Abstract
Objective. To measure changes in pharmacy and medical students’ empathy scores after a 40-minute workshop during which students observed and discussed a theatrical performance about the challenges of aging.
Methods. First-year pharmacy and medical students (n = 187 and n = 183, respectively) participating in the workshop observed and discussed a 10-minute performance in which students enacted problems and concerns faced by elderly patients. The Jefferson Scale of Empathy (JSE) was administered just prior to the workshop (pretest), immediately afterward (posttest 1), and 7 or 26 days afterward (posttest 2).
Results. Empathy increased significantly from pretest to posttest 1 for students of each profession (p <0.01). Improvement in empathy scores declined by the time the JSE was readministered to pharmacy students 7 days later and to medical students 26 days later (posttest 2). Similar patterns of improved and declining empathy were found when the data were analyzed by gender and medical student specialty interest (ie, primary vs non-primary care specialties).
Conclusion. Empathy scores increased but were not sustained for both pharmacy and medical students after a brief workshop on aging that required limited personnel resources.
Keywords: empathy, pharmacy students, medical students, geriatric, elderly, theatrical performance
INTRODUCTION
Empathy is an important component of the healthcare provider-patient relationship that has been linked to optimal patient outcomes.1 Indicators of empathic engagement in patient care, such as communication, positive talk, appropriate touch, eye contact, bodily posture, gestures, and quality and quantity of the encounter can lead to increased patient satisfaction,2-5 better compliance,6-8 patients’ feelings of being important,9 accuracy of diagnosis,10 and accuracy of prognosis.11 Given the increased level of direct patient interaction that occurs between the pharmacist and the patient, empathy is also a key component of the pharmacist-patient relationship.
Despite the importance of improving empathy in health-professions students, empathy declines as students progress through medical school,12-14 dental school,15 and postgraduate medical education.16,17 These findings are a warning signal to the leaders and faculty members of health-professions educational institutions that strategies need to be designed not only to prevent the erosion of empathy but also to enhance students’ empathic orientation to achieve better understanding of patients.
Numerous approaches have been suggested to improve empathy among health-professions students.18 One approach to enhancing empathy is for students to assume the roles of persons in need of medical care, including elderly persons with age-related impairments.19-25 Anecdotal reports suggest that these approaches result in better understanding of the concerns and experiences of elderly people with chronic or terminal diseases.20,26,27 However, the short- and long-term effects of such approaches have not been empirically documented by using a psychometrically sound instrument specific to measuring empathy in the context of patient care. Moreover, most exercises about aging consume a considerable amount of personnel resources.19 This study was designed to determine the immediate and sustained impact on empathy scores of a workshop during which pharmacy and medical students watched and discussed a brief theatrical performance on the challenges of aging.
METHODS
A workshop on empathy was developed for pharmacy and medical students as part of a required biochemistry course. While most aging workshops last at least 3 hours,19-23 the time and personnel constraints of the course28,29 limited the workshop to 40 minutes. Participants in the workshop included 187 first-year students in the Chicago College of Pharmacy (89% of 209 students in the class of 2014) and 183 first-year students in the Chicago College of Osteopathic Medicine (91% of 202 students in the class of 2014) at Midwestern University. Participants were divided into groups of 20 to 40 students and assembled in different classrooms at different times. Five faculty members each facilitated one to three 40-minute workshop sessions over a 3-hour period of a single day.
Upon arrival at the workshop, students were informed that the purpose of the workshop was to depict the problems and concerns of elderly patients through a brief enactment by 2 of their fellow students. Before the start of the play, the Jefferson Scale of Empathy (JSE) was administered. The JSE (HPS-Version for pharmacy students and JSE, S-Version, for medical students), which was developed following an extensive review of the literature, relies on the definition of empathy in the context of patient care as a predominantly cognitive attribute that involves an understanding of the patient's experiences, concerns, and perspectives, combined with a capacity to communicate this understanding and an intention to help.12,18 The scale includes 20 items answered on a 7-point Likert scale (ranging from strongly agree = 7 to strongly disagree = 1).
The JSE has been examined previously for its psychometrics in pharmacy students,30 and it has been used to measure their empathy.31 Evidence in support of the JSE's construct validity,32-36 criterion-related validity,33,34 predictive validity,37 internal consistency reliability,33,34,36 and test-retest reliability36 has been reported in medical students and physicians. The JSE has received broad acceptance and has been translated into 42 languages to date. (More information about versions of the JSE can be found at: www.tju.edu/jmc/crmehc/medu/oempathy.cfm.)
