Abstract
Thinners are chemical mixtures used as industrial solvents. Humans can come into contact with thinner by occupational exposure or by intentional inhalation abuse. Thinner sniffing causes damage to the brain, kidney, liver, lung, and reproductive system. We discuss some proposed mechanism by which thinner induces damage. Recently, the induction of oxidative stress has been suggested as a possible mechanism of damage. This paper reviews the current evidence for oxidative stress effects induced by thinner inhalation. Early ideas about the effects of thinner on lipids are discussed in one section. We discuss several studies that have shown the oxidative effects of thinner inhalation on: lipid peroxidation, levels of antioxidant enzymes, glutathione depletion, and oxidation of proteins and DNA. We have also included studies about oxidative stress effects induced by toluene, the principal component (60-70%) of thinner. Finally, work describing the effects of oxidative stress induced by thinner inhalation on different organs is discussed.
Keywords: Organ effects, oxidative stress, thinner inhalation
INTRODUCTION
Intentional inhalation is a health problem throughout the world. The majority of drug users are children or adolescents, and most of them get are initiated as drug abuser with thinner. One of the reasons of this is that it is easily available and inexpensive compared to other drugs.[1–3] Conversely, toxicology mechanism of thinner inhalation as mix is not frequent studied. Oxidative stress effects on these organs by thinner inhalation are reviewed. A systematic review was carried out in PubMed using the word thinner inhalation 96 articles were reviewed only 12 describes oxidative stress effect of thinner inhalation considering thinner as mix.
THINNER COMPOSITION
Thinner is a solvent mixture used in both household products and industrial settings; it has a highly variable composition, displaying both temporal and geographic differences. In addition, thinner components vary depending on regulatory specifications or processing techniques. Toluene and acetone were the most abundant compounds in commercial thinner samples from Mexico City analyzed in 1997. These samples were analyzed by gas chromatography, and the toluene content varied from 7% to 77%;[4] benzene was identified in 62% of the samples, and it accounted for 0% to 2.2% (average 0.3%, v/v). In Japan, Saito[5] analyzed four thinner preparations by capillary gas chromatography. Acetone and methyl isobutyl ketone, together with toluene, were the most common solvents found; chlorinated hydrocarbons and ethylene glycol derivatives were seldom detected.
Proportions of ingredients vary significantly; current regulatory laws have greatly reduced the inclusion of benzene, and in Mexico, there is a commercial thinner without benzene. This is important, since benzene is classified as genotoxic by the IARC.[6]
EARLY IDEAS ABOUT MECHANISM OF TOXICITY
The major component of thinner is toluene, a well-known neurotoxic agent. Acute and chronic effects of toluene on neurons have been well documented.[7] The first ideas to explain the mechanism of the neurotoxic effects of solvents such as toluene were based on the lipid hypothesis, which proposed that perturbation of the lipid bilayer would result in dysfunctional membrane proteins. Solvents were thought act on lipids in the cell membrane, because toluene and other solvents have lipophilic properties that allow them to reach high concentrations in the CNS. In this review, we include some studies about the effect of toluene on lipids. Lipid changes were observed in rat brain exposed to toluene (320 ppm) for 30 days. Total phospholipids were reduced in the cerebral cortex, where a slight increase in phosphatidic acid was also observed. No changes were observed in the brainstem. The mechanism for these changes is uncertain.[8] Studies of the effects of toluene on membrane fluidity demonstrated that in vivo administration of toluene in rat (1 g/kg, 1 h, i.p.) increased the synaptosomal membrane fluidity. The authors proposed a specific toluene-phospholipid interaction in synaptosomes that resulted in altered membrane composition and fluidity.[9] The same authors showed later that toluene increased phospholipid methylation and stimulated Na and K adenosine triphosphatase (ATPase) activity in synaptosomes both in vivo and in vitro.[10]
Inhibition of the integral enzymes acetylcholinesterase (AChE) and ATPase of rat synaptosomal membrane after incubation with 3 mM toluene was observed in vitro. Disruption of lipid–protein interactions was suggested as a mechanism of inhibition.[11]
Recently, biophysical studies of the protein-lipid interface, curvature elasticity, and the polymorphic potential of lipid assemblies have shown the dynamics of the lipid membrane, which can influence the function of membrane proteins. Changes in membrane lipids have an effect on elastic fluctuations of the lipid bilayer that influence protein insertion and conformational changes in the protein structure that are important for protein function.[12]
OXIDATIVE STRESS
Oxidative stress is a cellular state characterized by an excess of oxidants (reactive oxygen and nitrogen species) that overwhelms the antioxidant capacity. Oxidants are constituted by free radical species containing reactive oxygen and nitrogen species. The presence of unpaired electrons makes them unstable and highly reactive. DNA, RNA, proteins, and lipids are the targets of these radicals. Reactive oxygen species (ROS) include oxygen-derived free radicals: the superoxide anion radical and the hydroxyl radical or its derivates, such as hydrogen peroxide. ROS are the result of the aerobic environment, and the superoxide anion radical arises during mitochondrial respiration. Coenzyme Q (CoQ) sporadically loses an electron in the transfer of reducing equivalents through the electron chain. This electron is transferred to dissolve O2 producing superoxide. It is estimated that 1-2% of the O2 consumed by mitochondria is converted to the superoxide anion radical.[13] Oxidative stress induces oxidation of lipids, proteins, and DNA in cells and a response of a variety of cellular detoxification systems: superoxide dismutase (SOD), glutathione peroxidase (GPX), and glutathione (GSH).
