Summary
To compare the effective rates among one week, two week and four week treatment sessions of ozone therapy for lumbar disc herniation to provide a foundation for clinical decision-making. One hundred and eighty-seven lumbar disc herniation patients were divided into three groups, 103 cases for one week, 61 cases for two week and 23 cases for four week treatment sessions.
The clinical curative effective rates in the three groups were 82.52%, 85.24% and 95.65% respectively. The effective rate among the three groups showed no significant difference at statistical analysis. Considering the cost-effectiveness of ozone therapy, increasing the treatment course does not enhance the curative effect.
Key words: lumbar disc herniation, ozone, curative effect evaluation
Introduction
Ozone therapy for lumbar disc herniation has already achieved impressive results. It is popular with little trauma and a safe and good curative effect for the patients. As many factors can affect the curative effect of ozone therapy, it is important how the treatment session is chosen.
There are several treatment sessions with two weeks, three weeks and seven weeks popular in recent years. To date there has been no comparison of these treatment sessions showing which is the best length of ozone therapy. For clinicians, choosing a proper treatment course could not only improve the clinical effective rate, but also cut the cost of the therapy and shorten the time spent in hospital. These issues will be discussed in this article.
Materials and Methods
Clinical Record
From November 2003 to October 2008, 187 patients with diagnostically confirmed lumbar disc herniation entered the study. Their average age was 45.8 years old (ranging from 21 to 75 years) and patients included 115 men and 72 women. All patients complained of sciatica and low back pain lasting from one month to 12 years. In physical examination, all patients showed Lasègue's sign positive reaction. Diagnostic verification by CT and MRI exhibited disc protrusion with nerve root or thecal sac compression. The disc lesions in all patients occurred between L4/5 and L5/ S1.
These cases were classified into three groups for one week, two week and four week treatment sessions to compare the difference in clinical curative effect.
Group 1: a one week treatment course in which the patient only had one interventional procedure and dehydration medicine venous injection treatment for three days.
Group 2: a two week treatment session in which the patient had one interventional procedure and dehydration medicine venous injection treatments for three days repeated seven days later.
Group 3: a four week treatment session in which the patient had two interventional procedures and dehydration medicine venous injection treatments for three days repeated 28 days later.
Instrumenst and Equipment
X-Ray machine: We used the C-shaped XRay machine or CT to perform the procedure. The X-Ray machine is capable of multiple positions with high definition TV surveillance.
Ozone Generator: the generator can produce an oxygen-ozone mixture at a concentration of at least 25 μg/ml with real-time display of concentration and pressure. The concentration is stable and has a redox system.
Puncture needle: Slant needle or multi-side hole tapered hollow needle with 20-22G diameter.
Oxygen: High-pressure medical pure oxygen cylinders.
Indication for treatment
Patients with lumbar disc protrusion after failure of conservative treatment.
Procedure Method
The patient is positioned lying position on the healthy side with a pillow placed under the waist to fully extend the interspaces of the lumbar vertebrae. Some patients with a high ileum can take the position of crooking the lower side, straightening the upper side. 21G multiwhole or Chiba needles were selected for puncture. We defined the puncture point at the level of the disc lesion disc from 7~8 cm to the middle of the spine and then puncture the disc from the posterolateral approach after conventional disinfection and 2% lidocaine local anesthesia.
It is important to make sure the needle tip is located in the central lumbar space or lower third region in the anteroposterior and lateral perspective position. Imaging clearly shows the extent of disc herniation and whether or not the disc is broken. Radicular pain can induced to define the injured disc, but we do not usually do this as it will aggravate the pressure on the lumbar disc. Setting up the oxygen-ozone mixture at a concentration of 40Ìg/ml, the operator obtained a 10 ml oxygen-ozone mixture (it is important to avoid mixing the air) to inject into the lumbar disc at uniform speed.
