Abstract
Objective
The number of Chinese-American breast cancer survivors (BCS) is increasing as a result of increasing incidence rates. There has been little research on Chinese BCS’ follow-up cancer care. This qualitative study aims to understand how Chinese-American BCS experience and cope with physical distress relative to non-Hispanic White (NHW) survivors.
Methods
Seventy-one BCS (37 Chinese immigrant, 7 US-born Chinese, 27 NHW) were recruited from the Greater Bay Area Cancer Registry to participate in focus group discussions or one-on-one interviews about their survivorship experiences. All BCS were diagnosed with breast cancer at stage 0-IIA between 2006-2009, and had survived for 1-4 years without recurrence. Interviews were conducted in Cantonese, Mandarin, or English. Data analyses followed established qualitative methods of content analysis.
Results
BCS experienced pain and side effects from radiation, surgery, and hormonal therapy. Physical distress subsequently caused emotional concerns about recurrence or metastasis. Most BCS consulted physicians about their physical distress. Chinese immigrant BCS were less likely to have their issues resolved compared to NHW and US-born Chinese who were more likely to question physicians, ask for referrals, and make repeat attempts if their problems were not resolved. Some Chinese immigrant BCS turned to Traditional Chinese Medicine for relief or accepted the idea that physical distress was part of survivorship.
Conclusion
Chinese immigrant BCS may be at risk for greater distress compared with US-born Chinese and NHW BCS because of cultural norms that make them less inclined to express their needs to physicians or challenge physicians when their needs are not met. Furthermore, they may express symptoms in culturally unique ways (e.g., hot-cold imbalances). Further research is needed to determine how to best improve survivorship care experiences in this understudied population, with the goal of decreasing BCS’ physical distress and improving quality of life.
GOALS
Breast cancer incidence rates for Chinese-American women, the largest Asian subgroup in the United States (US), have been steadily rising in recent decades[1-3]. Data from the California Cancer Registry showed that between 2000-2004, incidence rates were 135.6 per 100,000 among US-born Chinese and 68.9 among foreign-born Chinese; rates increased 1-2% per year in each group[1]. Given that more than 75% of approximately 4 million Chinese Americans are over the age of 18 [4], the current estimated 2.6 million breast cancer survivors (BCS)[5] would include a substantial number of Chinese-Americans. It is projected that by 2050, Asian Americans will be the fastest growing population in the US[6]. Despite their growing numbers, very little is known about Chinese-American cancer patients’ quality of life (QoL) after treatment. Given that most Chinese-Americans are immigrants (~65%) and half do not speak English fluently[7], Chinese-American BCS’ experiences may differ from those of their non-Hispanic White (NHW) counterparts in fundamental ways.
Specifically, many Chinese-Americans view cancer as a fatal and stigmatized disease[8-11]; hold traditional Eastern views of care[12-14]; and experience barriers to accessing care[14,15]. For Chinese immigrants, potential challenges to coping with cancer distress may be amplified as a result of living in a different cultural environment[16-19]. Recent research indicated that Asian BCS who had lower English proficiency reported higher distress symptoms and lower QoL scores[20].
An exploratory study showed that Chinese-American BCS had more medical distress, but fewer physical and psychological problems than NHW survivors[21]; however, it is not known how medical distress in the Chinese-American BCS population differs from that of NHW survivors. Having difficulties in medical encounters may increase unmet needs pertaining to physical problems (e.g., treatment side effects) and subsequently increase physical and emotional distress[20,22-28]. Despite an increase in research on ethnic variability in QoL among BCS[29-34], studies that include Asian Americans are scarce[35,36].
In this paper, we present a pilot study that used qualitative approaches to understand similarities and differences in experiencing and coping with cancer-related physical distress in two ethnic groups—NHW and Chinese-Americans.
METHODS
Study population and setting
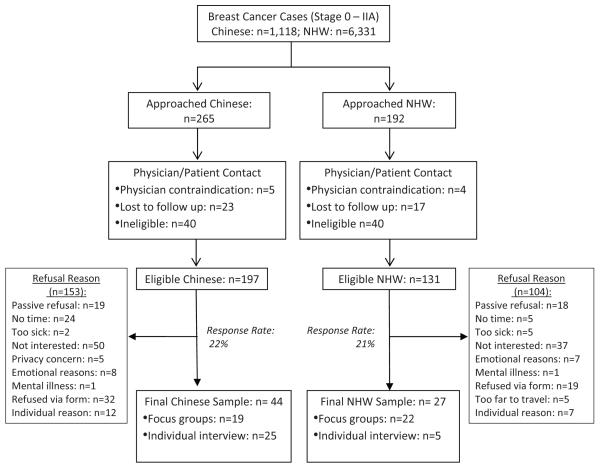
Participants were recruited from the population-based Greater Bay Area Cancer Registry (GBACR), a SEER registry in Northern California. Eligible participants: 1) were Chinese or NHW ethnicity; 2) were age ≥21; 3) had been diagnosed with first primary node-negative breast cancer at stage 0-IIA; 4) had completed primary treatments (surgery, radiation, chemotherapy) 1-4 years prior to recruitment, which started in 2010; and 5) had no incidence of recurrence or other cancers. Based on 2006-2009 breast cancer cases reported to GBACR, approximately 1,118 Chinese and 6,331 NHW cases potentially fit our study criteria. We sent invitation letters to randomly selected cases and then called those cases to screen for eligibility. Patients who had physician contraindications; who reported mental problems; or who were unable to clearly communicate with our field staff were not invited to participate. Figure 1 provides a summary of the recruitment procedures, response rates, and refusal reasons. Field interviewers confirmed participants’ eligibility during the invitation call. Seventy-one BCS (37 Chinese immigrant, 7 US-born Chinese, 27 NHW) participated in this study.
