Abstract
Numerous medical and psychiatric conditions can cause agitation; some of these causes are life threatening. It is important to be able to differentiate between medical and nonmedical causes of agitation so that patients can receive appropriate and timely treatment. This article aims to educate all clinicians in nonmedical settings, such as mental health clinics, and medical settings on the differing levels of severity in agitation, basic triage, use of de-escalation, and factors, symptoms, and signs in determining whether a medical etiology is likely. Lastly, this article focuses on the medical workup of agitation when a medical etiology is suspected or when etiology is unclear.
INTRODUCTION
Agitation is an extreme form of arousal that is associated with increased verbal and motor activity. These symptoms are caused by a variety of etiologies, both medical and psychiatric. Patients with agitation may present not only to an emergency department (ED) or a psychiatric emergency service (PES), but also to a clinic or acute care center that does not have the onsite medical resources of a physician or midlevel practitioner, such as a community mental health facility (termed nonmedical facility).
This article is one of a set of companion articles to address Best practices in the Evaluation and Treatment of Agitation in the emergency setting, Project BETA.1
LEVEL OF AGITATION
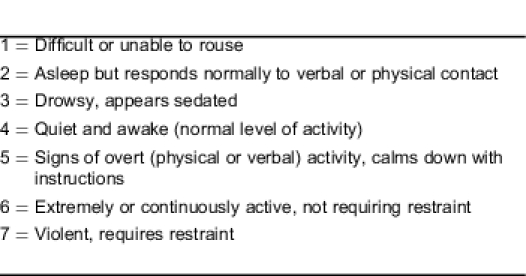
Various assessments of agitation are available to determine the patient's level of agitation, such as the Overt Agitation Severity Scale2 or Overt Aggression Scale.3 Another scale is the Behavioural Activity Rating Scale or BARS (Table 1).4 The American Association for Emergency Psychiatry does not consider one agitation rating scale to be better than another, although we find the BARS is easy to use reliably, even for one not trained in psychiatry or emergency medicine. The BARS was created to help assess agitation in pharmaceutical study trials. It is simple to use and does not require the participant/patient to answer questions.4 This scale is especially useful in the nonmedical setting, where decisions are made by those who are not medically trained.
Table 1.
Behavioural Activity Rating Scale.4
TRIAGE OF THE AGITATED PATIENT
Nonmedical Setting
When an agitated patient presents to a clinic without a medical team, the immediate task is to determine if the patient needs transfer to a higher level of care. This determination is based on whether a medical etiology is suspected by history or obvious signs and symptoms, as listed in Table 2, and on the patient's level of agitation. Algorithm 1 illustrates this process (Figure 1).
Table 2.
Findings that require immediate evaluation by a clinician.
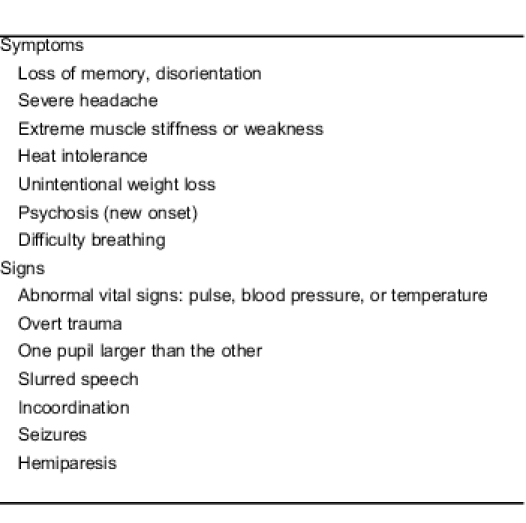
Figure 1.