The injection resistance is quite high in contained herniation patients and rupture of the annulus fibrosis must be avoided when pushing the gas into the disc space. The gas can be seen dispersing in irregular lines under in the disc space. In this condition we should adopt the "low-pressure injection cycle method" by pushing the injector handle back and forth repeatedly and then abandoning the remaining gas for the purpose of fully oxidating the nucleus and keep it unruptured. On the other hand, we can see the gas readily entering the epidural cavity in patients with ruptured annulus fibrosis depicting the lumbar posterior marginal linear optical image. Drawing the needle to the lumbar posterior marginal plane, we inject 1015 ml gas mixture into this area after confirming the needle point is not in the subarachnoid cavity. You can see the gas dispersing in the clearance of the psoas major muscle.
Lastly, we pull the needle out after injecting the anti-inflammation and pain killer liquid for nerve root block. There are three kinds of antiinflammation and pain killer liquid prescription, the first is dexamethasone 5 mg plus 2% lidocaine 5 ml; the second is prednisolone acetate 50 mg plus 2% lidocaine 5 ml; the third is diprospan 7 mg (including beclomethasone betamethasone 5 mg and betamethasone sodium phosphate 2 mg), mecobalamin 0.5 mg plus 2% lidocaine 5 ml. We chose the third prescription in this group.
The patients rest in bed for one day after the procedure. All the patients should be admitted to hospital and placed on an intravenous drip of 20% mannitol 250 ml, 5 mg dexamethasone and neurotrophic drugs for three days. Patients should then take full rest for two weeks after discharge, and then do muscle training according to their recovering condition. All patients must avoid weight-bearing and strong activities in the first six months after treatment.
The curative effect was evaluated by Macnab's criteria (Table 1).
Table 1.
Macnab curative effect evaluation criteria.
| Curative effect level |
Clinical manifestation |
|---|---|
| Significant effective |
Symptoms disappeared, normal work resumed |
| Effective | Symptoms disappeared evidently, be able to do light work |
| Common | Symptoms improved, not be able to work |
| No effect | Symptoms not improved |
Statistical analysis
Fisher's Exact Test fourfold table files were used to compare the one, two and four week treatment sessions. The level of statistical significance is P=0.05.
Results
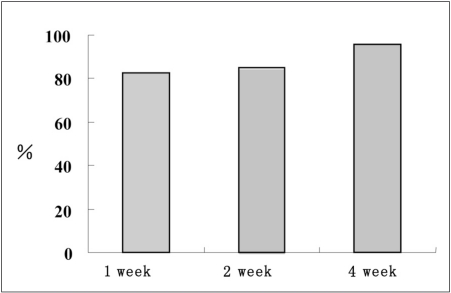
There were no significant differences in the three groups for age, sex, disease course or clinical feature after the variance analysis (P>0.05). We followed up all patients for three to forty-eight months after the procedure. The outcome was determined by the doctors. The total effective rate was 85.02% (159/187) in all groups. The effective rate was 82.52% (85/103) after the one 1 week treatment, 85.24% (52/61) after two weeks treatment and 95.65% (22/23) after four weeks treatment (Figure 1).
Figure 1.
The total effective rate in three different groups.
There were no significant differences in the total effective rate in the three groups (P=0.280) after statistical analysis.The statistical comparison between one week and two weeks, one week and four weeks, two weeks and four weeks showed no differences (Table 2).
Table 2.
Statistical analysis of the three treatment sessions.
| Treatment session |
Number of cases |
Number of effective cases |
Effective rate |
Chi-Square value |
P |
|---|---|---|---|---|---|
| 1 week | 103 | 85 | 82.52 | 2.549 | 0.280 |
| 2 weeks | 61 | 52 | 85.24 | ||
| 4 weeks | 23 | 22 | 95.65 | ||
| 1 week vs 2 weeks | 0.206 | 0.650 | |||
| 1 week vs 4 weeks | 0.194* | ||||
| 2 weeks vs 4 weeks | 0.272* | ||||
| * Fisher's Exact Test result. | |||||
Discussion
Many factors influence the curative effect of lumbar disc herniation, especially the choice of treatment sessions. We selected patients with disc protrusion and use the same therapy method to avoid the impact of other factors as far as possible. The focus of this article is the influence of different treatment sessions on the curative effect.
There exist uncertainty about the mechanism underlying the local injection of an O2/O3 mixture directly into intradiscal space. Bocci, a physiologist at Siena University in Italy hypothesized a mechanism. Based on his hypothesis and combining the results from our animal tests and human studies, we suggest the following mechanisms of action.
