Abstract
Background
Treatment decisions should be based on patients' goals of care to provide an ethical, patient-centered framework for decision-making.
Objectives
The purpose of this study is to improve our understanding about how patients' and surrogates' goals of care are communicated and interpreted in an MICU.
Methods
One hundred patients admitted to an MICU, or their surrogates, responded to an open-ended question about goals of care for their hospitalization followed by a closed-ended question regarding their most important goal of care. Investigators interpreted participants' open-ended responses and compared these interpretations with participants' closed-ended, most-important-goal selections.
Results
Investigators' interpretations of participants' open-ended goals of care responses matched participants' closed-ended most important goal of care in only 28 of 100 cases. However, there was good inter-rater reliability between investigators in their interpretation of participants' open-ended responses, with agreement in 78 of 100 cases.
Conclusions
Clinicians should be cautious in interpreting patients' or surrogates' responses to open-ended questions about goals of care. A shared understanding of goals of care may be facilitated by alternating open-ended and closed-ended questions to clarify patients' or surrogates' responses.
Keywords for Indexing: Health Communication, Intensive Care Units, Patient Care Planning, Goals of care, Ethics
Introduction
Approximately 20% of Americans receive intensive care unit (ICU) services at the end of life, and based on aging demographics it is anticipated that ICU use will continue to rise – with a doubling of demand by 2030.1 With this in mind, the need for good communication with patients admitted to the ICU, and with their families, is only increasing in importance. Communication must be open and honest to ensure patients and families have optimal participation in decision-making.2 However, communication in an ICU setting is challenging due to barriers such as the highly charged emotional environment wherein patients and family members may be anxious or depressed and the clinical context in which the care team may not have a prior relationship with the patient.3
Goals of care are an important component of discussions about medical interventions.4 Incorporating the patient's goals of care into discussions, along with efforts to clarify the diagnosis and prognosis, allows for a reasoned and directed approach to decision making about specific interventions.5 It also reduces the risk of inappropriately basing medical decisions on a ‘technological imperative’6 that assumes a treatment should be used because it is available, rather than because it is likely to help patients reach the goals of care that are most important to them. Furthermore, by incorporating the patient's goals of care in medical decision-making it becomes more apparent why a particular clinical decision is ethically justifiable.5
Researchers have examined various methods to encourage communication, including incorporating goals of care in discussions between patients, families and their ICU healthcare team. Examples of these methods include a structured communication system,7 dialogues,3 and techniques to recognize and maneuver through the barriers of communication.8 Despite the work done to increase the amount of communication in the ICU, little research has been done to explore the quality of communication between clinicians and families in the ICU.9
In an effort to understand how incorporating goals of care can improve discussions about medical decisions, a series of research projects using differing patient populations was initiated. The first project studied a population of general medical patients and investigated code status preference and goals of care.10 A second study investigated goals of care that are most important to patients and surrogates in the ICU setting.11 The current study draws from qualitative and quantitative data that were collected from the ICU investigation.
The purpose of this study is to improve our understanding about how patients and surrogates communicate their goals of care in an ICU setting and how their responses may be interpreted by clinicians.
Methods
Setting, participants, and interviews for original data collection
The current study uses qualitative and quantitative methods to analyze data originally collected during a study described in detail by a previous article.11 Institutional Review Board approval was received (IRB-01 study ID # 200809732). The study population consisted of adult patients or their legally-authorized surrogate decision makers who were admitted in the Medical Intensive Care Unit (MICU) of a large Midwestern academic medical center. An investigator approached patients who were alert, able to communicate, and able to understand the informed consent process. In the event that a patient was unable to provide consent (due, for example, to being unconscious or intubated), their legally authorized surrogate was invited to participate on behalf of the patient. Some patients and surrogates were not approached if participation was deemed inappropriate (due, for example, to patients having unstable conditions or undergoing withdrawal of life support). Other exclusion criteria included: 1) patients or surrogates who were unable to speak English; 2) patients who were currently incarcerated; 3) patients who were admitted to the MICU for attempted suicide or pharmacological desensitization; and 4) patients who had been in the MICU for less than 48 hours. For feasibility purposes, participants also had to be available for interviews during weekdays. A total of 100 participants, consisting of 20 patients and 80 surrogates, agreed to participate in this study. After completion of the informed consent process, interviews were conducted at the bedside or in a private location in the MICU, or (for some surrogates) by phone.