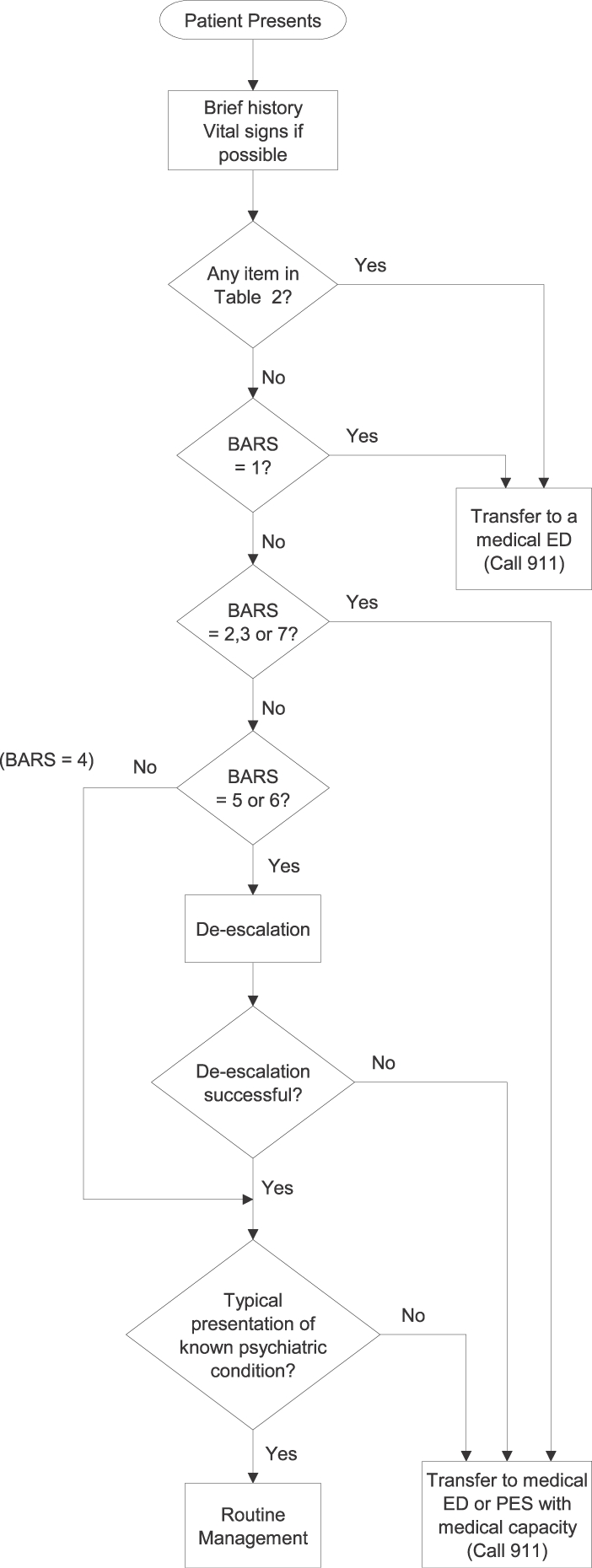
Evaluation in a nonmedical setting. BARS, Behavioural Activity Rating Scale; ED, emergency department; PES, psychiatric emergency service.
For any patient with signs or symptoms listed in Table 2 or with BARS score of 1, immediate transfer to a medical ED is indicated. Patients with a BARS score of 2, 3, or 7 should be transferred immediately to either a medical emergency department or a PES with medical capability. In the case of the highly agitated patient, transfer to an emergency service should happen quickly. For mild to moderate agitation (BARS = 5 or 6), the patient may be calmed with verbal de-escalation techniques, and environmental modification. If this is successful, further evaluation at the clinic is acceptable. For patients who do not respond, transport to an acute care facility, such as an ED or PES, is indicated. To protect the patient and staff, emergency medical services or ambulance should be contacted through 911 or a similar emergency system. The ED or PES should be notified before patient arrival to ensure that the staff is ready to receive the patient. The receiving facility needs to have a room, crash cart, and adequate number of staff ready to meet the ambulance on arrival.
