Abstract
Purpose
To evaluate the impact of individualised patient care, as an adjunct to standard care, on adherence to ocular hypotensive therapy.
Methods
A two-arm, single-masked exploratory randomised controlled trial recruited patients newly prescribed ocular hypotensive therapy. The intervention involved an individual assessment of health-care needs and beliefs and a 1-year follow-up period according to need. The primary outcome was refill adherence, measured by collating prescription and dispensing data for 12 months. Secondary outcomes included self-reported adherence, glaucoma knowledge, beliefs about illness and medicines, quality of care, intraocular pressure (IOP) fluctuation, and changes in clinical management assessed at 12 months. The strength of the intervention was measured following withdrawal by reviewing clinical outcomes for a further 12 months.
Results
In all, 127 patients were recruited (91% response rate). Intervention-arm patients collected significantly more prescriptions than control-arm patients. Self-report adherence was significantly better in the intervention-arm for patients who forgot drops and those who intentionally missed drops. The intervention group demonstrated significantly more glaucoma knowledge, expressed a significantly stronger belief in the necessity of eye drops and believed that they had more personal control over managing their condition. Control-arm patients had more IOP fluctuation and changes in clinical management. However, this finding only reached significance at 24 months.
Conclusion
Modelling patient care according to health-care needs and beliefs about illness and medicines can have a significant impact on improving adherence to therapy for this patient group, with the potential benefit of improving clinical outcomes.
Keywords: randomised controlled trial, open-angle glaucoma, ocular hypertension, adherence, ocular hypotensive therapy
Introduction
Successful management of patients diagnosed with ocular hypertension (OHT) or open-angle glaucoma (OAG) aims to prevent visual disability and blindness1 and relies on achieving a reduction in intraocular pressure (IOP) to slow down disease progression2, 3 or to prevent conversion of OHT to glaucoma.4 First-line therapy usually takes the form of ocular hypotensive eye drops. However, achieving good reduction rates can be hindered by poor adherence to therapy, which is known to be highly prevalent in chronic, asymptomatic diseases such as glaucoma.5 Poor adherence can be mistaken for suboptimal drug efficacy, which can result in additional medications or necessitate surgery,6 potentially increasing risk, cost, and further aggravating adherence issues.
Improving education has been seen as a key aspect in changing adherence behaviour.7, 8 A systematic review found inconsistencies in the assessment of knowledge.9 A survey by Hoevenaars et al6 did not find an overall improvement in adherence with better education, but found certain factors to correlate with adherence, such as previous knowledge of glaucoma, social support, and fulfilled information needs. Patients' ability to manage glaucoma medications can differ according to their socioeconomic status, health-care experiences, and health beliefs.10, 11, 12 Understanding individual patients' needs and providing follow-up support accordingly may prove to be more effective in promoting adherence than a standardised approach.
There is a scarcity of good-quality adherence studies. A 2009 Cochrane review13 found only eight randomised controlled trials (RCTs) involving adherence interventions, and only two that tested education and tailoring14, 15 (organising drop taking around daily routines); one was successful but lacked sufficient evidence to guarantee quality14 and the other that was underpowered did not find a significant difference in adherence.15 Both were short-term trials. The most recently published RCT, involving 66 patients and a 3-month follow-up, found a significant difference in adherence rates with a multi-faceted intervention involving a 10-min educational video, a review of barriers to drop taking, reminder phone calls, and a dosing aid device.16
There is a need for RCTs with longer follow-up times to evaluate the longevity of an adherence intervention for OHT and OAG patients. Our exploratory RCT tested the hypothesis that individualised patient care, according to health-care needs and beliefs, can improve adherence to ocular hypotensive therapy. The intervention incorporated a prescriptive assessment of needs and a 1-year follow-up period. The strength of the intervention was assessed following withdrawal by reviewing clinical outcomes for a further 12 months.
Materials and methods
Study design
The study design was a two-arm, single-masked, exploratory RCT with a 1-year follow-up period.
Participants
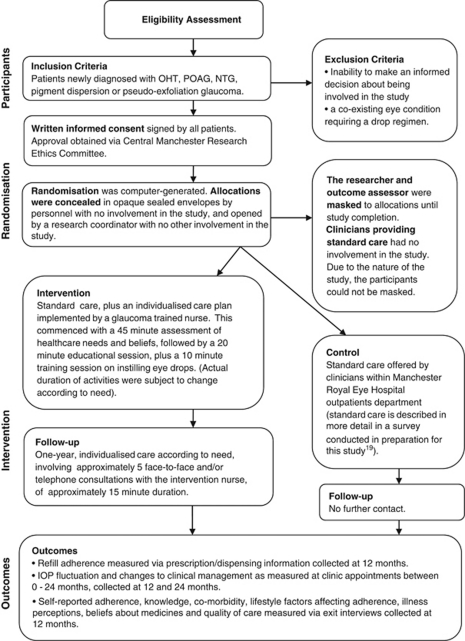
Patients were recruited consecutively from Manchester Royal Eye Hospital (MREH) clinics between April 2006 and April 2007. Eligible patients were newly diagnosed with OHT or OAG. The methods flow diagram in Figure 1 provides further details. Ethical approval was obtained from the Central Manchester Research Ethics Committee and the trial was registered with the ISRCTN (http://www.controlled-trials.com/ISRCTN13706134). We certify that all applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during this research.
