Abstract
Objective
Screening children for suicide risk when they present to the emergency department (ED) with nonpsychiatric complaints could lead to better identification and treatment of high-risk youth. Before suicide screening protocols can be implemented for nonpsychiatric patients in pediatric EDs, it is essential to determine whether such efforts are feasible.
Methods
As part of an instrument validation study, ED patients (10–21 years old) with both psychiatric and nonpsychiatric presenting complaints were recruited to take part in suicide screening. Clinically significant suicidal thoughts, as measured by the Suicidal Ideation Questionnaire, and suicidal behaviors were assessed, as well as patient opinions about suicide screening. Recruitment rates for the study as well as impact on length of stay were assessed.
Results
Of the 266 patients and parents approached for the study, 159 (60%) agreed to participate. For patients entering the ED for nonpsychiatric reasons (n = 106), 5.7% (n = 6) reported previous suicidal behavior, and 5.7% (n = 6) reported clinically significant suicidal ideation. There were no significant differences for mean length of stay in the ED for nonpsychiatric patients with positive triggers and those who screened negative (means, 382 [SD, 198] and 393 [SD, 166] minutes, respectively; P = 0.80). Ninety-six percent of participants agreed that suicide screening should occur in the ED.
Conclusions
Suicide screening of nonpsychiatric patients in the ED is feasible in terms of acceptability to parents, prevalence of suicidal thoughts and behaviors, practicality to ED flow, and patient opinion. Future endeavors should address brief screening tools validated on nonpsychiatric populations.
Keywords: suicide, screening, nonpsychiatric patients, feasibility
Youth suicide is an international public health threat. In the United States alone, more than 1200 children and adolescents die by suicide each year.1 Moreover, 1 million children and adolescents attempt suicide annually, and tens of millions more have intrusive thoughts about killing themselves.2 Consequently, 15- to 19-year-olds are the most common age group to present to emergency departments (EDs) with attempted suicide and self-inflicted injury.3
Despite high prevalence and known risk factors, most suicidal adolescents do not access mental health care services. Suicidal adolescents may be less likely to seek help for mental illness,4 and few suicide attempters receive appropriate assessment and follow-up care.5,6 Whereas many children and adolescents at risk for suicide are not identified by mental health providers, many adults and youth who die by suicide visit a nonpsychiatric clinician in the months before their deaths.7-10 In addition, nearly 40% of completed suicides among individuals 16 years and older have visited an ED in the prior year.11 Screening children for suicide risk when they present to the ED with nonpsychiatric complaints could lead to better identification and treatment of high-risk youth.12-16 However, this type of screening is not routine practice.
Screening for public health threats in the ED is a controversial topic. A tension exists between the pressures to treat acute health problems and the desire to prevent future health problems among patients and the community at large.17-19 Emergency department overcrowding is a critical national issue20-22; routine screening for medical and psychiatric conditions imposes additional burdens on efficient ED flow. Conversely, for millions of children and adolescents, the ED is their only contact with health care providers,18 suggesting that it may be uniquely positioned to capture at-risk youth. Nevertheless, mental health screening, of any type, is conducted in less than 10% of ED patients, half of which is prompted solely by chief complaint.23 Successful models of ED-based screening and intervention have been demonstrated in asthma,24 injury,25 and alcohol abuse.26,27
Before suicide screening protocols can be implemented for nonpsychiatric patients in pediatric EDs, it is essential to determine whether such efforts are realistic in this setting, particularly for patients who are not presenting with psychiatric complaints. Although pediatric ED mental health patients are screened for suicide risk,28 and validated tools exist for this population,29 there are currently no suicide screening tools for ED patients admitted for non–mental health–related reasons. In turn, it is not well documented how adolescents with nonpsychiatric complaints and their parents would react to being questioned about suicide during their ED visit. The purpose of this study was therefore to determine the feasibility of screening for suicide risk in nonpsychiatric patients presenting to the pediatric ED. For the purposes of this article, feasibility was assessed in 4 domains:
Acceptability: Would parents of nonpsychiatric patients allow their children to be screened for suicide?