Figure 1.
Flow Chart of Patient Enrollment
The Institutional Review Boards at Georgetown University Medical Center, the California Health and Human Services Agency, and the Cancer Prevention Institution of California (CPIC) approved this study.
Data collection
Semi-structured interview guides were developed to gather information on the survivorship experiences of Chinese and NHW survivors. This paper is limited to data on physical distress. The main themes covered in the interview guides were: QoL after treatment (e.g., physical functioning and emotional state), follow-up care (e.g., patient-provider communication and medical exams), social support, and self-care (e.g., dietary practices, activity changes). Both groups were also asked if they used any type of alternative therapies, including Traditional Chinese Medicine (TCM). Interview guides for Chinese BCS also included probes about how Chinese culture influenced the survivorship experience. Interview guides were written in English and Chinese languages. Chinese guides were back-translated to English to confirm semantic equivalence.
Trained research staff conducted four Chinese immigrant (n=19) and four NHW (n=22) focus groups, and 30 one-on-one interviews (5 NHW, 7 US-born Chinese, 18 Chinese immigrant) with BCS. We oversampled immigrant Chinese because little is known about survivorship in this group relative to research on NHW. We included US-born Chinese to further explore the impact of immigration on survivorship experience. Focus groups were conducted at CPIC and community centers in San Francisco’s Chinatown. One-on-one interviews were conducted via telephone, in order to elicit narratives from women who felt uncomfortable sharing their experiences in a group setting. This methodology provided the research team with a more inclusive understanding of survivorship experiences. Interviews lasted 1.5 – 2 hours. Participants received $35 gift cards as incentives. Interviews were audio-recorded and transcribed. Chinese language interviews were translated into English for analysis.
Data analysis
Transcripts were analyzed for major themes pertaining to BCS’ experiences. Two trained coders manually coded all interviews independently in order to make possible an unconstrained analysis of the data[37,38]. Data analyses followed established qualitative methods of content analysis[39]. Primary categories were created prior to transcription analysis and were refined during the initial coding process. The codebook taxonomy consisted of broad categories and specific codes within the categories. Initial intercoder reliability was 86.1%; however, all text was discussed and ultimately coded to consensus.
RESULTS
Socio-demographic and clinical data presented in Table 1 were based on self-reports. The ages of all BCS ranged from 38 to 73 (mean= 57.7). More Chinese immigrant BCS had mastectomies (43.2%) relative to US-born Chinese and NHW BCS (28.6%, and 22.2% respectively), consistent with previous research[40-42]. Although all BCS were insured, Chinese immigrant BCS had a higher percentage (32.4%) of annual household incomes below $30,000 compared to US-born Chinese and NHW BCS (see Table 1).
Table 1.
Characteristics of Study Sample
| Total (N=71) |
NHW (N=27) |
Chinese (N=44) |
||
|---|---|---|---|---|
| US-Born (N=7) | Immigrant (N=37) | |||
| Average Years in the US (S.D.) | * | 23.1 (2.8) | ||
|
| ||||
| Average Age (S.D.) | 57.7 (9.1) | 58.7 (10.0) | 58.3 (6.3) | 57.0 (9.1) |
|
| ||||
| Language | ||||
| Chinese only | 18.6% | 0 | 0 | 36.1% |
| English and Chinese | 38.6% | 0 | 57.1% | 63.9% |
| English only | 42.9% | 100.00% | 42.9% | 0 |
|
| ||||
| Marital Status | ||||
| Married/with partner | 67.6% | 48.1% | 85.7% | 78.4% |
| Separated/Divorced | 12.7% | 18.5% | 0 | 10.8% |
| Widowed | 8.5% | 11.1% | 0 | 8.1% |
| Never married | 11.3% | 22.2% | 14.3% | 2.7% |
|
| ||||
| Education | ||||
| Grade 1-12 | 25.4% | 11.1% | 0 | 40.5% |
| Vocational/ Technical school | 7.0% | 3.7% | 0 | 10.8% |
| Some college | 18.3% | 25.9% | 14.3% | 13.5% |
| College graduate | 31.0% | 29.6% | 71.4% | 24.3% |
| Master’s or Higher degree | 18.3% | 29.6% | 14.3% | 10.8% |
|
| ||||
| Employment Status | ||||
| Employed | 55.0% | 59.2% | 14.3% | 59.5% |
| Unemployed | 9.9% | 3.7% | 42.9% | 8.1% |
| Homemaker | 8.5% | 0 | 14.3% | 13.5% |
| Retired | 23.9% | 33.3% | 28.6% | 16.2% |
| Self-employed/Disabled | 2.8% | 3.7% | 0 | 2.7% |
|
| ||||
| Income | ||||
| < $30,000 | 16.9% | 0 | 0 | 32.4% |
| $30,000 - $49,999 | 14.1% | 11.1% | 0 | 18.9% |
| $50,000 - $69,999¥ | 12.6% | 11.1% | 28.6% | 10.8% |
| $80,000- $99,999 | 18.4% | 25.9% | 14.3% | 13.5% |
| > $100,000 | 23.9% | 37.0% | 42.9% | 10.8% |
| Don’t Know | 14.0% | 14.8% | 14.3% | 13.5% |
|
| ||||
| Insurance | ||||
| All are insured | 100% | 100% | 100% | 100% |
|
| ||||
| Stage of Cancer ≠ | ||||
| 0 | 59.2% | 55.6% | 57.1% | 62.2% |
| I | 26.8% | 33.3% | 42.9% | 18.9% |
| II | 2.8% | 3.7% | 0 | 2.7% |
| Don’t know | 11.3% | 7.4% | 0 | 16.2% |
|
| ||||
| Type of Treatment † | ||||