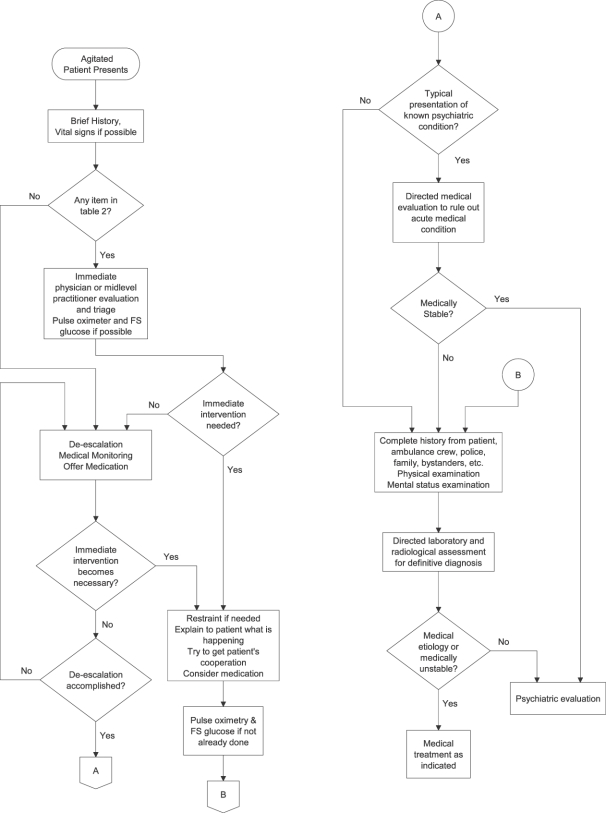
Medical Setting
Management of the agitated patient in the medical setting is illustrated in algorithm 2 (Figure 2). When triaging an agitated patient in the medical setting, a brief history and vital signs should be obtained if possible. If any item in Table 2 is found or suspected at initial intake triage, immediate evaluation by a clinician is indicated. Oxygenation level and blood sugar level should also be obtained if possible. The initial examination should be directed at identifying factors (Table 3) that could indicate serious, possibly life-threatening, conditions such as listed in Table 4. These, as well as other conditions that may be discovered after a more complete examination, are discussed in detail below. Unless immediate intervention is indicated, de-escalation should be attempted in an effort to gain the patient's cooperation. Likewise, if initial intake assessment does not point to items in Table 2, de-escalation should be attempted so that the patient can better participate in evaluation.
Figure 2.
Medical evaluation in the emergency department or psychiatric emergency service. FS glucose, finger-stick glucose.
Table 3.
Factors that could indicate serious, possibly life-threatening, conditions.
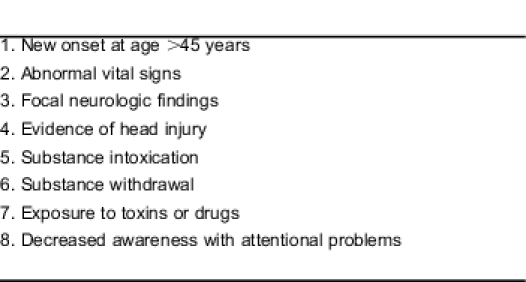
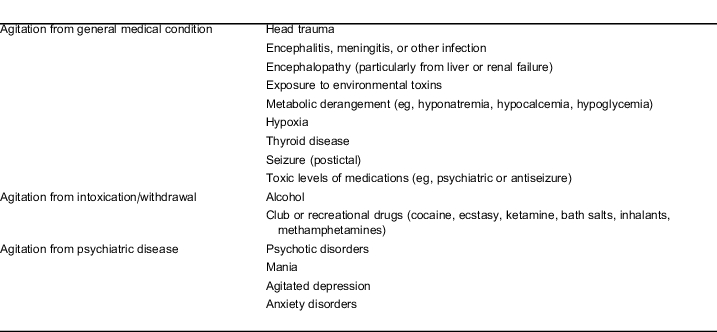
Table 4.
Conditions that may cause agitation.
As visualized in algorithm 2 (Figure 2), the agitated patient may, at any point during the medical evaluation, require medication, restraint, and increased behavioral support. For patients with high-risk indicators for a medical etiology of agitation, listed in Table 3, de-escalation may have to be interrupted and physical restraint may be needed to save the patient's life. Likewise, severely agitated patients who may not be cooperative are at risk for violent behavior and, thus, require restraint if de-escalation is impractical or ineffective. If a patient must be restrained, oxygenation level and finger stick blood glucose should be done immediately if previously it could not be obtained.
Although not fully illustrated in the algorithm, the complete history and physical examination of the patient may have to be interrupted to address the treatment of the patient's agitation, and will need to be resumed after the patient is less agitated. The patient may need treatment to reduce the level of agitation without having a definitive diagnosis. The goal of medication is to calm the patient enough to allow for a thorough evaluation.
Once de-escalation is accomplished, an important triage decision is to determine if the patient has a known psychiatric illness and if the presentation is typical of that illness. If so, the patient should have a directed medical evaluation to rule out an acute medical problem. If none is present, psychiatric evaluation and management are indicated. All other patients should have a complete history, physical examination, and mental status examination followed by directed laboratory and radiologic assessment to determine the definitive diagnosis.