Prevalence: Are suicidal ideation and behavior common enough in an ED nonpsychiatric population to warrant screening?
Practicality: Can nonpsychiatric patients who screen positive for suicide risk be managed effectively without disrupting ED flow?
Patient opinion: Do child and adolescent patients support suicide screening in the ED?
METHODS
Participant Population
We prospectively recruited a convenience sample of patients as part of a larger, cross-sectional study designed to validate an existing suicide screening instrument in patients with psychiatric and nonpsychiatric complaints. Participants aged 10 to 21 years, inclusive, were recruited within an urban, tertiary-care, academic pediatric ED with an annual patient volume exceeding 80,000 in 2009. Exclusion criteria included (1) developmental disability or cognitive impairment, such that the patient was unable to comprehend and answer questions; (2) triage level 1,30 suggesting that the patient was not medically stable enough to be approached; (3) parent or legal guardian was not present for patients younger than 18 years and; (4) parents/guardians and/or patients were non–English speaking. Given that psychiatric patients accounted for only 3% of total annual ED visits, we adopted a strategy of attempting to enroll every eligible psychiatric patient and every second nonpsychiatric patient who entered the ED while study staff was present.
Instruments
Risk of Suicide Questionnaire–Revised
The Risk of Suicide Questionnaire–Revised (RSQ-R) is a 17-item questionnaire based on risk factors for suicide in adolescents, including previous suicide history, suicidal ideation, depression, hopelessness, substance abuse, and social isolation. Included are 4 questions from the validated Risk of Suicide Questionnaire,29 a suicide screening tool routinely used at triage in this ED to assess suicide risk in pediatric patients presenting with psychiatric symptoms.29
Suicidal Ideation Questionnaire
The Suicidal Ideation Questionnaire (SIQ) is a self-reported measure of the severity of suicidal ideation in adolescents.31 Two versions of the SIQ are available, depending on age of participant. For this study, the 30-item SIQ was administered to participants older than 15 years; the 15-item SIQ-JR was administered to participants 14 years or younger. A cutoff of 31 or higher in the SIQ-JR and 41 or higher in the SIQ indicates the presence of clinically significant suicidal ideation warranting further psychiatric evaluation and is often used as a criterion standard in pediatric studies of suicide risk.14,29,31
Procedure
After the triage and initial assessment processes, and although they were in examination rooms waiting to be seen by a physician, participants were administered the RSQ-R, ascertaining suicide risk, followed by the criterion-standard SIQ.31 The 2 instruments were given in succession as part of the larger validation study to create a new suicide screening tool, based on the full 17-item RSQ-R but reduced to the fewest number of items, which could determine suicide risk with high sensitivity and specificity. An additional survey containing items on sociodemographic information, clinical features, and prior health care utilization was also administered, as well as several screening evaluation questions. Participants were told that, if the data collectors had any concerns about their safety, their parents would be notified, and their answers would be shared with the ED clinical staff. A licensed psychologist provided backup support and supervision for the data collectors.
Any nonpsychiatric patient who affirmed any 1 of 9 “trigger” screening questions (eg, any level of current suicidal ideation, past suicidal behavior, or severe depression) or scored positive on the SIQ required a further psychiatric assessment by a member of the ED psychiatric team, which consisted of 1 or 2 dedicated, licensed clinical social workers supervised by an attending psychiatrist. These patients are referred to in this article as “positive triggers.” If a patient screened negative, participation in the study concluded.
Quantitative and Qualitative Analysis
The norms of the SIQ suggest a prevalence rate for suicidal thinking of approximately 10% for a pediatric nonpsychiatric population. A sample size of 150 was calculated based on ensuring sufficient power for the larger, multisite study, which was designed to validate a new screening instrument in a pediatric nonpsychiatric population. The study was not separately powered to address the questions posed here. Data analyses were conducted using SPSS (SPSS Inc, Chicago, Ill). Descriptive statistics and univariate and multivariate analyses are reported.