| Mastectomy | 33.8% | 22.2% | 28.6% | 43.2% |
| Lumpectomy | 66.2% | 81.5% | 85.7% | 51.4% |
| Chemotherapy | 2.8% | 3.7% | 0 | 2.7% |
| Radiation | 46.5% | 48.1% | 71.4% | 40.5% |
|
| ||||
| Survival months‡ | ||||
| 0-12 months | 28.2% | 25.9% | 57.1% | 24.3% |
| 13-24 months | 40.9% | 40.8% | 28.6% | 43.3% |
| 25-36 months | 15.5% | 11.1% | 14.3% | 18.9% |
| 36-45 months | 15.5% | 22.2% | 0.0% | 13.5% |
Note. S.D. = Standard Deviation.
Only one NHW participant was born in South Africa and came to the US in 2006.
No participant reported income between $70,000 and $79,999.
Based on self-report, the distribution of treatment type for each stage in our sample was similar; about 31.0% of women at stage 0 and 31.6% at stage I had mastectomy; 69.0% at stage 0 and 73.7% at stage I had lumpectomy; 45.2% at stage 0, and 42.1% at stage I had both lumpectomy and radiation. Only one woman at stage I and one woman at stage II received chemotherapy. Stage II was not indicated as stage IIA in Table 1 since patients didn’t specifically mentioned stage IIA, but our cases from GBACR were restricted to stage IIA.
Individual participants might have received more than one type of treatment. Percentages were calculated based on participants’ self-reports of the receipt of all types of treatments.
Survival months were estimated based on the intervals between the completed date of primary treatment and the mail-out date of invitation letters for participation. The completed treatment date was based on women’s self-report since the cancer registry did not have an end treatment date.
Among all BCS, 44 (62%) reported varying levels of physical distress. There was a relationship between the length of survivorship and distress symptomology; however, this is likely due to the types of treatment that women consumed during varying stages of survivorship. For example, within the first 12 months, BCS were more likely to report pain from surgery. In the two periods, 0-12 months and 13-24 months, women reported distress related to radiation. For symptoms that could occur at any point during survivorship (e.g., side effects from hormonal therapy, acute pain), there were no differences across the length of survivorship categories shown on Table 1. In our sample, physical distress was more related to treatment type than stage. This may be due to the fact that the majority of our participants were at stage 0-I, so women had similar rates of total mastectomies, radiation, or hormonal therapy across stages (see notes in Table 1). Only two participants had chemotherapy. The highest frequency of discomfort (n=16, out of the 44) was associated with hormonal therapy (e.g., Tamoxifen and aromatase inhibitors), which triggered menopausal symptoms (e.g., hot flashes, mood swings), generalized pain, and decreased energy. Other side effects included weight gain and skin rashes. Six survivors rated these side effects as moderate and manageable; 10 BCS complained of severe side effects. Most women indicated that they were not informed about the potential side effects of hormonal therapy. In addition, these women reported that doctors failed to provide strategies to alleviate their discomfort, yet urged them to continue therapy for the recommended five years.
The second most frequently cited group of complaints was related to radiation side effects. Ten women listed fatigue, skin burns, and bone pain as side effects of radiation. Both Chinese and NHW participants complained of malaise and pain, but Chinese women were more likely to have itchy skin and rashes.
Five survivors, all of who had received total mastectomies, complained about severe or prolonged discomfort associated with their surgeries. It should be noted, however, that four out of the five were still within 12 months post-surgery. Six other BCS stated that they had some pain and suffered from limited range of motion while their bodies were healing from surgery, but the pain was as they had expected it to be. Overall, women were satisfied with their physicians’ responses to questions about post-surgical pain. For example, doctors explained that “tearing” sensations were caused by nerve and tissue healing. Medical staff recommended rehabilitation exercises for the arm and chest areas. With the exception of the first 12 months post-surgery, reports of pain did not vary by surgery type or length of survivorship.
An in-depth discussion of emotional distress is beyond the scope of this paper; however, 18 participants (25%) reported some level of emotional distress directly resulting from physical symptoms. Thirteen of the women’s complaints were related to treatment side effects. Five BCS reported that any pain, including pain in other parts of the body (e.g., head, shoulder, abdomen) brought on fears of metastasis. Rates of emotional distress resulting from physical discomfort were comparable across ethnic groups; however, when Chinese immigrant BCS expressed fear about recurrence, their language was graver than the other groups.
