Abstract
Background
In this study, pretargeted immuno-positron-emission tomography [PET] with a bispecific monoclonal anti-carcinoembryonic antigen [CEA] (CEACAM5) × anti-hapten antibody (bispecific monoclonal antibody [bsmAb]) and a small (1.5 kD) peptide labeled with 68Ga was compared to fludeoxyglucose [18F-FDG]-PET for detecting intraperitoneal [i.p.] CEA-expressing human colonic tumor xenografts in nude mice.
Methods
Two groups of female BALB/c nude mice were inoculated with LS174T human colonic tumor cells i.p. One group received 5 MBq 18F-FDG, and the other received intravenous injections of the bsmAb, followed 16 h later with 5 MBq of 68Ga-labeled peptide. One hour after the radiolabeled peptide or FDG was given, micro-PET/computed tomography images were acquired. Thereafter, the uptake of the 68Ga or 18F in dissected tissue was determined.
Results
Within 1 h, high uptake of the 68Ga-labeled peptide in the tumor lesions (23.4 ± 7.2% ID/g) and low background activity levels were observed (e.g., tumor-to-intestine ratio, 58 ± 22). This resulted in a clear visualization of all intra-abdominal tumor lesions ≥ 10 μL and even some tumors as small as 5 μL (2 mm diameter). 18F-FDG efficiently localized in the tumors (8.7 ± 3.1% ID/g) but also showed physiological uptake in various normal tissues (e.g., tumor-to-intestine ratio, 3.9 ± 1.1).
Conclusions
Pretargeted immuno-PET with bsmAb and a 68Ga-labeled peptide could be a very sensitive imaging method for imaging colonic cancer, disclosing occult lesions.
Keywords: colorectal cancer, carcinoembryonic antigen, imaging, PET, pretargeting, bispecific antibodies
Background
Colorectal cancer is a frequently diagnosed cancer type. It is the third most common cancer in both men and women in the Western world [1,2]. The overall 5-year survival is 40% to 60% [3,4]. The prognosis is mainly determined by the presence of local or distant metastases, especially in the liver and peritoneum, which occur in half of the patients. Only patients with a limited number of liver or lung metastases have a chance for cure by extensive surgery, generally combined with chemotherapy. However, up to half of the patients selected for metastasectomy have inoperable disease at laparotomy [5]. Therefore, preoperative staging for detecting extrahepatic disease is crucial to avoid futile major surgery [6].
Specific detection of malignant colorectal tumor lesions could be achieved by (pretargeted) antibody-guided radionuclide imaging. The combination of the specificity of antibody targeting and the sensitivity of positron-emission tomography [PET] is very promising. Radiolabeled antibodies have been tested for the detection of several cancer types. However, imaging with radiolabeled whole antibodies requires a relatively long interval between injection and imaging acquisition for adequate contrast to develop due to the slow accretion of intact antibodies in tumors and their slow clearance [7]. Pretargeting techniques were developed to improve radioimmunotargeting of tumors [8]. A two-step pretargeting method using bispecific monoclonal antibodies [bsmAb] has been developed. First, an unlabeled bsmAb with affinity for both the tumor and a small radiolabeled molecule is injected. When the bsmAb has cleared from the blood and has accumulated in the tumor, a radiolabeled and hapten-conjugated peptide that clears rapidly from the blood and the body but is trapped in the tumor by the anti-hapten binding arm of the bsmAb is administered [9-11]. Such a pretargeting method allows imaging within 1 h after the injection of the radiolabeled peptide, with high contrast, in animal models.
Coupling two haptens together improves peptide uptake and stability by a process known as affinity enhancement [12]. Chelate-metal complexes, such as DTPA-In, have been used as haptens [13].
Fludeoxyglucose [FDG]-PET/computed tomography [CT] has an established role in the work-up of patients with metastasized colorectal cancer and could change patient management in > 25% of patients [14-16]. Other clinical indications for PET scanning in patients with colorectal cancer are the detection of disease recurrence and characterization of undefined lesions on conventional imaging [17-20]. However, since FDG is a nonspecific tracer, it also has uptake in other tissues (e.g., physiological uptake in the bowel and uptake in (postsurgical) inflammatory or infectious lesions). FDG-PET frequently causes diagnostic dilemmas in assessing peritoneal disease [21-24].
In the present study, we examined the sensitivity of pretargeting with a bispecific monoclonal anti-carcinoembryonic antigen [CEA] × antihistamine-succinyl-glycine [HSG] antibody, TF2, and a 68Ga-labeled peptide, IMP288. Pretargeted immuno-PET was compared to 18F-FDG-PET in a preclinical orthotopic model in mice with small, intraperitoneally growing CEA-expressing colonic tumor lesions.
Methods
Pretargeting reagents TF2 and IMP288
The bsmAb, TF2, and the peptide IMP288 were provided by Immunomedics (Morris Plains, NJ, USA). The preparation of TF2 and binding properties has previously been described [25-29]. Gel filtration chromatography showed that TF2 bound > 90% of 68Ga-IMP288 peptide. IMP288 was synthesized and purified as described by McBride et al. [30]. IMP288 is a DOTA-conjugated D-Tyr-D-Lys-D-Glu-D-Lys tetrapeptide in which both lysine residues are substituted with an HSG moiety via their ε-amino group: 7,10-tetraazacyclododecane-N, N',N″,N″'-tetraacetic acid [DOTA]-D-Tyr-D-Lys(HSG)-D-Glu-D-Lys(HSG)-NH2.
TF2 was labeled with 125I (PerkinElmer, Waltham, MA, USA) by the iodogen method as described previously [31] to a specific activity of 58 MBq/nmol. 125I-labeled TF2 was purified by eluting the reaction mixture with phosphate-buffered saline [PBS] and 0.5% w/v bovine serum albumin [BSA] (Sigma Chemicals, Sigma-Aldrich Corporation, St. Louis, MO, USA) on a PD-10 column (GE Healthcare Bio-Sciences AB, Uppsala, Sweden). IMP288 was labeled with 68Ga as described previously [32]. Radiolabeling and purification for administration could be accomplished within 45 min. The final product was adjusted to have a specific activity of 20 MBq/nmol at the moment of injection. 18F-FDG was obtained from B.V. Cyclotron VU, Amsterdam, The Netherlands.