Thinner inhalation induces oxidative stress. Activation of free radical processes underlies the effect of many toxic substances like: ethanol, toluene, ionizing radiation, lead, arsenate, etc.[14] In the case of thinner, there are some proposed mechanisms:
One of them is the oxidative metabolism of benzene, toluene, xylene, ethanol, acetone, and tri-methylbenzene which generates cytosolic NADH. NADH is oxidized indirectly by mitochondria electron transport depending on hydrogen shuttling mechanism that involve carriers in the mitochondrial inner membrane. This condition that increases mitochondrial NADH and enhance the reducing pressure on the electron transport chain without increasing the rate of respiration promotes the formation of O2 in the electron transport chain.[15]
The production of quinones by cytochrome P450, particularly during toluene, and benzene metabolism is another mechanism proposed. These quinones are able to establish a futile redox cycle (quinones and semiquinone radicals), during which cytotoxic ROS are accumulated.[16]
Another mechanism is non-mitochondrial which increase ROS formation. Metabolism of thinner's components results in activation of cytochrome P450 isoforms like CYP2E1 which is prone to radical formation.[17]
In addition, toxic substances exposures cause inflammation. In the case of thinner, inhalation induces inflammatory response in lungs. Considerable evidence supports a role of inflammatory mediators released by phagocytic leukocytes and infiltrating macrophages in the generation of reactive oxygen and nitrogen species in lung. Macrophages produce NO (nitric oxide) via an inducible form of the enzyme, NO synthase. This enzyme is up-regulated by inflammatory mediators such as cytokines like tumor necrosis factor alpha (TNF-α). Moreover, rapid and persistent activation of nuclear factor κB (NF- κB) in alveolar macrophages induce the expression of an inducible form of the enzyme NO synthase (iNOS) and the TNF-α receptor. The highly reactive O2-(superoxide anion) is released by stimulated leukocytes including monocytes, macrophages, and polymorphonuclear leukocytes by the action of NADPH oxidase.[18,19] There are many different methods to evaluate oxidative stress.[20] The indices based on the composition of various biological specimens are the most used. Most publications used at least two methods to assay oxidative stress, evaluation of promoters and peroxidation products induced by oxidative,[21] oxidized proteins,[22] and DNA oxidation.[23]
We review the different assays for evaluating oxidative stress induced in different organs by inhalation of thinner and its principal component, toluene.
EFFECTS ON ORGANS
Brain
Some studies about the oxidative stress showed induction of ROS caused by intraperitoneal toluene exposure (1 g/kg, 1 h) in crude, synaptosomal, and microsomal fractions of cortex.[24] In vivo exposure to various doses (0.5, 1.0, and 1.5 g/kg, ip) of toluene elicited elevated ROS in crude mitochondrial fractions obtained from rat lung and kidney and synaptosomal fractions from striatum and hippocampus. Hippocampus had the highest induced levels of ROS.[25] Prenatal exposure of rats to toluene (1800 ppm, 6 hr/day on days 7-20 of pregnancy) induces long–lasting changes in the oxidative status and membrane fractions of the fetal brains.[26]
Chronic inhalation of toluene produces oxidative stress in the brain. Increased activities of glutathione peroxidase and the free radical process were observed with a dose of 10 times the maximum permissible concentration (MPC, 500 mg/m3 of toluene) and showed free radical activation (421 ± 70) in comparison to the control value (261±36).[27] Free radicals were measured directly using a chemiluminescent probe that forms fluorescent products upon interaction with free radicals. Partial spectral analysis of the chemiluminescence showed a predominance of red-light-emitting species arising from the singlet oxygen dimol emission peaks; a side reaction derived from the complex free radical sequence of lipid peroxidation probably leads to light emission.[28]