I get paranoid over even little things. Recently, I blew my nose, and noticed blood in my snot, I froze… I am very frightened. Can’t sleep. Can’t eat. Very scared. Scared that something will happen, like cancer might come back, or spread over other parts of the body. (Chinese Immigrant)
NHW women were more likely to become angry, frustrated, or dispirited about how the physical symptoms impacted their daily lives. For example, below is a quote from a participant who believed that taking aromatase inhibitors would decrease her chances of recurrence, but she was miserable. She constantly thought about recurrence.
The pill is about that big (pinches fingers, signifying the size of the pill) and I look at it before I swallow it at night and I’m thinking, “You better work! After what you’re putting me through, you better work!” (NHW)
The US-born Chinese BCS were more likely to tolerate their physical distress. While they were proactive about finding solutions to their distress, they also accepted the idea that some discomfort was to be expected. They either continued with daily activities or made modifications.
An essential practice for resolving physical distress or at least diminishing fears that BCS reported was communicating with their physicians (e.g., oncologists, surgeons, primary care physicians). Chinese immigrants and NHW women were equally likely to contact their physicians about physical distress; however, NHW women were most likely to report having their physical distress issues resolved following medical encounters. Among the 10 NHW survivors who reported contacting their physicians about their discomfort, five stated that their pain was alleviated by their physician’s advice.
I’m taking an anti-depressant that is also used to counteract hot flashes in menopausal women. I told my oncologist right away and she prescribed it right away and it really worked. It really worked. (NHW)
Of the 16 Chinese immigrant women who visited their doctors about their concerns, only one stated that her physical distress was alleviated. Six of these women reported being calmed by the physicians’ assurance that their pains were normal, even though their pain persisted. Like NHW survivors, US-born Chinese BCS stated that they were not satisfied with their physicians’ assurance that everything was fine. They were more likely to challenge physicians, asking for more comprehensive explanations about their discomfort and referrals to access additional resources. For example, among the seven US-born Chinese women, four reported that it was only after multiple contacts with their physicians that they ultimately received what they wanted (e.g., a referral to a specialist); two reported that their problems were not resolved; and one reported multiple encounters with the doctor before accepting his advice that she should stay on the medication that was causing her distress.
While we did not specifically ask Chinese participants what language their physicians spoke, many stated that language was not a huge barrier because many Bay Area medical facilities provide translators and have physicians who speak Chinese. Instead, the unmet needs may be due to the cultural propensity of Chinese to respect authority figures (i.e., doctors) and their time, resulting in less than optimal outcomes for BCS.
Of the 15 Chinese women whose issues were not resolved following biomedical visits, eight turned to TCM for relief. Two others were interested, but did not have the money or know how to access TCM. One NHW reported the use of acupuncture for pain relief. Several of the Chinese BCS stated that their physical problems, such as, skin rashes—a side effect reported by Chinese BCS, but not NHW survivors—were related to hot-cold imbalances and were resolved using TCM. For example, a Chinese immigrant BCS said that one of her breasts felt hotter than the other. Her Western physician said that this was impossible; however, her TCM doctor said that this was an imbalance resulting from radiation—one that is prevalent in ~2% of radiation patients. The TCM doctor gave her medicine to reduce heat; she was better in two weeks.
DISCUSSION
According to our data, many BCS still experienced pain and discomfort even at up to four years after diagnosis. These physical side effects became psychological reminders of their elevated risk for a second breast cancer, recurrence, or other cancers. The results of this study showed that many BCS, across ethnic or cultural backgrounds, look for answers from their physicians to cope with physical distress. Chinese immigrant BCS reported less relief from physical problems following medical encounters compared to US-born Chinese and NHW BCS, possibly resulting in excess physical distress relative to their counterparts.
This study, consistent with prior literature[21], also suggests ethnic differences in medical distress between Chinese and NHW BCS. Unlike US-born Chinese and NHW survivors who were more active in querying physicians to meet their needs, Chinese immigrant BCS reported accepting the idea that discomfort was part of the survivorship experience. While language barriers per se were not deemed to be an issue in the current study, due to the availability of resources, the variations in patient-provider interaction may be an example of cultural influence on individual behavior[43-45]. In Chinese culture, physicians represent the authority of medical knowledge and are highly respected[10]. Respect is demonstrated by listening to physicians and following their instructions without challenging their authority[45]. A cross-cultural investigation of physician-patient communication and cancer screening presented evidence that patients who perceive physicians as authority figures tend to adopt physician-centered communication by depending on physicians’ medical advice[44]. Previous research has shown that physician empathy and patient-centered communication are positively associated with cancer patients’ QoL[46-48]. Other studies point out that patients might not retain information given by physicians when they were overwhelmed with complex cancer treatment information[49-51]. Communication issues may be exacerbated when patients do not know how to ask questions or when they are situated in different cultural and medical systems.
In TCM, “chi” represents a concept of energy; yin-yang imbalance in chi may result in physical vulnerability[52,53]. The uptake of alternative medicine is common among cancer patients, especially when their physical problems are not resolved with biomedical treatments[54-59]. In the current study, intriguingly, Chinese survivors reported different side effects (e.g., skin problems) from treatments and were more likely to hold a concept of yin-chi (cold) and yang-chi (hot) balance in the body. More immigrant Chinese BCS turned to TCM to find cures when their physical distress was not relieved compared to their US-born counterparts. This may be partially attributed to US-born survivors’ limited knowledge of TCM, or the exclusion of TCM from regular healthcare plans.
