Abstract
Objective. To introduce pharmacy students to a patient-centered mnemonic to aid them in remembering the most important parameters when assessing a patient's drug therapy and to determine whether use of the device improved students’ clinical examination scores.
Design. Second-year pharmacy students were randomized to an intervention group or a control group. A 30-minute presentation on the rationale of the mnemonic and how to apply it to clinical scenarios was given to the intervention group and then a case-based multiple-choice clinical examination was administered. Students in the control group completed the same examination first and then were given the mnemonic.
Assessment. Ninety-five students completed the examination. Examination scores of students in the intervention group were 6% higher than those of students in the control group (p = 0.04). A 6-question survey instrument was administered to both groups and the majority of students agreed that they would use the mnemonic when assessing patients during their upcoming practice experiences. One-hundred percent of the students stated that the mnemonic definitely or probably helped them (or would have helped them) think critically when assessing the patient cases.
Conclusions. Pharmacy students who used a mnemonic device for pharmacotherapy assessment exhibited better decision-making skills and made fewer errors than students who did not use the mnemonic.
Keywords: mnemonic, educational tool, decision making
INTRODUCTION
The pharmacist's role continues to expand and now includes therapeutic decision making for individual patients. The outcomes created by the Center for the Advancement of Pharmaceutical Education (CAPE) strongly emphasize pharmacy students being able to provide patient-centered care.1 Similarly, the Accreditation Council for Pharmacy Education (ACPE) requires that pharmacy graduates be competent to provide patient-centered care and have the ability to design, implement, monitor, evaluate, and adjust pharmacy care plans that are patient-specific. In doing so, graduates are expected to minimize drug misadventures and optimize patient outcomes.2
When pharmacy students start their advanced pharmacy practice experiences (APPEs) they need to be able to think critically and feel confident in their decisions. The transition from classroom lectures to experiential learning is difficult. One of the fundamental challenges encountered by pharmacy students is applying knowledge learned in the classroom to specific patients, even if the students received excellent grades in therapeutics courses.3 To list all of the side effects and contraindications of lisinopril, for example, a student must recall memorized information. However, to determine whether a particular patient should receive lisinopril, a student must be able to assimilate previously learned knowledge and apply it to a unique clinical situation through reasoning and critical thinking. Students often struggle with making drug therapy recommendations for specific patients because they are afraid of making a critical mistake.
To maximize sound decision making and minimize errors, a systematic tool, such as a flowchart, checklist, or mnemonic, can be used. In their development of a flowchart for therapeutics integration, Winslade and colleagues stressed that pharmacy students must have a problem-solving decision-making framework to follow to help ensure that they consider all of the important information when assessing a patient's drug-related problems.3 “Adverse drug reaction,” “excess dose,” and “drug interaction” are decision points along the multiple-branching algorithm that must be considered as potential causes for a drug-related problem. By following the flowchart, students are less likely to overlook an existing or potential problem related to 1 of these 3 causes.
Similar to an arborization strategy such as a flowchart, a checklist offers a systematic and comprehensive method of outlining criteria that should be considered when undertaking a particular process.4 Hales and colleagues assert that checklists are “important tools to condense large quantities of knowledge in a concise fashion, reduce the frequency of errors of omission, create reliable and reproducible evaluations and improve quality standards.”4 Not only do checklists simplify information processing, they have the potential to improve the quality of patient care. For example, implementation of a 19-item World Health Organization safe-surgery checklist resulted in decreased rates of death and complications among patients.5
Similar to a flowchart or checklist, a mnemonic device can be used to navigate through a complicated clinical decision-making process. One unique advantage of mnemonic devices is that they can be remembered easily. Numerous examples of medical mnemonics exist. For example, the mnemonic “GOLD MARK” was introduced in a paper published in Lancet to describe the possible causes for an anion-gap metabolic acidosis (Glycols, Oxoproline (Tylenol overdose), L-lactate, D-lactate, Methanol, Aspirin, Renal failure, Ketoacidosis).6 Two other examples of mnemonics include “SAFE,” which was developed by members of the American College of Allergy, Asthma and Immunology and the American College of Emergency Physicians to remind physicians of the 4 basic action steps suggested for the care of a patient with anaphylaxis (Seek support, Allergen identification and avoidance, Follow-up for specialty care, and Epinephrine for emergencies)7, and “AIRESMOG” to assess contributors to poor asthma control (Allergy and adherence to therapy, Infection and inflammation, Rhinitis and rhinosinusitis, Exercise and error in diagnosis, Smoking and psychogenic factors, Medications, Occupational exposures, Obesity and obstructive sleep apnea, Gastroesophageal reflux disease).8 In each of the previous examples, the mnemonic is used to prompt the user to conduct a thorough assessment of the topic, decreasing the chance that any important parameters are overlooked during assessment.