Figure 1.
Methods flow diagram.
Randomisation
Computer-generated randomisation was conducted by a statistician with no involvement in data collection. Patients were allocated to receive either individualised patient care in addition to standard care or standard care alone. Stratified random sampling ensured equal proportions of patients within each arm from specialist glaucoma and general ophthalmic clinics.
Intervention and follow-up
Intervention-arm patients were contacted by the intervention nurse for a face-to-face needs assessment. The assessment incorporated medical history, physical, psychological, and lifestyle factors affecting drop instillation. This involved developing a deeper understanding of particular issues; for example, for a patient with poor dexterity, difficulties instilling drops would be explored. For a patient suffering from depression or short-term memory loss, motivation and reminder techniques would be investigated. Assessment for patients working night shifts or away from home would include issues integrating a drop regimen into their lifestyle. Patients' understanding of glaucoma was checked by establishing knowledge of prognosis, follow-up, repeat prescriptions, and duration of treatment. Beliefs about illness17 and medicines18 were assessed by incorporating questions to establish whether patients believed eye drops could cure or control glaucoma, or whether they worried about side effects or any long-term effects of therapy. After the assessment, patients were observed instilling eye drops.
A 1-year follow-up care plan was designed and implemented according to health-care needs, based on education and support, which was tailored to gaps in glaucoma knowledge, pre-existing beliefs, and ability to manage an eye drop regimen. An initial face-to-face educational session included facts about glaucoma given verbally and supplemented with booklets produced by the International Glaucoma Association. Drop instillation training and drop aids were provided as required. Drop diaries were given to all patients to monitor and act as a reminder for drop instillation in the initial weeks of therapy. Advice and support was offered to assist patients in incorporating a drop regimen into their daily routine. Liaison and training for informal carers and health-care professionals (pharmacists, district nurses, hospital nursing staff, and care home staff) involved in the patient's care were written into the care plan as required. Agreed time intervals were set for follow-up consultations, and patients were given the intervention nurse's contact telephone number for advice or assistance between consultations.
Follow-up involved ongoing training and support by both face-to-face and telephone consultations. This incorporated a review of drop diaries in the initial weeks of therapy (these were continued if found beneficial as a reminder tool), reminders to collect and use drops, and repetition of information as required. Needs were reassessed and the level of support adjusted accordingly at the end of each consultation. The intervention nurse was the same throughout, and the intervention was guided by prescriptive documentation. The methods flow chart (Figure 1) provides more details.
Standard care
There is no policy to define standard care within MREH. Education, advice, and support may vary from clinic to clinic. A preliminary survey found education and adherence promotion to be limited for many patients.19
Outcomes
The primary outcome was refill adherence measured by contacting general practitioners and pharmacists for prescription and dispensing information during the 1-year follow-up period. A bottle of ocular hypotensive drops has an expiry period of 28 days in the United Kingdom; therefore, patients are expected to commence a new bottle every 28 days to maintain therapy as prescribed. Refill adherence was calculated as an interval variable using the following formula:
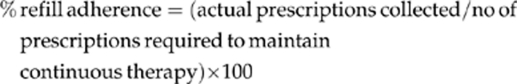 |
The refill adherence measure was dichotomised to provide a definition of good/poor refill adherence. Poor refill adherence was defined as <100% prescriptions collected.
Adherence was also measured by self-report in conjunction with knowledge, physical, psychological, and lifestyle factors affecting adherence, beliefs about illness and medicines, and quality of care. All were measured using questionnaires completed during exit interviews at the end of the 12-month follow-up period. Exit interviews involved four questionnaires, namely the Revised Glaucoma Adherence Questionnaire (GAQ-R), the Revised Illness Perception Questionnaire (IPQ-R),17 Beliefs about Medicines Questionnaire (BMQ),18 and the Patient Enablement Instrument (PEI).20 The original GAQ was developed and piloted during an earlier study19 and revised to become the GAQ-R in preparation for this RCT. This 39-item questionnaire included 14 questions, which tested glaucoma knowledge, with a maximum score of 19 (Table 1). The revised knowledge questions showed good internal consistency with Cronbach's α=0.90. Four questions explored intentional and non-intentional drop omission,18 and the remaining questions explored social status, co-morbidity, support, and lifestyle factors affecting adherence. The IPQ-R,17 and BMQ18 have been used extensively in chronic conditions. The PEI20 has previously been used to measure quality of care in primary-care settings. Minor modifications were made (with original authors' permission) to improve clarity for glaucoma patients; for example, the word ‘medicines' was modified to eye drops in the BMQ. Scoring and computation were performed as specified by the originators.17, 18, 20
Table 1. Knowledge scoring system (modified from earlier version19).
