Abstract
Background:
Revision anterior cruciate ligament (ACL) reconstruction is believed to have an inferior outcome compared with primary ACL reconstruction. The available literature on the outcome of revision ACL reconstruction is sparse compared with that for primary reconstruction. The purpose of this systematic review was to test the hypothesis that the outcome of revision ACL reconstruction compares unfavorably with the historical outcome of primary ACL reconstruction.
Methods:
A systematic review of studies evaluating the outcome of revision ACL reconstructions with a minimum of two years of follow-up was performed. Pooled data were collected when appropriate and a mixed-effect-model meta-analysis was performed for important outcome measures that were reported in several studies (objective graft failure, Lysholm score, International Knee Documentation Committee [IKDC] subjective score, and IKDC objective score). Objective failure was defined as repeat revision, a side-to-side difference of >5 mm measured with use of a KT1000 arthrometer, or a pivot-shift grade of 2+ or 3+.
Results:
Twenty-one studies were included, and 863 of the 1004 patients in these studies had a minimum of two years of follow-up and were analyzed. The pooled mean age of the patients at the time of the revision procedure was 30.6 years, and 66% were male. Objective failure occurred in 13.7% ± 2.7% of the patients (95% confidence interval, 8.0% to 19.4%). The mean Lysholm score in 491 patients was 82.1 ± 3.3 (95% confidence interval, 74.6 to 89.5) according to a mixed-model meta-analysis. The mean IKDC subjective score in 202 patients was 74.8 ± 4.4 (95% confidence interval, 62.5 to 87.0).
Conclusions:
Revision ACL reconstruction resulted in a worse outcome compared with primary ACL reconstruction. Patient-reported outcome scores were inferior to previously published results of primary ACL reconstruction, but these differences may not be clinically important. A dramatically elevated failure rate was noted after revision ACL reconstruction; this rate was nearly three to four times the failure rate in prospective series of primary ACL reconstructions.
Graft failure is a devastating outcome for patients who have undergone an anterior cruciate ligament (ACL) reconstruction. The physical demands associated with the surgical procedure, the time and energy invested in a prolonged rehabilitation program, and the emotional challenges associated with the altered activity level during the six-month or longer rehabilitation period can be daunting to a patient who is faced with needing a revision ACL reconstruction. Additionally, the general belief among orthopaedic surgeons is that outcomes after revision ACL reconstruction are worse than those after primary ACL reconstruction. This belief is based on anecdotal evidence and on outcomes reported in the literature1-8. Recently, this belief was also found to be the consensus view among a current group of surgeons involved in the Multi-center ACL Revision Study (MARS), which is a multi-surgeon, multi-center, prospective longitudinal cohort study that is currently enrolling patients9.
The number of studies evaluating the outcome of revision ACL reconstruction is miniscule compared with the number evaluating primary reconstruction7. Most of the literature on revision ACL reconstruction is related to technical aspects of performing the revision. The studies evaluating the outcome of revision ACL reconstruction have typically involved small numbers of patients and had a low level of evidence. We undertook the present systematic review and meta-analysis to provide an objective analysis of revision ACL reconstruction by examining multiple smaller studies in which homogeneous outcomes had been measured. Our hypothesis was that the outcome of revision ACL reconstruction would compare unfavorably with the historical outcome of primary ACL reconstruction. Better objective evidence regarding the outcome of revision ACL reconstruction will provide a baseline for comparison with future studies that attempt to achieve improved outcomes, and it will also facilitate improved counseling of patients regarding the expected outcome of revision ACL reconstruction.