Quality control of the radiolabeled preparations
Radiochemical purity of the radiolabeled TF2 and IMP288 preparations was determined as described previously [32]. In all experiments, the radiochemical purity of 125I-TF2 and 68Ga-IMP288 preparations exceeded 95%.
Animal experiments
All studies were approved by the Institutional Animal Welfare Committee of the Radboud University Nijmegen Medical Centre and conducted in accordance with their guidelines (revised Dutch Act on Animal Experimentation, 1997). Animals were accustomed to laboratory conditions for 1 week before use and housed in individually ventilated isolator cages under standard laboratory conditions (temperature, 20°C to 24°C; relative humidity, 50% to 60%; and light-dark cycle, 12 h) with free access to animal chow and water.
Female nude BALB/c mice (6 to 8 weeks old), weighing 20 to 25 g, received an intraperitoneal injection of 0.5 mL of a suspension of 1 × 106 LS174T cells, a CEA-expressing human colon carcinoma cell line (CCL-188; passage 7; American Type Culture Collection, Manassas, VA, USA). Three weeks after tumor cell inoculation, one group of five mice was injected intravenously with 5.0 nmol TF2 (0.2 mL) labeled with a trace amount of 125I (0.4 MBq). Sixteen hours later, 68Ga-IMP288 (5 MBq/025 nmol) was administered intravenously in 0.2 mL as described previously [32]. The other group of five mice received 5 MBq 18F-FDG intravenously [i.v.]. The mice were fasted for 10 h before the 18F-FDG injection, anesthetized, and kept warm at 37°C. The mice were euthanized 1 h after the injection of 68Ga-IMP288 or 18F-FDG by CO2/O2 asphyxiation, followed by cardiac puncture to obtain blood.
PET/CT scans of the mice were acquired 1 h after the injection of 68Ga-IMP288 or 18F-FDG with an Inveon animal PET/CT scanner (Siemens Preclinical Solutions, Erlangen, Germany) having an intrinsic spatial resolution of 1.5 mm [33]. The animals were placed in a supine position. PET scans were acquired for 15 min, preceded by CT scans for anatomical reference (spatial resolution, 113 μm; 80 kV; 500 μA; exposure time, 300 ms). Scans were reconstructed using Inveon Acquisition Workplace software (version 1.5; Siemens Preclinical Solutions) using a three-dimensional ordered subset expectation maximization/maximum a posteriori algorithm with the following parameters: matrix, 256 × 256 × 159; pixel size, 0.43 × 0.43 × 0.8 mm3; and maximum a posteriori prior β 0.5.
After the scans, the mice were dissected, and the abdomen was systematically and meticulously examined for tumors. The location of each lesion was documented, weighed, and measured, and then the activity in each lesion was determined in a gamma counter. The other organs of interest were weighed and counted in a gamma counter with standards prepared from the injected products, using appropriate energy windows for the radionuclide of interest. The percentage of the injected dose per gram tissue [% ID/g] was calculated. The correlation between the weight and uptake of 125I-TF2 as 68Ga-IMP288 per lesion was calculated.
Immunohistochemical analysis of CEA was performed on 4-μm-thick formalin-fixed, paraffin-embedded tissue sections. The sections were deparaffinized in xylol and rehydrated through a graded ethanol into water series. To block endogenous peroxidase, slides were blocked with 3% hydrogen peroxide in phosphate buffered saline (10 min at room temperature). Then sections were blocked with 20% normal goat serum (Vector Laboratories Inc., Burlingame, USA) in 1% BSA-PBS (30 min at room temperature [RT]). Subsequently, tumor sections were incubated with a 1:12,000 dilution of polyclonal rabbit anti-CEA antibody (A0115, Dako, Glostrup, Denmark) overnight at 4°C, followed by incubation with a goat-anti-rabbit biotinylated secondary antibody (1/200 in 1% BSA-PBS) (Vector Laboratories Inc., Burlingame, CA, USA) for 30 min at RT. Finally, avidin-biotin-enzyme complex (Vector Laboratories Inc.) was applied for 30 min at 37°C, and 3,39-diaminobenzidine was used to develop the tumor sections. Human colon carcinoma was used as a positive control, and substitution of the primary antibody with 1% BSA-PBS was used as the negative control.
Analysis of the PET images
PET/CT images were scored by a blinded, independent, experienced nuclear physician (W.O.), being asked to record the presence of intra-abdominal tumor lesions. When lesions were present, he was asked to draw a region of interest [ROI] around the tumor. Each lesion was given a number on a 1 to 3 scale that defined the reader's confidence that the uptake was related to a tumor (definitely, probably, or possibly a tumor). The imaging findings were then compared with the tumor lesions found at dissection. The detection rates for tumors < 10 μL and ≥ 10 μL were calculated, corresponding with a sphere diameter of < 2.7 or ≥ 2.7 mm, respectively.
Statistical analyses
Statistical analysis was performed using the SPSS software (Chicago, IL, USA) and GraphPad Prism version 5.00 for Windows (GraphPad Software, San Diego, CA, USA). Means and standard deviations were used to describe continuous data, unless stated otherwise. Correlations were determined using a Spearman's correlation test. The level of significance was set at p < 0.05.
Results
Tumor growth
Three weeks after the intraperitoneal injection of the LS174T cells, the mice did not show clinical signs of discomfort or change in body weight. At dissection, the abdomen contained multiple solid tumor lesions (median, n = 10/mouse; range, 4 to 17). Most frequent localizations were at the rectovesical pouch, the mesentery, and the subhepatic, -splenic, and -phrenic spaces. Some tumor nodules were adjoining in groups of two or three lesions. Three-dimensional caliper measurements indicated that the maximum diameter of the tumor lesions varied between 1 and 15 mm (median, 5 mm), and weights varied between 0.3 and 650 mg (median, 16 mg).
