Abstract
Introduction
Hypertension (HTN) is a leading risk factor for preventable cardiovascular disease, with over one in five adults affected worldwide. Lifestyle modification is a key strategy for the prevention and treatment of HTN. Stress has been associated with greater cardiovascular risk, and stress management is a recommended intervention for hypertensives. Stress reduction through relaxation therapies has been shown to have an effect on human physiology, including lowering blood pressure (BP). However, individualised behavioural interventions are resource intensive, and group stress management approaches have not been validated for reducing HTN. The HARMONY Study is a pilot randomised controlled trial designed to determine if mindfulness-based stress reduction (MBSR), a standardised group therapy, is an effective intervention for lowering BP in stage 1 unmedicated hypertensives.
Methods and analysis
Men and women unmedicated for HTN with mean daytime ambulatory blood pressure (ABP) ≥135/85 mm Hg or 24 h ABP ≥130/80 mm Hg are included in the study. Subjects are randomised to receive MBSR immediately or after a wait-list control period. The primary outcome measure is mean awake and 24 h ABP. The primary objective of the HARMONY Study is to compare ABP between the treatment and wait-list control arm at the 12-week primary assessment period. Results from this study will determine if MBSR is an effective intervention for lowering BP in early unmedicated hypertensives.
Ethics and dissemination
This research project was approved by the Sunnybrook Research Ethics Board and the University Health Network Research Ethics Board (Toronto, Canada). Planned analyses are in full compliance with the principles of the Declaration of Helsinki. Data collection will be completed by early spring 2012. Primary and secondary analysis will commence immediately after data monitoring is completed; dissemination plans include preparing publications for submission during the summer of 2012.
Trial registration number
This study is registered with http://clinicaltrials.gov (NCT00825526).
Article summary
Article focus
Does MBSR have a significant BP-lowering effect on awake and 24 h ABP?
Is MBSR a safe and feasible complementary treatment for high BP?
Is there interest in the general population to participate in a meditation/stress reduction programme to lower high BP?
Key messages
Results of this trial will contribute to the development of non-pharmacological treatment approaches to HTN.
If a positive outcome is achieved, the HARMONY Study could highlight MBSR as a new paradigm for delivering lifestyle therapy.
If successful, the next phase of the project will incorporate additional lifestyle intervention components to MBSR therapy (such as sodium and weight loss counselling), with the goal of ultimately building a standardised lifestyle therapy programme to which physicians can refer their hypertensive patients to the future.
Strengths and limitations of this study
First study to examine a standardised stress reduction group therapy, already funded in part by the Ontario Health Insurance Plan, for the management of high BP.
Large sample size and use of randomised controlled trial format minimises bias and maximises the opportunity to detect any BP-lowering effect of MBSR.
Due to the silent nature of high BP, the lack of immediate positive perceptible feedback when BP is lowered may hamper the reinforcement necessary to make permanent lifestyle changes.
Introduction
Based on an annual consensus conference reviewing the world literature including the Cochrane Collaboration Databases, the Canadian Hypertension Education Program recommends lifestyle modification as a key strategy for the prevention and treatment of hypertension (HTN).1 Over 5 million Canadians, part of a worldwide epidemic, are hypertensive.2 Data extrapolated from large population surveys and prospective studies3 4 show that approximately 250 000 Canadians with high-normal blood pressure (BP) (systolic blood pressure (SBP) 120–139 mm Hg or diastolic blood pressure (DBP) 80–89 mm Hg) will develop full-blown high BP every year (BP ≥140/90 mm Hg)—putting them at higher risk for heart attack and stroke, necessitating the use of medications in most of them. Preventing and controlling HTN is one of the most cost-effective strategies for reducing the global burden of premature cardiovascular disease and death.5 Reducing SBP by just 3 mm Hg in the general population has the potential to reduce stroke mortality by 8% and coronary artery disease mortality by 5%.6 7 The published findings of the InterStroke Study, one of the largest studies of its type in the world, concluded definitively that uncontrolled HTN is the single most influential risk factor for stroke.8
Stress has been associated with greater cardiovascular risk and consideration of stress management is a recommended intervention for hypertensives.1 However, specific stress management approaches are not well validated for reducing HTN.9–11 Stress management therapies can be differentiated based on their approach and delivery: single- or multicomponent approach and individualised or group delivery. Certain therapeutic approaches have been efficacious for reducing BP in subjects with hypertension: transcendental meditation (TM) (a single-component, individualised therapy), cognitive behavioural therapy (CBT) (a multicomponent, individualised therapy) and, more recently, contemplative meditation12 (a multicomponent, group therapy).