Materials and Methods
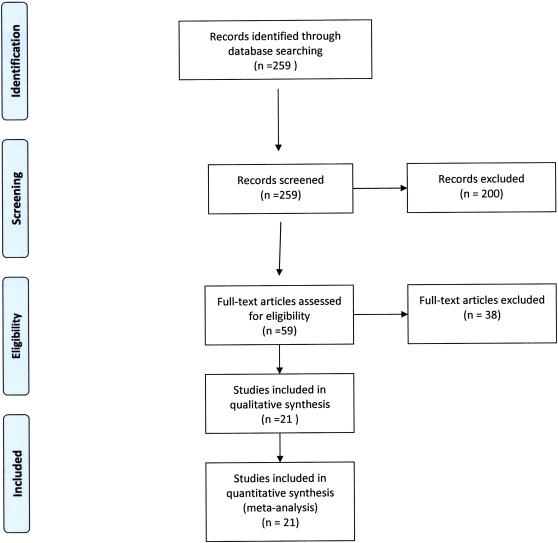
This systematic review and meta-analysis was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) format10. We performed an electronic search of the published literature by searching the PubMed database from 1966 through 2010, the Embase database from 1980 through 2010, and the Cochrane Controlled Trials Register from its inception through 2010 for papers appropriate to this study. The bibliographies of all identified studies were also searched, and a manual review of the last six months of appropriate journals (The American Journal of Sports Medicine, The Journal of Bone and Joint Surgery [American and British Volumes], Clinical Orthopaedics and Related Research, Arthroscopy, and The Journal of Knee Surgery) was performed. Terms for the database searches included anterior cruciate ligament or ACL and revision or redo. These searches identified 259 potentially eligible studies (Fig. 1).
Fig. 1.
PRISMA 2009 flow diagram for the meta-analysis and systematic review.
A study that reported the outcome of revision ACL reconstruction was potentially eligible for inclusion in the systematic review if the duration of follow-up was at least two years and the study was peer-reviewed and in the English language. Technical reviews, case reports, studies in a language other than English, studies that lacked peer review, and studies with less than two years of follow-up were excluded.
Review of the abstracts of the identified studies reduced the number of potentially eligible studies to fifty-nine. The full text of these articles was reviewed independently by three of the authors (R.W.W., C.S.G., and N.A.M.), and twenty-one studies were found to meet the inclusion criteria for this systematic review and meta-analysis. These studies underwent data extraction of demographic and outcome measures as well as quality appraisal by the same three authors. CONSORT (Consolidated Standards of Reporting Trials) and STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklists for the appropriate type of study were utilized for the analysis. Pooled data were collected when appropriate and a mixed-effect-model meta-analysis was performed for important outcome measures that were reported in several studies (objective graft failure, the Lysholm score, the International Knee Documentation Committee (IKDC) subjective score, and the IKDC objective score) by a statistician (L.C.) to take into account study differences and data complexity.
Results
The twenty-one studies originally included 1004 patients1,4,8,11-28 (see Appendix). The Level of Evidence (as determined with use of The Journal of Bone and Joint Surgery guidelines) was Level I or II for four studies, Level III for one, and Level IV for sixteen. A total of 863 patients (86.0%) had at least two years of follow-up. The percentage of patients with adequate follow-up ranged from 66% to 100%, with only one study having <70% patient follow-up. The duration of follow-up of the individual patients ranged from two to eighteen years, and the pooled mean duration of follow-up was 5.4 years. The duration of follow-up in any individual study did not impact our comparisons or conclusions regarding outcome measures.
Not all studies reported information on the patient age and sex distributions. On the basis of the available information, the pooled mean age of the patients at the time of revision was 30.6 years and 66% were male. The time from the previous ACL reconstruction to the revision reconstruction was reported for 607 patients and averaged 4.6 years (fifty-five months). The number of revisions was reported for 140 patients, and 30% were undergoing a second or subsequent revision.
The previous graft material was reported for 495 patients; 86.1% had an autograft, 5.5% had an allograft, and 8.5% had had a synthetic graft. The cause of the previous graft failure was reported for 511 patients and was a technical error in 45.8%, a traumatic reinjury in 49.3%, and biological factors in 4.9% (Table I). The graft choice for the revision was reported for 766 patients. Autograft was used in 89.4% (685) and consisted of bone-patellar tendon-bone in 48%, hamstring in 40%, and quadriceps tendon in 12%.
TABLE I.
Reported Etiology of Failure of the Previous Reconstruction*
| Cause | % |
| Technical error | 45.8 |
| Traumatic reinjury | 49.3 |
| Biological factors | 4.9 |
This information was available for 511 patients.