OVERVIEW OF MEDICAL EVALUATION
During the time the patient is being behaviorally stabilized, the ambulance crew, police, family, friends, relatives, and nursing home personnel should be interviewed to obtain a history or collaborative information. According to Olshaker and colleagues,5 the patient history has a sensitivity of 94% and the physical examination has a sensitivity of 51% for detecting medical problems during the evaluation of psychiatric patients.
The history and physical examination can lead to clues that a nonpsychiatric etiology of agitation may be responsible for the presentation. If a patient presents with known psychiatric disease that is inconsistent with previous presentations, a medical etiology should be suspected. New onset of agitation in a person older than 45 years with no psychiatric history would suggest a medical etiology, since most psychiatric disorders have an earlier onset.
Abnormal vital signs, abnormal physical examination results, overt signs of alcohol or drug intoxication or withdrawal,6 evidence of exposure to toxins,7,8 and decreased awareness with attentional problems9 are all indicative of a medical etiology. Neurologic problems must also be considered. Head injury10 or a history of disease that can cause neurologic changes,7 such as history of stroke,11 cancer, parkinsonism, and multiple sclerosis, would also indicate that the agitation has a medical etiology.
As previously mentioned, decreased awareness and attentional problems are very important because these are signs and symptoms of delirium, which can be subtle and frequently overlooked. Delirium can be defined as a disturbance in level of awareness and reduced ability to direct, focus, sustain, or shift attention and a change in cognition, such as deficits in orientation, executive ability, language, visuoperception, learning, and memory.12 Careful assessment is most important because delirium indicates an underlying medical etiology.
Agitation can be due to a general medical condition,9,13 intoxication and withdrawal,6 and decompensated psychiatric disease. Medical conditions include head trauma;10 infection7 leading to meningitis, encephalitis,14 or sepsis; encephalopathy, usually from renal or liver failure; hypoxia; metabolic derangement;7 thyroid disease;15 toxic levels of psychiatric or antiseizure medications;8 and exposure to environmental toxins.7 Alcohol or other drug intoxication or withdrawal6 is a common source for agitation. Conditions that must be considered when evaluating the agitated patient are listed in Table 4.
For those in the nonmedical setting, the only evidence of these at triage may be agitation, disorientation, abnormal vital signs, signs of trauma, odor of alcohol, and history of substance use. Presence of these signs and symptoms usually indicate that a medical evaluation is indicated to determine if a reversible etiology of the agitation needs to be addressed. Conditions can be life-threatening if not treated quickly. Many of the specific symptoms or signs related to medical conditions that cause agitation can be elicited after obtaining a directed history and observing the patient (Table 2). If any of these conditions are suspected, the patient will need a complete physical examination by a physician or midlevel practitioner and must be transferred to an emergency department for medical evaluation.
MAJOR CATEGORIES OF ETIOLOGY OF AGITATION
Agitation from a General Medical Condition
When a person has head trauma, there will often be history given of the incident. Bleeding or contusions may be visible. The person might complain of headache, memory loss, or loss of consciousness. There may be physical signs such as abnormal vital signs, one pupil being significantly larger than the other, slurred speech, or other motor problems. With encephalitis14 or encephalopathy, the person may have an altered mental state in the form of confusion or agitation, may exhibit inattentiveness and impaired judgment, and may exhibit new physical symptoms, such as motor incoordination, seizures, or hemiparesis. Fever, headache, or stiffening of the neck are concerning symptoms.14 A generalized, systemic infection will usually cause a fever (this might not be present in an immunocompromised patient). With sepsis, there may be a high fever, possible seizures, disorientation, and agitation.7 Hallucinations can also occur, especially visual. In fact, visual hallucinations are a common symptom in delirium, especially in elderly patients.16,17 Exposure to environmental toxins can cause a wide variety of symptoms, depending on the toxin. Clues often come from the history. Symptoms are often nonspecific and related to a toxic metabolic disturbance; these symptoms include disorientation, somnolence, agitation,8 and seizures. If this is suspected, poison control should be contacted immediately. Metabolic derangements can cause encephalopathy, cardiac arrhythmias, mental status changes,7,16 