TM is a standardised form of meditation where an individual repeats a mantra to move the mind towards a higher state of concentration; this in turn leads to a greater sense of relaxation and physiological calming.9 Evidence indicates that single-component interventions like TM are efficacious in some conditions,13–18 including HTN,19 with possible long-term effects.16 The BP-lowering effect of TM has been further supported by two meta-analyses, each suggesting TM can reduce both SBP and DBP.20 21 However, other meta-analyses have suggested that the available clinical trials had significant ‘methodological weaknesses and (were) potentially biased by the affiliation of authors to the TM organization’9; thus, one must proceed with caution when evaluating if TM has a cumulative positive effect on lowering BP.9 CBT teaches subjects to be aware of stressors and to re-evaluate negative life events.22 In a carefully controlled trial, Linden et al demonstrated that CBT decreased BP in unmedicated participants with hypertension.23 While CBT, a multicomponent individualised therapy, has demonstrated efficacy in treating HTN, the cost of administering this one-on-one therapy presents a significant barrier to its widespread use. Contemplative meditation has demonstrated promising results; however, limited research on the topic indicates that more work must be done before final conclusions can be drawn.12
Mindfulness-based stress reduction (MBSR), like CBT, is a multicomponent therapy that encourages participants to modify their thought pattern through changing their relationship and approach to stressors in their lives.24 However, unlike CBT, MBSR is a standardised group therapy, which can be delivered to a heterogeneous population. It is now available for stress reduction through some community and hospital complementary medicine programmes, and in Ontario, it is covered in part by the Ontario Health Insurance Plan. While CBT can be viewed as an acute treatment option, MBSR works as both an acute and preventive treatment as it provides participants with strategies for working with the challenges and stressors in their lives.25 MBSR teaches participants to use mindfulness as an approach to adapt to stress, pain and illness. In both clinical and non-clinical populations, MBSR and related mindfulness-based therapeutic practices have demonstrated benefits for chronic pain,26–29 anxiety,30–34 depression,30 33–37 fibromyalgia,38–40 binge-eating41 and psoriasis,42 as well as improved psychological well-being, immune function and cortisol levels in cancer subjects,43–54 psychological well-being of cancer patient's partners55 and glycaemic control in diabetic populations.56 Three meta-analyses57–59 support the efficacy of MBSR for improving both physical and mental well-being in groups of subjects with mixed medical illness. By bringing mindfulness to life stressors, MBSR participants may more clearly see the full context of a situation, have access to a broader range of emotional responses and therefore cope with stressful situations more effectively.32
Preliminary information suggests that participating in an MBSR programme also lowers BP23 43 56 and improves certain components of cardiovascular functioning.60 Barnes et al initiated one of the earliest studies investigating MBSR and BP; compared to control, those who participated in a 2-month meditation intervention based on MBSR techniques demonstrated lower SBP as measured by an automated device: −4 mm Hg (intervention) compared to +2 mm Hg (control).61 A follow-up study using ambulatory blood pressure monitoring (ABPM) also found significant differences in BP reduction for the meditation group at specific time periods (eg, after school).62 In an abstract, Van Wielingen et al reported that patients with breast cancer who participated in MBSR had lower automated home BP compared to those on wait-list control.63 Examining the treatment group alone, those with higher BP at baseline demonstrated a greater decrease in SBP compared to those with lower SBP at baseline.63 A similar treatment effect was described by Linden in subjects also starting with higher BP levels.64 Two studies by Carlson et al demonstrated high rates of MBSR class attendance, compliance and home meditation,44 45 with the follow-up study reporting consistent drops in clinic BP persisting up to 1 year.43 A randomised controlled trial of an abbreviated 6-week programme using MBSR principles for pain tolerance in normotensive university students found improved pain tolerance and lower DBP in both the treatment and control groups.65 These early studies point towards a BP-lowering effect from MBSR. However, more rigorous methodology and larger sample sizes are required to demonstrate whether MBSR can truly lower BP.
Before a large outcome study can evaluate the use of MBSR for the treatment of HTN, it is necessary to collect data documenting efficacy and treatment effect. The HARMONY Study, a randomised controlled pilot trial investigating the use MBSR for unmedicated stage 1 HTN, will test whether MBSR can significantly lower BP in unmedicated hypertensives. If found effective, the HARMONY Study will provide evidence to support a larger randomised controlled trial by evaluating the feasibility and safety of MBSR as a complementary or alternative treatment for HTN.
Methods
Study design
The HARMONY Study is a randomised, prospective, two-armed, wait-list controlled pilot trial. The intervention is a standard 8-week MBSR programme. A wait-list controlled trial design was chosen in order to model our methodology after Linden et al.23 The main outcome measure is mean awake and 24 h systolic and diastolic ambulatory blood pressure (ABP). The study population consists of unmedicated men and women with stage 1 HTN. Based on the power analysis, the established recruitment goal was 100 subjects. Screening baseline ABPM determines hypertensive eligibility. Screening and follow-up visits take place at Sunnybrook Health Sciences Centre, Toronto, Ontario. All MBSR therapy is conducted at the University Health Network's Toronto General Hospital, Toronto, Ontario.
Study participants
Eligible participants include adults aged 20–75 years old, with mean awake systolic or diastolic ABP ≥135 mm Hg or 85 mm Hg, or mean 24 h ABP ≥130 mm Hg or 80 mm Hg. There must be no antihypertensive use within 6 months of the screening/baseline ABPM visit. We recognise the possibility that an individual may choose to go off antihypertensive therapy when they should not, and may potentially base this decision on wanting to be in the HARMONY Study. In these events, screening with the BPTru and ABPM should capture those individuals whose BP is too high and who should be on active antihypertensive therapy. When screening BP is too high, individuals receive one-on-one counselling with the primary investigator (ST) about their BP, antihypertensive therapy and why they could not be in the study. Using this methodology, we hope to only recruit those who have moderately elevated BP (stage 1) and do not require antihypertensive therapy at the time of enrolment.