Prior meniscectomy was reported to have been performed at the time of the previous ACL reconstruction in 53.5% of 383 patients and was medial in 71.9% and lateral in 28.9% (Table II). Prior meniscal repair was reported to have been performed at the time of the previous ACL reconstruction in 20.8% of 212 patients. Meniscectomy was reported to have been performed at the time of the revision in 55.6% of 554 patients, and 64% of the meniscectomies were partial medial meniscectomies. Meniscal repair was reported to have been performed at the time of the revision in 14.3% of 407 patients. The articular cartilage was reported to have been damaged at the time of the revision in 56.2% of 393 patients. In the patients noted to have articular cartilage damage, the chondrosis was Grade 1 in 34.1%, Grade 2 in 44.8%, Grade 3 in 17.6%, and Grade 4 in 3.4%; the compartment involved was the medial in 29.1%, the lateral in 37.5%, and the patellofemoral in 33.3% (Table III).
TABLE II.
Reported Concomitant Meniscal Treatment
| Previous ACL Reconstruction | Revision ACL Reconstruction | |
| Meniscectomy | 53.5% of 383 patients | 55.6% of 554 patients |
| Medial | 71.9% | 64% |
| Lateral | 28.9% | 36% |
| Meniscal repair | 20.8% of 212 patients | 14.3% of 407 patients |
TABLE III.
Reported Articular Cartilage Damage at the Time of the Revision ACL Reconstruction*
| % | |
| Grade | |
| 1 | 34.1 |
| 2 | 44.8 |
| 3 | 17.6 |
| 4 | 3.4 |
| Location of damage | |
| Medial | 29.1 |
| Lateral | 37.5 |
| Patellofemoral | 33.3 |
Damage was present in 56.2% of the 393 patients for which the cartilage status was reported.
A variety of outcome measures were reported postoperatively. The Cincinnati score was reported in 109 patients, and the pooled mean was 81 (range, 68 to 89). The Tegner score was reported in 299 patients, and the mean was 6.1. Mixed-model meta-analysis was performed for the Lysholm score in 491 patients; the mean (and standard deviation) was 82.1 ± 3.3 and the corresponding 95% confidence interval (CI) was 74.6 to 89.5. The IKDC subjective score was 74.8 ± 4.4 (95% CI, 62.5 to 87.0) in 202 patients. The IKDC objective score was reported as A (normal), B (nearly normal), C (abnormal), or D (severely abnormal) in some of the included studies and as AB or CD in others. In the studies that reported all four scores separately, the IKDC grade was A in 28.7% ± 4.8% (95% CI, 17.8% to 39.6%), B in 46.2% ± 3.2% (95% CI, 39.2% to 53.2%), C in 18.7% ± 2.9% (95% CI, 12.2% to 25.2%), and D in 5.1% ± 2.5% (95% CI, 0.0% to 10.6%). Two studies reported only combined AB and CD scores. Combining these studies with the studies that reported all four scores separately, the IKDC score was A or B in 71.1% ± 5.4% (95% CI, 59.3% to 82.8%) and C or D in 28.9% ± 5.4% (95% CI, 17.2% to 40.6%). Objective failure (defined as repeat revision, a side-to-side difference of >5 mm measured with use of a KT1000 arthrometer (MEDmetric, San Diego, California), or a pivot-shift grade of 2+ or 3+) occurred in 13.7% ± 2.7% (95% CI, 8.0% to 19.4%).
Satisfaction was reported in 275 patients but the definition of satisfaction varied among the studies. Satisfaction was typically determined simply by asking the patients whether they were satisfied with the outcome, and 80% indicated that they were. Return to unrestricted activities or to the previous level of activity was reported in only 54% of 485 patients.
Discussion
Orthopaedic surgeons typically believe that revision ACL reconstruction results in a worse outcome compared with primary ACL reconstruction. This impression has been based on studies that typically have a low Level of Evidence and involve a small number of patients. Given the relative infrequency of revision ACL reconstruction in any single surgeon's practice, it is difficult to obtain a large enough sample size in a reasonable time frame to allow appropriate analysis. The small number of patients also limits the ability to appropriately perform a randomized clinical trial in a timely fashion. Our goal in this systematic review and meta-analysis was to determine the overall results across a series of studies in order to compare these results with the reported results of primary ACL reconstruction, to better inform patients of expected outcomes, and to guide our future research.