Survey instrument for original data collection
A member of the research team, who was a pulmonary/critical care post-graduate fellow, used a survey instrument previously developed for general medicine patients and modified for use in the MICU setting. The survey instrument provided a verbatim guide for the interviewer and included both open-ended and closed-ended questions regarding patients' goals of care. For the purposes of this study, we focused on only one open-ended question and one closed-ended question. The first open-ended question asked: “Please tell me what your goals of care are for your (or your loved one's) treatment in the hospital.” If the participant did not seem to understand this question, then a follow-up question was posed: “What are you expecting will be accomplished by your (or your loved one's) treatment in the hospital”? All responses to the open-ended questions were recorded in writing in real time by the interviewer.
For the closed-ended questions, study participants were presented with a list of the six goals and asked if each goal was relevant to them (or their loved one) during the current hospitalization. The goals presented to the participants were derived from a structured literature review12 and consisted of the following: to be cured; to live longer; to improve/maintain current health (or quality of life and independence); to be comfortable; to achieve life goals (such as accomplishing something particular in life); and to provide support for family/caregivers. Participants were also offered a choice of ‘other’. If ‘other’ was selected, the participants were asked to explain their ‘other’ goals. Participants were then asked to specify which selected goal was the most important.
Chart review for original data collection
Patients' medical records were reviewed at the time of the interviews to collect demographic information, including age, race and Acute Physiology and Chronic Health Evaluation II (APACHE II) scores, which were used as an indicator of illness severity.
Analysis for the current study
An interdisciplinary team of investigators conducted the qualitative analysis, consisting of a nurse, a research associate with several years of goals of care research experience, and a physician. The investigators were blinded to the participants' closed-ended selections regarding their most important goal of care as well as demographic and medical information until after the categorization process was complete.
It is important to note that there is a contrast between the six closed-ended goal categories that we presented to participants in the MICU study and the seven goal categories we used to categorize the participants' open-ended responses. The validation of the structured literature review,13 which resulted in the addition of a seventh goal of care ‘understanding of patient's diagnosis/prognosis’, was conducted while the original MICU data collection was still in progress. Given the importance of this goal based on the results of the validation study, we elected to include it in the data analysis. We did not expect to find concordance between open-ended responses that were categorized by investigators as ‘understanding of patient's diagnosis/prognosis’ and participants' closed-ended selections specifying their most important goal of care since this ‘diagnosis/prognosis’ category was not provided to patients/surrogates as a closed-ended option during the MICU study and would have arisen only if a patient/surrogate mentioned it spontaneously as an ‘other’ goal.
Using seven goals of care categories, two of the investigators independently selected the one goal of care category that was deemed most representative of the participants' open-ended response to either the initial question (“Please tell me what your goals of care are for your (or your loved one's) treatment in the hospital”) or the follow-up question (“What are you expecting will be accomplished by your (or your loved one's) treatment in the hospital”?). The two investigators' categorizations were assessed for inter-rater reliability. In the event consensus on categorization was lacking, a third investigator was consulted to adjudicate responses so that a final consensus categorization could be used to determine the degree of matching between participants' closed-ended selection of their most important goal of care and the investigators' consensus categorization of participants' open-ended goal of care. Figure 1 summarizes the study design.
Figure 1.