Study participants consist of those who meet the screening criteria, are willing and able to participate in the MBSR programme, can attend all necessary study visits and complete all safety BP evaluations. Further details regarding inclusion and exclusion criteria can be found in box 1.
Box 1. Study inclusion and exclusion criteria.
Inclusion criteria:
Age 20–75 years.
Hypertensive as determined by ambulatory blood pressure monitoring (ABPM) at baseline (daytime ≥135/85 mm Hg or 24 h ABPM ≥130/80 mm Hg).
Willing and able to participate in the mindfulness-based stress reduction (MBSR) programme.
Willing to be followed for safety blood pressure (BP) checks if deemed necessary.
Willing to accept a possible waiting period of 12 weeks for MBSR.
Written informed consent.
Exclusion criteria:
Use of antihypertensive within 6 months of the screening ABPM.
Screening office BP >180/100 mm Hg and ABPM ≥160/100 mm Hg.
Diabetes.
Secondary hypertension.
Renal disease (Glomerular filtration rate <60 ml/min or overt nephropathy).
History of heart attack.
History of stroke or transient ischemic attack.
Re-vascularisation procedure.
Active malignant disease (except non-melanoma skin cancer).
Epileptic seizure 6 months before the screening visit.
Congestive heart failure.
Severe liver disease.
Pregnancy or lactation period.
Participation in a clinical trail or receipt of investigational compound or treatment in the 3 months prior to the initial screening visit.
Planned elective surgery during the study period except for cataract surgery.
Inability or unwillingness to perform three or four ABPMs over 6 to 10 months.
Study recruitment
The original planned recruitment rate was 25 subjects every 6 months for a total of 100 subjects. Potential participants have been identified through the clinical practices and referral bases of BLA, MM and ST. Additional successful screening strategies have included public information sessions, advertisements in local newspapers and hospital posters. Screening is performed using a validated automated BP device, the BpTRU (VSM MedTech Ltd, Coquitlam, Canada). Individuals with unmedicated office BP ≥135/85 mm Hg are invited to the next step of screening using 24 h ABPM.
Randomisation and study blinding
Randomisation to one of two study arms is done by sealed envelope method using the permuted block design, with blocks of two and four subjects to maintain the adequacy of randomisation. A computer program generated a random number sequence, which was used to allocate subjects to the treatment or wait-list control group. The randomisation schedule and sealed envelopes were prepared by an individual who worked closely with the Centre for Statistical Design and Analysis and was not directly involved in the study. Blinding is not possible for the HARMONY Study due to the wait-list control design of the study. However, those delivering the MBSR therapy are not informed as to which arm subjects are randomised to.
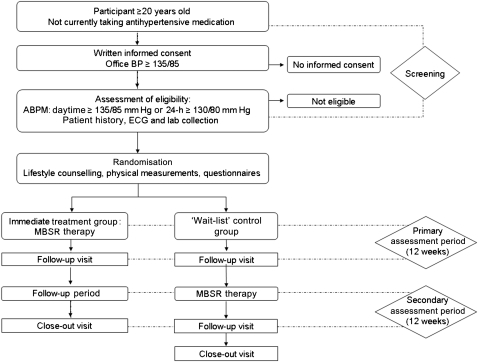
Upon review of the screening ABPM results, consenting subjects who meet study inclusion criteria are randomised. Screening ABP is then used as the baseline ABP for those enrolled in the study. Subjects are randomised to either ‘early’ or ‘delayed’. Those randomised to ‘early’ begin MBSR within 4 weeks of their screening/baseline visit and repeat ABPM 12 weeks after the baseline/screening visit (coinciding with completion of the MBSR course). Those randomised to ‘delayed’ are wait-listed for 12 weeks, repeat ABPM after that wait-list period and subsequently begin MBSR within 4 weeks of that ABPM (figure 1).
Figure 1.
HARMONY Study design. ABPM, ambulatory blood pressure monitoring; MBSR, mindfulness-based stress reduction.
Primary outcome
The primary outcome measure is mean awake and 24 h ABP. The primary objective of the HARMONY Study is to compare mean awake and 24 h ABP between the treatment and control arms at the 12-week post-baseline primary assessment period (figure 1).
Secondary outcomes
Secondary outcomes include evaluating a within-group effect of MBSR on ABP from pre- to post-MBSR intervention. Persistence of effect 12 weeks after completing the therapy will also be investigated (figure 1). Between- and within-group comparisons of the effect of MBSR on night-time ABP will also be assessed. The proportion of subjects achieving BP targets (24 h ABP <130/80, daytime ABP <135/85 mm Hg), those requiring the initiation of medical therapy during the study and adverse events will also be examined. The amount of MBSR practiced outside the classroom will be analysed (via participant diaries and homework logs) with respect to change in BP to evaluate any dose–response interactions. Associations between the effect of MBSR on ABP and individual participant characteristics will also be explored. This will be achieved by examining covariates and incorporating them into a model with BP. See box 2 for further details regarding data collected at study visits.
Box 2. Baseline and ongoing data collection. All listed measurements are collected baseline. All measurements except for ECG are repeated at subsequent study visits (before mindfulness-based stress reduction (MBSR), following MBSR and at the 12-week study close-out).
Ambulatory blood pressure monitoring (ABPM):
Participants wear an ambulatory blood pressure monitor (model 90207, Spacelabs Medical Inc., Redmond, Washington, USA).
