlphaFIM® and mRS scores (t=–0.842, p<0.01). The severity of stroke for all patients assessed by mRS is presented in Table 1.
TABLE 1.
Stroke severity of patients included in the study
| Stroke Severity | In-Patient Rehabilitation Candidates | Non-Candidates for In-Patient Rehabilitation | All | |
|---|---|---|---|---|
| Number | Percentage | |||
| Modified Rankin Scale score: | ||||
| No symptoms (0) | 0 | 2 | 2 | 29.3% |
| No disability (1) | 0 | 72 | 72 | |
| Slight disability (2) | 5 | 37 | 42 | |
| Moderate disability (3) | 30 | 29 | 59 | 51.0% |
| Moderately severe disability (4) | 89 | 54 | 143 | |
| Severe disability (5) | 23 | 49 | 72 | 18.2% |
| Insufficient data to score | 0 | 6 | 6 | 1.5% |
| Totals | 147 | 249 | 396 | |
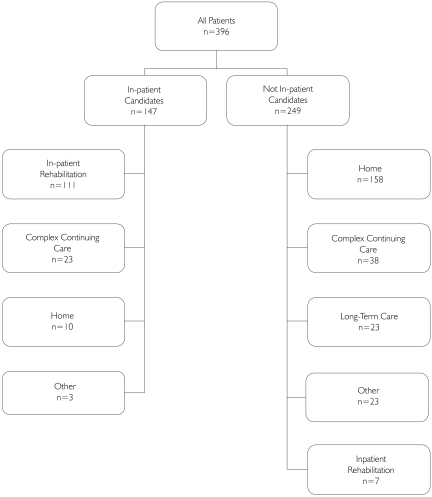
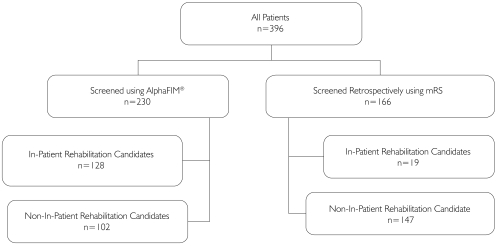
The flow of all patients included in the study is presented in Figure 1. Of the 396 patients admitted to acute care, 147 (37.1%) were identified as appropriate candidates for in-patient rehabilitation. Basic demographic details of both candidates and non-candidates are presented in Table 2. The number of patients who were assessed using prospective and retrospective data is presented in Figure 2. The percentages of patients identified as in-patient rehabilitation candidates among low-, medium- and high-volume institutions were 27.5%, 41% and 37%, respectively.
FIGURE 1.
Flow diagram indicating patients' discharge destination from acute care
TABLE 2.
Data for in-patient rehabilitation candidates and non-candidates
| Candidates (n=147) | Non-Candidates (n=249) | |
|---|---|---|
| Mean age (years) ± SD | 70.5 ± 12.8 | 74.3 ± 11.9 |
| Male/female (#, %) | 82 (56)/65 (44) | 126 (51)/123 (49) |
| Mean LOS (days) ± SD | 14.0 ± 17 | 9.8 ± 13.8 |
| Median (IQR) | 9 (9) | 5 (8) |
| Mean Alc days ± sD | 4.6 ± 8.4 | 1.48 ± 6.4 |
| Total Alc days | 480 | 351 |
LOS: Length of stay
IQR: Interquartile range
ALC: Alternative level of care
FIGURE 2.
Rehabilitation candidacy criteria determined by prospective and retrospective data
Of the rehabilitation-eligible patients, 111 (75%) were discharged from acute care to an in-patient rehabilitation unit, after an average of 10.0 ± 8.7 days. At the time of discharge from the acute unit, 107 patients had fulfilled the readiness criteria for activity tolerance and 110 had for medical stability. Sixty-two rehabilitation-eligible patients remained in acute care for at least one day longer than was medically necessary. The most frequently documented reason that the 36 remaining, appropriate candidates were not transferred to an in-patient rehabilitation service was lack of an available bed (n=19). The majority of eligible candidates who were not discharged to in-patient rehabilitation were transferred to a complex continuing care (CCC) bed, where rehabilitation service provision was limited and variable. The final discharge destinations of these patients were not recorded.