Human Subjects’ Concerns
This study was approved by the institutional review board at Children’s National Medical Center. Written informed consent was obtained from the parent/guardian, and written informed assent was obtained from participants 17 years or younger. All participants older than 18 years gave informed consent.
RESULTS
Recruitment of Participants
Of the 366 patients approached during the study period, 100 were ineligible because of exclusion criteria (Fig. 1). Reasons for ineligibility included no parent or guardian present (n = 33, 33%), the medical or psychiatric condition of the patient was too severe to approach for consent (n = 26, 26%), language barriers (n =18, 17%), cognitive impairment (n = 16, 16%), or patient presented to the ED in police custody (n = 4, 4%). In cases where the medical, surgical, or psychiatric condition was too severe, a nurse or social worker requested that the data collector not approach the patient.
FIGURE 1.
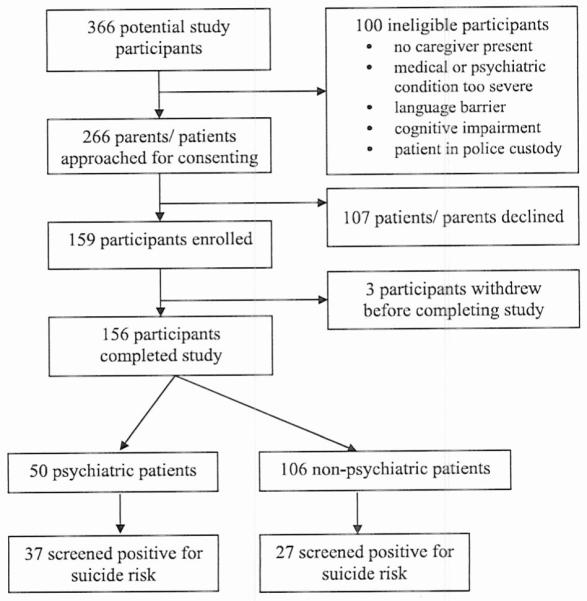
Enrollment of patients.
Acceptability: Would Parents of Nonpsychiatric Patients Allow Their Children to Be Screened for Suicide?
Of the 266 patients who were eligible for participation in the study, 60% (n = 159) agreed to participate. Reasons for declines included concerns that the patient was not in a state to answer questions because of medical symptoms such as pain or fatigue (n = 14, 18%), objections to the parent leaving the room (n = 9, 12%), objections to the nature of the questions (n = 6, 8%), psychiatric symptoms such as acute distress (n = 5, 6%), and concerns that the patient was too young (10 years) to be asked about suicide (n = 3, 4%). There were no significant differences in age or presenting complaint (psychiatric or non-psychiatric) between those who declined and those,who enrolled in the study. It should be noted that 3 patients who initially gave informed consent withdrew from the study: 2 because of discharge from the ED, and 1 withdrew because of procedure interrupting data collection process. Ultimately, 156 patients completed the study. Demographics of study participants are presented in Table 1. The racial and ethnic demographics reflect the patient population treated in this particular pediatric ED.
TABLE 1.
Demographics of Study Participants (n = 156)
| Sex | |
| Male | 68 (43.6%) |
| Female | 88 (56.4%) |
| Race or ethnicity | |
| African American | 104 (66.7%) |
| White | 23 (14.7%) |
| Hispanic/Latino | 8 (5.1%) |
| Mixed/other | 21 (13.5%) |
| Age, mean (SD) | 14.6 (2.76) y |
| 10–11 y | 20 (12.8%) |
| 12–17 y | 108 (69.2%) |
| 18–21 y | 28 (17.9%) |
| Presenting complaint | |
| Medical | 106 (67.9%) |
| Psychiatric | 50 (32.1%) |
Prevalence: Are Suicidal Thoughts and Behaviors Common Enough in an ED Nonpsychiatric Population to Warrant Screening?