hemiparesis, seizures, and abnormal neurologic findings on examination. Hypoglycemia and hyperglycemia,7 for instance, can lead to these symptoms, if left untreated, and are easily reversible. The same is true with hypoxia. Key signs that the patient is not receiving enough oxygen include changes in breathing pattern, difficult or rapid breathing, and an abnormal oxygen saturation level. Thyrotoxicosis may happen suddenly. Common symptoms include heat intolerance, recent unintentional weight loss, proximal muscle weakness, palpitations, and anxiety. This condition can progress to cardiac arrhythmias, agitation, psychosis, and even death if left untreated.15 Physical signs of thyrotoxicosis may include skin that is warm and moist to the touch, infrequent blinking or lid lag, and a failure to wrinkle the brow with an upward gaze. Vital signs are often abnormal with a marked tachycardia.18,19 If a person has recently had a seizure, the “postictal” state can leave the patient confused and agitated.20,21 When a person ingests toxic levels of psychiatric or antiseizure medications, disorientation, somnolence, or agitation may be the first symptoms. Certain psychiatric medications can lead to life-threatening syndromes such as neuroleptic malignant syndrome (NMS)22 and serotonin syndrome.23 In both of these cases, abnormal vital signs such as tachycardia, labile blood pressures, and fever are typically noted. In NMS, the patient has “lead pipe” rigidity whereas the patient with serotonin syndrome has myoclonus and hyperreflexia.
Agitation from Alcohol and/or Recreational Substance Intoxication or Withdrawal
A common reason for change in mental status is intoxication with drugs or alcohol or a patient in substance withdrawal.6 Getting a drug and alcohol history can add insight and help direct immediate care. In a young person presenting with agitation, without history of psychiatric illness, drug intoxication needs to be considered. It may be difficult to get a reliable history from the agitated, intoxicated patient. The only clues might be abnormal vital signs, odor of alcohol, and possibly drug paraphernalia on the person. If intravenous drug use is suspected, there may be evidence of drug injection, such as track marks on the arms or legs. For withdrawal syndromes, alcohol and benzodiazepine withdrawal are the most medically concerning. They can cause disorientation, agitation, hallucinations, as well as seizures.6 A person in severe withdrawal may also experience autonomic instability.6
Agitation from Psychiatric Disease
If no medical etiology is found for the agitation, the patient can be seen by mental health specialists. Causes of agitation may be related to psychosocial stressors or a primary psychiatric disorder. During an evaluation, history will be helpful in determining likely causes and aid in the intervention or focus of treatment. Any of the major psychiatric illnesses can manifest as agitation, including schizophrenia, agitated depression, or bipolar illness. Patients with a new psychiatric complaint or a presentation that is inconsistent with their prior psychiatric illness may require more intensive testing, as a medical cause may be more likely.
MEDICAL WORKUP
The medical workup of an agitated patient, as with any patient who presents to an ED or PES, begins with completion of the history, vital signs, physical examination, and diagnostic tests, if they are deemed necessary for the evaluation process.24 The physical examination should be a focused, unclothed, but gowned, examination of the patient that includes an assessment of the heart, lungs, abdomen, skin, and neurologic system. The patient presenting with abnormal behavior needs a full neurologic examination as well as adequate mental status examination. During this assessment, healthcare providers should attempt a provisional diagnosis of the most likely etiology of the agitation. The workup will then largely be guided by this provisional diagnosis.
Agitation from General Medical Condition
Agitation, in which a medical condition is strongly suspected, in which the patient has abnormal vital signs, or in which the patient has medical comorbidities, such as immunosuppressive disease or neurologic disease, requires a medical workup. The workup should be targeted to the underlying condition and may include directed laboratory analysis, neuroimaging, or lumbar puncture, as appropriate.
Agitation from Substance Intoxication or Withdrawal
The medical workup for these individuals may be variable. Young healthy adults with a good history of ingestion may be observed for withdrawal, especially from alcohol or benzodiazepines. A workup should be considered if the amount of ingestion is unknown or if there are symptoms or signs that suggest something more serious, such as alcohol poisoning. A more thorough workup, however, should be strongly considered for older adults with medical comorbidities or who are chronic substance abusers.