Following screening, 249 patients (62.9%) were not considered candidates for in-patient rehabilitation. Of these, 111 patients had mRS scores ranging from 0 to 2; 62 were discharged on or before day 3, technically before the screen could be completed prospectively. All but one of the 111 patients who had experienced a mild stroke were discharged directly home from acute care after an average of 3.9 ± 2.6 days. No follow-up rehabilitation services were recommended for 83 of these patients, while either in-home or hospital-based outpatient programs were recommended for 28 remaining patients following discharge. Of the 49 patients who were assessed using the SRCST, 26 (53%) had no rehabilitation goals, four were not willing to participate and one had not demonstrated functional improvement. In four cases, the length of stay was too short to determine whether improvement had occurred. At least one of the candidacy criteria was not documented in 13 cases. The itemized results of the candidacy screening tool for patients with mRS scores of 3, 4 and 5, who were not candidates for in-patient rehabilitation, are presented in Table 3.
TABLE 3.
Candidacy criteria of 138 patients with modified Rankin Scale scores of 3 to 5 who were not candidates for in-patient rehabilitation
| Candidacy Criteria | Modified Rankin Scale Scores | |||
|---|---|---|---|---|
| 3 (n=29) | 4 (n=54) | 5 (n=49) | ||
| Follows commands | ||||
| No | 0 | 9 | 25 | |
| Yes | 28 | 41 | 22 | |
| Not documented | 1 | 1 | 2 | |
| Has Rehab Goals | ||||
| No | 4 | 12 | 22 | |
| Yes | 14 | 19 | 12 | |
| Not documented | 11 | 23 | 15 | |
| Demonstrates Change | ||||
| No | 0 | 17 | 37 | |
| Yes | 23 | 26 | 4 | |
| Not documented | 3 | 6 | 7 | |
| LOS too short to determine | 3 | 5 | 1 | |
| Willing to Participate | ||||
| No | 6 | 12 | 12 | |
| Yes | 15 | 14 | 10 | |
| Not documented | 4 | 20 | 8 | |
| Not applicable | 4 | 8 | 9 | |
Discussion
The Ontario Stroke Network has recently set a benchmark of 39%, indicating the percentage of all patients who should be admitted for in-patient rehabilitation following discharge from an acute care facility in Ontario (Hall et al. 2010). This figure was calculated retrospectively using a paired-mean approach (Kiefe et al. 1998) based on in-patient rehabilitation admissions from the 11 Regional Stroke Centres in Ontario over seven quarters (from 2006 to 2008). In this study of 396 unselected patients admitted to eight acute care institutions, 37.1% were identified as appropriate candidates for in-patient rehabilitation using a standardized screening method. This figure, derived using a prospective process, is quite similar to the proposed benchmark. However, the estimates of either 37% or 39% of individuals who require in-patient rehabilitation services following stroke diverge sharply from historical estimates of those who have received it. From the years 2003 to 2008, between 21% and 23% of all stroke patients in Ontario were admitted for in-patient rehabilitation (Hall et al. 2010). Moreover, the percentage of patients who were admitted to in-patient rehabilitation programs ranged from 9% to 45% across regions, suggesting variations in admitting practices. Previously, there has been no reference point from which to assess whether the level of service provided was a reflection of actual need or the limits of capacity; the results of this study may suggest the latter.