Biodistribution
The biodistribution of 125I-TF2 and 68Ga-IMP288 in the mice is shown in Figure 1a. High uptake of the bsmAb (3.73 ± 1.2% ID/g) and peptide (23.4 ± 7.2% ID/g) in the tumor lesions was observed with very low accretion in the normal organs. This resulted in high tumor-to-normal-tissue ratios of 68Ga-IMP288 (e.g., tumor-to-intestine ratio, 58 ± 22; tumor-to-liver ratio, 15 ± 3).
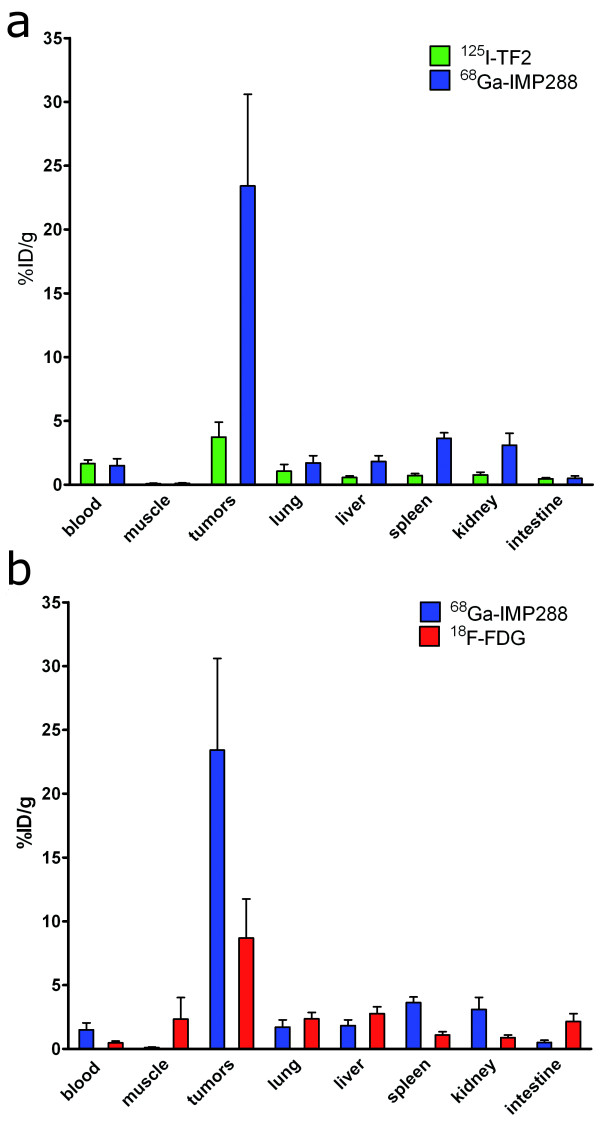
Figure 1.
Biodistribution. (a) 6.0 nmol 125I-TF2 (0.37 MBq) and 0.25 nmol 68Ga-IMP288 (5 MBq) 1 h after i.v. injection of 68Ga-IMP288 in BALB/c nude mice with intraperitoneal CEA-expressing LS174T tumors. (b) 0.25 nmol 68Ga-IMP288 (5 MBq) and 18F-FDG (5 MBq) 1 h after i.v. injection in the BALB/c nude mice with intraperitoneal CEA-expressing LS174T tumors. Values are given as means ± standard deviation (n = 5).
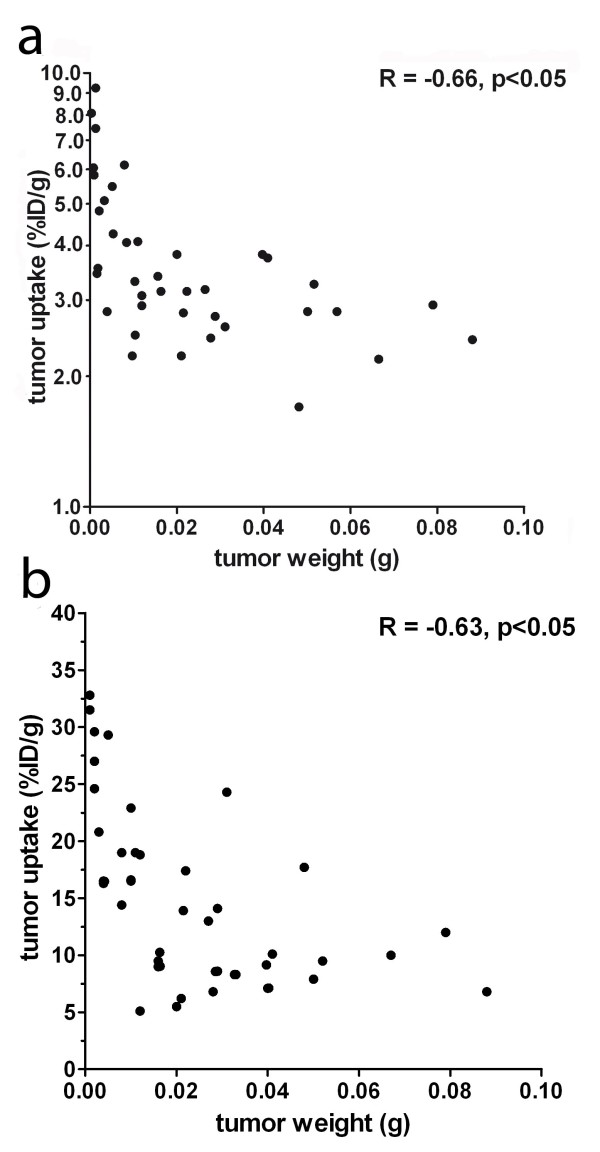
18F-FDG localized efficiently in the tumors (8.7 ± 3.1% ID/g; Figure 1b) but with physiological uptake in various normal tissues and with lower tumor-to-normal tissue ratios (e.g., tumor-to-intestine ratio, 3.9 ± 1.1; tumor-to-liver ratio, 2.9 ± 0.5). Tumor uptake of both 125I-TF2 and 68Ga-IMP288 correlated inversely with tumor size, as shown in Figure 2a, b (Spearman's rho = -0.66, p < 0.05, and Spearman's rho = -0.63, p < 0.05, respectively).