| GAQ-RQ no. | Question |
Patients' responses were allocated a score if the
following information was included
|
||||
|---|---|---|---|---|---|---|
| Scored 0 | Scored 1 | Scored 2 | Scored 3 | Max score | ||
| 3 | What condition do you have? | Do not know/incorrect answer | Glaucoma/ocular hypertension or raised eye pressure | NA | NA | 1 |
| 4 | Can you tell me which part of the eye becomes damaged in glaucoma? | Do not know/incorrect answer | Back of the eye | Retina | Optic nerve | 3 |
| 5 | What do you think causes the damage? | Do not know/incorrect answer | Raised pressure/weak optic nerve/poor blood supply | NA | NA | 1 |
| 6 | Are there any symptoms that act as a warning that glaucoma is developing? | Do not know/incorrect answer | No | NA | NA | 1 |
| 7 | Can you tell me what effect glaucoma has on vision if left untreated? | Do not know/incorrect answer | You go blind/you gradually go blind/you lose vision | You get tunnel vision | NA | 2 |
| 8 | Can you tell me what part of vision glaucoma affects the most? | Do not know/incorrect answer | Visual field/field of vision/side vision | NA | NA | 1 |
| 9 | Is glaucoma hereditary? | Do not know/incorrect answer | Yes | NA | NA | 1 |
| 10 | Can you tell me the three most important investigations/tests that are carried out regularly to monitor changes in your condition? | Do not know/incorrect answer | Either IOP measurement or visual field test or optic nerve head examination (in patients' own words) | Any two of the tests (in patients' own words) | All three tests (in patients own words) | 3 |
| 11 | Do you know the name(s) of the drop(s) that has/have been prescribed for you? | Do not know/incorrect answer | Yes (drop(s) named and answers checked against prescription) | NA | NA | 1 |
| 12 | Do you know what the drops do? | Do not know/incorrect answer | Lower/reduce/control eye pressure | NA | NA | 1 |
| 13 | How can you tell the drops are working? | Do not know/incorrect answer | I cannot/the doctor tells me at clinic | NA | NA | 1 |
| 14 | Do you know how long you will have to use drops for? | Do not know/incorrect answer | For life/forever | NA | NA | 1 |
| 15 | How often do you collect prescriptions? | Do not know/incorrect answer | Collects 1 bottle per 28 days/month or 2 bottles every 2 months, etc. | NA | NA | 1 |
| 17 | After opening a bottle do you know how long you can use drops before they expire? | Do not know/incorrect answer | 1 month/28 days | NA | NA | 1 |
| Total | 19 | |||||
Clinical outcomes included IOP mean, IOP fluctuation (SD of IOP measures from the worse eye, using Goldmann Applanation Tonometry), and changes in clinical management (change or addition of eye drops and/or surgical intervention). The data were collected from patients' hospital records for between-group comparisons at 12 months (the end of the follow-up period) and then at 24 months. The 24-month assessment allowed for testing the intervention effect after a 12-month withdrawal. IOP level recordings and decisions regarding clinical management were made at routine clinic visits and were the responsibility of clinicians with no involvement in the study.
Sample size
A pragmatic approach was adopted for sample size calculation (in the absence of similar studies for comparison) based on the number of eligible patients attending MREH. A 12-month recruiting period and an expected 80% take-up rate led to the estimation that 120 patients could be recruited. This study was exploratory because it was not possible to detect a predetermined effect for the primary outcome.
Data analysis
Demographic and clinical variables were expressed in frequencies, means, and SD when distributions were normal and in medians and range when skewed. We analysed under the intention-to-treat (ITT) principle. Differences between randomised groups were analysed by Pearson's test for dichotomous variables, the test for trend for ordinal variables, Student's t-test for normally distributed interval data, and Mann–Whitney U-test when skewed. Linear regression analysis was performed to identify independent predictors of refill adherence. Tests were two tailed with α=0.05. Analysis was conducted with SPSS 16.0 (IBM SPSS, Chicago, IL, USA).