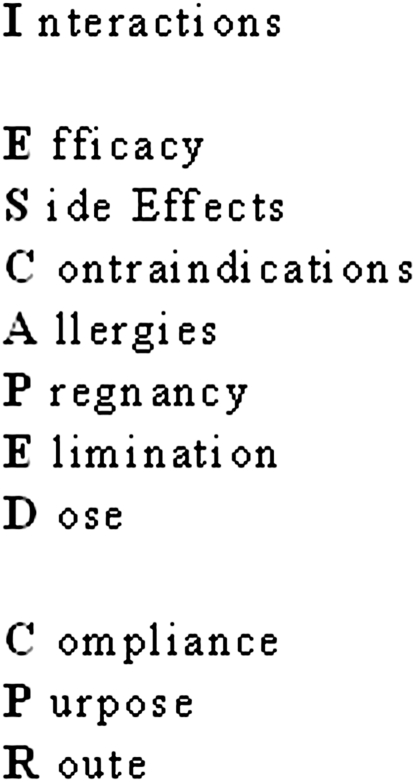
The mnemonic that we devised, “I ESCAPED CPR” is a patient-centered tool that offers a simple method to remember the most important parameters when assessing drug therapy for a patient and is the first mnemonic proposed for use in pharmacotherapy decision-making. The mnemonic, as shown in Figure 1, can be used to analyze current therapy and potential therapy being considered. It was our objective for pharmacy students to use the mnemonic I ESCAPED CPR to improve their scores on a case-based clinical examination. We hypothesized that students who learned the mnemonic would be more skilled at systematically approaching drug-therapy decisions for a particular patient, while minimizing the risk for errors. It was not our intention to test students’ recollection of memorized facts, but rather to test the success of a tool to increase students’ abilities to systematically organize their thoughts, resulting in safe, effective, and appropriate patient-specific decisions about pharmacotherapy.
Figure 1.
“I ESCAPED CPR” Mnemonic.
DESIGN
The letters in the mnemonic I ESCAPED CPR stand for: Interations, Efficacy, Side effects, Contraindications, Allergies, Pregnancy, Elimination, Dose, Compliance, Purpose, and Route. “Interactions” refers to any drug or food interaction that will affect therapy. “Efficacy” refers to whether the therapy is working currently or is likely to work. This can be evaluated by drug levels, vital signs, laboratory tests, subjective parameters, etc. “Side effects” relates to any current or potential adverse effects due to therapy. “Contraindications” refers to any reason that makes it inadvisable to administer a certain medication. This is probably the most comprehensive element of the mnemonic because contraindications can encompass any part of the patient's profile, eg, history, laboratory data, concurrent therapy. “Allergies” and “Pregnancy” are considerations that may seem obvious but are undoubtedly overlooked by many students recommending drug therapy. “Elimination” reminds students to consider renal and hepatic function of the patient when assessing the current therapy or when recommending a new medication. “Dose” signals the student to double check all medication doses, including starting doses, target doses, maximum doses, and doses for special populations. “Compliance” is an important factor to remember and can significantly impact a therapeutic decision. If a patient is not taking the medication that he or she already possesses, it is futile and potentially dangerous to increase the dose or add another medication. Likewise, a patient with compliance problems is unlikely to adhere to a medication dosed 4 times daily. “Purpose” encourages the student to verify that all medications on a patient's profile have an appropriate indication. “Route” makes certain that a student contemplates the most appropriate administration of a drug. For example, it may not be advisable for a neutropenic patient to be given a suppository as the insertion process may increase the risk of infection.