Pooled demographic data were compared with data for the first 460 patients in the Multi-center ACL Revision Study (MARS) cohort9. MARS is a multi-surgeon, multi-center, prospective longitudinal cohort study that began enrolling patients in 20069. Demographics in the two studies were similar, with some small differences. The median age of the patients in the MARS cohort was twenty-six years compared with a pooled mean age of 30.6 years in the present systematic review. In addition, the percentage of male patients was 57% in the MARS cohort compared with 66% in the present study. The lower percentage of male patients in the MARS cohort may reflect changes in the population of patients with an ACL injury between the time of the studies included in the present review and the time of patient enrollment in the MARS study. It may also reflect increased female participation in sports since the institution of Title IX rules. Autograft had been chosen for the previous ACL reconstruction in 70% of the patients in the MARS cohort compared with 86.1% in the present study. Autograft was chosen for the revision ACL reconstruction in 45% of the patients in the MARS cohort compared with 89.4% in the current study. Forty percent of the patients in the MARS cohort had sustained a new medial meniscal tear and 35% had sustained a new lateral meniscal tear compared with 69.9% who had a new medial or lateral tear in the current study.
One of our goals was to compare the pooled results of revision ACL reconstruction with those of large prospective studies and systematic reviews of primary ACL reconstruction that used the same outcome measures (Table IV). Not all of the studies included in our meta-analysis used identical outcomes measures, and we were therefore able to pool only a portion of the studies for each scoring tool. Both the mean Cincinnati score and the mean Lysholm score were lower after revision ACL reconstruction than after primary reconstruction. A systematic review by Spindler et al. compared the use of hamstring autograft with patellar tendon autograft in nine studies of primary ACL reconstruction29. The mean Cincinnati scores in the studies included in that meta-analysis ranged from 86 to 94 compared with 81 in our study. Five studies in the review by Spindler et al. also evaluated the results with use of the Lysholm score; the mean score was 85 in one study and >90 in the other four compared with 82.1 in our study. A validated minimal clinically important difference has not been established for the Lysholm score, but an eight-point difference likely trends toward a clinically important difference between the two groups30,31. Furthermore, the mean IKDC subjective score in the MOON (Multicenter Orthopaedic Outcomes Network) primary ACL reconstruction cohort was 8432 compared with 74.8 in the mixed-model meta-analysis in the present study. It has been established previously that an 11.5-point change in the IKDC subjective score represents the minimal clinically important difference33. Thus, the 9.2-point difference between these two studies approaches a clinically important difference between the patient-reported results of primary and revision ACL reconstruction.
TABLE IV.
Comparison of the Current Systematic Review with the MARS and MOON ACL Reconstruction Cohorts
| Current Systematic Review | MARS Revision ACL Reconstruction Cohort | MOON Primary ACL Reconstruction Cohort | |
| Pooled mean age (yr) | 30.6 | 26 | |
| Male sex | 66% | 57% | |
| Autograft used for previous ACL reconstruction | 86.1% | 70% | |
| Autograft used for revision ACL reconstruction | 89.4% | 45% | |
| IKDC subjective score* | 74.8 | 84 | |
| Objective failure rate | 13.7% | 2.9% |
IKDC = International Knee Documentation Committee.
The objective failure rate after revision ACL reconstruction in the present study was 13.7% compared with 3.67% after primary ACL reconstruction in the prospective studies analyzed by Spindler et al.29. The failure rate after primary ACL reconstruction was 2.9% at two years of follow-up in the MOON cohort34 and 5.8% at a minimum of five years of follow-up in a recent systematic review35. Thus, the failure rate after revision ACL reconstruction in the present meta-analysis of twenty-one studies with a minimum of two years of follow-up was nearly three to four times that after primary ACL reconstruction.
Our study has many strengths and a few limitations. We were able to perform a mixed-model meta-analysis that pooled results across several studies, adding power to our findings and making them more generalizable for sports medicine physicians and their patients. We were able to do this for important clinical outcome measures including objective graft failure and the IKDC objective, IKDC subjective, Lysholm, and Cincinnati outcome measures. Strict inclusion and exclusion criteria allowed us to narrow our review to those papers that measured the outcomes of interest at a minimum of two years of follow-up.