Students were asked to write a 4-digit ID code (numeric, alphabetic, or combination of both) of their choice on the JSE. They were told to remember or make a note of the ID code to use on 2 posttests. Students were ensured that their individual responses were confidential, and that the survey tools would be destroyed after data were entered into computer files. The volunteer student actors did not complete the pretest.
After the students completed the JSE, the 10-minute performance began. A table was placed near the front of the room with 2 chairs on opposite sides. One actor portrayed an elderly person who was being admitted to a long-term assisted-care living facility. The other actor portrayed the assistant manager of the facility. The assistant manager and elderly patient entered the room, sat down in the chairs and started to talk, following the script written by one of the faculty members and given to them prior to the workshop. (A copy of the script can be obtained from the corresponding author.) The actor who played the role of the elderly person wore protective eye goggles covered with petroleum jelly to simulate visual impairment and earplugs to simulate hearing problems. The actor slowly entered the room where the other students had assembled, using a walker to simulate movement problems. The actor assumed a demanding personality, exhibiting impatient behavior and using a grumpy tone of voice, and asked questions about what to do in case of emergency, how food service is provided, schedules for taking their medicine, and other issues. The actor who played the role of the assistant manager showed more concern about rules and regulations related to running the facility than about attempting to understand the elderly person's concerns.
After the performance was over, students were encouraged to reflect on the interaction that had taken place between the characters and discuss their views and provide feedback. If the 30-minute group discussion lagged, facilitators intervened by asking predesignated questions (eg, “Do you recommend this workshop to other students?” and “Could the learning experience from this workshop help you in your future profession?”).
The JSE was administered to students again immediately after the workshop (posttest 1) and a final time to pharmacy students 7 days following the workshop and to medical students 26 days after the workshop (posttest 2).
Analysis of variance was used for repeated-measure design or pairing-design t tests for adjacent groups to test the significance of the changes in empathy scores for the matched samples, and the level of significance (probability of type 1 error) was set at 0.05 (Statistical Analysis System, Cary, NC, version 9.1 for Windows). This study fulfilled the criteria for exemption by the Midwestern University Institutional Review Board.
RESULTS
The response rates for the pretest, posttest 1, and posttest 2 were 89%, 96% and 84%, respectively, for pharmacy students completing survey tools with or without ID codes, and 91%, 99% and 92%, respectively, for medical students completing survey tools with or without ID codes. Ninety-nine percent of pharmacy and medical student participants (n = 186 and n = 182, respectively) used their unique identification code on the JSE just prior to and immediately after the workshop (pretest and posttest 1), allowing these nearly complete sets of data to be merged for inferential statistical analysis. However, only 148 pharmacy students (79%) and 85 medical students (46%) included their ID codes on all 3 test administrations (pretest, posttest 1, and posttest 2). Because of this, the data are presented in 2 sets: a comparison of matched pretest to posttest 1 scores and a comparison of matched pretest, posttest 1, and posttest 2 scores.
Empathy scores increased significantly (p <0.01) among both pharmacy and medical students (n = 186 and n = 182, respectively) between pretest and posttest 1. For pharmacy students, the JSE mean (±SD) scores for the pretest and posttest 1 were 110.8 ± 12.1 and 113.3 ± 13.2, respectively, and the difference was significant (p < 0.01). For medical students, the JSE mean scores for pretest and posttest 1 were 111.9 ± 11.1 and 113.7 ± 12.9, respectively, and the difference was significant (p < 0.01).
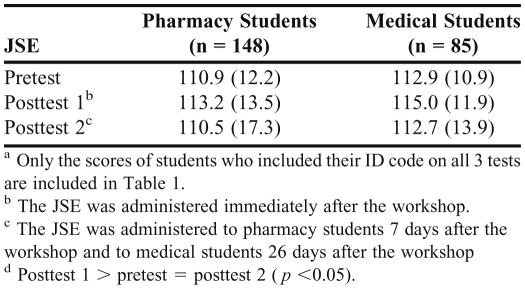
The means and standard deviations for empathy scores on pretest, posttest 1, and posttest 2 for those pharmacy students (n = 148) and medical students (n = 85) who included their ID code on all 3 tests are reported in Table 1. As shown in the table, the F-ratios were significant for pharmacy (F(2, 294) = 3.6, p < 0.05) and medical (F(2, 168) = 4.1, p < 0.05) students.
Table 1.