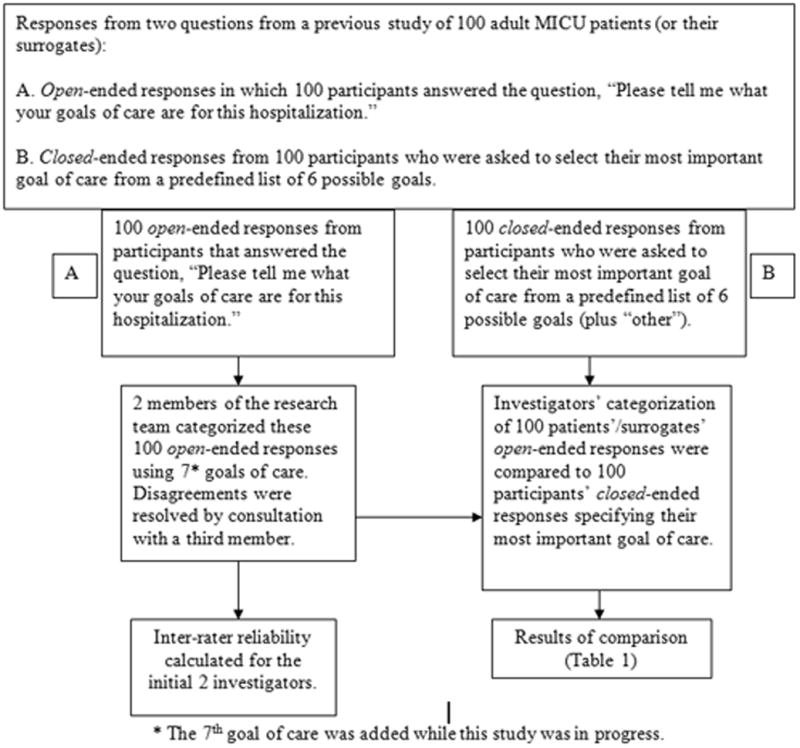
Summary of study design
For quantitative analysis, SAS Version 9.2 (SAS Institute Inc., Cary, NC) was used to calculate frequency statistics, and Fisher's exact test of significance was used for analysis due to small cell sizes. Differences were considered statistically significant at the p<0.05 level.
Results
Participant characteristics
A complete description of participant characteristics has been reported previously.11 Basic demographic and medical information about the study participants includes the following: interviewees were patients (20%) and surrogates (80%); patients were women (51%) and men (49%); and patients had a mean age of 58.1 years (range 18-89). Surrogates were related to patients as spouses (49%), adult children (22%), parents (11%), siblings (10%), legal guardians (2%), persons with durable power of attorney for health care (2%), nephews (2%), and friends (2%). The race/ethnicity of participants was White (95%), Black (2%), Hispanic (2%), and Native American (1%). The mean APACHE II score for patients was 22.5 (range 7-43), indicative of a mortality risk of approximately 40%.14
Participants' ability to respond to open-ended questions
Eighty-eight percent of the study participants were able to answer the open-ended question “Please tell me what your goals of care are for your (or your loved one's) treatment in the hospital.” The remaining 12% were able to answer the follow-up question used for clarification without further prompting.
Analysis of participants' closed-ended selection
The frequencies of patients' and surrogates' closed-ended selections of most important goals of care (alongside investigators' consensus categorizations of participants' open-ended responses) are shown in Table 1. There were statistically significant differences between the frequency of the most important goals of care selected by patients versus surrogates (p=.0008). Patients were most likely to select ‘accomplishing life goals’, ‘improving/maintaining health’, and ‘supporting family/caregiver’. Surrogates were most likely to select ‘cure’, improving/maintaining health, and comfort. Investigators were most likely to select ‘improving/maintaining health’, based upon their categorization of participants' open-ended responses.
Table 1. Frequencies of most important goals of care selections among patients and surrogates, and goals of care categorizations by investigators.
| Goal of Care Affirmed | Patients' closed-ended selections (N=20)* |
Surrogates' closed-ended selections (N=80)* |
Investigators' consensus categorizations of participants' open-ended responses |
|---|---|---|---|
| Cure | 1 (5%) | 24 (30%) | 11 |
| Live longer | 0 (0%) | 5 (6%) | 7 |
| Improve/maintain health | 5 (25%) | 24 (30%) | 60 |
| Make comfortable | 1 (5%) | 14 (18%) | 11 |
| Accomplish life goals | 8 (40%) | 8 (10%) | 6 |
| Provide support for family/caregivers | 3 (15%) | 4 (5%) | 0 |
| Understanding diagnosis/prognosis | 5 | ||
| Other OR all equally important | 2 (10%) | 1 (1%) | 0 |
A significant difference (p=.008) is noted between the frequency of patient and surrogates closed-ended selections.