Blood pressure is recorded every 15 min during the day and every 30 min between 23:00 and 7:00.
Mean values calculated for systolic and diastolic blood pressure.
Anthropometric measurements:
Body weight and height measured to calculate body mass index.
Waist circumference measured at the top of the iliac crest.
Office blood pressure:
Seated office systolic and diastolic blood pressure measured by BpTRU.
Device takes six measurements every 2 min. Last five measurements are averaged to determine the average seated blood pressure.
Fasting serum samples:
Plasma glucose, HbA1c, total cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, creatinine, electrolytes and liver enzyme levels.
Urine samples:
Urine creatinine levels and microalbuminuria levels.
ECG
To detect any abnormal heart rhythms and left ventricular hypertrophy.
The following questionnaires were included in the study protocol to account for external confounders: (1) Demographics and Lifestyle Questionnaire, (2) State-Trait Anger Expression Inventory-2,66 (3) Hospital Anxiety and Depression Scale,67 (4) Perceived Stress Scale,68 (5) Psychosocial Stress Questionnaire,69 (6) Exercise questionnaire, (7) Job Content Questionnaire,70 (8) Five-Facet Mindfulness Questionnaire,71 (9) Clinical Outcome Routine Evaluation Outcome Measure72 and (10) Toronto Mindfulness Scale.73 All questionnaires are administered at baseline with questionnaires 2, 4, 5 and 6 repeated at each study visit (ie, pre-MBSR, post-MBSR and study close-out). The Toronto Mindfulness Scale is administered after a period of meditation during the second and seventh MBSR class. Planned future analyses include evaluating the relationships between BP, gender and responses from the questionnaires.
Intervention
MBSR is a multicomponent group therapy that provides systematic training in mindfulness meditation as a self-regulation approach to stress reduction and emotion management. MBSR provides training in formal meditation approaches, with the primary goal of cultivating psychological resilience and resistance to stress. This is achieved through fostering the quality of ‘mindfulness’, defined as the capacity to intentionally be in the present moment without judgement.24 MBSR teaches attendees to approach stressful situations ‘mindfully’, allowing them to identify what is occurring in their bodies and minds and to step back from thoughts and feelings during stressful situations. This affords participants the opportunity to make wise choices with respect to managing stressful situations, such as choosing to avoid engaging in anxious worry that may otherwise escalate into a cycle of stress reactivity and contribute to more emotional distress.24 74–76
The MBSR programme is delivered by trained therapists to groups of 25–30 individuals and consists of 10 sessions: an introductory session, eight weekly sessions of 2.5 h and a 6 h intensive session/silent retreat held between week 6 and 7 of the course on a Saturday or Sunday. The MBSR programme incorporates four major therapeutic elements: formal meditation, informal mindfulness practice (such as bringing mindfulness to daily activities), psychoeducational activities and self-monitoring/reflection exercises. Each session also includes group discussion. The development of mindfulness depends heavily upon regular and repeated practice; thus participants commit to daily 45 min homework meditation practice. Homework includes both formal and informal meditation practices, as well as self-observation questions. CDs are included to guide attendees in daily formal meditation practice.
Participants learn new mindfulness practices each week, as well as strategies to incorporate mindfulness perspectives and approaches into daily activities. Some examples of mindfulness practices include the body scan, sitting meditation, mindful yoga, mindful walking, mindful eating and loving kindness meditation. Participants are asked to complete a weekly homework log, which tracks the number of minutes spent on formal meditation practice and whether informal mindfulness was practiced that day. Subjects are given new homework logs each week when they return for class. Both adherence to MBSR and class attendance are captured via the homework logs. Homework logs are faxed weekly from Toronto General Hospital to Sunnybrook Health Sciences Centre where they are entered into the electronic database. HARMONY research staff are asked to contact participants if more than two classes are missed without explanation; this also affords study staff and participants an opportunity to discuss causes for poor class attendance. As the MBSR programme is standardised, subjects can be accommodated in other MBSR classes throughout the course if necessary for scheduling. If too many classes are missed due to unforeseen personal circumstances (and not due to lack of commitment/interest by the study subject), then attempts are made to accommodate them to another MBSR course if possible.
Data collection
Study subject information is organised into individual subject charts and uploaded electronically into a Microsoft Access Database file. All data of enrolled participants are collected on denominated data collection forms, with the contact information page and homework logs being the only exceptions. Data from potential study participants/screen fail participants are kept in a screening log binder and a screen fail binder, respectively. Coding of enrolled study participants is done by study ID, executed in sequential in order (first participant = study ID 001). Data entry is completed by a research assistant; future plans include auditing all study charts and the study database at the end of the trial to ensure data was entered accurately.
All study data are maintained in a secure location only accessible to study related personnel; this includes lab computers, which are accessible only through authentication with ID and password. Study data are shared with family physicians or the Nephrology Research Group at Sunnybrook Health Sciences Centre only with the participant's consent. All source information collected is retained under the primary investigator (ST) as custodian. After all data entry/data auditing are completed, paper copies of study data will be stored at Iron Mountain and destroyed after 25 years as per Health Canada guidelines. Electronic study data will be kept in the Microsoft Access Database until data analysis is completed. Maintenance of study data and study confidentiality is done in full conformance with requirements from the Sunnybrook Research Ethics Board, the University Health Network Research Ethics Board and Health Canada.