Notably, approximately 32% of Chinese immigrant survivors had annual household incomes less than $30,000, compared to 0% of NHW and US-born Chinese survivors. Among those Chinese immigrants who visited physicians for physical problems, only one reported relief from her pain. This may relate to socioeconomic disparities in obtaining quality care. However, population-based research showed that foreign-born Chinese women had lower survival rates than US-born, even after adjusting for sociodemographic and clinical factors, including stage[60,61]. More research on Chinese BCS is needed, particularly those of low socioeconomic status.
This study has several limitations. First, our findings are limited to patient narratives due to constrained resources to support an investigation of actual survivor-provider encounters. Research has stressed that physicians play a key role in facilitating the quality of follow-up care [48,62-64]. This pilot study presents rare information regarding survivorship care experiences from a cross-cultural perspective, which may demonstrate the need for larger scale cross-cultural research and perhaps, medical education for treating immigrants. Second, these qualitative results may not be generalizable since our Chinese and NHW samples were small, and, despite sampling from a population-based cancer registry, may not representative. The low participation rates (~21%) in Figure 1, consistent with prior qualitative research on multiethnic cancer survivors[65], might be due to the time commitment associated with qualitative interviews. These results should not be generalized to Chinese BCS populations in other parts of the country, given that the Greater San Francisco Bay area likely has the most resources available to Chinese BCS (e.g., Chinese support groups and media), which makes this research is important as medical and physical distress may be worse where fewer resources are available. Third, our participants were all diagnosed with early stage breast cancer and were short-term survivors; thus, their issues and needs might be very different from later stage or long-term survivors.
Despite these caveats, the findings of this study contribute to a small, but growing, body of knowledge about Chinese-American and NHW women’s survivorship experiences. The inclusion of US-born Chinese and NHW survivors in contrast to immigrant Chinese survivors provides a significant examination of cultural and ethnic difference in patients’ responses to physical distress following breast cancer diagnosis and treatment. Although this current qualitative study cannot determine whether unrelieved physical symptoms among Chinese immigrant BCS will impact their quality of life and eventually affect their surveillance outcomes, our findings warrant future large-scale investigations of physical distress, physician-survivor communication, as well as the effectiveness of TCM on relieving physical distress, ultimately leading to optimal surveillance care and outcomes.
Research Highlights.
Chinese and White breast cancer survivors were queried about their physical distress.
All had distress, but Chinese immigrants were less likely to have issues resolved.
Many Chinese immigrants used Traditional Chinese Medicine for distress relief.
Acknowledgements
This research was supported by a Lance Armstrong Foundation Young Investigator Award and the National Institutes of Health/National Cancer Institute R21 Grant# CA139408-01. This research was also supported by the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000040C awarded to the Cancer Prevention Institute of California. The collection of cancer incidence data used in this study was supported by the California Department of Health Services as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement #1U58 DP000807-01 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the authors, and endorsement by the State of California, the California Department of Health Services, the National Cancer Institute, or the Centers for Disease Control and Prevention or their contractors and subcontractors is not intended nor should be inferred.
We appreciate field staff at CPIC, Pagan Morris, Mei-chin Kuo, Kathie Lau, and Daisy Lubag for their efforts in participant enrollment and preparation for focus groups. We sincerely thank Dr. Frances M. Lewis, Dr. Grace X. Ma, and Dr. Rena Pasick for their constructive comments on the interview guides to enhance our qualitative data collection.
Footnotes
Conflict of Interest Statement The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- (1).Gomez SL, Quach T, Horn-Ross PL, Pham JT, Cockburn M, Chang ET, et al. Hidden Breast Cancer Disparities in Asian Women: Disaggregating Incidence Rates by Ethnicity and Migrant Status. Am J Public Health. 2010;100:S125–S131. doi: 10.2105/AJPH.2009.163931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Parkin DM. The global burden of cancer. Semin Cancer Biol. 1998;8(4):219–235. doi: 10.1006/scbi.1998.0080. [DOI] [PubMed] [Google Scholar]
- (3).Gomez SL, Le GM, Miller T, Undurraga DM, Shema SJ, Stroup A, et al. Cancer incidence among Asians in the Greater Bay Area. Northern California Cancer Center; Available: http://www.nccc.org/pdf/Registries/annual_reports/Special_Report_Cancer_Asians_1990-2002.pdf. [Google Scholar]
- (4).Asian Pacific American Legal Center. Asian American Justice Center . A Community of contrasts. Asian American Center for Advancing Justice; 2011. [Google Scholar]
- (5).Altekruse S, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, et al. Estimated number of cancer survivors in the United States from 1971 to 2008. National Cancer Institute; Available: http://cancercontrol.cancer.gov/ocs/prevalence/prevalence.html. 9-4-2011. [Google Scholar]
- (6).U.S. Department of State Increasing diversity predicted in U.S. population: Hispanic and Asian populations both poised to triple. 2005 Available: http://usinfo.state.gov/scv/Archive/2005/May/17-40125.html.