Among patients deemed to be appropriate candidates for in-patient rehabilitation in this study, 75% were discharged to a location where they would receive this service. The main reason that an appropriate rehabilitation candidate was not discharged to a rehabilitation bed was availability. Whether bed shortages were chronic or cyclical is unknown; however, patients in this study spent a substantial number of days in ALC status awaiting a rehabilitation bed. In addition, seven patients were screened and deemed not to be suitable candidates but were nevertheless discharged to an in-patient rehabilitation facility, suggesting that factors other than suitability for rehabilitation sometimes determine discharge destination. One of these patients was unable to follow commands, had no rehabilitation goals and was unwilling to participate in an in-patient program. In this particular case, pressure to vacate the acute care bed at a time when a rehabilitation bed was available may have been the deciding factor.
The screening tool was designed to be patient-focused. It de-emphasized initial stroke severity as the primary criterion and minimized the use of prognostic and external factors such as age and caregiver availability among the candidacy criteria, factors that are often used in clinical decision-making. As a result, patients from across the severity spectrum were identified as in-patient rehabilitation candidates, including those with severely disabling strokes. Although within the limits of a constrained healthcare system these patients have not traditionally been considered good candidates for in-patient rehabilitation, evidence suggests that they do benefit. Using the definition of “non-ambulatory” to classify stroke as severe, patients admitted to a specialized rehabilitation program demonstrated significant improvements in FIM® scores from admission to discharge and 43% returned home (Teasell et al. 2005). Almost certainly, without that opportunity a large number of these patients would otherwise have been admitted directly to a long-term care institution.
The use of the SRCST had been adopted voluntarily within the preceding year by the participating institutions; its use was not mandatory. The tool had not been completed prospectively on a substantial number of patients. In some cases, this may have been due to early discharge, because 24% of patients were discharged on or before day 5 following admission. Alternatively, it may also suggest that busy clinicians saved themselves additional work, anticipating that these patients would not be considered appropriate candidates and would be discharged imminently, or they engaged in their own informal pre-screening. Regardless of the reason, of the 166 patients who were not screened during their hospital stay and discharged, 19 were later identified as rehabilitation candidates when the SRCST tool was scored by chart audit. It is of concern that a large percentage of patients were discharged from acute care within the first five days of stroke without their need for rehabilitation services having been assessed.
The results of this study may be used to estimate the number of patients who require in-patient rehabilitation on a provincial level. Using the most updated data from the Ontario Stroke Evaluation Report (Hall et al. 2010: 39), a total of 13,219 patients were discharged alive from an acute care facility following stroke in a single year (2007/08). In that same year, 2,998 (22.7%) patients were discharged to a rehabilitation facility. If we use the estimate of 37% from the present study, then 4,891 patients should have had access to a rehabilitation bed but did not, leaving 1,893, or 14.3% of all admissions, with an unmet need. The gap between the need for care and current levels of service availability is notable.
One of the strengths of this study was that candidacy criteria were applied in a standardized fashion. We did not use a statistical modelling approach that included an array of prognostic factors to predict admission to a rehabilitation program as a surrogate marker for the patients who require in-patient rehabilitation, as others have (Treger et al. 2008; Ilett et al. 2010; Schlegel et al. 2003; Rundek et al. 2000). These studies, which included patients already admitted for in-patient rehabilitation, have assumed that all patients who were admitted were suitable candidates and excludes the unknown number of patients who were not admitted but who might have been appropriate candidates had they been assessed.
There are several limitations to this study. For a large number of patients (41%), candidacy assessment was completed using a retrospective process. Because patients were not followed to their final destination, some may have been admitted for in-patient rehabilitation following discharge to an intermediate destination, such as CCC or home. Another limitation is that pre-stroke living arrangements were unknown. Given that it is unlikely that a patient admitted to acute care from a LTC facility would be considered a rehabilitation candidate, this may have slightly inflated our reported estimate of the percentage of patients requiring in-patient rehabilitation. Patients who presented with stroke requiring neurosurgical services were not included in this study and may have led to an underestimate. These patients were transferred to the regional tertiary care centre for treatment. Although the standardized tool we developed and used may require modifications and adaptations for broader use, we have demonstrated that it is feasible to screen patients for in-patient rehabilitation eligibility in the early days following stroke.