Comparisons of Students’ Scores on the Jefferson Scale of Empathy (JSE) Before, Immediately After, and 7 or 26 Days After a Workshop on the Challenges of Aging, Mean (SD)a
Post hoc pairwise mean comparison tests showed that the mean empathy score increased significantly immediately after the workshop (posttest 1) but returned to the pretest level in posttest 2. We observed the same pattern of mean test scores when the entire populations of pharmacy or medical student test results were considered (>84% response rate on each test for each profession), although these unmatched data could not be analyzed using our inferential statistical method.
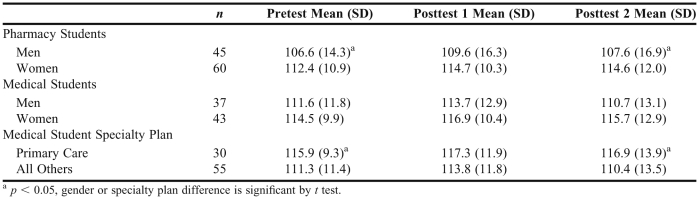
Only 105 pharmacy students and 80 medical students specified their gender and ID code on all 3 tests (Table 2). The pattern of changes in empathy scores for male and female pharmacy and medical students is similar to that obtained for the total samples (eg, mean score increased in posttest 1 but returned to baseline in posttest 2). Among pharmacy students, females had a significantly higher mean score than their male counterparts on the pretest and posttest 2 but not on posttest 1, indicating that the gender difference in feelings of empathy may have been diminished somewhat immediately after the workshop but was apparent again later. Although female medical students obtained a higher mean score on all 3 test administrations, none of the gender differences were significant.
Table 2.
Means and Standard Deviations (SD) of Pharmacy and Medical Students’ Scores on the Jefferson Scale of Empathy (JSE) in Pre- and Post-Tests of a Workshop about Aging, by Gender and Specialty Interest
All 85 medical students in the matched sample indicated the specialty they planned to pursue after graduation. The pattern of changes in empathy scores for medical students who planned to pursue a primary care specialty and for those interested in other specialties is similar to that observed in the total samples (eg, mean empathy score increased in posttest 1 but returned to the original level in posttest 2; Table 2). Those who planned to pursue a primary care specialty had higher mean empathy scores than other students on the pretest and posttest 2, but the difference was not significant in posttest 1, indicating that the pretest difference between the 2 groups diminished somewhat immediately after the workshop but the change was only temporary.
DISCUSSION
After watching a brief theatrical performance depicting various problems of elderly patients, there was an increase in the empathy scores of pharmacy and medical students but the increase was not sustained. Although the observed increases in empathy scores from pretest to posttest 1 were significant, they were not substantial, based on the magnitudes of effect-size estimates of the differences (effect sizes of 0.19 for both pharmacy and medical students are not considered substantial).38 However, the consistency of the pattern of findings, regardless of academic program, gender, or specialty interest, is important. The brevity of the performance (10 minutes) may have contributed to the small effect estimates.
A typical exercise about aging in medical education often requires all students to assume the identity of older adults and become actively involved in the role-playing rather than watching a performance by others. For example, the University of Minnesota's game on aging is often a half-day workshop coupled with an additional half day of clinical geriatrics teaching.19 A more substantial effect size could be obtained by using an expanded version of the workshop presented in our project, but such speculation awaits empirical verification.
Although increased empathy scores returned to the original level over time, our results are still encouraging, given that empathy tends to decline during health-professions education.12-17 We observed a similar pattern for patient-centered orientation scores of first-year medical students participating in a 2-hour workshop on reciprocity in relationships.39 The designs of other interventions that have been outlined18 could be altered to provide exposure to fresh empathy-raising activities throughout health-professions training. Longitudinal research would be needed to confirm the long-term effects of such interventions if they were used in the curriculum as regularly reoccurring events. In this regard, our preliminary studies show a longer increase in the patient-centered orientation scores of osteopathic medical students performing regular critical reflection as members of learning teams.40,41 However, these results need to be confirmed and expanded by using the JSE.
Limitations of this work include the single institution study and the low match rate in medical students on all 3 tests; both may jeopardize the external validity or generalization of the findings, although the match rate was 99% for the pretest and posttest 1. The lack of a randomly assigned control group (ie, with no participation in the workshop) for comparison with their participant counterparts further limits the attribution of changes exclusively to the workshop activities. Replication of this study by including control groups and representative samples from multiple institutions would enable us to generalize the findings and to infer cause-and-effect relationships.