Percentages of suicidal ideation and behavior among nonpsychiatric and psychiatric patients are presented in Table 2. Of the 106 nonpsychiatric patients, 27 (25%) were considered to have “positive triggers” and required additional follow-up with psychiatry because of concerns about suicidal ideation or depression. Each of these patients was assessed in real time for suicide risk, according to the ED’s standard of care, which entailed a consultation with a dedicated, licensed ED psychiatric social worker to assess imminent risk of self-harm. The social worker then consulted with the on-call attending psychiatrist to formulate a recommendation for treatment. None of these patients required psychiatric hospitalization. All positive triggers were given a list of psychiatric services available in their local area.
TABLE 2.
Rates of Suicidal Thoughts and Behaviors in the Entire Cohort and Among Psychiatric and Nonpsychiatric Patients Separately
| Total (n = 156) |
Psychiatric Patients (n = 50) |
Nonpsychiatric Patients (n = 106) |
OR (95% CI) | |
|---|---|---|---|---|
| Patients requiring further assessment for suicide risk | 27 (17.3%) | 50 (100%)* | 27 (25%) | N/A |
| SIQ positive | 26 (16.7%) | 20 (40%) | 61† (5.7%) | 7.1 (3.0-16.5) |
| Previous suicide attempt | 20 (12.8%) | 14 (28%) | 6† (5.7%) | 4.9 (2.0-12.1) |
All psychiatric patients presenting to the ED receive a psychiatric consultation.
Not the same 6 patients.
Psychiatric patients were significantly more likely than nonpsychiatric patients to report clinically significant suicidal ideation (40% vs 5.7%, respectively; odds ratio [OR], 7.1; 95% confidence interval [CI], 3.0–16.5). Similarly, psychiatric patients were significantly more likely than nonpsychiatric patients to report previous suicide attempt(s) (28% vs 5.7%, respectively; OR, 4.9; 95% CI, 2.0–12.1).
Six (5.7%) of the nonpsychiatric patients reported clinically significant suicidal ideation (as assessed by the criterion-standard SIQ). There were no significant differences in race, ethnicity, sex, or presence of a chronic medical illness between nonpsychiatric patients who required additional follow-up with psychiatry and those who did not.
Practicality: Can Nonpsychiatric Patients Who Screen Positive for Suicide Risk Be Managed Effectively Without Disrupting ED Workflow?
When a nonpsychiatric patient had a positive trigger response, ED psychiatric staff conducted abbreviated psychiatric evaluations as a result of positive triggers that lasted between 5 and 20 minutes, averaging 12 minutes. Typically, the screening process occurred while patients awaited evaluation by ED physicians. There were no significant differences for mean length of stay in the ED for nonpsychiatric patients with positive triggers and those who screened negative (means, 382 [SD, 198] and 393 [SD, 166] minutes, respectively; P = 0.80].
Patient Opinion: Do Child and Adolescent Patients Support Suicide Screening in the ED?
Responses to screening evaluation questions are presented in Table 3 (see Appendix A for a list of all study evaluation questions). Most respondents supported the notion that nurses should ask children and adolescents in the ED about suicide. At the end of the interview, participants were asked: “What was it like to be asked these questions?” Of the 156 participants, 28 (18%) described the experience as positive, stating that they were relieved to “tell the truth,” talk about something that was “weighing on them,” or that the questions gave them a new perspective that their lives were “not so bad.” Most respondents (103/156 or 66%) gave a neutral response (eg, “fine” or “OK”). Eleven participants (8%) reported that the experience was stressful, and 13 (8%) of 156 reported that it was somewhat “weird” or “awkward.”
TABLE 3.