The expected outcome from our curricular innovation was to demonstrate, by use of the mnemonic, an increase in pharmacy students’ ability to analyze a unique clinical situation, synthesize all of the information given, and evaluate drug therapy accordingly. These skills are described by Bloom's Taxonomy to be in the cognitive domain and revolve around critical thinking.9 Although students must possess the foundation of knowledge necessary to ultimately judge, compare, consider, and weigh all pharmacotherapy options, the mnemonic was designed to serve as a structured pattern to follow amid the scattered and disorganized thinking that can occur when evaluating complex patient cases.
The College of Pharmacy at Touro University California offers a curriculum in which pharmacy students have 2 years of classroom courses and 2 years of APPEs. Thus, second-year pharmacy students who had just completed their 2 years of classroom work were chosen for participation in the study as they would be starting their APPEs within several weeks. The study was administered in May 2011 during a week-long course, Pre-Rotational Educational Program (PREP), which is offered every spring for second-year students to prepare them for starting the experiential portion of the curriculum.
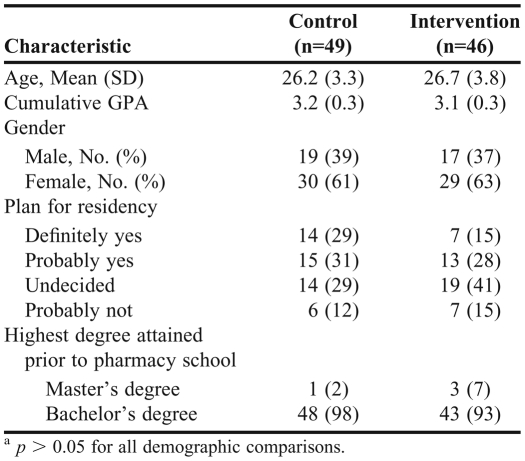
All second-year pharmacy students were randomized into 1 of 2 groups, the intervention group and a control group. As summarized in Table 1, a comparison of the demographics showed that there were no significant differences between the 2 groups. Of the initial 100 students who were randomized, 95 students completed the study. Of the 5 students not included in the analysis, 3 arrived late and 2 did not attend the PREP on that day. Before working up the clinical cases, the intervention group (n= 46) received a 30-minute presentation that consisted of detailed information on the rationale of the mnemonic and how to apply it to clinical scenarios. The control group (n= 49) did not receive the mnemonic until after working up the clinical cases. Two proctors, a faculty member and a pharmacy practice resident, were present in each of the examination rooms. Both groups of students were given 30 minutes to complete the clinical examination.
Table 1.
Characteristics of Pharmacy Students Participating in a Study to Determine the Effectiveness of a Mnemonic Device for Pharmacotherapy Assessmenta
EVALUATION AND ASSESSMENT
A written clinical examination was developed by a clinical pharmacy faculty member and consisted of 2 patient scenarios and 18 pharmacotherapy-related multiple-choice questions. The patient scenarios were designed to address the most common parameters that should be considered when determining whether a medication is appropriate for a specific individual (drug interactions, potential side effects, allergies, contraindications, etc). The examination was reviewed for appropriateness and accuracy by 2 other faculty members and multiple revisions were made The examination was then pilot tested with 3 third-year students not participating in the comparison who demonstrated that the average student, without knowledge of the mnemonic, could complete the case-based examination in approximately 30 minutes. Additional edits were made to the examination based on feedback from the students.
Students were asked to assess the appropriateness of medications for each patient scenario using a 3-point Likert scale (1 = likely to benefit the patient; 2 = likely to neither benefit/harm the patient; 3 = likely to harm the patient). For example, 1 case involved an individual with human immunodeficiency virus (HIV) who was taking a protease inhibitor-based antiretroviral regimen and needed relief for his seasonal allergies. Fluticasone nasal spray was presented as an option and the students were asked to respond regarding the appropriateness of this selection by selecting 1 of 3 possible answers, as described above. Each response was weighted on a scale of correctness (correct answer = 4 points, neutral answer = 2 points, incorrect answer = 0 points).
Students were allowed to use any online reference accessible on their laptops. It was not our intention to test students’ recollection of memorized facts, but rather the success of a tool to increase their ability to systematically organize their thoughts, thus resulting in safe, effective, and appropriate patient-specific decisions about pharmacotherapy. As an incentive, $5 gift cards were offered to the students with the top 15 scores in each group.