No significant differences were found with respect to most important goals of care selections based on patient gender (p=.56), APACHE II score dichotomized at the mean (p=.48), or when, among surrogates, comparing spousal and non-spousal surrogates (p=.23). There was not enough diversity in the study sample to assess for differences based on race/ethnicity.
Categorization of the participants' open-ended responses
There was generally a high level of inter-rater reliability between the two investigators in their categorization of the participants' responses to the open-ended questions (Fleiss kappa scores ranged from 0.6 – 1.0, with the exception of the categorization of “be cured”, which had a kappa score of 0.4). Overall, there was 78% agreement between the two investigators (78 out of 100 cases).
Comparison of investigators' consensus categorization of participants' open-ended responses and participants' closed-ended responses
In contrast to the high level of inter-rater reliability, investigators' consensus categorizations of participants' open-ended responses did not match very well to the participants' closed-ended selections of their most important goal of care. There was only 28% agreement between the investigators' consensus categorizations and the participants' closed-ended selections (28 of 100 cases). Venn diagrams (Figure 2) illustrate the generally poor degree of overlap between the investigators' consensus categorizations of participants' open-ended responses and the participants' closed-ended selections of their most important goal of care. When evaluating patients and surrogates separately, there was greater overlap of investigators' consensus categorizations with surrogates' closed-ended selections (25/80, or 31% matching) than with patients' closed-ended selections (3/20, or 15% matching).
Figure 2.
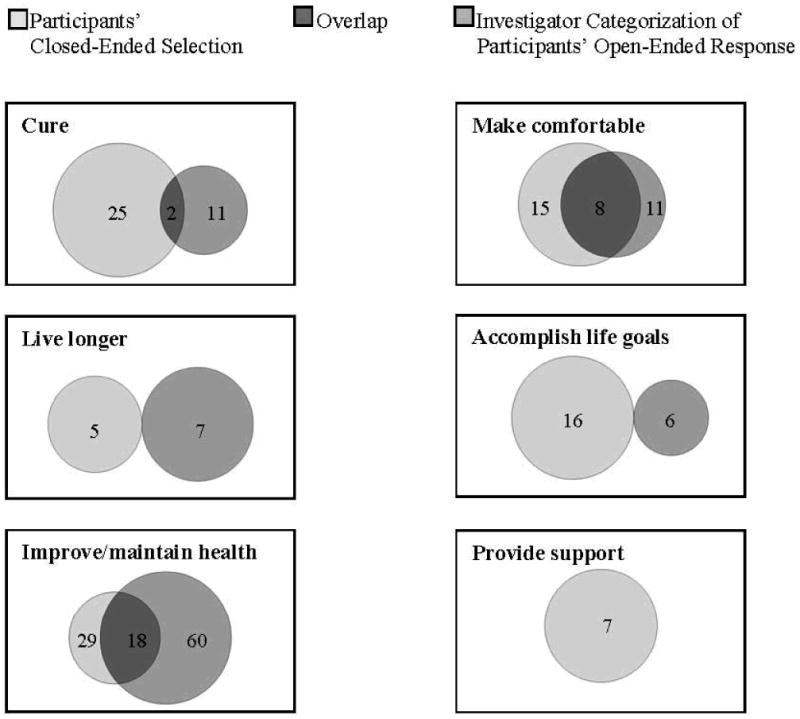
Venn diagrams of participants' closed-ended selections of most important goals of care and investigators' categorizations of participants' open-ended goals of care responses.
Examples of investigators' consensus categorizations of participants' open-ended goals of care responses, alongside participants' closed-ended selections of their most important goal of care, are presented in Table 2. Examples demonstrate both instances of concordance and discordance between investigators and participants.