Figure 2.
Correlation between tumor uptake of 125I-TF2 (A) and 68Ga-IMP288 (B) and tumor size. (Spearman's rho = -0.66, p < 0.05 and Spearman's rho = -0.63, p < 0.05, respectively.)
PET/CT images
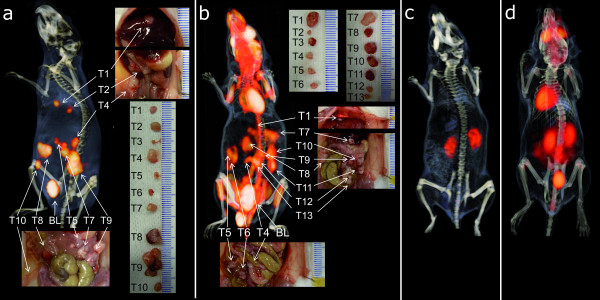
Immuno-PET with TF2 and 68Ga-IMP288 resulted in a clear delineation of the tumors. An example of a PET/CT image is shown in Figure 3a. It shows the cross sections through several tumor lesions. The photographs show their localization in the abdomen as well as their size. Apart from the activity in the bladder, very low uptake in normal tissues was seen. Due to the highly specific uptake in the tumor lesions and low background concentration, the immuno-PET/CT images could even be used to guide the localization of tumor lesions during dissection. Tumors that were more difficult to find macroscopically because they were localized in the retroperitoneal cavities or posterior to the liver were easily seen and localized on the images.
Figure 3.
Images. 3D-volume rendering of the pretargeted immuno-PET scan (a) and the FDG-PET/CT scan (b) of the BALB/c nude mice with intraperitoneal LS174T tumors that received 6.0 nmol TF2 and 5 MBq 68Ga-IMP288 (0.25 nmol) with a 16-h interval (a) or 18F-FDG (b). The animals were imaged 1 h after 68Ga-IMP288 or 18F-FDG injection. Digital pictures were made during dissection to localize and measure individual tumors. On the pretargeted immuno-PET/CT images (a), all dissected tumors were very clearly distinguishable, except for the two very small tumors (1.2 and 4.7 μL, respectively). In the FDG-PET/CT images (b), arrows are pointed at the localizations where tumors were found at dissection, but the signal was difficult to be discriminated from the intestines. Figure 3c, d shows the PET/CT images of mice without intraperitoneal images after TF2 and 68Ga-IMP288 injection (c) or 18F-FDG injection (d).
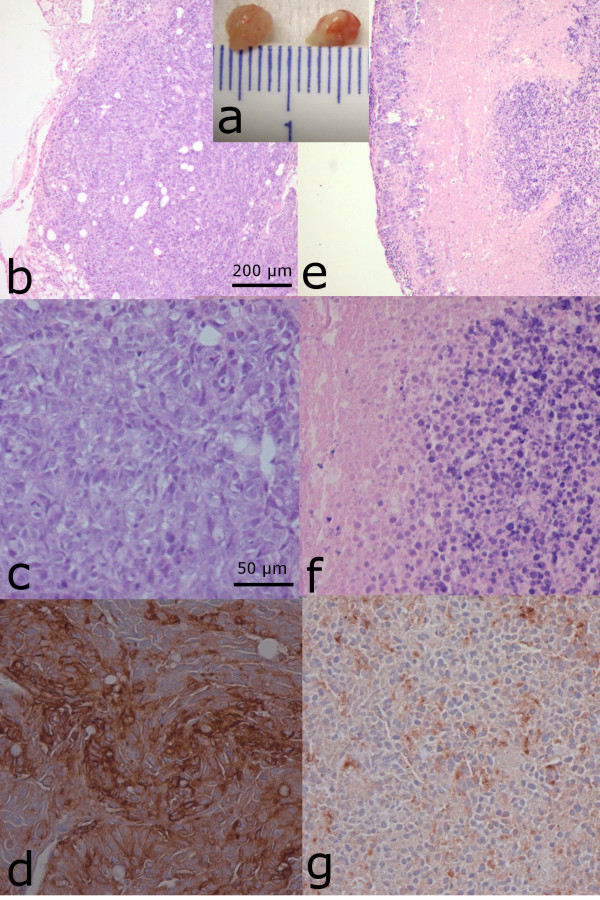
Interestingly, one lesion that was macroscopically doubtful to be a tumor, and showing minimal uptake on immuno-PET, had an activity concentration as low as 0.49% ID/g. This uptake level was much lower than that of the other lesions in the same animal (range, 16.3 to 29.6% ID/g). This lesion with the low uptake was shown by immunohistochemistry to consist > 90% of necrotic tissue and infiltrated leukocytes, lack CEA expression, and have only a small rim of vital tumor cells (Figure 4), which explains its low signal on immuno-PET.
Figure 4.
Immunohistochemistry. Two tumor lesions dissected from the abdomen of a BALB/c nude mouse that received 68Ga-IMP288 after pretargeting with TF2 (a). One lesion (a: left lesion) showed normal vital tumor cells on microscopic hematoxylin and eosin [HE]- and CEA-stained images (b: HE, × 5; c: HE, × 20; and d: CEA, × 20) and high specific tumor uptake of 68Ga-IMP288 (17.7% ID/g). On the contrary, another lesion in the same animal (a: right lesion) showed much lower tumor activity concentration (0.49% ID/g) in biodistribution and a much lower signal on the PET/CT images. This result was explained by the HE sections and CEA-stained images showing > 90% of non-vital tumor tissue (necrosis and infiltrated lymphocytes), lacking CEA expression (e: HE, × 5; f: HE, × 20; and g: CEA, × 20).