Answers to Screening Evaluation Questions Among Psychiatric and Nonpsychiatric Patients
| Total (n = 156) |
Psychiatric Patients (n = 50) |
Nonpsychiatric (n = 106) |
Nonpsychiatric Patients Who Screened Positive (n = 27) |
||
|---|---|---|---|---|---|
| Do you think it’s a good idea for nurses to ask kids about suicide in the ER? |
Yes | 149 (96%) | 47 (94%) | 102 (96%) | 26 (96%) |
| Have you ever been asked about suicide before? | Yes | 55 (35%) | 22 (44%) | 33 (31%) | 15 (55%) |
DISCUSSION
Screening both psychiatric and nonpsychiatric patients for suicide risk in a pediatric ED was well received by most patients and their parents and did not result in prolonged ED stays. With minimal disruption to patient flow through the ED and with acceptance by most patients and parents approached, 106 principally minority patients aged 10 to 21 years seen with nonpsychiatric complaints in a busy urban pediatric ED were screened for suicide risk. A quarter of these patients required further evaluation for suicide risk, and 6% revealed clinically significant suicidal ideation. The length of stay for those patients who screened positive was not significantly different than the length of stay for those who screened negative. With respect to all 4 of our stated domains, these results suggest that screening children and adolescents presenting with nonpsychiatric complaints to an ED for suicide risk is feasible.
Acceptability
When this study was first proposed, staff voiced concerns that parents of pediatric patients presenting to an ED would not allow their children to be screened for suicide. Even with each participant being told that any response that indicated suicide risk would be shared with their clinical care team and their parents, most pediatric nonpsychiatric patients were willing to participate and were forthcoming about their suicidal thoughts and past suicidal behaviors. In addition, most parents approached for study enrollment agreed to allow their children to be interviewed about suicidal thoughts and behaviors. Clearly, there are some cases in which severity of medical or surgical illness would preclude suicide screening, and any future protocols for screening will require proper exclusion criteria.
Of note, however, 40% of patients approached declined to be in the study. Most patients or parents declined to participate because they were not interested in the study or because they were concerned about pressing medical or surgical problems. Several of the declines acknowledged the value of screening but were concerned that their child was too young (eg, 10 years old) to be asked about suicide. It may be that if the screening tool was standard of care with appropriate exclusion criteria, the percentage of those declining would be decreased.
Prevalence of Suicidal Ideation and Behavior
Screening is most effective when conducted with populations in which the condition of interest is neither too rare nor too common.32 Our results showed that 25% of the nonpsychiatric patients enrolled required further psychiatric evaluation to assess suicide risk and that 6% of the nonpsychiatric patients reported clinically significant suicidal ideation. Given that medically ill patients are considered a vulnerable population at greater risk for suicidal thoughts and behaviors than their healthier counterparts33-36 and that for many medically ill children, ED visits are their only contact with the health care system, the pediatric ED is a promising venue for capturing youth at risk. In addition, the more common practice of depression screening has been shown to not capture all cases of suicide.33 As suicide risk factors among the nonpsychiatric patient population are still unknown, depression screening alone is not adequate for capturing at-risk pediatric patients in a medical setting.14 There are no reports of iatrogenic harm in asking adolescents about suicide,37 but there is a chance for profound benefit in identifying at-risk youth. In this study, 12 patients identified as at risk for suicide stated that they had never been asked about suicide before; for these youth, the ED stands as the only place that recognized their distress because they were directly asked about suicide.
Practicality
Emergency departments are increasingly challenged by high volumes and high acuity.20-22 Additional screening for medical and/or psychiatric conditions not obviously related to the patients’ presenting complaints may add to these burdens, with negative implications for the efficiency of patient flow through the ED. Our screening procedure, however, lasted only 12 minutes and was generally conducted while the patient was in the examination room awaiting the physician. Overall lengths of stay were unaffected. Nonetheless, given the high and rising rates of adolescent suicide,38 we believe that the high positive yield on the screening process makes the minimal interruption in ED flow worthwhile.