Table 2. Examples of participants' open-ended goals of care statements followed by instances of concordant and discordant pairs of participants' closed-ended selections of most important goal of care and investigators' consensus categorizations of the open-ended goals of care statements.
| Patient/surrogate open-ended statement | Patients'/surrogates' closed-ended selection of most important goal of care | Investigators' consensus categorization of patients'/surrogates' open-ended response |
|---|---|---|
| Concordant Pairs | ||
| “Get the yeast infection (in the blood) cleared up, get her healthy enough for transplant, and get her home where she can lead a long life.” | Cure | Cure |
| “Don't know what to expect.” “To not prolong his situation and not allow him to suffer.” | Comfort | Comfort |
| “Get well and get out of here.” | Improve/maintain health | Improve/maintain health |
| Discordant Pairs | ||
| “to be cancer free” | Accomplish life goals | Cure |
| “To follow whatever the doctor sets up for me and to be active on my farm again.” | Provide support for family and caregivers | Achieve life goals |
| “Mobility, feeling well, apartment living again.” | Comfort | Improve/maintain health |
| “Comfortable, careful medical attention and support, and deal with any psychological factors.” | Improve/maintain health | Comfort |
| ”To get her back on her feet again and recognize who I am.” | Cure | Improve/maintain health |
| “My goal is to cooperate with the doctors 100% until they tell me there is no more hope.” | Improve/maintain health | Live longer |
Discussion
To our knowledge, this is the first study examining patient and surrogate responses to open- and closed-ended questions about goals of care. Our findings demonstrate that there was a high level of inter-rater reliability between the two investigators in their categorization of the participants' open-ended goals of care responses. But our findings also reveal that investigator categorizations of participants' open-ended responses did not match very well to participants' closed-ended selections of their most important goals of care. This suggests that it may be difficult for clinicians to accurately identify patients' or surrogates' goals of care based only on their interpretation of responses to open-ended questions.
The lack of a good match between investigators' categorizations of participants' open-ended responses and participants' own selections of their most important goals of care warrants consideration. In the context of this study, such a mismatch could occur for a variety of reasons. First of all, participants' responses to the open-ended question may have represented an initial response that did not actually represent the response they would give after further reflection. Since the closed-ended responses were solicited after the open-ended questions, it may be the case that participants' closed-ended responses represented their more considered judgments. Another potential source of misunderstanding may have arisen from the way in which the participant ‘voiced’ their open-ended response due to difficulty expressing their thoughts in the ICU setting. For example, four participants expressed versions of “get me out of here” as the goal of care, which were interpreted by the investigators as meaning the goal of improving function enough to be discharged from the ICU. However, each of these four participants had different closed-ended responses when asked about their most important goal of care, ranging from ‘cure’ to ‘comfort’ to ‘improve/maintain health’ to ‘achieve life goal’.
A third source of misunderstanding might have arisen from the way in which investigators ‘heard’ participants' open-ended responses. In categorizing participant responses to open-ended questions, investigators may have been tuned in to key words that would serve as a signal for the participant's primary goal of care. For example, in three cases terms such as “get infection out”, “back to 150%” and “cancer-free” were interpreted by the investigators as the participants' desire for cure. However, these three participants identified non-cure goals of care in their closed-ended selections--‘comfort’, ‘improve or maintain health’ and ‘achieve life goal’, respectively. Our findings suggest that it is important to recognize that commonly used words may not be directly translatable into goals of care categories. Therefore, it is vital for clinicians to continue to probe for clarification in an effort to reach a shared understanding of goals of care.
This probing may be accomplished by the use of alternating open and closed-ended questions to clarify the goals of care between the patient and clinician. Imagine, for instance, that a patient is admitted to the hospital with an exacerbation of congestive heart failure and a clinician asks, “So that we can know how best to care for you, could please tell me what your goals of care are for your treatment in the hospital?” The patient replies, “I want to get back to 100%.” The clinician probes for clarification by asking, “So that I can be sure I understand, can you tell me more about what it means for you to get back to 100%?” The patient replies further by saying, “I want my health to get back to normal.” The clinician then asks, “Are you saying that your goal is to be cured of your heart problem, or do you mean that you want to get back to the level of function you had before coming to the hospital?” This way allows the patient to articulate their own goals in their own words while also encouraging them to identify specific goals of care that are reflective of their expectations and are also understood by clinicians. The alternating movement between open and closed-ended questions should lead to better understanding between the patient and clinician and, it is hoped, to a more patient-centered process of decision making.