Safety
Lifestyle therapy is indicated for people who have stage 1 HTN (140–159/90–99 mm Hg) with no underlying risk factors.1 Linden has previously demonstrated the role and safety of the wait-list control methodology and determined it to be appropriate in studies with stage 1 and 2 hypertensives (140–179/90–109 mm Hg).23 64 In accordance with the Canadian standard of care for BP management, all participants receive standard recommendations of suggested lifestyle modifications for BP management at study entry.
With participant consent, primary care physician(s) are informed of their patient's participation in the study. Physicians are asked to delay the start of their patient's antihypertensive therapy until after they have completed the study. If physicians believe that antihypertensive should be initiated, they are asked to communicate their decision to study staff before doing so. A letter updating their patient's progress, along with laboratory and ABPM results, is sent to the primary care physician after each study visit.
Automated office BP safety assessments are included to closely monitor subjects' BP. The primary investigator is notified if subjects exceed BP safety limits. If any of the following conditions are discovered during study, enrolment participants are withdrawn and treated: (1) increases in ABP of 20/10 mm Hg or greater, (2) accelerated HTN with an office reading of 160/100 mm Hg or greater, (3) macrovascular target organ damage, (4) diabetes mellitus or (5) chronic kidney disease (GFR<60 ml/min). Any subject started on antihypertensive therapy during the study remains in the study, and the initiation of medical therapy is recorded.
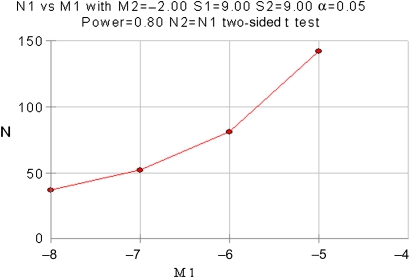
Sample size considerations
The main objective of this study was to assess the difference in mean awake and 24 h systolic and diastolic ABP 12 weeks post-baseline between the treatment and wait-list control arm. The following calculations/analyses are based on the work by Linden and the difference in mean SBP between treatment groups measured as by ABPM. Linden found a 6.1 mm Hg SBP drop from baseline to the end of the primary assessment period for participants in the immediate intervention group; the wait-list control group showed a 0.9 mm Hg increase in the same time interval23 This resulted in a 7.0 mm Hg difference between the two groups,23 a relatively large treatment effect, due in part to the use of subjects with higher BP.
Unlike Linden who found BP rising in the control group, more recent results from the Double Exposure Study found that BP tended to fall over time, even in unmedicated hypertensives. This may have been due in part to an adoption of lifestyle changes.77 78 Baseline data from the unmedicated hypertensive cohort in the Double Exposure Study demonstrated mean awake ABP equal to 137/85±8/5 mm Hg. After 1 year, mean awake ABP had fallen to 133/83±8/7 mm Hg. Based on these results, it is reasonable to assume that BP will fall in the HARMONY wait-list control arm.
Very conservative assumptions were made for the HARMONY power analysis. A reduction of 2.0 mm Hg for mean systolic ABP (half the change observed in the Double Exposure Study) was assumed for the control group (compared to the rise that Linden found23). The variance recorded in the study by Linden (9 mm Hg) was used for the HARMONY power analysis; variance higher than that recorded in the Double Exposure cohort (8 mm Hg in only 35 subjects). Linden found a BP difference of 7.0 mm Hg between the treatment and control group. In our power analysis, the difference between treatment and control groups was reduced from the results of Linden to a more conservative value, 6 mm Hg. This value was chosen for two reasons: (1) it was closer to findings from the meta-analysis of Dickinson11 and (2) participants' overall BP is anticipated to be lower in the HARMONY Study (stage 1 hypertensives) compared to Linden's study (stage 1 and stage 2 hypertensives).23 Using a two-tailed two-sample t test, an estimated group SD of 9.0 mm Hg and a significance level of 0.05, it was determined that a sample size of 37 subjects in each group would provide sufficient power (81%) to detect a SBP difference of 6.0 mm Hg between the null hypothesis (both groups start with equal means and have an equal a drop in SBP of 8.0 mm Hg) and the alternative hypothesis (control group SBP will fall by only 2.0 mm Hg). To account for potential dropouts and subjects lost to analysis (25% lost in the study by Linden23), the number of subjects was increased to 50 subjects per group (figure 2).
Figure 2.
Power analysis graph illustrating necessary sample size.
Statistical analysis
The primary outcome will be examined using an intent-to-treat analysis. An intent-to-treat population is defined as all subjects in the study who completed at least one session of MBSR. The primary outcome measure is mean awake and 24 h systolic and diastolic ABP. ABP between treatment and control will be compared by two-tailed two-sample t test at the end of the 12-week primary outcome period. Within-subject analysis of the effect of MBSR on ABP will be performed by a paired t test. Persistence of effect of MBSR on BP will be assessed using repeated analysis of variance measures, comparing group differences between subsequent study visits (baseline, pre-MBSR, post-MBSR and study close-out). The proportion of subjects achieving BP targets will be analysed using χ2 tests. Multiple regression analyses will be employed to assess differences in BP between subjects while adjusting for covariates. Subjects may be started on antihypertensive therapy during the study. If this leads to imbalance between the study arms, a per-protocol analysis may be performed to take this variable into account. All analyses will be carried out using SAS V.9.1 (SAS Institute).