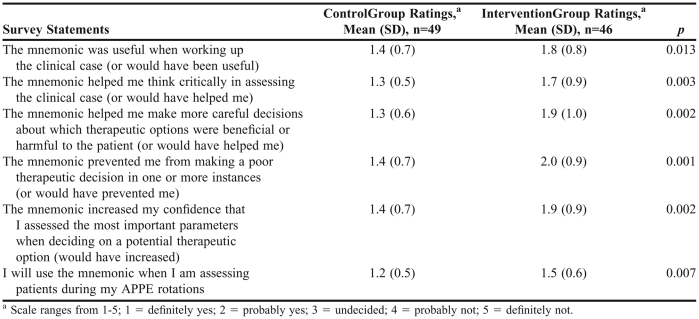
After completing the case-based examination, a 6-item survey instrument was administered to students in the intervention group to determine whether the mnemonic had helped them to make safer and more appropriate pharmacotherapy decisions and whether it increased their confidence in the decision-making process. Students in the control group received the mnemonic after taking the examination. After the mnemonic tutorial, they completed a similar survey with questions on whether the mnemonic would have benefited them had they received it beforehand.
All statistical analyses were conducted using SPSS for Windows, version 14 (SPSS Inc, Chicago, IL). As the survey was primarily descriptive in nature, continuous data are reported as mean ± standard deviation, and categorical data are reported as numbers and percentages of respondents. Student t test and chi-square tests were used for comparisons of continuous and categorical data, respectively. A p value of less than 0.05 was considered a significant difference.
The mean scores in the intervention group were 6% higher than scores in the control group (50.1 ± 7.1 vs. 46.3 ± 10.2, respectively; p = 0.04). The majority of students (52% in the intervention group and 82% in the control group) stated they would use the mnemonic when assessing patients during future APPEs (Table 2). More than 50% of students in the intervention group stated that the mnemonic definitely helped them think critically. Just less than half (46%) felt the mnemonic definitely helped them make decisions more carefully regarding therapeutic options for the patient. More than 75% of all participants responded definitely or probably on all questions. In the control group, greater than 70% of students stated the mnemonic definitely would have helped them think critically in assessing the clinical case and would have helped them make more careful decisions about which therapeutic options were beneficial or harmful to the patient.
Table 2.
Student Perceptions of a Mnemonic Device for Pharmacotherapy Assessment
DISCUSSION
Students who used the I ESCAPED CPR mnemonic when completing a case-based examination were better able to approach drug-therapy decisions systematically, resulting in improved decision-making and fewer errors. The mnemonic improved students’ scores on the complex case-based examination by 6%. Such an improvement could potentially translate to medication error reduction in clinical practice as well. Thus, we believe that the improvement in score seen with the mnemonic may represent not only a statistically significant result, but a clinically significant one as well. Other similar, relatively simple interventions, such as providing students or pharmacists with an educational leaflet or an algorithm, have been effective in achieving large reductions in medical error rates.10
The point at which students must recommend drug therapy is a critical one, charged with uncertainty, and it is at this stage of patient care that most preventable adverse drug events resulting from medication errors occur.11 The prescribing step, or the prescribing recommendation step for that matter, is critical because it is the juncture at which a healthcare provider's thoughts are transformed into decisions that will ultimately affect the patient.12 Computerized physician order entry systems linked with computerized decision support systems (CDSS) have helped reduce error rates at this step and have improved provider performance.13-22 We believe that the I ESCAPED CPR mnemonic is similar to the CDSS in that it aids prescribers in decision-making by integrating patient-specific data into the decision support system. Although it does not alert providers of existing drug-drug interactions, contraindications, allergies, etc, the mnemonic reminds the provider to consider and assess these general categories.
We reviewed the literature on drug-therapy problems to ensure that the mnemonic covered all necessary parameters requiring evaluation. Schwinghammer and Koehler postulate that problems in drug therapy relate to one or more of the following categories: unsafe therapy, ineffective therapy, inappropriate indication, and non-compliance.23 Using this classification, each major category of drug-therapy problems is accounted for by a parameter included in the mnemonic I ESCAPED CPR (unsafe therapy can be addressed by analyzing interactions, side effects, contraindications, allergies, pregnancy, elimination, dose, and route; ineffective therapy can be addressed by efficacy, dose, and route; inappropriate indication can be addressed by purpose; and noncompliance can be addressed by evaluating compliance). Importantly, the mnemonic prompts students to address additional critical areas that are an extension of the 4 general categories defined by Schwinghammer and Koehler.