Conclusion
This is the first study to assess the rehabilitation candidacy of patients within a defined cohort using a standardized method. While only eight hospitals in southwestern Ontario were included, the estimate we report of 37% of patients who require in-patient rehabilitation following a stroke could be used as an approximation of need in other jurisdictions for planning and assessing rehabilitation capacity. This work serves as an important first step to address the question of whether the current level of access to stroke rehabilitation in Ontario reflects the true need for service.
The findings in this study – that one in four eligible patients was not admitted for rehabilitation because a bed was not available, and that the mean number of ALC days waiting for rehabilitation was greater than that for all other discharge destinations – are concerning. They suggest a mismatch between existing rehabilitation resources and need, an inefficient use of those resources resulting in poor flow across the system, or both.
As Ontario embarks on its access-to-care initiative and examines the role of the rehabilitation and complex continuing care sectors, the estimate of in-patient rehabilitation need will be important for assessing current capacity within the province and its local health integration networks.
Acknowledgements
This project was supported by funds from the Canadian Stroke Network, the Ontario Stroke Network and South West LHIN.
Special thanks to Christina O'Callaghan, Executive Director of the Ontario Stroke Network, for her assistance with this project.
Appendix
Stroke Rehabilitation Candidacy Screening Tool
Date of Stroke: ___________________________
Rehabilitation Candidacy
Functional Status: AlphaFIM®
| Eating | 1 2 3 4 5 6 7 |
| Grooming | 1 2 3 4 5 6 7 |
| Bowel management | 1 2 3 4 5 6 7 |
| Toilet transfer | 1 2 3 4 5 6 7 |
| Expression | 1 2 3 4 5 6 7 |
| Memory | 1 2 3 4 5 6 7 |
Motor conversion score: ___ Cognitive conversion score: ___ Total FIM® score: ___/126 Date Part 1 completed: ________________
Ability to Follow Commands: □ Yes □ No
Verbal: “Close your eyes”
Nonverbal: Follows written command “Close your eyes” and/or Follows addition of gestural cue for “Close your eyes”
Rehabilitation Goals: □ Yes □ No If yes, select from goals below
From your assessment, the patient requires in-patient rehabilitation to improve:
-
□
communication
-
□
arm and hand function
-
□
cognitive, perceptual ability
-
□
mobility (transfers, ambulation, sitting with comfort)
-
□
ability to perform role (home & money management, organizational, socialization, vocational skills)
-
□
caregiver/family's ability to manage the patient's care after discharge
-
□
return to oral diet (swallowing)
-
□
self care (bathing, dressing, toileting)
-
□
continence (bowel/bladder control)
-
□
other: ________________________________________________
Demonstrates Change: □ Yes □ No
Demonstrates improvement in function over time that is related to rehabilitation goals. (Time over which change will be demonstrated will vary depending on the severity of the stroke.)
Verbal Consent to Participate In Rehabilitation: □ Yes □ No
Patient/substitute decision maker has agreed to Rehabilitation Goals as identified above and indicates willingness to participate in rehabilitation intervention post acute care.
“Would you be willing to participate in rehabilitation services (cite relevant services e.g. PT, OT, SLP, SW or rehabilitation program) to (cite patient/family goals as listed above) after the doctors feel you are ready to leave this acute care service?”
Patient meets all criteria above and should be considered a candidate for rehabilitation: □ Yes □ No
Rehabilitation Readiness
All qualifying candidates will be followed to determine when rehabilitation readiness is achieved as follows:
Tolerance: Tolerates a minimum of one hour sitting up in a wheelchair (or upright out of bed) twice per day. Tolerance achieved: □ Yes □ No
Medical Stability
To guide you in your decision about medical stability, please consider the following:
MRP identifies that patient no longer requires acute care
Cause of stroke explored; medical investigations completed or in process
Secondary prevention/medication plan initiated
Co-morbid medical conditions managed/stable
Patient is not palliative (life expectancy > 6 months)
Medical Stability achieved: □ Yes □ No
Date Part 2 completed: ___________________
Instructions for Completion
AlphaFIM®: Please score according to the AlphaFIM® Instrument Guide and FIM® System Decision Trees.