Results
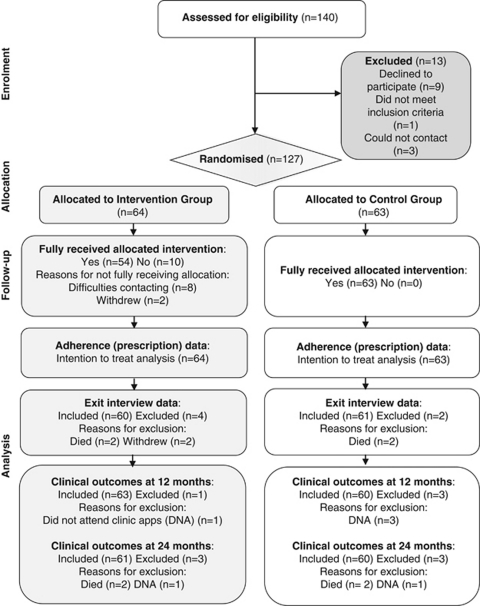
A total of 140 patients were invited to participate, but 13 were excluded before randomisation, giving a response rate of 91%. The remaining 127 patients were randomised to receive individualised care in addition to standard care (intervention group, n=64) or standard care alone (control group, n=63). In all, 54 patients of the intervention group (84%) received the intervention in full. Ten intervention-arm patients did not receive the intervention in full either because of withdrawal from the study (n=2) or due to difficulties contacting patients (n=8). Separate descriptive analyses were undertaken to examine this group's beliefs, adherence behaviour, and clinical outcomes. The CONSORT flow diagram21 (Figure 2) provides details of participant numbers at each stage.
Figure 2.
Consort flow diagram.21
Patient characteristics
Baseline demographic characteristics were similar (Table 2), apart from gender, in which by chance there were slightly more women in the intervention group and more men in the control group (the difference would not have been significant had it been a testable hypothesis).
Table 2. Baseline characteristics.
| Baseline characteristics | Intervention (n=64) n (%) | Control (n=63) n (%) |
|---|---|---|
| Age | ||
| Mean (SD) | 65.4 (13.1) | 67.2 (12.0) |
| Range | 36–91 | 30–88 |
| Gender | ||
| Male | 27 (42.2) | 37 (58.7) |
| Female | 37 (57.8) | 26 (41.3) |
| Ethnicity | ||
| White British/Irish/other White background | 60 (93.7) | 54 (85.7) |
| Black African/Caribbean | 2 (3.1) | 6 (9.5) |
| Mixed White/Black African background | 1 (1.6) | 0 (0.0) |
| Asian Indian/Pakistani | 1 (1.6) | 3 (4.8) |
| Education | ||
| No qualifications | 36 (56.2) | 37 (58.8) |
| One or more GCSE/O level/CSE/Leavers cert | 9 (14.1) | 8 (12.7) |
| Vocational qualification/one or more A level | 14 (21.9) | 12 (19.0) |
| First/higher degree | 5 (7.8) | 6 (9.5) |
| Known glaucoma family history | ||
| Yes | 20 (31.2) | 21 (33.3) |
| No | 44 (68.8) | 42 (66.6) |
| IOP | ||
| Mean (SD) | 25.3 (7.2) | 25.1 (5.8) |
| IOP (Pre-therapy) | ||
| Mean (SD) | 25.3 (7.2) | 25.1 (5.8) |
| Prescription (All patients were commenced on single therapy) | ||
| Travoprost OD | 47 (73.4) | 41 (65.1) |
| Latanoprost OD | 13 (20.3) | 16 (25.4) |
| Bimatoprost OD | 0 (0.0) | 1 (1.6) |
| Timoptol La OD | 3 (4.7) | 3 (4.8) |
| Timolol maleate BD | 1 (1.6) | 2 (3.2) |
Adherence
In an ITT analysis, good refill adherence was found to be significantly better in the intervention arm (70% vs 43%, χ2=9.75, df=1, P=0.002). Intervention-arm patients collected significantly more prescriptions than did control-arm patients (Mann–Whitney Z=−3.56, P<0.001). Nine intervention-arm patients who did not receive the full intervention were classed as having poor refill adherence.
Self-report adherence was also found to be significantly better in the intervention group for patients who intentionally (Mann–Whitney Z=−6.22, P<0.001) and unintentionally missed drops (Mann–Whitney Z=−6.68, P<0.001). Reasons for intentionally missing drops included inconvenience when away from home, not renewing prescription in time, and discontinuing therapy because of feeling no benefit. Drops were unintentionally missed due to a change of routine, for example, when working away from home, in hospital, or on holiday. Control-arm patients reported missing significantly more drops on average per month than did intervention-arm patients (χ2(trend)=39.52, df=1, P<0.001).