If students systematically (as if checking off items on a to-do list) consider each variable represented in the mnemonic, the probability of forgetting a major element in the decision-making process is greatly decreased. Without using the mnemonic, students may be less thorough in their drug therapy analyses and feel less confident about their decisions. With practice, this analytical process should become faster and more intuitive. The mnemonic can be used to train the brain so that clinical decision making in the future is based on a well-learned pattern of thinking.
This is the first study to objectively assess the efficacy of a mnemonic to improve performance on a pharmacotherapeutic case examination. However, this study was not without limitations. Students who received the mnemonic before taking the case-based examination had less than 30 minutes to absorb the information and practice using the mnemonic before testing. Although the mnemonic is designed to provide organization, clarity, and efficiency, at first use it can be tedious and actually increase the time required for pharmacotherapeutic analysis. Ideally, the mnemonic would be learned and used repeatedly to increase the students’ comfort level and proficiency in its application before testing. Also, this study was conducted at the end of the second year of pharmacy school, shortly after students completed their final examinations and the 2-year cumulative examination that students are required to pass before beginning APPEs. Although students were given a small incentive to perform well on the case-based examination used in this study, it is possible that some students did not view it as high-stakes as it was not graded and would not affect their GPA. Another possible limitation was the use of multiple-choice Likert scale questions rather than open-ended questions as the Likert scale responses did not allow for or require open decision-making skills and may have greatly under- or overestimated students’ true knowledge. Finally, the mnemonic is not an all-encompassing tool, as it does not address cost or pharmacokinetic variables, such as absorption or distribution, which can be affected by characteristics such as age, fluid status, etc.
Although the mnemonic was well-received, with greater than 90% of students rating it favorably, acceptance was not unanimous. The lack of time given to absorb and apply the mnemonic likely contributed to its lack of universal acceptance. For all survey statements, results were more favorable in the control group, which received the mnemonic after having worked-up the case. This might be partially explained by the control students’ attributing any perceived poor performance to not having the additional help from a tool, such as the mnemonic. Hence, the control group may have overstated how much the mnemonic would have helped them perform had they received it beforehand. Nevertheless, both groups rated the mnemonic favorably. When data for “definitely” and “probably” response were combined, responses were greater than 90% for all questions, with 100% of students stating that the mnemonic helped them (or would have helped them) think critically when assessing the patient. We believe that with consistent and repeated use, the mnemonic will continue to gain approval. Also, only half of our study population actually used the mnemonic to assess the clinical case. The students in the control group rated the mnemonic based only on their perception of how it would have helped them had they had it during the examination.
This mnemonic could easily be integrated into the curriculum at other institutions if desired. If pharmacy students were taught the mnemonic earlier in the PharmD program, they would have the opportunity to use it when assessing patient cases in class. Future studies may want to identify the most optimal time to introduce the I ESCAPED CPR mnemonic in the pharmacy curriculum.
SUMMARY
The mnemonic I ESCAPED CPR provides students a simple and organized approach to complex pharmacotherapeutic decision-making. It enhances pharmacy students’ ability to remember the most important parameters when assessing a patient's drug therapy to maximize benefit and minimize risk. Pharmacists are expected to quickly and accurately analyze medication regimens and recommend safe and effective drug therapy for specific patients and they must have a thorough and systematic way to confidently make these decisions. Learning how to make good clinical decisions is a skill that is acquired over time and with experience. A mnemonic is one of the many tools that a pharmacy student can use in learning to think critically and systematically about patient care.
ACKNOWLEDGEMENTS
The authors thank Touro University for the monetary awards given to the students as an incentive to participate. The authors also thank Dr. Cheryl Horlen for her inspiration for this project.
REFERENCES
- 1.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes. http://aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed: December 20, 2011.
- 2.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed December 20, 2011.