It should be noted that a full psychiatric evaluation was not expected to be completed in the approximately 12-minute psychiatric assessments that was conducted on positive triggers. Rather, this period was utilized to assess imminent risk of self-harm. Nevertheless, the value in even this brief evaluation was to connect the patient with follow-up services if warranted, to allow the patient to discuss distressing thoughts of self-harm and, most importantly, to make the parent aware of potentially unknown suicidal thoughts and behaviors that his/her child may be harboring. Recognition is the critical first step in making an impact.13
Patient Opinion
In addition to concerns over whether parents would find suicide screening in an ED acceptable, it was also unknown how pediatric patients would respond to such screening. There are concerns raised from the research literature and parents that children may be “stressed” by questions about suicide. Most of our sample (66%) gave 1-word responses that are typical for adolescents: “fine” or “OK.” But 18% gave more poignant answers. For example, patients who did affirm suicidal ideation or behavior stated that answering these questions was like “coming out with the truth.” These patients reported that “lots of kids don’t know where to go for help, so they don’t get the help [they need]” or commented on the ease of telling personal fears to a professional/stranger rather than their parents. Interestingly, some patients who were negative for suicide risk reported that hearing the risk questions made them realize that their lives were “not so bad.” A small minority of our sample, 8%, reported feeling “nervous” about being asked. When probed further, they reported feeling uncomfortable by the questions. We believe that although some discomfort may arise, the message conveyed is that suicidal thoughts are taken seriously by the medical profession and can be discussed openly. The final 8% found the questions to be “weird” or “awkward.” However, some of these patients also thought that screening was important. As 1 patient said “[the questions] were kind of weird but might help other kids who have problems.” Child reactions to these questions are hypothesized to be the same as raising other important issues with youth, such as drug use and safe sex practices. Overall, the patient participants in this study deemed such questions as nonburdensome and worthy of being asked of all patients in the ED, regardless of presenting complaint. As 1 child described, “Kids get sad and don’t have anyone to talk about it with, so if a kid is already in the ER and with people who are trained, it’s a good time to talk.”
Currently, pediatric nonpsychiatric patients are typically not asked directly about suicidal thoughts or behaviors. Given that more than 1.5 million adolescents utilize the ED as their primary source of health care,39 the ED visit may be an opportune time to utilize screening. Resistance from an already overburdened health care system without adequate mental health resources might be expected. A brief screening tool that can be administered by nonpsychiatric clinicians to guide assessment would be optimal in the busy ED setting and is currently under development using the larger data set from which these data originate.
LIMITATIONS
Given that this study reports only initial results from a larger study, the small sample size limits our ability to draw conclusions about differences between nonpsychiatric and psychiatric patients in the ED. Participants were assessed by a research team that had time to devote to screening and ensuring follow-up. Once a valid screening tool is developed to assess patients entering the ED, flow and length of stay will need to be assessed in greater detail. Given this is a single-site, specific urban pediatric ED population, generalizability may be limited. A larger data set including non–English-speaking patients and individuals in foster care is recommended for future study.
FUTURE DIRECTIONS
Future studies should focus on pediatric medical patients who screen positive and their adherence to follow-up recommendations. Outcome data on the impact of screening for risk of suicide among children and adolescents in the ED and other settings such as primary care clinics and schools are greatly needed.
CONCLUSIONS
Screening pediatric nonpsychiatric patients for suicide risk proved to be feasible in a large, urban, tertiary-care ED. Mental health resources and effective interventions are essential to responsibly and effectively manage positive screens. Asking pediatric patients directly about suicidal thoughts and behaviors seems valuable. Most likely, children and adolescents are not going to offer up this information without prompting. As one very articulate child subject reported “if you don’t ask them, they may never tell you.”
ACKNOWLEDGMENTS
The authors thank Janet Heekin, Khristine Helfin, the CNMC Emergency Department staff, Angelica Kloos, Rebecca Prengler, Deborah Snyder, David Jobes, Amy Goldstein, Joseph Snow, Jeffrey Bridge, Elizabeth Wharff and Kathryn Ginnis, as well as the patients and their families who participated.
The research for this article was supported by the Intramural Research Program of the National Institutes of Health and the National Institute of Mental Health.
APPENDIX A
Study Evaluation Questions:
Footnotes
The views expressed in this article are the authors’ views and do not necessarily represent the views of the National Institutes of Health, Department of Health and Human Services, or any other government agency or official.
REFERENCES
- 1.National Center for Injury Prevention and Control Web-based Injury Statistics Query and Reporting System. Web site. Available at: http://www.cdc.gov/ncipc/wisqars/default.html. Accessed December 4, 2009.