Illness perceptions
Intervention-arm patients believed that they had more personal control over managing (Mann–Whitney Z=−4.65, P<0.001) and influencing glaucoma (Mann–Whitney Z=−5.83, P<0.001), and that their own actions could determine the course of their condition (Mann–Whitney Z=−5.75, P<0.001). There were no differences between the groups in emotional representation, for example, being angry, anxious, or afraid of their condition (Mann–Whitney Z=−0.53, P=0.599) or overall treatment control (Mann–Whitney Z=−1.01, P=0.315). However, for the statement, ‘My treatment can control my condition', control-arm patients scored significantly lower, indicating their uncertainty (Mann–Whitney Z=−6.85, P<0.001). Four intervention-arm patients who did not receive the intervention in full also scored low for this item.
Beliefs about medicines
Intervention-arm patients expressed a significantly stronger belief in the necessity of drops (Mann–Whitney Z=−5.58, P<0.001) and significantly less concern about long-term effects (Mann–Whitney Z=−4.28, P<0.001). Control-arm patients were significantly more concerned about harm (Mann–Whitney Z=−6.01, P<0.001) and overuse of medicines in general (Mann–Whitney Z=−3.84, P<0.001). Intervention-arm patients who did not receive the full intervention had similar mean scores to the control group for the necessity of drops (16.6, SD 4.2), concerns about harm of medicines in general (9.1, SD 2.0), and higher scores for concerns regarding overuse of medicines (14.8, SD 2.6).
Knowledge
Intervention-arm patients were significantly more knowledgeable about glaucoma (Mann–Whitney Z=−6.81, P<0.001). The median knowledge score was 14 (range 2–18) for the intervention group and 6 (range 0–17) for the control group. The median knowledge score for intervention-arm patients who did not receive the full intervention was 8 (range 4–15).
Quality of care
Intervention-arm patients believed that they were significantly more enabled to understand, cope with, and manage their condition and were more confident about their eye care than were control-arm patients (Mann–Whitney Z=−8.60, P<0.001).
Clinical outcomes
At the end of the 12-month follow-up period, there was no statistical difference between the intervention and control group in mean IOP (16.9, SD 3.6 vs 17.4, SD 3.5 mm Hg, respectively, t=−0.78, df=123, P=0.435). The difference in IOP fluctuation at 12 months was not significant (2.7, SD 1.7 vs 3.2, SD 1.9, t=−1.71, df=121, P=0.090). There was no difference in changes in clinical management at 12 months. Twenty-six (41%) of the intervention group and 27 (45%) of the control group had medication changes (χ2=0.17, df=1, P=0.676). Three control-arm patients and one intervention-arm patient who did not receive the full intervention did not attend clinic appointments during the 12-month follow-up period.
At 24 months, there was no significant difference in mean IOP (17.0, SD 3.4 mm Hg vs 17.1, SD 2.9 mm Hg, t=−0.26, df=124, P=0.795), yet a statistically significant difference was found in IOP fluctuation (2.7, SD 1.5 vs 3.4, SD 1.5 mm Hg, t=−2.53, df=119, P=0.013) and changes in clinical management (χ2=4.39, df=1, P=0.036). Control-arm patients were found to have significantly more IOP fluctuation and changes to therapy/surgical intervention (21 intervention-arm patients had changes in clinical management vs 32 control-arm patients). Two control-arm and two intervention-arm patients who did not receive the full intervention regularly failed to attend clinic appointments between 13 and 24 months. Six of the latter had changes in clinical management within this period.
Significant clinical outcome findings were entered into a linear regression model. The model identified that the intervention, IOP fluctuation, and changes in clinical management were significant independent predictors of refill adherence, as shown in Table 3. Patients with good adherence had the least IOP fluctuation and changes in clinical management and were more likely to be in the intervention group.
Table 3. Summary of linear regression analysis for refill adherence.
| Variable | Coefficient | P-value | 95% CI |
|---|---|---|---|
| Intervention | 9.8 | 0.017 | 1.82–17.83 |
| IOP fluctuation 0–24 months | −3.3 | 0.017 | −6.02 to −0.62 |
| Changes in clinical management between 13 and 24 months | −10.6 | 0.014 | −19.01 to −2.21 |
R2=0.46, adjusted R2=0.21, ANOVA F=10.39, df=3,117, P<0.001.
Discussion
The findings support the hypothesis that an intervention based on individualised care according to health-care needs and beliefs can have a positive effect on adherence behaviour to ocular hypotensive therapy.
As far as the authors are aware, this is the first adherence intervention to be based on an assessment of health-care needs and beliefs about illness and medicines for patients prescribed ocular hypotensive therapy. Other RCTs in this field have assisted patients to tailor drop instillation around daily activities, but not assessed individual needs and beliefs.14, 15, 16, 22 In an earlier study,19 we found that patients vary in terms of the support required to manage therapy effectively; therefore, individualised patient care based on need appears to be more appropriate than standard care in promoting adherence.