In contrast, it was more difficult to discriminate the tumor lesions from other intra-abdominal structures on the FDG-PET images because the uptake in the tumors was only slightly higher than that in the intestines, as is shown in Figure 3b. FDG-PET images showed physiological uptake in the brain and the myocardium.
To illustrate the low uptake of the pretargeting peptide in the background, the immuno-PET/CT and FDG-PET/CT images of the mice without intraperitoneal tumors, which were imaged according to the same scanning protocol, are shown in Figure 3c, d. In pretargeted immuno-PET/CT images, only a low signal in the kidneys was observed, whereas no uptake was observed in the other normal organs. The FDG-PET/CT image of the animal without abdominal tumors clearly showed uptake in the bowel.
Sensitivity
There was a major difference in the number of detected lesions in the immuno-PET/CT compared with the FDG-PET/CT. Table 1 shows the number of tumors that were correctly aligned by the independent nuclear physician for each imaging method. For the pretargeted immuno-PET, all tumor lesions ≥ 10 μL were detected (100%, 23/23). A separate analysis for the smaller lesions, < 10 μL, showed a detection rate of 20% (3/15). The score on the probability scale was 'definitely positive' for 88% of the delineated lesions. In contrast, in the FDG-PET images, the detection rate of the tumors ≥ 10 μL was only 48% (13/27). A similar small proportion of the smaller lesions were found by FDG-PET/CT compared to immuno-PET/CT (25%, 3/12). Interestingly, the nuclear medicine physician was much less confident about aligning the ROIs in the FDG-PET/CT images. For none of the lesions, he scored 'definitely positive' and only 'possibly positive' for 69% (11/16).
Table 1.
Number of tumors correctly aligned by pretargeted immuno-PET/CT and FDG-PET/CT
| Pretargeted immuno-PET/CT | FDG-PET/CT | ||
|---|---|---|---|
| Tumors > 10 μL | Dissected | 23 | 27 |
| Detected in images | 23 (100%) | 13 (48%) | |
| Tumors < 10 μL | Dissected | 15 | 12 |
| Detected in images | 3 (20%) | 3 (25%) | |
| Probability assigned by the nuclear physician | Definitely positive | 23 (88%) | 0 |
| Possibly positive | 3 (12%) | 11 (69%) | |
| Probably positive | 0 | 5 (31%) |
Alignment and confidence rate was done by the independent nuclear physician.
Discussion
This study showed that pretargeted immuno-PET is a very sensitive imaging modality to detect CEA-expressing tumor lesions in an orthotopic mouse model. The intraperitoneal tumors were clearly delineated with a high tumor-to-background contrast, providing high sensitivity: all tumor lesions ≥ 10 μL were detected with this method at a very good confidence rate. The smallest lesions that were detected had a volume as low as 5 to 8 μL, which is in the same range of the spatial resolution of the dedicated animal PET scanner.
The animal model used in this study was well characterized by Koppe et al [34]. The human colon carcinoma cell line LS174T has a reproducible growth pattern in BALB/c nude mice after intraperitoneal injection. Three weeks after tumor cell inoculation, small tumor nodules were observed in the rectovesical pouch, the mesentery, and the subhepatic, -splenic, and -phrenic spaces. The preclinical model mimics peritoneal disease of patients with metastasized colorectal cancer [35,36].
In a previous imaging study, we demonstrated the feasibility of pretargeted immuno-PET using 68Ga- or 18F-labeled di-HSG peptides in mice with subcutaneous tumors [32]. In the current study, the activity concentration of the 68Ga-labeled IMP288 in the intraperitoneal tumors was similar to that in the subcutaneous tumors [32,37]. In our intraperitoneal tumor model, the variation in tumor size was much wider than that in the subcutaneous model. Our biodistribution results showed an inverse relationship between tumor weight and activity concentration. This correlation corresponds with the findings of other investigators [38-41]. Sharkey et al. showed specific uptake of 124I-labeled peptide after pretargeting with TF2 in microdisseminated human colon cancer colonies in the lungs of nude mice. In that model, high tumor-to-non-tumor ratios were obtained, illustrating the excellent tumor targeting potential of the pretargeting strategy [42].
FDG-PET/CT has shown high sensitivity and negative predictive value in diagnosing CRC [43,44]. Therefore, it was used in the present study as a reference method. The imaging quality of FDG-PET in this preclinical study was optimized by minimizing uptake of FDG in other organs by anesthesia, fasting, and warming of the animals [45]. Its uptake in the myocardium, brain, intestines, and liver is comparable to the clinical situation. The ratios between normal and tumor tissues might have appeared to be less favorable than in patients, which might have compromised the detection of the tumors.
Based on our preclinical results, we feel that pretargeted immuno-PET can be of additive value in the clinical setting. When staging patients with primary tumors in the detection of eventual metastases, a highly sensitive and specific imaging method is required. Furthermore, in patients to be screened prior to curative liver metastasectomy, the disclosure of occult extrahepatic lesions will prevent useless operations. More so, immuno-PET can help select patients who could undergo radioimmunotherapy. As the pretargeting system with the DOTA-conjugated peptides is very flexible, it can be labeled with a broad variety of radionuclides, such as 90Y and 177Lu for pretargeted radioimmunotherapy, or with 111In and 99 mTc for SPECT imaging. Our preclinical results show similar biodistribution of the 111In/177Lu- or 68Ga-labeled peptide [37]. Images about targeting known, non-biopsied lesions can confirm antigen expression and accessibility of the therapeutic dose. Information on the biodistribution and pharmacokinetics can help adjust treatment regimes by providing dosimetry data. This could be used to optimize dosing and to avoid toxicities.