Oxidation of proteoglycan in the nucleus pulposus. Ozone is a potent oxidant with a halflife of twenty minutes at normal temperature. The oxidation process finishes in a very short time. Ozone causes oxidation of proteoglycan in the disc nucleus pulposus and triggers water loss and then decreases the osmotic pressure of disc tissue. The disc nucleus exhibited shrinkage, degeneration, necrosis and atrophy, which relieve compression on the nerve root. In our animal experiments, this mechanism was verified by the dog disc nucleus that appeared shrunken, lost elastic features and became rough one month after ozone injection into the intradiscal space. The degeneration, necrosis and atrophy of the dog disc nucleus were observed two to three months later, but there was no disc change in the control group which received pure oxygen injection only.
Anti-inflammatory action. Back pain and sciatica are caused not only by mechanical compression of the herniated disc on the nerve root, but also by non-bacterial inflammation induced by local never root edema and effusion resulting from local venous circulation blockage. Meanwhile, the inflammatory factors such as histamine, β-protein and glycoproteins released from damaged discal tissue could stimulate the nerve root to cause pain. It is possible for ozone injection into intradiscal and paraspinal spaces to relieve the pain by blocking the release of inflammatory factors and directly expanding the blood vessels to improve local circulation, reduce local never root edema and conglutination.
Analgesic action. One hypothesis from acupuncture treatment for low back pain and sciatica holds that fine needle acupuncture into intradiscal and paraspinal spaces stimulates the inhibiting interneurons to produce endophilinlike substances which play an important role in the relief of pain. This was called "chemical acupuncture"1. The ozone treatment session could relieve the pain within one to three days by this pain relief pathway.
For the pharmacological mechanisms underlying oxygen-ozone therapy for herniated disc, Simonetti et Al postulated that pain caused by nerve root compression should be deemed a symptom of multifactorial origin in which the neural and perineural inflammatory reaction and its biohumoral mediators play a major role, flanked by venous stasis due to mass effect on the perineural circulation. Nerve compression appears to play an adjuvant role by generating nerve conduction abnormalities due to fibre demyelination with a direct or indirect anoxicischaemic mechanism. As pain is multifactorial, ozone may also have a multifactorial pharmacological effect alleviating disc compression by shrinkage and triggering pro-fibrosing mechanisms in the herniated disc thereby counteracting the inflammatory cascade of biohumoral and cell-mediated components and improving the hypoxic status linked to arterial compression and venous stasis. Lastly, ozone may have a reflex therapy effect ("chemical acupuncture") breaking the chain of chronic pain stimulating anti-nociceptor analgesic mechanisms2.
Comparison of treatment strategies in different countries
The popular treatment method in Italy in around 2000 was a two week treatment session with widely different curative effects. Muto and Avella in Italy reported the effective rate in 93 cases was 78% in 19983. Alexandre in Spain who published a multi-center study from İ994 to 2000 reported a total effective rate of 93.3% including 5392 cases (80.9%) whose pain was completely relieved, 827 cases (12.4%) whose symptoms improved and 446 cases (6.7%) whose symptoms had worsened4. He et Al in China reported the total effective rate was 75.8% in 129 cases in 20035. Andreula et Al reported combined intradiscal and periganglionic injection of medical ozone and periganglionic injection of steroids has a cumulative effect that enhances the overall outcome of treatment for pain caused by disc herniation. The effective rate in their report was excellent or good outcome in 70.3% and success in 78.3% in 20036. Bonetti et Al reported their experience of intraforaminal O2-O3 versus periradicular steroidal infiltrations in lower back pain. They reported that oxygen-ozone treatment was highly effective in relieving acute and chronic lower back pain and sciatica. The gas mixture was administered as a first treatment to replace epidural steroids. Clinical outcomes were poor in 13 (15.1%) out of 86 patients receiving O2-O3 infiltration and in 18 (22.5%) out of 80 patients receiving steroid injection. Among patients without disc disease, six (8.6%) out of 70 patients receiving O2-O3 infiltration but 21.4% of the patients receiving steroid injections had poor outcomes 7.