Intervention intensity and duration may be the key to promoting good adherence. It is known that adherence improves with attention,23 often causing the adherence rate to improve equally in intervention and control groups.15, 24 Education and training in the initial months of commencing therapy helps prevent poor adherence from developing.25 We focused on specific gaps in knowledge and challenged pre-existing beliefs. Intervention intensity decreased over time, but many patients required repetition of information and advice throughout the follow-up period and continued support to maintain motivation. For some, a change in circumstances or increasing comorbidity during the study led to greater need. The 1-year follow-up period allowed for changes in the intensity of support and provided a security net for patients at risk of poor adherence.
It has been argued that it is difficult to establish the most effective component of multi-faceted regimes.16, 26 Our intervention involved a number of elements, but these were centred around a prescriptive assessment of health-care needs and beliefs on which education and ongoing support was based. Although education is frequently highlighted as being important in improving adherence,7, 27 we feel as others do,6, 28 that education alone may not adequately tackle the problem.
Beliefs about illness and medicines have been widely researched in chronic disease,29, 30, 31, 32 but not until recently in glaucoma. A cross-sectional survey of glaucoma patients, which incorporated the Brief IPQ33 and the BMQ,18 found as we did that patients with poor adherence had more concerns and less belief in the necessity of drops.34 Intervention-arm patients were more aware of the consequences of glaucoma and believed that they had more control over their treatment and course of their disease. These findings are reflective of the education and support provided by the intervention nurse in our study.
In other chronic diseases such as renal transplant or diabetes, minimal deviation from a therapy regimen is associated with rapid negative outcomes.24, 35 However, in glaucoma, a long-term follow-up is necessary to monitor the effect of poor adherence on clinical outcomes. Okeke et al16 compared IOP levels at the end of a 3-month follow-up period, but found no difference between groups; this may have been due to the short-term follow-up period. IOP fluctuation is a potential risk factor for glaucomatous damage,36 and poor adherence may result in IOP fluctuation over time. In our study, IOP levels in the control group were found to vary more than those in the intervention group; but only reached significance at 24 months. Control group patients also experienced more changes in clinical management between 13 and 24 months. The linear regression model revealed that these factors together with intervention were significant predictors of adherence. Reviewing clinical outcomes after a period of withdrawal of the intervention also provided insights into the duration of intervention effect.
Of the intervention-arm patients who did not receive the intervention in full, 90% did not collect adequate prescriptions to maintain continuous therapy and 60% demonstrated poor clinical outcomes at 24 months. These patients either withdrew from the study or were difficult to contact because of other priorities or a belief that their condition did not warrant assistance in managing drops. However, at interview, these patients were found to have a fairly poor knowledge of glaucoma, did not feel that drops were a necessity, and were less confident about managing their condition than other intervention-arm patients. According to Pound et al,37 people who resist medicine taking should be recognised and assisted with information, feedback, and support. The assessment used in this study could assist in identifying patients who may be at risk of poor adherence, so that action can be taken. Further research is warranted to explore those who resist glaucoma medications.
Although refill adherence is an objective measure, it does not capture all aspects of adherence behaviour. Electronic monitoring may have provided more details, but we did not want to raise awareness of the monitoring process, which may have resulted in a change of behaviour38 by patients or clinicians. To minimise performance bias, clinicians were not involved in the study apart from their role in referring eligible patients. A meta-analysis found self-report to be a good estimate of patient adherence when compared with electronic monitoring.39 The good correlation between self-report and refill adherence found in our study and reported elsewhere40, 41, 42 supports the validity of these two measures. In combination, they can assist in achieving an accurate measure for patient adherence.39
It is unfortunate that more reliable clinical outcome measures could not be used, but within the time scale and number of follow-up visits, it is unlikely that changes in the visual field or optic nerve head would reach significance. IOP recordings taken at clinic visits are known to be unreliable at predicting adherence as some patients pay more attention to medication taking immediately before and after clinic appointments;16, 43 however, as both IOP fluctuation and changes in clinical management correlated well with refill and self-report adherence, the authors believe their inclusion was justified for the time period available.
This RCT has demonstrated that modelling patient care according to health-care needs and beliefs about illness and medicines can have a significant impact on improving adherence to ocular hypotensive therapy with the potential to delay disease progression.
Acknowledgments
The project was jointly funded by the University of Manchester and Pfizer Limited UK and supported by the Manchester Academic Health Sciences Centre (MAHSC) and the NIHR Manchester Biomedical Research Centre. We thank Professor John Howie for his permission to use the PEI and Professor Rob Horne for his permission to use the BMQ and IPQ-R and for his advice regarding this paper. Pfizer Limited UK provided funding for research support, but had no role in the design or conduct of this research.