For clinical application, 68Ga has some major advantages. It is readily available in a nearly carrier-free state from an in-house 68Ge/68Ga generator. IMP288-DOTA can be stably and rapidly labeled with 68Ga. Its half-life matches the pharmacokinetics of the peptide. In the present study, the positron range of 68Ga (median range, 3.5 mm) might have limited image resolution. Visser et al. [33] showed that with the intrinsic spatial resolution (approximately 1.5 mm) of our state-of-the-art, small-animal PET scanner, the finite positron range has become the limiting factor for the overall spatial resolution and activity recovery in small structures imaged with 68Ga. Combined with the partial volume effect, this could explain the lower detection rate of the smallest tumor lesions with pretargeted immuno-PET despite the higher radioactivity concentration of TF2 and 68Ga-IMP288 in the smaller tumors.
Due to the flexibility of the di-HSG peptides, the use of other PET radionuclides for this pretargeting system can be explored. 18F, the most widely used positron-emitting radioisotope, would be suitable due to its short positron range in the tissue (0.62 mm), which might increase the image resolution. McBride and, subsequently, Laverman et al. developed an innovative and rapid method for labeling peptides with 18F based on a metal chelator [46,47]. The biodistribution and PET images in the subcutaneous LS174T tumors in the nude mice showed the feasibility of this approach [32]. Translation of this preclinical imaging method to the clinical situation will show the effect of the intrinsic resolution of the clinical PET scanner in combination with the spatial resolution of the radionuclide.
Conclusions
In summary, this study indicates that pretargeted immuno-PET with TF2 and 68Ga-IMP288 is a specific and sensitive method for detecting colon cancer in a preclinical model. Further clinical trials should focus on the diagnostic accuracy of pretargeted immuno-PET and determine its additional value in the clinical setting.
Competing interests
WJM, DMG, and C-HC are employed by or have financial interest in Immunomedics, Inc. and/or IBC Pharmacauticals, Inc. The other authors declare that they have no competing interests.
Authors' contributions
RS conceived the study, carried out the imaging studies and the analysis of the studies, and drafted the manuscript. WTAG conceived the study and helped draft the manuscript. RMS participated in the design of the study and helped draft the manuscript. GMF carried out the labeling procedures and the imaging studies. WJM and C-HC synthesized and purified the pretargeting agents. PL carried out the imaging studies and helped with the analysis of the studies. DMG participated in the design of the study and helped draft the manuscript. WJGO carried out the analysis of the imaging studies and helped draft the manuscript. OCB conceived the study, participated in the design of the study, and helped draft the manuscript. All authors read and approved the final manuscript.
Contributor Information
Rafke Schoffelen, Email: r.schoffelen@nucmed.umcn.nl.
Winette TA van der Graaf, Email: w.vandergraaf@onco.umcn.nl.
Robert M Sharkey, Email: rmsharkey@gscancer.org.
Gerben M Franssen, Email: g.franssen@nucmed.umcn.nl.
William J McBride, Email: bmcbride@immunomedics.com.
Chien-Hsing Chang, Email: kchang@immunomedics.com.
Peter Laverman, Email: p.laverman@nucmed.umcn.nl.
David M Goldenberg, Email: dmg.gscancer@att.net.
Wim JG Oyen, Email: w.oyen@nucmed.umcn.nl.
Otto C Boerman, Email: o.boerman@nucmed.umcn.nl.
Acknowledgements
We thank Bianca Lemmers-van de Weem, Kitty Lemmens-Hermans, Jonathan Disselhorst, and Melissa Roeffen for their technical assistance. The work was supported by the Dutch Cancer Society (KWF Kankerbestrijding) grant no. KUN 2008-4038, and the National Institutes of Health grant (National Institute of Biomedical Imaging and Bioengineering, R43 EB003751).
References
- Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. http://www.cancer.gov
- Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001;2:533–543. doi: 10.1016/S1470-2045(01)00486-7. [DOI] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence. http://www.nice.org
- Hughes KS, Simon R, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, Maclean BJ, Foster JH, Daly JM, Fitzherbert D. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Surgery. 1986;100:278–284. [PubMed] [Google Scholar]
- Ruers TJ, Wiering B, van der Sijp JR, Roumen RM, de Jong KP, Comans EF, Pruim J, Dekker HM, Krabbe PF, Oyen WJ. Improved selection of patients for hepatic surgery of colorectal liver metastases with (18)F-FDG PET: a randomized study. J Nucl Med. 2009;50:1036–1041. doi: 10.2967/jnumed.109.063040. [DOI] [PubMed] [Google Scholar]
- Jain RK. Physiological barriers to delivery of monoclonal antibodies and other macromolecules in tumors. Cancer Res. 1990;50:814s–819s. [PubMed] [Google Scholar]
- Reardan DT, Meares CF, Goodwin DA, McTigue M, David GS, Stone MR, Leung JP, Bartholomew RM, Frincke JM. Antibodies against metal chelates. Nature. 1985;316:265–268. doi: 10.1038/316265a0. [DOI] [PubMed] [Google Scholar]