Ability to Follow Commands: Give the verbal command “close your eyes”. If the patient does not respond appropriately, show them the written command “close your eyes”. If the patient is still unable to respond appropriately, repeat the command verbally “close your eyes” and, while keeping your eyes open, point to your eyes and make a gesture to close them (four fingers horizontally lower as if lowering a blind). Do not close your eyes as this would be testing the patient's ability to copy your action versus follow a command.
Rehabilitation Goals: Please check off any goals that, based on your assessment and clinical judgment, apply to the patient and require treatment in an in-patient rehabilitation setting.
Demonstrates Change: Improvement in function over time that is related to rehabilitation goals. The time over which change in function should be observed is based on stroke severity as follows:
Mild (FIM® >80) over 3 days
Moderate (FIM® 40–80) over 7 days
Severe (FIM® <40) over 14 days
Candidacy: Patient meets all criteria above. Select Yes, if the patient is able to follow commands, has rehab goals and demonstrates change over time according to the criteria above. The AlphaFIM® score will be used to select the appropriate service.
Verbal Consent to Participate in Rehabilitation: Obtain the patient/substitute decision maker's consent using the question provided in the tool.
Tolerance: Identify the length of time that a patient is able to tolerate sitting up out of bed in a wheelchair by observation, or from discussion with the patient's care team, to determine if they meet the minimum requirement. ‘Tolerate’ refers to remaining awake and alert, and reasonably comfortable.
Medical Stability: The points under medical stability are meant to guide you in your decision. It is not meant to be a checklist. MRP refers to the most responsible physician. Select Yes or No based on the information you are able to gather from the chart and patient care team on the day that Part 2 of the assessment is completed.
Contributor Information
Deborah Willems, Regional Rehabilitation Coordinator, Southwestern Ontario Stroke Network, London Health Sciences Centre, London, ON.
Katherine Salter, Research Associate, Aging, Rehabilitation & Geriatric Care Program, Lawson Health Research Institute, London, ON.
Matthew Meyer, Research Associate, Aging, Rehabilitation & Geriatric Care Program, Lawson Health Research Institute, Parkwood Hospital London, ON.
Andrew Mcclure, Research Associate, Aging, Rehabilitation & Geriatric Care Program, Lawson Health Research Institute, Parkwood Hospital, London, ON.
Robert Teasell, Chair/Chief and Professor, Department of Physical Medicine & Rehabilitation, St. Joseph's Health Care London and the Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON.
Norine Foley, Research Associate, Aging, Rehabilitation & Geriatric Care Program, Lawson Health Research Institute, Parkwood Hospital London, ON.