Our study also suggests that there may be differences between the goals of care emphasized by patients compared with their surrogates. For instance, surrogates in our study were more likely to emphasize cure and the improvement of health, whereas patients were more likely to stress the importance of accomplishing life goals. Though our study did not compare patients and surrogates with respect to their respectively voiced goals of care within given patient-surrogate dyads, if the differences in frequencies between patients' and surrogates' goals of care that we found are representative, these differences may bear some relation to findings from a meta-analysis showing that surrogates incorrectly predicted the end-of-life treatment preferences of their loved ones about one-third of the time.15 If the basic principle of surrogate decision making is that the surrogates should articulate decisions on the basis of their understanding of patients' values, wishes, and goals (rather than their own)15, then any indication that surrogates may not understand their patients' values, wishes, or goals should be taken seriously. In the same way that surrogates may not understand patients' treatment preferences, surrogates may also at times not understand patients' goals of care. Patients and surrogates should be encouraged to talk about their goals of care before mentally-incapacitating illnesses occur so that the risk of misunderstandings can be reduced.
Our study had limitations. First, we did not include “understanding of patient's diagnosis/prognosis” as a closed-ended option when asking participants about their most important goal of care, since this goal was introduced while the data gathering for this study was in progress. Second, this study was conducted in a single MICU. Third, certain disease categories (postoperative complications, cardiovascular disease and trauma) were underrepresented despite a wide range of critical illnesses.11 Fourth, there was limited ethnic and racial diversity among the participants. Fifth, there were fewer patients (n=20) than surrogates (n=80), though this unequal balance reflects the reality that patients are often unable to participate in decision-making in the ICU setting.16 Lastly, investigators were blinded to the clinical context of the patients and therefore did not know clinically relevant information about the patients involved (diagnosis, severity of illness, and prognosis), information which would be expected to influence the way clinicians actually interpret patients' and surrogates' responses during real goals of care discussions.
Conclusions
Our findings suggest that clinicians should exercise caution in interpreting patients' or surrogates' responses to open-ended questions about their goals of care, at least until those responses have been clarified and confirmed through appropriate dialogue. As demonstrated by our results, a mixed method of communication may be needed to elicit a patient's goals of care accurately, using open-ended and closed-ended approaches to complement each other. One can think of this process as an attempt to facilitate a genuine goals of care dialogue in the true meaning of that word. “Dialogue” is derived from the Greek prefix dia, meaning “through, thoroughly, entirely,” and legein, which means “speak”.17
Clarification of goals of care is particularly important in an ICU setting which has inherent challenges. As suggested by our study, misunderstandings may occur because of the timing of a response (before or after a patient or surrogate has had time to reflect on the situation), because of the particular way a patient or surrogate voices a goal, or because of the way a clinician hears a response. This study demonstrates the importance of alternating open-ended and closed-ended questions to elicit and clarify patients' and surrogates' goals of care, thus resulting in a truly dialogical approach to communication which may lead to a shared understanding of the patient's or surrogate's goals of care, as illustrated in Figure 3. The open and closed-ended questions used in this study can be used by clinicians as starting points in developing a dialogue.
Figure 3.
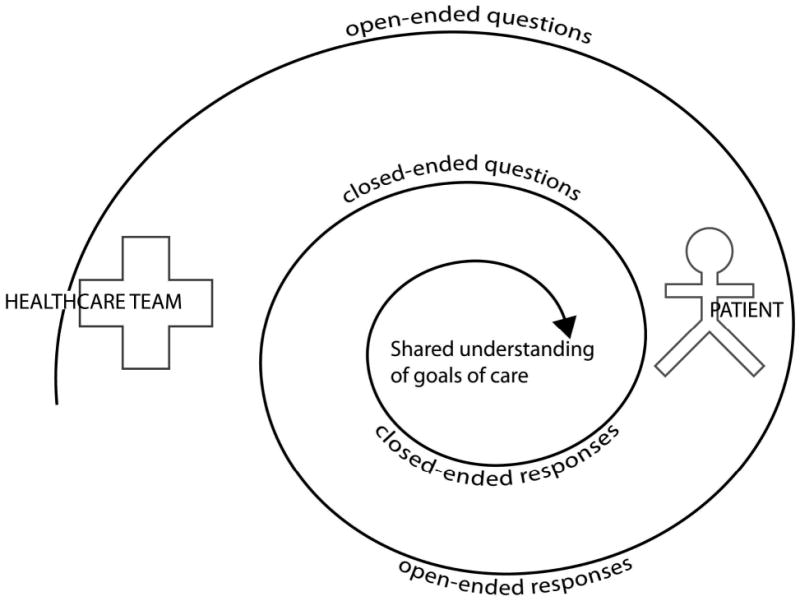
Changing the anatomy of goals of care dialogue.