Undifferentiated Agitation
Agitation in this category (for which no provisional diagnosis can be assigned, or for which information is not immediately available) should be presumed to be from a general medical condition until proven otherwise. Workup should be targeted to any underlying conditions and may include laboratory analysis, neuroimaging, or lumbar puncture, as appropriate.
Agitation from Psychiatric Disease
If psychiatric disease is strongly suspected, but the patient has no previous history of psychiatric disease (or is younger or older than a typical patient with psychiatric disease), then the agitation should be presumed to be from a general medical condition until proven otherwise, as noted above. In a patient with preexisting psychiatric disease who presents with symptoms similar to his or her previous psychiatric disease, and with normal vital signs and normal mentation, little to no testing may be considered.
The routine examination should include a complete set of vital signs, blood glucose measurement (finger stick), and determination of oxygenation level, if not obtained during triage. The laboratory tests completed should be directed by likelihood of a medical illness causing or exacerbating the psychiatric presentation. Universal laboratory studies done without indication tend to be low yield25,26 and can increase healthcare costs.27 Evidence also shows that routine tests for a large population may find abnormalities that were not originally suspected but that have no clinical significance.28 On the other hand, patients without prior psychiatric history need a complete evaluation that may include detailed laboratory evaluation and radiographic imaging.29
CONCLUSION
The consensus of Project BETA members is as follows:
1. Routine laboratory testing is not indicated; rather, directed testing should be based on the most likely diagnosis. Workup of agitation from a general medical condition should be directed toward identifying most likely causes.
2. New-onset agitation should be presumed to be agitation from a general medical condition.
3. There should be a high level of suspicion of agitation from a medical condition in a patient with concerning past medical history, such as immunosuppression, or when onset is outside the normal age ranges of psychiatric disease.
Footnotes
Supervising Section Editor: Shahram Lotfipour, MD, MPH
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
REFERENCES
- 1.Holloman GH, Jr, Zeller SL. Overview of Project BETA: best practices in evaluation and treatment of agitation. West J Emerg Med. 2011;13:1–2. doi: 10.5811/westjem.2011.9.6865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopecky HJ, Kopecky CR, Yudofsky SC. Reliability and validity of the Overt Agitation Severity Scale in adult psychiatric inpatients. Psychiatr Q. 1998;69:301–323. doi: 10.1023/a:1022182114925. [DOI] [PubMed] [Google Scholar]
- 3.Silver JM, Yudofsky SC. The Overt Aggression Scale: overview and guiding principles. J Neuropsychiatry Clin Neurosci. 1991;3:S22–S29. [PubMed] [Google Scholar]
- 4.Swift RH, Harrigan EP, Cappelleri JC, et al. Validation of the behavioural activity rating scale (BARS): a novel measure of activity in agitated patients. J Psychiatr Res. 2002;36:87–95. doi: 10.1016/s0022-3956(01)00052-8. [DOI] [PubMed] [Google Scholar]
- 5.Olshaker JS, Browne B, Jerrard DA, et al. Medical clearance and screening of psychiatric patients in the emergency department. Acad Emerg Med. 1997;4:124–128. doi: 10.1111/j.1553-2712.1997.tb03718.x. [DOI] [PubMed] [Google Scholar]
- 6.Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World. 1998;22:5–12. [PMC free article] [PubMed] [Google Scholar]
- 7.Caplan LR. Delirium: a neurologist's view—the neurology of agitation and overactivity. Rev Neurol Dis. 2010;7:111–118. [PubMed] [Google Scholar]
- 8.Acute poisoning following ingestion of medicines: initial management: how to treat life-threatening complications and to evaluate the risk of delayed effects and psychological distress. Prescrire Int. 2010;19:284–291. [PubMed] [Google Scholar]
- 9.Mittal V, Muralee S, Williamson D, et al. Review: delirium in the elderly: a comprehensive review. Am J Alzheimers Dis Other Demen. 2011;26:97–109. doi: 10.1177/1533317510397331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciurli P, Formisano R, Bivona U, et al. Neuropsychiatric disorders in persons with severe traumatic brain injury: prevalence, phenomenology, and relationship with demographic, clinical, and functional features. J Head Trauma Rehabil. 2011;26:116–126. doi: 10.1097/HTR.0b013e3181dedd0e. [DOI] [PubMed] [Google Scholar]
- 11.Oldenbeuving AW, de Kort PL, Jansen BP, et al. Delirium in the acute phase after stroke: incidence, risk factors, and outcome. Neurology. 2011;76:993–999. doi: 10.1212/WNL.0b013e318210411f. [DOI] [PubMed] [Google Scholar]
- 12.American Psychiatric Association. 2011. http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=32 DSM-5 development: proposed definition of delirium. Available at. Accessed July 11.