REFERENCES
- Canadian Institute for Health Information (CIHI) 2009. Analysis in Brief: Alternative Level of Care in Canada. Retrieved December 12, 2011. <http://secure.cihi.ca/cihiweb/products/ALC_AIB_FINAL.pdf>
- Hall R., O'Callaghan C., Bayley M., Meyer S., Khan F., Liu Y., et al. 2010. Ontario Stroke Evaluation Report 2010: Technical Report. Toronto: Institute for Clinical Evaluative Sciences; Retrieved December 12, 2011. <http://www.ices.on.ca/webpage.cfm?site_id=1&org_id=32&morg_id=0&gsec_id=6118&item_id=6118&category_id=43> [Google Scholar]
- Ilett P.A., Brock K.A., Graven C.J., Cotton S.M. 2010. “Selecting Patients for Rehabilitation After Acute Stroke: Are There Variations in Practice?” Archives of Physical Medicine & Rehabilitation 91: 788–93 [DOI] [PubMed] [Google Scholar]
- Kiefe C.I., Weissman N.W., Allison J.J., Farmer R., Weaver M., Williams O.D. 1998. “Identifying Achievable Benchmarks of Care: Concepts and Methodology.” International Journal for Quality in Health Care 10: 443–47 [DOI] [PubMed] [Google Scholar]
- Lai S.M., Alter M., Friday G., Lai S.L., Sobel E. 1998. “Disposition After Acute Stroke: Who Is Not Sent Home from Hospital?” Neuroepidemiology 17: 21–29 [DOI] [PubMed] [Google Scholar]
- Mahler M.P., Zuger K., Kaspar K., Haefeli A., Jenni W., Leniger T., et al. 2008. “A Cost Analysis of the First Year After Stroke – Early Triage and In-patient Rehabilitation May Reduce Long Term Costs.” Swiss Medical Weekly 138: 459–65 [DOI] [PubMed] [Google Scholar]
- Mayo N.E., Hendlisz J., Goldberg M.S., Korner-Bitensky N., Becker R., Coopersmith H. 1989. “Destinations of Stroke Patients Discharged from the Montreal Area Acute-Care Hospitals.” Stroke 20: 351–56 [DOI] [PubMed] [Google Scholar]
- Rundek T., Mast H., Hartmann A., Boden-Albala B., Lennihan L., Lin I.F., et al. 2000. “Predictors of Resource Use After Acute Hospitalization: The Northern Manhattan Stroke Study.” Neurology 55: 1180–87 [DOI] [PubMed] [Google Scholar]
- Schlegel D., Kolb S.J., Luciano J.M., Tovar J.M., Cucchiara B.L., Liebeskind D.S., et al. 2003. “Utility of the NIH Stroke Scale as a Predictor of Hospital Disposition.” Stroke 34: 134–37 [DOI] [PubMed] [Google Scholar]
- Stillman G., Granger C., Niewczyk P. 2009. “Projecting Function of Stroke Patients in Rehabilitation Using the AlphaFIM Instrument in Acute Care.” Physical Medicine & Rehabilitation 1: 234–39 [DOI] [PubMed] [Google Scholar]
- Stroke Unit Trialists' Collaboration 2007. Organised In-patient (Stroke Unit) Care for Stroke (Review). Cochrane Database of Systematic Reviews 4. Art. no.: CD000197. doi:10.1002/14651858.CD000197.pub2 [Google Scholar]
- Teasell R.W., Foley N.C., Bhogal S.K., Chakravertty R., Bluvol A. 2005. “A Rehabilitation Program for Patients Recovering from Severe Stroke.” Canadian Journal of Neurological Sciences 32: 512–17 [DOI] [PubMed] [Google Scholar]
- Treger I., Ring H., Schwartz R., Tsabari R., Bornstein N.B., Tanne D. 2008. “Hospital Disposition After Stroke in a National Survey of Acute Cerebrovascular Diseases in Israel.” Archives of Physical Medicine and Rehabilitation 89: 435–40 [DOI] [PubMed] [Google Scholar]
- van Swieten J.C., Koudstaal P.J., Visser M.C., Schouten H.J., van Gijn J. 1988. “Interobserver Agreement for the Assessment of Handicap in Stroke Patients.” Stroke 19: 604–7 [DOI] [PubMed] [Google Scholar]
- Wade D.T. 2003. “Selection Criteria for Rehabilitation Services.” Clinical Rehabilitation 17: 115–18 [DOI] [PubMed] [Google Scholar]
- Willems D., Bryant D., O'Callaghan C. 2009. “Determining the Need for In-patient Rehabilitation Services Post Stroke in Southwestern Ontario: Inter-Rater Reliability of a Screening Tool.” Stroke 40(4): e236 [Google Scholar]