CONCLUSIONS
A brief workshop to improve empathic understanding of elderly people increased empathy scores of pharmacy and medical students. The workshop was uniquely short (40 minutes), undemanding of personnel resources, and replicated in 2 groups of health-professions students. Enhancing health professionals’ empathic understanding of elderly patients is important and timely, considering the increasing number of elderly people in society who are treated by younger healthcare providers.
ACKNOWLEDGMENTS
We thank Dorissa Bolinski for her editorial assistance and Paulette Burdick for collecting and organizing the survey tools. We also thank faculty members in the Department of Biochemistry at Midwestern University who each facilitated 2 or 3 workshop sessions.
REFERENCES
- 1.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physician Empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–364. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 2.Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Med Care. 1988;1988;26(7):657–675. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237–251. doi: 10.1177/0163278704267037. [DOI] [PubMed] [Google Scholar]
- 4.Zachariae R, Pedersen CG, Jensen AB, Ehrnrooth E, Rossen PB, Von der Maase H. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer. 2003;88(5):658–665. doi: 10.1038/sj.bjc.6600798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians' characteristics influence patients' adherence to medical treatment: Results from the medical outcomes study. Health Psychol. 1993;12(2):93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 6.DiMatteo MR, Hays RD, Prince LM. Relationship of physicians' nonverbal communication skills to patient satisfaction, appointment noncompliance and physician workload. Health Psychol. 1986;5(6):581–594. doi: 10.1037//0278-6133.5.6.581. [DOI] [PubMed] [Google Scholar]
- 7.Falvo D, Tippy P. Communicating information to patients. Patient satisfaction and adherence as associated with resident skill. J Fam Pract. 1988;26(6):643–647. [PubMed] [Google Scholar]
- 8.Squier RW. A model of empathetic understanding and adherence to treatment regimens in practitioner-patient relationships. Soc Sci Med. 1990;30(3):325–339. doi: 10.1016/0277-9536(90)90188-x. [DOI] [PubMed] [Google Scholar]
- 9.Colliver JA, Willis MS, Robbs RS, Cohen DS, Swartz MH. Assessment of empathy in a standardized-patient examination. Teach Learn Med. 1998;10(1):8–10. [Google Scholar]
- 10.Barsky AJ. Hidden reasons some patients visit doctors. Ann Intern Med. 1981;94(4 pt 1):492–498. doi: 10.7326/0003-4819-94-4-492. [DOI] [PubMed] [Google Scholar]
- 11.Dubnicki C. Relationships among therapist empathy and authoritarianism and a therapist's prognosis. J Consult Clin Psychol. 1977;45(5):958–959. doi: 10.1037//0022-006x.45.5.958. [DOI] [PubMed] [Google Scholar]
- 12.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 13.Newton BW, Barber L, Clardy J, et al. Is there hardening of the heart during medical school? Acad Med. 2008;83(3):244–249. doi: 10.1097/ACM.0b013e3181637837. [DOI] [PubMed] [Google Scholar]
- 14.Chen D, Lew R, Hershman W, Orlander J. Cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–1438. doi: 10.1007/s11606-007-0298-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherman JJ, Cramer BS. Measurement of changes in empathy during dental school. J Dent Educ. 2005;69(3):338–345. [PubMed] [Google Scholar]
- 16.Bellini LM, Shea JA. Mood change and empathy decline persist during three years of internal medicine training. Acad Med. 2005;80(2):164–167. doi: 10.1097/00001888-200502000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Mangione S, Kane GC, Caruso JW, et al. Assessment of empathy in different years of years of internal medicine training. Med Teach. 2002;24(4):370–373. doi: 10.1080/01421590220145725. [DOI] [PubMed] [Google Scholar]
- 18.Hojat M. Ten approaches for enhancing empathy in health and human services cultures. J Health Hum Serv Adm. 2009;31(4):412–450. [PubMed] [Google Scholar]
- 19.Pacala JT, Boult C, Hepburn K. Ten years’ experience conducting the aging game workshop: was it worth it? J Am Geriatr Soc. 2006;54(1):144–149. doi: 10.1111/j.1532-5415.2005.00531.x. [DOI] [PubMed] [Google Scholar]
- 20.Mcvey LJ, Davis DE, Cohen HJ. The ‘aging game’: an approach to education in geriatrics. JAMA. 1989;262(11):1507–1509. doi: 10.1001/jama.262.11.1507. [DOI] [PubMed] [Google Scholar]