One of the limitations involved the quality of the included studies, which represented primarily retrospective Level-IV evidence, with all of the shortcomings associated with retrospective case series. This review would have been much stronger if more Level-I and II studies had been available for inclusion. Another limitation was the heterogeneity of the twenty-one included studies, which varied in surgical technique and in the outcomes that were measured. This limited our ability to pool the studies in a way that allowed us to analyze predictors of the outcome. Nevertheless, the choice of graft material was surprisingly homogeneous, with 89.4% of the patients having undergone revision ACL reconstruction with use of autograft. These limitations demonstrate the need for future prospective longitudinal cohort studies and randomized trials.
In summary, a systematic review and mixed-model meta-analysis demonstrated that revision ACL reconstruction resulted in a worse outcome compared with primary ACL reconstruction, as assessed with a variety of measures. Patient-reported outcomes were inferior, although the differences may not have been clinically important. A dramatically elevated failure rate was noted after revision ACL reconstruction; this rate was nearly three to four times that in prospective studies of primary ACL reconstruction. Prospective studies of revision ACL reconstruction will be necessary to determine whether this elevated failure rate persists despite our increasing knowledge of the technical aspects of revision reconstruction.
Supplementary Material
A table summarizing the characteristics of the included studies
Acknowledgments
Note: This publication was made possible by Grant Number UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. The authors thank Linda Burnworth for editorial assistance.
Footnotes
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Johnson DL, Swenson TM, Irrgang JJ, Fu FH, Harner CD. Revision anterior cruciate ligament surgery: experience from Pittsburgh. Clin Orthop Relat Res. 1996;325:100-9 [DOI] [PubMed] [Google Scholar]
- 2.Noyes FR, Barber-Westin SD. Revision anterior cruciate ligament surgery: experience from Cincinnati. Clin Orthop Relat Res. 1996;325:116-29 [DOI] [PubMed] [Google Scholar]
- 3.Uribe JW, Hechtman KS, Zvijac JE, Tjin-A-Tsoi EW. Revision anterior cruciate ligament surgery: experience from Miami. Clin Orthop Relat Res. 1996;325:91-9 [DOI] [PubMed] [Google Scholar]
- 4.Wirth CJ, Kohn D. Revision anterior cruciate ligament surgery: experience from Germany. Clin Orthop Relat Res. 1996;325:110-5 [DOI] [PubMed] [Google Scholar]
- 5.Getelman MH, Friedman MJ. Revision anterior cruciate ligament reconstruction surgery. J Am Acad Orthop Surg. 1999;7:189-98 [DOI] [PubMed] [Google Scholar]
- 6.George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2026-37 [DOI] [PubMed] [Google Scholar]
- 7.Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199-217 [DOI] [PubMed] [Google Scholar]
- 8.Wright RW, Dunn WR, Amendola A, Andrish JT, Flanigan DC, Jones M, Kaeding CC, Marx RG, Matava MJ, McCarty EC, Parker RD, Vidal A, Wolcott M, Wolf BR, Spindler KP; MOON Cohort Anterior cruciate ligament revision reconstruction: two-year results from the MOON cohort. J Knee Surg. 2007;20:308-11 [DOI] [PubMed] [Google Scholar]
- 9.MARS Group, Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, Stuart MJ. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38:1979-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22:128, author reply [DOI] [PubMed] [Google Scholar]
- 11.Battaglia MJ, 2nd, Cordasco FA, Hannafin JA, Rodeo SA, O'Brien SJ, Altchek DW, Cavanaugh J, Wickiewicz TL, Warren RF. Results of revision anterior cruciate ligament surgery. Am J Sports Med. 2007;35:2057-66 [DOI] [PubMed] [Google Scholar]
- 12.Carson EW, Anisko EM, Restrepo C, Panariello RA, O'Brien SJ, Warren RF. Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. J Knee Surg. 2004;17:127-32 [DOI] [PubMed] [Google Scholar]