- (7).Asian Pacific Islander American Health Forum (APIAHF) Demographic and socioeconomic profiles of Asian Americans, Native Hawaiians, and Pacific Islanders in the United States. 2011 1986-2011. Available: http://www.apiahf.org/resources/resources-database/profilesofaanhpi.
- (8).Wong-Kim E, Sun A, Merighi JR, Chow EA. Understanding quality-of-life issues in Chinese women with breast cancer: a qualitative investigation. Cancer Control. 2005;12(Suppl 2):6–12. doi: 10.1177/1073274805012004S02. [DOI] [PubMed] [Google Scholar]
- (9).Wong-Kim E, Sun A, DeMattos MC. Assessing cancer beliefs in a Chinese immigrant community. Cancer Control. 2003;10(5 Suppl):22–28. doi: 10.1177/107327480301005s04. [DOI] [PubMed] [Google Scholar]
- (10).Wang JH, Liang W, Schwartz MD, Lee MM, Kreling B, Mandelblatt JS. Development and evaluation of a culturally tailored educational video: changing breast cancer-related behaviors in Chinese women. Health Educ Behav. 2008;35(6):806–820. doi: 10.1177/1090198106296768. [DOI] [PubMed] [Google Scholar]
- (11).Wang JH, Sheppard VB, Schwartz MD, Liang W, Mandelblatt J. Disparities in cervical cancer screening between Asian and non-Hispanic White women. Cancer Epidemiol Biomarkers Prev. 2008;17(8):1968–1973. doi: 10.1158/1055-9965.EPI-08-0078. [DOI] [PubMed] [Google Scholar]
- (12).Ngo-Metzger Q, Massagli MP, Clarridge BR, Manocchia M, Davis RB, Lezzoni LI, et al. Linguistic and cultural barriers to care: perspectives of Chinese and Vietnamese immigrants. J Gen Intern Med. 2003;18(1):44–52. doi: 10.1046/j.1525-1497.2003.20205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Wang JH, Liang W, Chen MY, Cullen J, Feng S, Yi B, et al. The influence of culture and cancer worry on colon cancer screening among older Chinese-American women. Ethn Dis. 2006;16(2):404–411. [PMC free article] [PubMed] [Google Scholar]
- (14).Wang JH, Mandelblatt J, Liang W, Yi B, M IJ, Schwartz M. Knowledge, cultural, and attitudinal barriers to mammography screening among non-adherent immigrant Chinese women: ever versus never screened status. Cancer. 2009;115(20):4828–4838. doi: 10.1002/cncr.24517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Tsai DT, Lopez RA. The use of social supports by elderly Chinese immigrants. Journal of Gerontol Social Work. 1997;29(1):77–94. [Google Scholar]
- (16).Kim J, Ashing-Giwa KT, Kagawa SM, Tejero JS. Breast cancer among Asian Americans: is acculturation related to health-related quality of life? Oncol Nurs Forum. 2006;33(6):E90–E99. doi: 10.1188/06.ONF.E90-E99. [DOI] [PubMed] [Google Scholar]
- (17).Sun A, Wong-Kim E, Stearman S, Chow EA. Quality of life in Chinese patients with breast cancer. Cancer. 2005;104(12):2952–2954. doi: 10.1002/cncr.21516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Tam-Ashing K, Padilla G, Tejero J, Kagawa-Singer M. Understanding the breast cancer experience of Asian American women. Psychooncology. 2003;12(1):38–58. doi: 10.1002/pon.632. [DOI] [PubMed] [Google Scholar]
- (19).Tsai TI, Morisky DE, Kagawa-Singer M, Ashing-Giwa KT. Acculturation in the adaptation of Chinese-American women to breast cancer: a mixed-method approach. J Clin Nurs. 2011 doi: 10.1111/j.1365-2702.2011.03872.x. [DOI] [PubMed] [Google Scholar]
- (20).Yi JK, Swartz MD, Reyes-Gibby CC. English proficiency, symptoms, and quality of life in Vietnamese- and Chinese-American breast cancer survivors. J Pain Symptom Manage. 2011;42(1):83–92. doi: 10.1016/j.jpainsymman.2010.09.014. [DOI] [PubMed] [Google Scholar]
- (21).Kagawa-Singer M, Wellisch DK, Durvasula R. Impact of breast cancer on Asian American and Anglo American women. Cult Med Psychiatry. 1997;21(4):449–480. doi: 10.1023/a:1005314602587. [DOI] [PubMed] [Google Scholar]
- (22).Fernandes-Taylor S, Bloom JR. Post-treatment regret among young breast cancer survivors. Psychooncology. 2011;20(5):506–516. doi: 10.1002/pon.1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: lost in transition. The National Academies Press; 2005. [Google Scholar]
- (24).Hewitt M, Greenfield S, Stovall E. Meeting psychosocial needs of women with breast cancer. The National Academies Press; 2004. [PubMed] [Google Scholar]
- (25).Lam WW, Bonanno GA, Mancini AD, Ho S, Chan M, Hung WK, et al. Trajectories of psychological distress among Chinese women diagnosed with breast cancer. Psychooncology. 2010;19(10):1044–1051. doi: 10.1002/pon.1658. [DOI] [PubMed] [Google Scholar]