- 3.Winslade N. Large group problem-based learning: a revision from traditional to pharmaceutical care-based therapeutics. Am J Pharm Educ. 1994;58(1):64–73. [Google Scholar]
- 4.Hales B, Terblanche M, Fowler R, Sibbald W. Development of medical checklists for improved quality of patient care. Int J Q Health Care. 2008;20(1):22–30. doi: 10.1093/intqhc/mzm062. [DOI] [PubMed] [Google Scholar]
- 5.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 6.Mehta AN, Emmett JB, Emmett M. GOLD MARK: an anion gap mnemonic for the 21st century. Lancet. 2008;372(9642):892. doi: 10.1016/S0140-6736(08)61398-7. [DOI] [PubMed] [Google Scholar]
- 7.Lieberman P, Decker W, Camargo CA, Jr, Oconnor R, Oppenheimer J, Simons FE. SAFE: a multidisciplinary approach to anaphylaxis education in the emergency department. Ann Allergy Asthma Immunol. 2007;98(6):519–523. doi: 10.1016/s1081-1206(10)60729-6. [DOI] [PubMed] [Google Scholar]
- 8.Thorsteinsdottir B, Volcheck GW, Enemark Madsen B, et al. The ABCs of asthma control. Mayo Clin Proc. 2008;83(7):814–820. doi: 10.4065/83.7.814. [DOI] [PubMed] [Google Scholar]
- 9.Bloom BS. Taxonomy of Educational Objectives, Handbook I: The Cognitive Domain. New York, NY: David McKay Co. Inc.; 1956. [Google Scholar]
- 10.Ioannidis JP, Lau J. Evidence on Interventions to Reduce Medical Errors: An Overview and Recommendations for Future Research. J Gen Intern Med. 2001;16(5):325–334. doi: 10.1046/j.1525-1497.2001.00714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. J Am Med Assoc. 1995;274(1):29–34. [PubMed] [Google Scholar]
- 12.Eslami S, Abu-Hanna A, De Keizer NF. Evaluation of Outpatient Computerized Physician Medication Order Entry Systems: A Systematic Review. J Am Med Inform Assoc. 2007;14(4):400–406. doi: 10.1197/jamia.M2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schedlbauer A, Vibhore P, Mulvaney C, et al. What Evidence Supports the Use of Computerized Alerts and Prompts to Improve Clinicians’ Prescribing Behavior? J Am Med Inform Assoc. 2009;16(4):531–538. doi: 10.1197/jamia.M2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Von Laue NC, Schwappach DLB, Koeck CM. The epidemiology of preventable adverse drug events: A review of the literature. Wien Klin Wochenschr. 2003;115(12):407–415. doi: 10.1007/BF03040432. [DOI] [PubMed] [Google Scholar]
- 15.Aranow M. What works: Clinical information systems. Order entry rules. Healthcare enterprise achieves physician acceptance, reduced medication errors and improved patient outcomes through CIS and CPOE technology. Health Manag Technol. 2002;23(7):34–38. [PubMed] [Google Scholar]
- 16.Bennett JW, Glasziou PP. Computerised reminders and feedback in medication management: A systematic review of randomised controlled trials. Med J Aust. 2003;178(5):217–222. doi: 10.5694/j.1326-5377.2003.tb05166.x. [DOI] [PubMed] [Google Scholar]
- 17.Bobb A, Gleason K, Husch M, et al. The epidemiology of prescribing errors: The potential impact of computerized prescriber order entry. Arch Intern Med. 2004;164(7):785–792. doi: 10.1001/archinte.164.7.785. [DOI] [PubMed] [Google Scholar]
- 18.Garg AX, Adhikari NKJ, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: A systematic review. JAMA. 2005;293(10):1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 19.Hodgkinson B, Koch S, Nay R, Nichols K. Strategies to reduce medication errors with reference to older adults. Int J Evid Based Healthc. 2006;4(1):2–41. doi: 10.1111/j.1479-6988.2006.00029.x. [DOI] [PubMed] [Google Scholar]
- 20.Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: A systematic review. Arch Intern Med. 2003;163(12):1409–1416. doi: 10.1001/archinte.163.12.1409. [DOI] [PubMed] [Google Scholar]
- 21.Oren E, Shaffer ER, Guglielmo BJ. Impact of emerging technologies on medication errors and adverse drug events. Am J Health-Syst Pharm. 2003;60(14):1447–1458. doi: 10.1093/ajhp/60.14.1447. [DOI] [PubMed] [Google Scholar]
- 22.Van der Sijs H, Aarts J, Vulto A, Berg M. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;13(2):138–147. doi: 10.1197/jamia.M1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwinghammer T, Koehler J. Pharmacotherapy Casebook: A Patient-Focused Approach, 7th Ed. McGraw-Hill: 2009. 1-10. [Google Scholar]