- Boerman OC, van Schaijk FG, Oyen WJ, Corstens FH. Pretargeted radioimmunotherapy of cancer: progress step by step. J Nucl Med. 2003;44:400–411. [PubMed] [Google Scholar]
- Chang CH, Sharkey RM, Rossi EA, Karacay H, McBride W, Hansen HJ, Chatal JF, Barbet J, Goldenberg DM. Molecular advances in pretargeting radioimunotherapy with bispecific antibodies. Mol Cancer Ther. 2002;1:553–563. [PubMed] [Google Scholar]
- Sharkey RM, Cardillo TM, Rossi EA, Chang CH, Karacay H, McBride WJ, Hansen HJ, Horak ID, Goldenberg DM. Signal amplification in molecular imaging by pretargeting a multivalent, bispecific antibody. Nat Med. 2005;11:1250–1255. doi: 10.1038/nm1322. [DOI] [PubMed] [Google Scholar]
- Le Doussal JM, Martin M, Gautherot E, Delaage M, Barbet J. In vitro and in vivo targeting of radiolabeled monovalent and divalent haptens with dual specificity monoclonal antibody conjugates: enhanced divalent hapten affinity for cell-bound antibody conjugate. J Nucl Med. 1989;30:1358–1366. [PubMed] [Google Scholar]
- Karacay H, McBride WJ, Griffiths GL, Sharkey RM, Barbet J, Hansen HJ, Goldenberg DM. Experimental pretargeting studies of cancer with a humanized anti-CEA × murine anti-[In-DTPA] bispecific antibody construct and a (99 m)Tc-/(188)Re-labeled peptide. Bioconjug Chem. 2000;11:842–854. doi: 10.1021/bc0000379. [DOI] [PubMed] [Google Scholar]
- Wiering B, Krabbe PF, Jager GJ, Oyen WJ, Ruers TJ. The impact of fluor-18-deoxyglucose-positron emission tomography in the management of colorectal liver metastases. Cancer. 2005;104:2658–2670. doi: 10.1002/cncr.21569. [DOI] [PubMed] [Google Scholar]
- Park IJ, Kim HC, Yu CS, Ryu MH, Chang HM, Kim JH, Ryu JS, Yeo JS, Kim JC. Efficacy of PET/CT in the accurate evaluation of primary colorectal carcinoma. Eur J Surg Oncol. 2006;32:941–947. doi: 10.1016/j.ejso.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Llamas-Elvira JM, Rodriguez-Fernandez A, Gutierrez-Sainz J, Gomez-Rio M, Bellon-Guardia M, Ramos-Font C, Rebollo-Aguirre AC, Cabello-Garcia D, Ferron-Orihuela A. Fluorine-18 fluorodeoxyglucose PET in the preoperative staging of colorectal cancer. Eur J Nucl Med Mol Imaging. 2007;34:859–867. doi: 10.1007/s00259-006-0274-4. [DOI] [PubMed] [Google Scholar]
- Tzimas GN, Koumanis DJ, Meterissian S. Positron emission tomography and colorectal carcinoma: an update. J Am Coll Surg. 2004;198:645–652. doi: 10.1016/j.jamcollsurg.2003.11.015. [DOI] [PubMed] [Google Scholar]
- Topal B, Flamen P, Aerts R, D'Hoore A, Filez L, Van Cutsem E, Mortelmans L, Penninckx F. Clinical value of whole-body emission tomography in potentially curable colorectal liver metastases. Eur J Surg Oncol. 2001;27:175–179. doi: 10.1053/ejso.2000.1075. [DOI] [PubMed] [Google Scholar]
- Pelosi E, Deandreis D. The role of 18F-fluoro-deoxy-glucose positron emission tomography (FDG-PET) in the management of patients with colorectal cancer. Eur J Surg Oncol. 2007;33:1–6. doi: 10.1016/j.ejso.2006.10.020. [DOI] [PubMed] [Google Scholar]
- Herbertson RA, Scarsbrook AF, Lee ST, Tebbutt N, Scott AM. Established, emerging and future roles of PET/CT in the management of colorectal cancer. Clin Radiol. 2009;64:225–237. doi: 10.1016/j.crad.2008.08.008. [DOI] [PubMed] [Google Scholar]
- Rosenbaum SJ, Lind T, Antoch G, Bockisch A. False-positive FDG PET uptake--the role of PET/CT. Eur Radiol. 2006;16:1054–1065. doi: 10.1007/s00330-005-0088-y. [DOI] [PubMed] [Google Scholar]
- Metser U, Miller E, Lerman H, Even-Sapir E. Benign nonphysiologic lesions with increased 18F-FDG uptake on PET/CT: characterization and incidence. AJR Am J Roentgenol. 2007;189:1203–1210. doi: 10.2214/AJR.07.2083. [DOI] [PubMed] [Google Scholar]
- Even-Sapir E, Parag Y, Lerman H, Gutman M, Levine C, Rabau M, Figer A, Metser U. Detection of recurrence in patients with rectal cancer: PET/CT after abdominoperineal or anterior resection. Radiology. 2004;232:815–822. doi: 10.1148/radiol.2323031065. [DOI] [PubMed] [Google Scholar]
- Dirisamer A, Schima W, Heinisch M, Weber M, Lehner HP, Haller J, Langsteger W. Detection of histologically proven peritoneal carcinomatosis with fused 18F-FDG-PET/MDCT. Eur J Radiol. 2009;69:536–541. doi: 10.1016/j.ejrad.2007.11.032. [DOI] [PubMed] [Google Scholar]
- Goldenberg DM, Rossi EA, Sharkey RM, McBride WJ, Chang CH. Multifunctional antibodies by the Dock-and-Lock method for improved cancer imaging and therapy by pretargeting. J Nucl Med. 2008;49:158–163. doi: 10.2967/jnumed.107.046185. [DOI] [PubMed] [Google Scholar]
- Lindmo T, Boven E, Cuttitta F, Fedorko J, Bunn PA Jr. Determination of the immunoreactive fraction of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J Immunol Methods. 1984;72:77–89. doi: 10.1016/0022-1759(84)90435-6. [DOI] [PubMed] [Google Scholar]
- Morel A, Darmon M, Delaage M. Recognition of imidazole and histamine derivatives by monoclonal antibodies. Mol Immunol. 1990;27:995–1000. doi: 10.1016/0161-5890(90)90122-G. [DOI] [PubMed] [Google Scholar]