- 2.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ. 2008;57:1–131. [PubMed] [Google Scholar]
- 3.Doshi A, Boudrcaux ED, Wang N, et al. National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997–2001. Ann Emerg Med. 2005;46(4):369–375. doi: 10.1016/j.annemergmed.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Husky MM, McGuire L, Flynn L, et al. Correlates of help-seeking behavior among at-risk adolescents. Child Psychiatry Hum Dev. 2009;40:15–24. doi: 10.1007/s10578-008-0107-8. [DOI] [PubMed] [Google Scholar]
- 5.Holi MM, Pelkonen M, Karlsson L, et al. Detecting suicidally among adolescent outpatients: evaluation of trained clinicians suicidality assessment against a structured diagnostic assessment made by trained raters. BMC Psychiatry. 2008;8:97–103. doi: 10.1186/1471-244X-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suominen K, Isometsa E, Ostamo A, et al. Level of suicidal intent predicts overall mortality and suicide after attempted suicide: a 12 year follow-up study. BMC Psychiatry. 2004;4:11–18. doi: 10.1186/1471-244X-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan YJ, Lee BM, Chiang HC, et al. The recognition of diagnosablc psychiatric disorders in suicide cases’ last medical contacts. Gen Hosp Psychiatry. 2009;31:181–184. doi: 10.1016/j.genhosppsych.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Frakenfield DL, Keyl PM, Gielen A, et al. Adolescent patients: healthy or hurting? Missed opportunities to screen for suicide risk in the primary care setting. Arch Pediatr Adolesc Med. 200();154:162–168. doi: 10.1001/archpedi.154.2.162. [DOI] [PubMed] [Google Scholar]
- 9.Clark D. Suicidal behavior in childhood and adolescence: recent studies and clinical implications. Psychiatr Ann. 1993;23:271–283. [Google Scholar]
- 10.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry. 2003;183:28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- 12.Horowitz LM, Ballard ED, Pao M. Suicide screening in schools, primary care and emergency departments. Curr Opin Pediatr. 2009;21:620–627. doi: 10.1097/MOP.0b013e3283307a89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pena JB, Caine ED. Screening as an approach for adolescent suicide prevention. Suicide Life Threat Behav. 2006;36:614–637. doi: 10.1521/suli.2006.36.6.614. [DOI] [PubMed] [Google Scholar]
- 14.King CA, O’Mara RM, Hayward CN, et al. Adolescent suicide risk screening in the emergence department. Acad Emerg Med. 2009;16(11):1234–1241. doi: 10.1111/j.1553-2712.2009.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asarnow JR, Baraff LJ, Beck M, et al. Pediatric emergency department suicidal patients: two-site evaluation of suicide ideators, single attempters, and repeat attempters. J Am Acad Child Adolesc Psychiatry. 2008;48:958–966. doi: 10.1097/CHI.0b013e3181799ee8. [DOI] [PubMed] [Google Scholar]
- 16.Grupp-Phelan J, Harman JS, Kelleher KJ. Trends in mental health and chronic condition visits by children presenting for care at US emergency departments. Public Health Rep. 2007;122:55–61. doi: 10.1177/003335490712200108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernstein SL, D’Onofrio G. Public health in the emergency department: Academic Emergency Medicine Consensus Conference executive summary. Acad Emerg Med. 2009;16(11):1037–1039. doi: 10.1111/j.1553-2712.2009.00548.x. [DOI] [PubMed] [Google Scholar]
- 18.McKay MP, Vaca FE, Field C, et al. Public health in the emergency department: overcoming barriers to implementation and dissemination. Acad Emerg Med. 2009;16(11):1132–1137. doi: 10.1111/j.1553-2712.2009.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bernstein SL, Bernstein E, Boudreaux ED, et al. Public health considerations in knowledge translation in the emergency department. Acad Emerg Med. 2007;14:1036–1041. doi: 10.1197/j.aem.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 20.Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. s2000;35(l):63–68. doi: 10.1016/s0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 21.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402–405. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hostetler MA, Mace S, Brown K, et al. Emergency department overcrowding and children. Pediatr Emerg Care. 2007;23(7):507–515. doi: 10.1097/01.pec.0000280518.36408.74. [DOI] [PubMed] [Google Scholar]