Ethical considerations
This research project is approved by the research ethics board at Sunnybrook Research Institute (Toronto, Canada) and the University Health Network Research Ethics Board (Toronto, Canada). Planned data analyses are in full conformance with the principles of the ‘Declaration of Helsinki’.79 Conduct of the HARMONY Study is fully adherent to the principles outlined in the ‘Guideline for Good Clinical Practice’ ICH Tripartite Guideline (January 1997)80 and in the second edition of Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans.81
Dissemination plans
Data collection will be completed by early spring 2012. Primary and secondary analysis will commence immediately after data monitoring is completed; publications will be prepared for submission in the summer of 2012. Study findings are also planned to be presented at the following conferences: October 2012: Hypertension Canada, May 2013: American Society of Hypertension, June 2013: European Society of Hypertension, September 2013: International Society of Hypertension.
Supplementary Material
Acknowledgments
We would like to extend our gratitude and sincere thanks to Sarah Greenwood and Theresa Dudley for all of their hard work. We would also like to thank the Centre for Statistical Design and Analysis for their advice on the present project, as well as the Heart and Stroke Foundation of Ontario for their support of the study.
Footnotes
To cite: Blom K, How M, Dai M, et al. Hypertension Analysis of stress Reduction using Mindfulness meditatiON and Yoga (The HARMONY Study): study protocol of a randomised control trial. BMJ Open 2012;2:e000848. doi:10.1136/bmjopen-2012-000848
Contributors: ST and BB conceptualised the study, and MD, MM, SA, BLA, NP and JI assisted with the study design. KB, MH and MD collected data, which were overseen by NP. KB and MH cleaned the collected data, preformed interim analyses and interpreted interim results. ST is the guarantor. KB, MD, MH and ST wrote and revised the article, as well as designed figures. NP, BB, MM, SA, BLA and JI critically revised the draft for important intellectual content. All authors approved the final version to be published.
Funding: This work was supported by Heart and Stroke Foundation of Ontario (NA 6349). The Heart and Stroke Foundation of Ontario played no role in the study design, data collection, writing of this article or the decision to submit it for publication.
Competing interests: None.
Ethics approval: Ethics approval was provided by Sunnybrook Research Ethics Board and University Health Network Research Ethics Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data available.
References
- 1.Rabi DM, Daskalopoulou SS, Padwal RS, et al. The 2011 Canadian hypertension education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol 2011;27:415–33 [DOI] [PubMed] [Google Scholar]
- 2.Chockalingam A, Campbell NR, Fodor JG. Worldwide epidemic of hypertension. Can J Cardiol 2006;22:553–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasan RS, Larson MG, Leip EP, et al. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 2001;358:1682–6 [DOI] [PubMed] [Google Scholar]
- 4.Julius S, Nesbitt S, Egan B, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med 2006;354:1685–97 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Preventing chronic diseases: a vital investment. http://www.who.int/chp/chronic_disease_report/contents/en/index.html (accessed 27 Apr 2007).
- 6.Stamler J, Rose G, Stamler R, et al. INTERSALT study findings. Public health and medical care implications. Hypertension 1989;14:570–7 [DOI] [PubMed] [Google Scholar]
- 7.Appel LJ. Lifestyle modification as a means to prevent and treat high blood pressure. J Am Soc Nephrol 2003;14:S99–102 [DOI] [PubMed] [Google Scholar]
- 8.O'Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–23 [DOI] [PubMed] [Google Scholar]
- 9.Canter PH, Ernst E. Insufficient evidence to conclude whether or not transcendental meditation decreases blood pressure: results of a systematic review of randomized clinical trials. J Hypertens 2004;22:2049–54 [DOI] [PubMed] [Google Scholar]
- 10.Parati G, Steptoe A. Stress reduction and blood pressure control in hypertension: a role for transcendental meditation? J Hypertens 2004;22:2057–60 [DOI] [PubMed] [Google Scholar]
- 11.Dickinson HO, Mason JM, Nicolson DJ, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens 2006;24:215–33 [DOI] [PubMed] [Google Scholar]
- 12.Manikonda JP, Stork S, Togel S, et al. Contemplative meditation reduces ambulatory blood pressure and stress-induced hypertension: a randomized pilot trial. J Hum Hypertens 2008;22:138–40 [DOI] [PubMed] [Google Scholar]
- 13.Wenneberg SR, Schneider RH, Walton KG, et al. A controlled study of the effects of the transcendental meditation program on cardiovascular reactivity and ambulatory blood pressure. Int J Neurosci 1997;89:15–28 [DOI] [PubMed] [Google Scholar]
- 14.Castillo-Richmond A, Schneider RH, Alexander CN, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke 2000;31:568–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schneider RH, Staggers F, Alxander CN, et al. A randomised controlled trial of stress reduction for hypertension in older African Americans. Hypertension 1995;26:820–7 [DOI] [PubMed] [Google Scholar]