- 13.Peisah C, Chan DK, McKay R, et al. Practical guidelines for the acute emergency sedation of the severely agitated older patient. Intern Med J. 2011;41:651–657. doi: 10.1111/j.1445-5994.2011.02560.x. [DOI] [PubMed] [Google Scholar]
- 14.Sarkari NB, Thacker AK, Bathwal SP, et al. Japanese encephalitis (JE), part I: clinical profile of 1,282 adult acute cases of four epidemics. J Neurol. 2011. published online ahead of print June 17. [DOI] [PubMed]
- 15.Burger AG, Philippe J. Thyroid emergencies. Baillieres Clin Endocrinol Metab. 1992;6:77–93. doi: 10.1016/s0950-351x(05)80332-5. [DOI] [PubMed] [Google Scholar]
- 16.Khurana V, Gambhir IS, Kishore D. Evaluation of delirium in elderly: a hospital-based study. Geriatr Gerontol Int. 2011;11:467–473. doi: 10.1111/j.1447-0594.2011.00710.x. [DOI] [PubMed] [Google Scholar]
- 17.Harris RL, Musher DM, Bloom K, et al. Manifestations of sepsis. Arch Intern Med. 1987;147:1895–1906. [PubMed] [Google Scholar]
- 18.Bahn RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract. 2011;17:456–520. doi: 10.4158/ep.17.3.456. [DOI] [PubMed] [Google Scholar]
- 19.Melish JS. Thyroid disease. In: HK Walker, WD Hall, Hurst JW., editors. The History, Physical and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990. pp. 637–642. [PubMed] [Google Scholar]
- 20.Augoustides JG, Greenblatt E, Abbas MA, et al. Clinical approach to agitation after electroconvulsion therapy: a case report and literature review. J ECT. 2002;18:213–217. doi: 10.1097/00124509-200212000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Lambrey S, Adam C, Baulac M, et al. Postictal psychosis syndrome: a clinical entity to be recognized. Rev Neurol (Paris) 2009;165:155–163. doi: 10.1016/j.neurol.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 22.Gurrera RJ, Caroff SN, Cohen A, et al. An international consensus study of neuroleptic malignant syndrome diagnostic criteria using the Delphi method. J Clin Psychiatry. 2011;72:1222–1228. doi: 10.4088/JCP.10m06438. [DOI] [PubMed] [Google Scholar]
- 23.Poeschla BD, Bartle P, Hansen KP. Serotonin syndrome associated with polypharmacy in the elderly. Gen Hosp Psychiatry. 2011;33:301.e9–301.e11. doi: 10.1016/j.genhosppsych.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 24.Thomas P, Alptekin K, Gheorghe M, et al. Management of patients presenting with acute psychotic episodes of schizophrenia. CNS Drugs. 2009;23:193–212. doi: 10.2165/00023210-200923030-00002. [DOI] [PubMed] [Google Scholar]
- 25.Dolan JG, Mushlin AI. Routine laboratory testing for medical disorders in psychiatric inpatients. Arch Intern Med. 1985;145:2085–2088. [PubMed] [Google Scholar]
- 26.Lukens TW, Wolf SJ, Edlow JA, et al. Clinical policy: critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. Ann Emerg Med. 2006;47:79–99. doi: 10.1016/j.annemergmed.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Zun LS, Hernandez R, Thompson R, et al. Comparison of EP's and psychiatrists' laboratory assessment of psychiatric patients. Am J Emerg Med. 2004;22:175–180. doi: 10.1016/j.ajem.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 28.Munro J, Booth A, Nicholl J. Routine preoperative testing: a systematic review of the evidence. Health Technol Assess. 1997;1:i–iv,1. –62. [PubMed] [Google Scholar]
- 29.Henneman PL, Mendoza R, Lewis RJ. Prospective evaluation of emergency department medical clearance. Ann Emerg Med. 1994;24:672–677. doi: 10.1016/s0196-0644(94)70277-2. [DOI] [PubMed] [Google Scholar]