Pepa et Al in Argentina reported on a seven week treatment session 5. They used the ozone mixture at a concentration of 27 ug/ml injecting 7 ml into the lumbar disc and around 3 ml into the nerve root and 1 ml into the corresponding bilateral small joint space in the first week. Then they injected 30 ml each time into the lumbar muscles from the third to the seventh week. Their series of 104 cases included ten cases of cervical vertebra disc herniation, 94 cases of lumbar disc herniation. The effective rate was 78 cases (75%) had completely pain relief, 25 cases (24.04%) had improvement and one case (0.96%) worsened. The authors claimed that ozone treatment is an effective way to treat low back pain compared with surgery with obvious advantages in terms of low risk and low cost 8.
At the same time, Kumar et Al in India reported on a three week treatment session treating 70 cases after conservative treatment failed. They injected 4 ml of ozone mixture at a concentration of 29 ug/ml into the lumbar disc and then injected with 12 ml of the same concentration of ozone mixture around the dural sac and 12 ml into the lumbar foramen in the first week. Lastly, they injected around the nerve root, vertebral lamina and lumbar foramen with same method in the third week. The whole ozone treatment course was combined with physical treatment sessions, convalescence, physical training, biotechnology, psychology and nutrition consultation, etc. Their results indicated that the effective rate was 88%, including 55% significant effect, 33% effective and 12% no change with no complications 9.
Bonetti et Al reported on oxygen-ozone therapy associated with magnetic bioresonance in degenerative arthrosis of the spine. They also used the four treatment sessions method with a clinical curative rate of 81%10.
Conclusions
In our series, there was no significant statistical difference between one and two treatment sessions, so that increasing treatment course did not improve the curative effect. This means we should advocate a single treatment session as the first choice, and postpone a second injection after one month's observation. This strategy will not only guarantee the curative effect, but also reduce the cost of treatment.
References
- 1.Bocci V, et al. Oxygen-Ozone treatment session: a critical evaluation. Dordrecht: Kluwer Academic Publishers; 2002. pp. 241–324. [Google Scholar]
- 2.Simonetti L, Raffi L, et al. Pharmacological mechanisms underlying oxygen-ozone therapy for herniated disc. Rivista Italiana di Ossigeno-Ozonoterapia. 2003;2:7–11. [Google Scholar]
- 3.Muto M, Avella F. Percutaneous treatment of lumbar disc herniation by intradiscal oxygen-ozone injection. Interventional Neuroradiology. 1998;4:273–286. doi: 10.1177/159101999800400403. [DOI] [PubMed] [Google Scholar]
- 4.Alexandre A. Intradiscal injection of O2-O3 to treat lumbar disc herniation. Rivista Italiana di Ossigeno-Ozonoterapia. 2002;1:165–169. [Google Scholar]
- 5.He XF, Yu ZJ, et al. Treatment of lumbar disc herniation by using percutaneous intradiscal and paraspinal space injection of O2-O3 mixture. Chin J Radiol. 2003;37:9. [Google Scholar]
- 6.Andreula CF, Simonetti L, et al. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. Am J Neuroradiol. 2003;24:996–1000. [PMC free article] [PubMed] [Google Scholar]
- 7.Bonetti M, Fontana A, et al. Intraforaminal O2-O3 versus periradicular steroidal infiltrations in lower back pain: randomized controlled study. Am J Neuroradiol. 2005;26:996–1000. [PMC free article] [PubMed] [Google Scholar]
- 8.Pepa O, Ferrario A, et al. Oxygen-ozone treatment session experience in Argentina. Interventional Neuroradiology. 2005;11(Sup 2):82–83. [Google Scholar]
- 9.Kumar VS. Intradiscal ozonucleolysis using fluoroscopic image guidance. The India experience. Interventional Neuroradiology. 2005;11(Sup 2):83. [Google Scholar]
- 10.Bonetti M, Fontana A, Parodi F. Oxygen-ozone therapy associated with magnetic bioresonance in degenerative arthrosis of the spaine:preliminary findings. International Journal of Ozone Therapy. 2007;6:29–35. [Google Scholar]