Acknowledgments
This publication was made possible by Grant Number TL1RR024981 (training support for DB) from the National Center for Research Resources (NCRR), a part of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CTSA or NIH.
The authors would like to thank Dr. Robert Orr and Dr. Sean Philpott for their thoughtful reviews of the manuscript during the process of preparation. The authors would also like to thank Kellie Bodeker-Goranson, MSHS, CCRC, for her assistance with Figure 3.
Contributor Information
Debra S. Brandt, The University of Iowa College of Nursing and Institute for Clinical and Translational Science, The University of Iowa
Laura A. Shinkunas, Program in Bioethics and Humanities, University of Iowa Carver College of Medicine, The University of Iowa
Thomas G. Gehlbach, Pulmonary and Critical Care Medicine, Dean Clinic
Lauris C. Kaldjian, Department of Internal Medicine and Program in Bioethics and Humanities, University of Iowa Carver College of Medicine, The University of Iowa
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 2.Kinlaw K. Ethical issues in palliative care. Semin Oncol Nurs. 2005;21(1):63–68. doi: 10.1053/j.soncn.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Levin TT, Moreno B, Silvester W, Kissane DW. End-of-life communication in the intensive care unit. Gen Hosp Psychiatry. 2010;32(4):433–442. doi: 10.1016/j.genhosppsych.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Emanuel L, Scandrett KG. Decisions at the end of life: have we come of age? BMC Med. 2010;8:57. doi: 10.1186/1741-7015-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaldjian LC. Teaching practical wisdom in medicine through clinical judgment, goals of care, and ethical reasoning. J Med Ethics. 2010;36(9):558–562. doi: 10.1136/jme.2009.035295. [DOI] [PubMed] [Google Scholar]
- 6.Orr RD, Meilaender G. Ethics & life's ending: an exchange. First Things. 2004;145:31–38. [PubMed] [Google Scholar]
- 7.Daly BJ, Douglas SL, O'Toole E, et al. Effectiveness trial of an intensive communication structure for families of long-stay ICU patients. Chest. 2010;138(6):1340–1348. doi: 10.1378/chest.10-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiner JS, Roth J. Avoiding iatrogenic harm to patient and family while discussing goals of care near the end of life. J Palliat Med. 2006;9(2):451–463. doi: 10.1089/jpm.2006.9.451. [DOI] [PubMed] [Google Scholar]
- 9.Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin. 2004;20(3):363–380. doi: 10.1016/j.ccc.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Kaldjian LC, Erekson ZD, Haberle TH, et al. Code status discussions and goals of care among hospitalised adults. J Med Ethics. 2009;35(6):338–342. doi: 10.1136/jme.2008.027854. [DOI] [PubMed] [Google Scholar]
- 11.Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139(4):802–809. doi: 10.1378/chest.10-1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Goals of care toward the end of life: a structured literature review. Am J Hosp Palliat Care. 2009;25(6):501–511. doi: 10.1177/1049909108328256. [DOI] [PubMed] [Google Scholar]
- 13.Haberle TH, Shinkunas LA, Erekson ZD, Kaldjian LC. Goals of care among hospitalized patients: a validation study. Am J Hosp Palliat Care. 2010 Nov 21; doi: 10.1177/1049909110388505. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 15.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166(5):493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 16.Arnold RM, Kellum J. Moral justifications for surrogate decision making in the intensive care unit: implications and limitations. Crit Care Med. 2003;31(5 Suppl):S347–353. doi: 10.1097/01.CCM.0000065123.23736.12. [DOI] [PubMed] [Google Scholar]
- 17.Harper D. [Accessed March 28, 2011];Online Etymology Dictionary. http://www.etymonline.com/index.php?term=dia-