- (26).Lermam C, Daly M, Walsh WP, Resch N, Seay J, Barsevick A, et al. Communication between patients with breast cancer and health care providers. Determinants and Implications. Cancer. 1993;72(9):2612–2620. doi: 10.1002/1097-0142(19931101)72:9<2612::aid-cncr2820720916>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- (27).Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- (28).Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- (29).Fu OS, Crew KD, Jacobson JS, Greenlee H, Yu G, Campbell J, et al. Ethnicity and persistent symptom burden in breast cancer survivors. J Cancer Surviv. 2009;3(4):241–250. doi: 10.1007/s11764-009-0100-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Janz NK, Mujahid MS, Hawley ST, Griggs JJ, Alderman A, Hamilton AS, et al. Racial/ethnic differences in quality of life after diagnosis of breast cancer. Journal of Cancer Survivorship-Research and Practice. 2009;3(4):212–222. doi: 10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Bowen DJ, Alfano CM, McGregor BA, Kuniyuki A, Bernstein L, Meeske K, et al. Possible socioeconomic and ethnic disparities in quality of life in a cohort of breast cancer survivors. Breast Cancer Res Treat. 2007;106(1):85–95. doi: 10.1007/s10549-006-9479-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Moy B, Tu D, Pater JL, Ingle JN, Shepherd LE, Whelan TJ, et al. Clinical outcomes of ethnic minority women in MA.17: a trial of letrozole after 5 years of tamoxifen in postmenopausal women with early stage breast cancer. Ann Oncol. 2006;17(11):1637–1643. doi: 10.1093/annonc/mdl177. [DOI] [PubMed] [Google Scholar]
- (33).Fatone AM, Moadel AB, Foley FW, Fleming M, Jandorf L. Urban voices: the quality-of-life experience among women of color with breast cancer. Palliate Support Care. 2007;5(2):115–125. doi: 10.1017/s1478951507070186. [DOI] [PubMed] [Google Scholar]
- (34).Gil KM, Mishel MH, Belyea M, Germino B, Porter LS, Laney IC, et al. Triggers of uncertainty about recurrence and long-term treatment side effects in older African American and Caucasian breast cancer survivors. Oncol Nurs Forum. 2004;31(3):633–639. doi: 10.1188/04.onf.633-639. [DOI] [PubMed] [Google Scholar]
- (35).Ashing-Giwa KT, Lim JW. Predicting physical quality of life among a multiethnic sample of breast cancer survivors. Qual Life Res. 2010;19(6):789–802. doi: 10.1007/s11136-010-9642-4. [DOI] [PubMed] [Google Scholar]
- (36).Giedzinska AS, Meyerowitz BE, Ganz PA, Rowland JH. Health-related quality of life in a multiethnic sample of breast cancer survivors. Ann Behav Med. 2004;28(1):39–51. doi: 10.1207/s15324796abm2801_6. [DOI] [PubMed] [Google Scholar]
- (37).Saldana J. The coding manual for qualitative researchers. Sage Publication; Thousand Oaks,CA: 2009. [Google Scholar]
- (38).Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry. 2002;36:717–732. doi: 10.1046/j.1440-1614.2002.01100.x. [DOI] [PubMed] [Google Scholar]
- (39).LeCompte MD, Schensul JJ, Schensul SL. Analyzing and interpreting ethnographic data. Altamira Press; Baltimore: 1999. [Google Scholar]
- (40).Killoran M, Moyer A. Surgical treatment preferences in Chinese-American women with early-stage breast cancer. Psychooncology. 2006;15(11):969–984. doi: 10.1002/pon.1032. [DOI] [PubMed] [Google Scholar]
- (41).Gomez SL, France A, Lee MM. Socioeconomic status, immigration/acculturation, and ethnic variations in breast conserving surgery. Ethn Dis. 2004;14:134–140. [PubMed] [Google Scholar]
- (42).Prehn AW, Topol B, Stewart S, Glaser SL, O’Connor L, West DW. Differences in treatment patterns for localized breast carcinoma among Asian/Pacific islander women. Cancer. 2002;95(11):2268–2275. doi: 10.1002/cncr.10965. [DOI] [PubMed] [Google Scholar]
- (43).Gao G, Burke N, Somkin CP, Pasick R. Considering culture in physician-patient communicatiion during colorectal cancer screening. Qual Health Res. 2009;19(6):778–789. doi: 10.1177/1049732309335269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Napoles-springer AM, Santoyo J, Houston K, Perez-Stable EJ, Stewart AL. Patients’ perceptions of cultural factors affecting the quality of their medical encounters. Health Expect. 2005;8(1):4–17. doi: 10.1111/j.1369-7625.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).Health and health care for Chinese American Elder. University of Hawaii; 2011. Tom LASH. Available: http://www.stanford.edu/group/ethnoger/chinese.html. [Google Scholar]
- (46).Venetis MK, Robinson JD, Turklewicz KL, Allen M. An evidence base for patient-centered cancer care: a meta-analysis of studies of oberved communication between cancer specialists and their patients. Patient Educ Couns. 2009;77(3):379–383. doi: 10.1016/j.pec.2009.09.015. [DOI] [PubMed] [Google Scholar]