Pfizer Limited UK provided funding for research support, which included computer equipment and part funding of Ms Trish Gray's salary. Dr Robert Harper and Ms Anne Fiona Spencer have been paid by Pfizer Limited UK as lecturers and workshop facilitators at educational events. Ms Cecilia Fenerty, Dr Malcolm Campbell, Professor David Henson, and Professor Heather Waterman do not have any financial interests to disclose.
References
- Forsman E, Kivela T, Vesti E. Lifetime visual disability in open-angle glaucoma and ocular hypertension. J Glaucoma. 2007;16 (3:313–319. doi: 10.1097/IJG.0b013e318033500f. [DOI] [PubMed] [Google Scholar]
- Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK. Visual field progression in the Collaborative Initial Glaucoma Treatment Study the impact of treatment and other baseline factors. Ophthalmology. 2009;116 (2:200–207. doi: 10.1016/j.ophtha.2008.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The AGIS Investigators The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130 (4:429–440. doi: 10.1016/s0002-9394(00)00538-9. [DOI] [PubMed] [Google Scholar]
- Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma Arch Ophthalmol 2002120(6701–713.discussion 829–730. [DOI] [PubMed] [Google Scholar]
- Sleath B, Ballinger R, Covert D, Robin AL, Byrd JE, Tudor G. Self-reported prevalence and factors associated with nonadherence with glaucoma medications in veteran outpatients. Am J Geriatr Pharmacother. 2009;7 (2:67–73. doi: 10.1016/j.amjopharm.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Hoevenaars JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Will improvement of knowledge lead to improvement of compliance with glaucoma medication. Acta Ophthalmol. 2008;86 (8:849–855. doi: 10.1111/j.1755-3768.2007.01161.x. [DOI] [PubMed] [Google Scholar]
- Chen X, Chen Y, Sun X. Notable role of glaucoma club on patients' knowledge of glaucoma. Clin Exp Ophthalmol. 2009;37 (6:590–594. doi: 10.1111/j.1442-9071.2009.02101.x. [DOI] [PubMed] [Google Scholar]
- Herndon LW, Brunner TM, Rollins JN. The glaucoma research foundation patient survey: patient understanding of glaucoma and its treatment. Am J Ophthalmol. 2006;141 (1 Suppl:S22–S27. doi: 10.1016/j.ajo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- Olthoff CM, Schouten JS, van de Borne BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112 (6:953–961. doi: 10.1016/j.ophtha.2004.12.035. [DOI] [PubMed] [Google Scholar]
- Cross V, Shah P, Bativala R, Spurgeon P. Glaucoma awareness and perceptions of risk among African-Caribbeans in Birmingham, UK. Divers Health Social Care. 2005;2 (2:81–90. [Google Scholar]
- Hoevenaars JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Socioeconomic differences in glaucoma patients' knowledge, need for information and expectations of treatments. Acta Ophthalmol Scand. 2006;84 (1:84–91. doi: 10.1111/j.1600-0420.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- Sleath B, Robin AL, Covert D, Byrd JE, Tudor G, Svarstad B. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113 (3:431–436. doi: 10.1016/j.ophtha.2005.10.034. [DOI] [PubMed] [Google Scholar]
- Gray TA, Orton LC, Henson D, Harper R, Waterman H.Interventions for improving adherence to ocular hypotensive therapyCochrane Database of Systematic Reviews (2): Art. no. CD006132. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006132.pub2/pdf. [DOI] [PubMed]
- Norell SE. Improving medication compliance: a randomised clinical trial. Br Med J. 1979;2 (6197:1031–1033. doi: 10.1136/bmj.2.6197.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard J, Warner J, Kelley K. An evaluation of the effectiveness of a nurse-led glaucoma monitoring clinic. Int J Ophthal Nurs. 2003;7 (2:15–21. [Google Scholar]
- Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y, et al. Interventions improve poor adherence with once daily glaucoma medications in electronically monitored patients. Ophthalmology. 2009;116 (12:2286–2293. doi: 10.1016/j.ophtha.2009.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron L, Buick D. The Revised Illness Perception Questionnaire (IPQ-R) Psychol Health. 2002;17 (1:1–16. [Google Scholar]
- Horne R, Weinman J, Hankins M. The Beliefs about Medicines Questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14 (1:1–24. [Google Scholar]
- Gray TA, Fenerty C, Harper R, Lee A, Spencer AF, Campbell M, et al. Preliminary survey of educational support for patients prescribed ocular hypotensive therapy. Eye (Lond) 2010;24 (12:1777–1786. doi: 10.1038/eye.2010.121. [DOI] [PubMed] [Google Scholar]
- Howie JG, Heaney DJ, Maxwell M, Walker JJ. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract. 1998;15 (2:165–171. doi: 10.1093/fampra/15.2.165. [DOI] [PubMed] [Google Scholar]
- Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148 (4:295–309. doi: 10.7326/0003-4819-148-4-200802190-00008. [DOI] [PubMed] [Google Scholar]
- Laster SF, Martin JL, Fleming JB. The effect of a medication alarm device on patient compliance with topical pilocarpine. J Am Optom Assoc. 1996;67 (11:654–658. [PubMed] [Google Scholar]
- Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009;116 (2:191–199. doi: 10.1016/j.ophtha.2008.09.004. [DOI] [PubMed] [Google Scholar]
- De Geest S, Schafer-Keller P, Denhaerynck K, Thannberger N, Kofer S, Bock A, et al. Supporting medication adherence in renal transplantation (SMART): a pilot RCT to improve adherence to immunosuppressive regimens. Clin Transplant. 2006;20 (3:359–368. doi: 10.1111/j.1399-0012.2006.00493.x. [DOI] [PubMed] [Google Scholar]
- Lacey J, Cate H, Broadway DC. Barriers to adherence with glaucoma medications: a qualitative research study. Eye. 2009;23 (4:924–932. doi: 10.1038/eye.2008.103. [DOI] [PubMed] [Google Scholar]
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X.Interventions for enhancing medication adherence Cochrane Database Systematic Review 2008(2): Art. No: CD000011. DOI: 10.1002/14651858.CD000011.pub3(2): CD000011. [DOI] [PubMed]
- Danesh-Meyer HV, Deva NC, Slight C, Tan YW, Tarr K, Carroll SC, et al. What do people with glaucoma know about their condition? A comparative cross-sectional incidence and prevalence survey. Clin Exp Ophthalmol. 2008;36 (1:13–18. doi: 10.1111/j.1442-9071.2007.01624.x. [DOI] [PubMed] [Google Scholar]
- Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60 (7:657–665. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- Horne R, Graupner L, Frost S, Weinman J, Wright SM, Hankins M. Medicine in a multi-cultural society: the effect of cultural background on beliefs about medications. Soc Sci Med. 2004;59 (6:1307–1313. doi: 10.1016/j.socscimed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47 (6:555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Reynolds NR, Testa MA, Marc LG, Chesney MA, Neidig JL, Smith SR, et al. Factors influencing medication adherence beliefs and self-efficacy in persons naive to antiretroviral therapy: a multicenter, cross-sectional study. AIDS Behav. 2004;8 (2:141–150. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs. J Hum Hypertens. 2004;18 (9:607–613. doi: 10.1038/sj.jhh.1001721. [DOI] [PubMed] [Google Scholar]
- Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60 (6:631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Rees G, Leong O, Crowston JG, Lamoureux EL. Intentional and unintentional nonadherence to ocular hypotensive treatment in patients with glaucoma. Ophthalmology. 2010;117 (5:903–908. doi: 10.1016/j.ophtha.2009.10.038. [DOI] [PubMed] [Google Scholar]
- Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes. Am J Med. 2000;108 (1:20–27. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- Lee PP, Walt JW, Rosenblatt LC, Siegartel LR, Stern LS. Association between intraocular pressure variation and glaucoma progression: data from a United States chart review. Am J Ophthalmol. 2007;144 (6:901–907. doi: 10.1016/j.ajo.2007.07.040. [DOI] [PubMed] [Google Scholar]
- Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61 (1:133–155. doi: 10.1016/j.socscimed.2004.11.063. [DOI] [PubMed] [Google Scholar]
- Leonard K, Masatu MC. Outpatient process quality evaluation and the Hawthorne effect. Soc Sci Med. 2006;63 (9:2330–2340. doi: 10.1016/j.socscimed.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Shi L, Liu J, Fonseca V, Walker P, Kalsekar A, Pawaskar M. Correlation between adherence rates measured by MEMS and self-reported questionnaires: a meta-analysis. Health Qual Life Outcomes. 2010;8:99. doi: 10.1186/1477-7525-8-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42 (7:649–652. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- George J, Shalansky SJ. Predictors of refill non-adherence in patients with heart failure. Br J Clin Pharmacol. 2007;63 (4:488–493. doi: 10.1111/j.1365-2125.2006.02800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Benner JS, Glynn RJ, Winkelmayer WC, Mogun H, Avorn J. How well do patients report noncompliance with antihypertensive medications? A comparison of self-report versus filled prescriptions. Pharmacoepidemiol Drug Saf. 2004;13 (1:11–19. doi: 10.1002/pds.819. [DOI] [PubMed] [Google Scholar]
- Dreer LE, Girkin C, Mansberger SL.Determinants of medication adherence to topical glaucoma therapy J Glaucoma 2011. e-pub ahead of print 26 May 2011; doi: 10.1097/IJG.0b013e31821dac86 [DOI] [PMC free article] [PubMed]