- 16.Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons > or = 55 years of age with systemic hypertension. Am J Cardiol 2005;95:1060–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paul-Labrador M, Polk D, Dwyer JH, et al. Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med 2006;166:1218–24 [DOI] [PubMed] [Google Scholar]
- 18.Schneider RH, Alexander CN, Staggers F, et al. A randomized controlled trial of stress reduction in African Americans treated for hypertension for over one year. Am J Hypertens 2005;18:88–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nidich SI, Rainforth MV, Haaga DA, et al. A randomized controlled trial on effects of the transcendental meditation program on blood pressure, psychological distress, and coping in young adults. Am J Hypertens 2009;22:1326–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson JW, Liu C, Kryscio RJ. Blood pressure response to transcendental meditation: a meta-analysis. Am J Hypertens 2008;21:310–16 [DOI] [PubMed] [Google Scholar]
- 21.Rainforth MV, Schneider RH, Nidich SI, et al. Stress reduction programs in patients with elevated blood pressure: a systematic review and meta-analysis. Curr Hypertens Rep 2007;9:520–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beck AT. The current state of cognitive therapy: a 40-year retrospective. Arch Gen Psychiatry 2005;62:953–9 [DOI] [PubMed] [Google Scholar]
- 23.Linden W, Lenz JW, Con AH. Individualized stress management for primary hypertension: a randomized trial. Arch Intern Med 2001;161:1071–80 [DOI] [PubMed] [Google Scholar]
- 24.Kabat-Zinn J. Full Catastrophe Living: Using The Wisdom Of Your Body And Mind To Face Stress, Pain And Illness. New York: Delta, 1990 [Google Scholar]
- 25.Praissman S. Mindfulness-based stress reduction: a literature review and clinician's guide. J Am Acad Nurse Pract 2008;20:212–16 [DOI] [PubMed] [Google Scholar]
- 26.Plews-Ogan M, Owens JE, Goodman M, et al. A pilot study evaluating mindfulness-based stress reduction and massage for the management of chronic pain. J Gen Intern Medicine 2005;20:1136–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain 2008;134:310–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Esmer G, Blum J, Rulf J, et al. Mindfulness-based stress reduction for failed back surgery syndrome: a randomized controlled trial. J Am Osteopath Assoc 2010;110:646–52 [PubMed] [Google Scholar]
- 29.Rosenzweig S, Greeson JM, Reibel DK, et al. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. J Psychosom Res 2010;68:29–36 [DOI] [PubMed] [Google Scholar]
- 30.Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med 1998;21:581–99 [DOI] [PubMed] [Google Scholar]
- 31.Astin JA. Stress reduction through mindfulness meditation. Effects psychological symptomatology, sense control, spiritual experiences. Psychother Psychosom 1997;66:97–106 [DOI] [PubMed] [Google Scholar]
- 32.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992;149:936–43 [DOI] [PubMed] [Google Scholar]
- 33.Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Women's Ment Health 2008;11:67–74 [DOI] [PubMed] [Google Scholar]
- 34.Vollestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behav Res Ther 2011;49:281–8 [DOI] [PubMed] [Google Scholar]
- 35.Barnhofer T, Duggan D, Crane C, et al. Effects of meditation on frontal alpha-asymmetry in previously suicidal individuals. Neuroreport 2007;18:709–12 [DOI] [PubMed] [Google Scholar]
- 36.Kenny MA, Williams JM. Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behav Res Ther 2007;45:617–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kingston J, Chadwick P, Meron D, et al. A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. J Psychosom Res 2007;62:297–300 [DOI] [PubMed] [Google Scholar]
- 38.Grossman P, Tiefenthaler-Gilmer U, Raysz A, et al. Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom 2007;76:226–33 [DOI] [PubMed] [Google Scholar]
- 39.Sephton SE, Salmon P, Weissbecker I, et al. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis Rheum 2007;57:77–85 [DOI] [PubMed] [Google Scholar]
- 40.Schmidt S, Grossman P, Schwarzer B, et al. Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Pain 2011;152:361–9 [DOI] [PubMed] [Google Scholar]
- 41.Kristeller JL, Hallett CB. An exploratory study of a meditation-based intervention for binge eating disorder. J Health Psychol 1999;4:357–63 [DOI] [PubMed] [Google Scholar]
- 42.Kabat-Zinn J, Wheeler E, Light T, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosom Med 1998;60:625–32 [DOI] [PubMed] [Google Scholar]
- 43.Carlson LE, Speca M, Faris P, et al. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun 2007;21:1038–49 [DOI] [PubMed] [Google Scholar]
- 44.Carlson LE, Speca M, Patel KD, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology 2004;29:448–74 [DOI] [PubMed] [Google Scholar]
- 45.Carlson LE, Speca M, Patel KD, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med 2003;65:571–81 [DOI] [PubMed] [Google Scholar]
- 46.Henderson VP, Clemow L, Massion AO, et al. The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Res Treat 2012;131:99–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lengacher CA, Johnson-Mallard V, Barta M, et al. Feasibility of a mindfulness-based stress reduction program for early-stage breast cancer survivors. J Holist Nurs 2011;29:107–17 [DOI] [PubMed] [Google Scholar]
- 48.Lengacher CA, Johnson-Mallard V, Post-White J, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology 2009;18:1261–72 [DOI] [PubMed] [Google Scholar]
- 49.Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology 2009;18:571–9 [DOI] [PubMed] [Google Scholar]