- 13.Colosimo AJ, Heidt RS, Jr, Traub JA, Carlonas RL. Revision anterior cruciate ligament reconstruction with a reharvested ipsilateral patellar tendon. Am J Sports Med. 2001;29:746-50 [DOI] [PubMed] [Google Scholar]
- 14.Denti M, Lo Vetere D, Bait C, Schönhuber H, Melegati G, Volpi P. Revision anterior cruciate ligament reconstruction: causes of failure, surgical technique, and clinical results. Am J Sports Med. 2008;36:1896-902 [DOI] [PubMed] [Google Scholar]
- 15.Diamantopoulos AP, Lorbach O, Paessler HH. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36:851-60 [DOI] [PubMed] [Google Scholar]
- 16.Ferretti A, Conteduca F, Monaco E, De Carli A, D'Arrigo C. Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am. 2006;88:2373-9 [DOI] [PubMed] [Google Scholar]
- 17.Fox JA, Pierce M, Bojchuk J, Hayden J, Bush-Joseph CA, Bach BR., Jr Revision anterior cruciate ligament reconstruction with nonirradiated fresh-frozen patellar tendon allograft. Arthroscopy. 2004;20:787-94 [DOI] [PubMed] [Google Scholar]
- 18.Garofalo R, Djahangiri A, Siegrist O. Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy. 2006;22:205-14 [DOI] [PubMed] [Google Scholar]
- 19.Grossman MG, ElAttrache NS, Shields CL, Glousman RE. Revision anterior cruciate ligament reconstruction: three- to nine-year follow-up. Arthroscopy. 2005;21:418-23 [DOI] [PubMed] [Google Scholar]
- 20.Lidén M, Ejerhed L, Sernert N, Bovaller A, Karlsson J, Kartus J. The course of the patellar tendon after reharvesting its central third for ACL revision surgery: a long-term clinical and radiographic study. Knee Surg Sports Traumatol Arthrosc. 2006;14:1130-8 [DOI] [PubMed] [Google Scholar]
- 21.Noyes FR, Barber-Westin SD. Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am. 2001;83:1131-43 [DOI] [PubMed] [Google Scholar]
- 22.Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med. 2006;34:553-64 [DOI] [PubMed] [Google Scholar]
- 23.O'Neill DB. Revision arthroscopically assisted anterior cruciate ligament reconstruction with previously unharvested ipsilateral autografts. Am J Sports Med. 2004;32:1833-41 [DOI] [PubMed] [Google Scholar]
- 24.O'Shea JJ, Shelbourne KD. Anterior cruciate ligament reconstruction with a reharvested bone-patellar tendon-bone graft. Am J Sports Med. 2002;30:208-13 [DOI] [PubMed] [Google Scholar]
- 25.Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K. Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5- to 9-year follow-up. Am J Sports Med. 2006;34:1604-14 [DOI] [PubMed] [Google Scholar]
- 26.Thomas NP, Kankate R, Wandless F, Pandit H. Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med. 2005;33:1701-9 [DOI] [PubMed] [Google Scholar]
- 27.Weiler A, Schmeling A, Stöhr I, Kääb MJ, Wagner M. Primary versus single-stage revision anterior cruciate ligament reconstruction using autologous hamstring tendon grafts: a prospective matched-group analysis. Am J Sports Med. 2007;35:1643-52 [DOI] [PubMed] [Google Scholar]
- 28.Woods GW, Fincher AL, O'Connor DP, Bacon SA. Revision anterior cruciate ligament reconstruction using the lateral third of the ipsilateral patellar tendon after failure of a central-third graft: a preliminary report on 10 patients. Am J Knee Surg. 2001;14:23-31 [PubMed] [Google Scholar]
- 29.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986-95 [DOI] [PubMed] [Google Scholar]
- 30.Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17:31-9 [DOI] [PubMed] [Google Scholar]
- 31.Wright RW. Knee sports injury outcome measures. J Knee Surg. 2005;18:69-72 [DOI] [PubMed] [Google Scholar]
- 32.Dunn WR, Spindler KP; MOON Consortium Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38:2040-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, Shelbourne KD; International Knee Documentation Committee Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34:1567-73 [DOI] [PubMed] [Google Scholar]
- 34.Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131-4 [DOI] [PubMed] [Google Scholar]
- 35.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years following ACL reconstruction: a systematic review. JBJS. 2011;93:1159-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A table summarizing the characteristics of the included studies