- 21.Varkey P, Chutka DS, Lesnick TG. The aging game: improving medical students’ attitudes toward caring for the elderly. J Am Med Dir Assoc. 2005;7(4):224–229. doi: 10.1016/j.jamda.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Henry BW, Douglass C, Kostiwa IM. Effects of participation in an aging game simulation activity on attitudes of allied health students toward elderly adults. Internet Journal of Allied Health Sciences and Practice. 2007;5(4) ( http://ijahsp.nova.edu). Accessed November 16, 2011. [Google Scholar]
- 23.Robinson SB, Rosher R. Effect of the “half-full aging game experience” on medical students’ attitudes. Gerontol Geriatr Educ. 2001;21(pt 3):3–12. [Google Scholar]
- 24.Shapiro J, Hunt L. All the world's a stage: the use of theatrical performance in medical education. Med Educ. 2003;37(10):922–927. doi: 10.1046/j.1365-2923.2003.01634.x. [DOI] [PubMed] [Google Scholar]
- 25.Deloney LA, Graham CJ. Wit: using drama to teach first-year medical students about empathy and compassion. Teach Learn Med. 2003;15(4):247–251. doi: 10.1207/S15328015TLM1504_06. [DOI] [PubMed] [Google Scholar]
- 26.Stokes J. Grief and the performing arts: a brief experiment in humanistic medical education. J Med Educ. 1980;55(3):215. [PubMed] [Google Scholar]
- 27.Holleman WL. The play's the thing: using literature and drama to teach about death and dying. Fam Med. 2000;32(8):523–524. [PubMed] [Google Scholar]
- 28.Van Winkle LJ, Sefcik D. Medical students’ attitudes toward using simulated patients to introduce basic science concepts in a large classroom setting. Internet J Med Ed. 2010;1(2) [Google Scholar]
- 29.Sefcik D, Van Winkle LJ. Motivating students to attend basic science lectures. Acad Med. 2011;86(2):152. doi: 10.1097/ACM.0b013e3182042a49. [DOI] [PubMed] [Google Scholar]
- 30.Fjortoft N, Van Winkle LJ, Hojat M. Measuring empathy in pharmacy students: a psychometrics study of the Jefferson Scale of Empathy. Am J Pharm Educ. 2011;75(6) doi: 10.5688/ajpe756109. Article 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen JT, LaLopa J, Dang DK. Impact of patient empathy modeling on pharmacy students caring of underserved. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720240. Article 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hojat M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes. New York: Springer; 2007. [Google Scholar]
- 33.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Measure. 2001;61(2):349–365. [Google Scholar]
- 34.Hojat M, Gonnella JS, Mangione S, et al. Empathy in medical students as related to clinical competence, gender, and academic performance. Med Educ. 2002;36(6):522–527. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- 35.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloski JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77(10 Suppl):S58–S60. doi: 10.1097/00001888-200210001-00019. [DOI] [PubMed] [Google Scholar]
- 36.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement and relationship to gender and specialty. Am J Psychiatry. 2002;159(9):1563–1569. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 37.Hojat M, Mangione S, Nasca TJ, Gonnella JS. Empathy scores in medical school and ratings of empathic behavior 3 years later. J Soc Psychol. 2005;145(6):663–672. doi: 10.3200/SOCP.145.6.663-672. [DOI] [PubMed] [Google Scholar]
- 38.Hojat M, Xu G. A visitor's guide to effect size: statistical versus practical significance of research findings. Adv Health Sci Educ Theory Pract. 2004;9(3):241–249. doi: 10.1023/B:AHSE.0000038173.00909.f6. [DOI] [PubMed] [Google Scholar]
- 39.Van Winkle LJ, Dobie S, Ross VR, Sharma U, Green JM, Lynch SM. Acute Intervention to Foster Reflection on Reciprocity in Relationships Increased Participants’ Patient- or Student-centered Orientation Scores in Association with a Medical Biochemistry Course. Internet J Med Ed. 2011;1(2) [Google Scholar]
- 40.Van Winkle LJ, Robson C, Chandar N, Green JM, Viselli SM, Donovan K. Use of poems written by physicians to elicit critical reflection by students in a medical biochemistry course. J Learn Through Arts. 2011;7(1) [Google Scholar]
- 41.Van Winkle LJ, Chandar N, Green JM, Lynch SM, Viselli SM, Burdick P. Does critical reflection by biochemistry learning teams foster patient-centered beliefs among medical students? Med Sci Educ. 2011;21(2):158–168. [Google Scholar]