- (47).Neumann M, Wirtz M, Bollschweiler E, Mercer SW, Warm M, Wolf J, et al. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns. 2007;69(1-3):63–75. doi: 10.1016/j.pec.2007.07.003. [DOI] [PubMed] [Google Scholar]
- (48).Epstien RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute; Bethesda, MD: 2011. NIH publication 07-6225. [Google Scholar]
- (49).Polacek GN, Ramos MC, Ferrer RL. Breast cancer disparities and decision-making among U.S. women. Patient Educ Couns. 2007;65(2):158–165. doi: 10.1016/j.pec.2006.06.003. [DOI] [PubMed] [Google Scholar]
- (50).Keating NL, Guadagnoli E, Landrum MB, Borbas C, Weeks JC. Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement? J Clin Oncol. 2002;20(6):1437–1439. doi: 10.1200/JCO.2002.20.6.1473. [DOI] [PubMed] [Google Scholar]
- (51).Keating NL, Landrum MB, Ayanian J, Winer EP, Guadagnoli E. Consultation with a medical oncologist before surgery and type of surgery and type of surgery among older women with early-stage breast cancer. J Clin Oncol. 2003;21(24):4532–4539. doi: 10.1200/JCO.2003.05.131. [DOI] [PubMed] [Google Scholar]
- (52).Hwu YJ, Coates VE, Boore JR. The health behaviours of Chinese people with chronic illness. Int J Nurs Stud. 2001;38(6):629–641. doi: 10.1016/s0020-7489(00)00114-0. [DOI] [PubMed] [Google Scholar]
- (53).Simpson PB. Family beliefs about diet and traditional Chinese medicine for Hong Kong women with breast cancer. Oncol Nurs Forum. 2003;30(5):834–840. doi: 10.1188/03.ONF.834-840. [DOI] [PubMed] [Google Scholar]
- (54).Gray RE, Fitch M, Greenberg M. A comparison of physician and patient perspectives on unconventional cancer therapies. Psychooncology. 1998;7(6):445–452. doi: 10.1002/(SICI)1099-1611(199811/12)7:6<445::AID-PON329>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- (55).Wong-Kim E, Merighi JR. Complementary and alternative medicine for pain management in U.S.- and foreign-born Chinese women with breast cancer. J Health Care Poor Underserved. 2007;18(4 Suppl):118–129. doi: 10.1353/hpu.2007.0123. [DOI] [PubMed] [Google Scholar]
- (56).Lee MM, Lin SS, Wrensch MR, Adler SR, Eisenberg D. Alternative therapies used by women with breast cancer in four ethnic populations. J Natl Cancer Inst. 2000;92(1):42–47. doi: 10.1093/jnci/92.1.42. [DOI] [PubMed] [Google Scholar]
- (57).Cui Y, Shu XO, Gao Y, Wen W, Ruan ZX, Jin F, et al. Use of complementary and alternative medicine by Chinese women with breast cancer. Breast Cancer Res Treat. 2004;85(3):263–270. doi: 10.1023/B:BREA.0000025422.26148.8d. [DOI] [PubMed] [Google Scholar]
- (58).Boon H, Stewart M, Kennard MA, Gray R, Sawka C, Brown JB, et al. Use of complementary/alternative medicine by breast cancer survivors in Ontario: prevalence and perceptions. J Clin Oncol. 2000;18(13):2515–2521. doi: 10.1200/JCO.2000.18.13.2515. [DOI] [PubMed] [Google Scholar]
- (59).Lengacher CA, Bennett MP, Kip KE, Gonzalez L, Jacobsen P, Cox CE. Relief of symptoms, side effects, and psychological distress through use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum. 2006;33(1):97–104. doi: 10.1188/06.ONF.97-104. [DOI] [PubMed] [Google Scholar]
- (60).Chuang SC, Chen W, Hashibe M, Li G, Zhang ZF. Survival rates of invasive breast cancer among ethnic Chinese women born in East Asia and the United States. Asian Pac J Cancer Prev. 2006;7(2):221–226. [PubMed] [Google Scholar]
- (61).Gomez S, Clarke CA, Shema SJ, Chang ET, Keegan TH, Glaser SL. Disparities in breast cancer survival among Asian women by ethnicity and immigrant status: a population-based study. Am J Public Health. 2011;100(5):861–869. doi: 10.2105/AJPH.2009.176651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (62).Arora NK, Reeve BB, Hays RD, Clauser SB, Oakley-Girvan I. Assessment of Quality of Cancer-Related Follow-Up Care From the Cancer Survivor’s Perspective. J Clin Oncol. 2011;29:1280–1289. doi: 10.1200/JCO.2010.32.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (63).Arora NK, Weaver KE, Clayman ML, Oakley-Girvan I, Potosky AL. Physicians’ decision-making style and psychosocial outcomes among cancer survivors. Patient Educ Couns. 2009;77(3):404–412. doi: 10.1016/j.pec.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (64).Ganz PA. Survivorship: adult cancer survivors. Prim Care. 2009;36(4):721–741. doi: 10.1016/j.pop.2009.08.001. [DOI] [PubMed] [Google Scholar]
- (65).Quach T, Nuru-Jeter A, Morris P, Allen L, Shema SJ, Winters JK, et al. Experiences and perceptions of medical discrimination among a multi-ethnic sample of breast cancer patients in the San Francisco Bay area. Am J Public Health. doi: 10.2105/AJPH.2011.300554. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]