- 50.Matchim Y, Armer JM, Stewart BR. Mindfulness-based stress reduction among breast cancer survivors: a literature review and discussion. Oncol Nurs Forum 2011;38:E61–71 [DOI] [PubMed] [Google Scholar]
- 51.Matchim Y, Armer JM, Stewart BR. Effects of mindfulness-based stress reduction (MBSR) on health among breast cancer survivors. West J Nurs Res 2011;33:996–1016 [DOI] [PubMed] [Google Scholar]
- 52.Matousek RH, Dobkin PL. Weathering storms: a cohort study of how participation in a mindfulness-based stress reduction program benefits women after breast cancer treatment. Curr Oncol 2010;17:62–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smith JE, Richardson J, Hoffman C, et al. Mindfulness-based stress reduction as supportive therapy in cancer care: systematic review. J Adv Nurs 2005;52:315–27 [DOI] [PubMed] [Google Scholar]
- 54.Witek-Janusek L, Albuquerque K, Chroniak KR, et al. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun 2008;22:969–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psychooncology 2010;19:1004–9 [DOI] [PubMed] [Google Scholar]
- 56.Rosenzweig S, Reibel DK, Greeson JM, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med 2007;13:36–8 [PubMed] [Google Scholar]
- 57.Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Sci Pract 2003;10:125–43 [Google Scholar]
- 58.Grossman P, Niemann L, Schmidt S, et al. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res 2004;57:35–43 [DOI] [PubMed] [Google Scholar]
- 59.Bohlmeijer E, Prenger R, Taal E, et al. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res 2010;68:539–44 [DOI] [PubMed] [Google Scholar]
- 60.Ditto B, Eclache M, Goldman N. Short-term autonomic and cardiovascular effects of mindfulness body scan meditation. Ann Behav Med 2006;32:227–34 [DOI] [PubMed] [Google Scholar]
- 61.Barnes VA, Treiber FA, Davis H. Impact of transcendental meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. J Psychosom Res 2001;51:597–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barnes VA, Davis HC, Murzynowski JB, et al. Impact of meditation on resting and ambulatory blood pressure and heart rate in youth. Psychosom Med 2004;66:909–14 [DOI] [PubMed] [Google Scholar]
- 63.Van Wielingen LE, Carlson LE, Campbell TS. Mindfulness-based stress reduction (MBSR), blood pressure and psychological functioning in women with cancer. [abstract]. Psychosom Med 2007;69:A43 [Google Scholar]
- 64.Linden W, Moseley JV. The efficacy of behavioral treatments for hypertension. Appl Psychophysiol Biofeedback 2006;31:51–63 [DOI] [PubMed] [Google Scholar]
- 65.Kingston T, Dooley B, Bates A, et al. Mindfulness-based cognitive therapy for residual depressive symptoms. Psychol Psychotherapy 2007;80:193–203 [DOI] [PubMed] [Google Scholar]
- 66.Spielberger C, Jacobs G, Russel S, et al. Assessment of anger: the state-trait anger scale. In: Butcher J, Spielberger C, eds. Advances in Personality Assesment. Hillsdale, NJ: Lawrence Erlbaum Associates, 1983:112–89 [Google Scholar]
- 67.Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002;52:69–77 [DOI] [PubMed] [Google Scholar]
- 68.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–96 [PubMed] [Google Scholar]
- 69.Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:953–62 [DOI] [PubMed] [Google Scholar]
- 70.Karasek R, Brisson C, Kawakami N, et al. The job content questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 1998;3:322–55 [DOI] [PubMed] [Google Scholar]
- 71.Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment 2008;15:329–42 [DOI] [PubMed] [Google Scholar]
- 72.Evans C, Connell J, Barkham M, et al. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE-OM. Br J Psychiatry 2002;180:51–60 [DOI] [PubMed] [Google Scholar]
- 73.Lau MA, Bishop SR, Segal ZV, et al. The Toronto mindfulness scale: development and validation. J Clin Psychol 2006;62:1445–67 [DOI] [PubMed] [Google Scholar]
- 74.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985;8:163–90 [DOI] [PubMed] [Google Scholar]
- 75.Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosom Med 2002;64:71–83 [DOI] [PubMed] [Google Scholar]
- 76.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry 1982;4:33–47 [DOI] [PubMed] [Google Scholar]
- 77.Baker B, Paquette M, Szalai JP, et al. The influence of marital adjustment on 3-year left ventricular mass and ambulatory blood pressure in mild hypertension. Arch Intern Med 2000;160:3453–8 [DOI] [PubMed] [Google Scholar]
- 78.Tobe SW, Kiss A, Sainsbury S, et al. The impact of job strain and marital cohesion on ambulatory blood pressure during 1 year: the double exposure study. Am J Hypertens 2007;20:148–53 [DOI] [PubMed] [Google Scholar]
- 79.World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Seoul: From the 59th World Medical Association Assembly, 2008. http://www.wma.net/en/30publications/10policies/b3/17c.pdf (accessed 29 Dec 2011). [Google Scholar]
- 80.Health Canada Int Conf Harmonization (ICH) Guidance E6. Good Clin Pract Consolidated Guidel, 1997. http://www.hc-sc.gc.ca/dhp-mps/prodpharma/applic-demande/guide-ld/ich/efficac/e6-eng.php (accessed 29 Dec 2011). [Google Scholar]
- 81.Goverment of Canada Panel Of Research Ethics. 2nd edn Of Tri-Council Policy Statement: Ethical Conduct for research involving Humans, 2010. http://www.pre.ethics.gc.ca/eng/policy-politique/initiatives/tcps2-eptc2/Default/ (accessed 29 Dec 2011). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.