- 23.Habis A, Tall L, Smith J, et al. Pediatric emergency medicine physicians’ current practices and beliefs regarding mental health screening. Pediatr Emerg Care. 2007;23:387–393. doi: 10.1097/01.pec.0000278401.37697.79. [DOI] [PubMed] [Google Scholar]
- 24.Teach SJ, Crain EF, Quint DM, et al. Improved asthma outcomes in a high-morbidity pediatric population: results of an emergency department-based randomized clinical trial. Arch Pediatr Adolesc Med. 2006;160:535–541. doi: 10.1001/archpedi.160.5.535. [DOI] [PubMed] [Google Scholar]
- 25.Posner JC, Hawkins LA, Garcia-Espana F, et al. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics. 2004;113:1603–1608. doi: 10.1542/peds.113.6.1603. [DOI] [PubMed] [Google Scholar]
- 26.Dill PL, Wells-Parker E, Soderstrom CA. The emergency care setting for screening and intervention for alcohol use problems among injured and high-risk drivers: a review. Traffic Inj Prev. 2004;5:278–291. doi: 10.1080/15389580490465364. [DOI] [PubMed] [Google Scholar]
- 27.Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473–480. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joint Commission [Accessed December 4, 2009];National Patient Safety Goals Web site. 2010 Available at: www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals. [Google Scholar]
- 29.Horowitz LM, Wang PS, Koochcr GP, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics. 2001;107:1133–1137. doi: 10.1542/peds.107.5.1133. [DOI] [PubMed] [Google Scholar]
- 30.Wuerz RC, Travers D, Gilboy N, et al. Implementation and refinement of the emergency severity index. Acad Emerg Med. 2001;8:170–176. doi: 10.1111/j.1553-2712.2001.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 31.Reynolds W. Suicidal Ideation Questionnaire. Psychological Assessment Resources; Odessa, FL: 1987. [Google Scholar]
- 32.Jakel JF, Katz DL, Elmore JG. Epidemiology, Biostatistics and Preventive Medicine. 2nd ed WB Saunders; Philadelphia, PA: 2001. [Google Scholar]
- 33.Recklitis CJ, Lockwood RA, Rothwell MA, et al. Suicidal ideation and attempts in adult survivors of childhood cancer. J Clin Oncol. 2006;24:3852–3857. doi: 10.1200/JCO.2006.06.5409. [DOI] [PubMed] [Google Scholar]
- 34.Goodwin RD, Marusic A. Asthma and suicidal ideation among youth in the community. Crisis. 2004;25:99–102. doi: 10.1027/0227-5910.25.3.99. [DOI] [PubMed] [Google Scholar]
- 35.Goodwin RD. Diabetes and suicidal ideation among youth in the community. Arch Pediatr Adolesc Med. 2002;156:841. doi: 10.1001/archpedi.156.8.841. [DOI] [PubMed] [Google Scholar]
- 36.Robins LN, Report of the Secretary’s Task Force on Youth Suicide . Strategies for the Prevention of Youth Suicide. Vol. 4. US Government Printing Office; Washington, DC: 1989. Suicide attempts in teen-aged medical patients. DHHS Publication ADM89-1624. [Google Scholar]
- 37.Gould MS, Morrocco FA, Kleinman M, et al. Evaluating iatrogenic risk of youth suicide programs: a randomized control trial. JAMA. 2005;293:1635–1643. doi: 10.1001/jama.293.13.1635. [DOI] [PubMed] [Google Scholar]
- 38.Bridge JA, Greenhouse JB, Weldon AH. Suicide trends among youths aged 10 to 19 years in the United States, 1996–2005. JAMA. 2008;300(9):1025–1026. doi: 10.1001/jama.300.9.1025. [DOI] [PubMed] [Google Scholar]
- 39.Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolese Med. 2000;154:361–365. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]