- Rossi EA, Goldenberg DM, Cardillo TM, McBride WJ, Sharkey RM, Chang CH. Stably tethered multifunctional structures of defined composition made by the dock and lock method for use in cancer targeting. Proc Natl Acad Sci USA. 2006;103:6841–6846. doi: 10.1073/pnas.0600982103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey RM, Goldenberg DM, Goldenberg H, Lee RE, Ballance C, Pawlyk D, Varga D, Hansen HJ. Murine monoclonal antibodies against carcinoembryonic antigen: immunological, pharmacokinetic, and targeting properties in humans. Cancer Res. 1990;50:2823–2831. [PubMed] [Google Scholar]
- McBride WJ, Zanzonico P, Sharkey RM, Noren C, Karacay H, Rossi EA, Losman MJ, Brard PY, Chang CH, Larson SM, Goldenberg DM. Bispecific antibody pretargeting PET (immunoPET) with an 124I-labeled hapten-peptide. J Nucl Med. 2006;47:1678–1688. [PubMed] [Google Scholar]
- Fraker PJ, Speck JC Jr. Protein and cell membrane iodinations with a sparingly soluble chloroamide, 1,3,4,6-tetrachloro-3a,6a-diphrenylglycoluril. Biochem Biophys Res Commun. 1978;80:849–857. doi: 10.1016/0006-291X(78)91322-0. [DOI] [PubMed] [Google Scholar]
- Schoffelen R, Sharkey RM, Goldenberg DM, Franssen G, McBride WJ, Rossi EA, Chang CH, Laverman P, Disselhorst JA, Eek A, van der Graaf WT, Oyen WJ, Boerman OC. Pretargeted immuno-positron emission tomography imaging of carcinoembryonic antigen-expressing tumors with a bispecific antibody and a 68Ga- and 18F-labeled hapten peptide in mice with human tumor xenografts. Mol Cancer Ther. 2010;9:1019–1027. doi: 10.1158/1535-7163.MCT-09-0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser EP, Disselhorst JA, Brom M, Laverman P, Gotthardt M, Oyen WJ, Boerman OC. Spatial resolution and sensitivity of the Inveon small-animal PET scanner. J Nucl Med. 2009;50:139–147. doi: 10.2967/jnumed.108.055152. [DOI] [PubMed] [Google Scholar]
- Koppe MJ, Hendriks T, Boerman OC, Oyen WJ, Bleichrodt RP. Radioimmunotherapy is an effective adjuvant treatment after cytoreductive surgery of experimental colonic peritoneal carcinomatosis. J Nucl Med. 2006;47:1867–1874. [PubMed] [Google Scholar]
- Meyers MA. Dynamic radiology of the abdomen: normal and pathologic anatomy. 5. New York: Springer-Verlag; 2000. [Google Scholar]
- De Gaetano AM, Calcagni ML, Rufini V, Valenza V, Giordano A, Bonomo L. Imaging of peritoneal carcinomatosis with FDG PET-CT: diagnostic patterns, case examples and pitfalls. Abdom Imaging. 2009;34:391–402. doi: 10.1007/s00261-008-9405-7. [DOI] [PubMed] [Google Scholar]
- Schoffelen R, van der Graaf WT, Franssen G, Sharkey RM, Goldenberg DM, McBride WJ, Rossi EA, Eek A, Oyen WJ, Boerman OC. Pretargeted 177Lu radioimmunotherapy of carcinoembryonic antigen-expressing human colonic tumors in mice. J Nucl Med. 2010;51:1780–1787. doi: 10.2967/jnumed.110.079376. [DOI] [PubMed] [Google Scholar]
- Sharkey RM, Primus FJ, Goldenberg DM. Antibody protein dose and radioimmunodetection of GW-39 human colon tumor xenografts. Int J Cancer. 1987;39:611–617. doi: 10.1002/ijc.2910390512. [DOI] [PubMed] [Google Scholar]
- Moshakis V, McIlhinney RA, Raghavan D, Neville AM. Localization of human tumour xenografts after i.v. administration of radiolabeled monoclonal antibodies. Br J Cancer. 1981;44:91–99. doi: 10.1038/bjc.1981.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan PL, Halpern SE, Dillman RO, Shawler DL, Johnson DE, Chen A, Krishnan L, Frincke J, Bartholomew RM, David GS, Carlo D. Tumor size: effect on monoclonal antibody uptake in tumor models. J Nucl Med. 1986;27:422–427. [PubMed] [Google Scholar]
- Blumenthal RD, Sharkey RM, Kashi R, Natale AM, Goldenberg DM. Influence of animal host and tumor implantation site on radio-antibody uptake in the GW-39 human colonic cancer xenograft. Int J Cancer. 1989;44:1041–1047. doi: 10.1002/ijc.2910440617. [DOI] [PubMed] [Google Scholar]
- Sharkey RM, Karacay H, Vallabhajosula S, McBride WJ, Rossi EA, Chang CH, Goldsmith SJ, Goldenberg DM. Metastatic human colonic carcinoma: molecular imaging with pretargeted SPECT and PET in a mouse model. Radiology. 2008;246:497–507. doi: 10.1148/radiol.2462070229. [DOI] [PubMed] [Google Scholar]
- Chowdhury FU, Shah N, Scarsbrook AF, Bradley KM. [18F]FDG PET/CT imaging of colorectal cancer: a pictorial review. Postgrad Med J. 2010;86:174–182. doi: 10.1136/pgmj.2009.079087. [DOI] [PubMed] [Google Scholar]
- Esteves FP, Schuster DM, Halkar RK. Gastrointestinal tract malignancies and positron emission tomography: an overview. Semin Nucl Med. 2006;36:169–181. doi: 10.1053/j.semnuclmed.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Fueger BJ, Czernin J, Hildebrandt I, Tran C, Halpern BS, Stout D, Phelps ME, Weber WA. Impact of animal handling on the results of 18F-FDG PET studies in mice. J Nucl Med. 2006;47:999–1006. [PubMed] [Google Scholar]
- McBride WJ, Sharkey RM, Karacay H, D'Souza CA, Rossi EA, Laverman P, Chang CH, Boerman OC, Goldenberg DM. A novel method of 18F radiolabeling for PET. J Nucl Med. 2009;50:991–998. doi: 10.2967/jnumed.108.060418. [DOI] [PubMed] [Google Scholar]
- Laverman P, McBride WJ, Sharkey RM, Eek A, Joosten L, Oyen WJ, Goldenberg DM, Boerman OC. A novel facile method of labeling octreotide with (18)F-fluorine. J Nucl Med. 2010;51:454–461. doi: 10.2967/jnumed.109.066902. [DOI] [PMC free article] [PubMed] [Google Scholar]