More recently, the effect of chronic toluene exposure (15, 30, and 45 days) on oxidative stress was investigated. Increases in the levels of the thiobarbituric acid reactive substance (TBARS), glutathione reductase (GR), glutathione disulphide (GSSG), and superoxide dismutase (SOD) were observed in various organs of the rat. Furthermore, the cortex and cerebellum showed the greatest increase in an apoptotic marker (caspase 3), indicating that apoptosis may play a role in toluene neurotoxicity.[29]
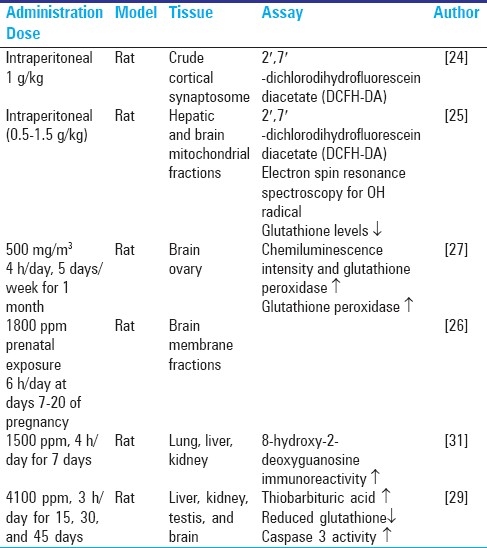
In the experimental studies performed on rats, levels of inhaled exposure are 3000 ppm toluene at various durations of exposure. This level of exposure in experimentation is comparable to the inhaled exposure which produces euphoria in humans[30] [Table 1].
Table 1.
Oxidative stress effects of toluene on different organs
There are not many studies about the effects on brain of thinner inhalation. One case with pathological and tomography analyses was reported by Escobar.[32] The patient was a 27-year-old male who had been addicted for 12 years to glue and thinner inhalation and had developed neurological and behavioral disturbances and finally died. Computed tomography showed cerebral and cerebellar atrophy and dilated lateral ventricles that were confirmed by pathological examination. There was a decrease in neuron density replaced by a diffuse gliosis, demyelination, and thinning of both the cortex and corpus callosum. Giant axonal degeneration was evident in long ascending and descending tracts in the spinal cord. Another pathological and magnetic resonance study describes cerebellar and cerebral demyelination as well as atrophy in humans as a result of toluene abuse.[33] Table 2 shows experimental studies of thinner inhalation on rats all these studies toluene concentrations are more than 3000 ppm, this level is comparable to the inhaled exposure which produces euphoria in humans [Table 2].
Table 2.
Oxidative stress effects of toluene on different organs
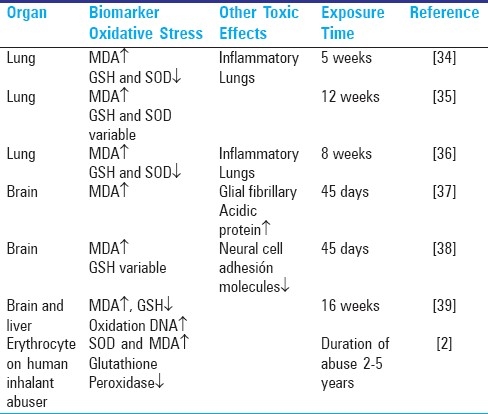
More recently, oxidative stress effects of thinner inhalation (45 days) have been demonstrated in brain. Neuronal damage induced by thinner inhalation generates glial reactivity in the hippocampus, cortex, and cerebellum. This reactivity is demonstrated by a marked elevation of glial fibrillary acidic protein (GFAP). Melatonin, a pineal hormone, is a free radical scavenger, and it prevents oxidative damage to lipids, proteins, and nucleic acids induced by thinner inhalation; it also prevents the increase of GFPA and decreases the oxidative effects induced by thinner inhalation.[37]
Chronic exposure to thinner inhalation (45 days) induced oxidative stress in brain; the lipid peroxidation level was increased, and the expression of neural cell adhesion molecules (NCAM) 140 and NCAM 180 in hippocampus and the cortex was reduced. The mechanism postulated was the interference with the synthesis of NCAM by thinner-induced oxidative stress. NCAM proteins are crucial for the stabilization of cell binding at synaptic sites. In addition, rats showed learning and memory deficits in the passive avoidance and Morris water maze tasks.[38]
Oxidative stress effects in the brain of rats exposed to chronic thinner inhalation (16 weeks) were an increase of MDA and a decrease of GSH. These effects correlate well with oxidative DNA damage in lymphocytes over the course of the treatment.[39]
Normal brain consumes a large quantity of oxygen, naturally forms oxidants for auto-oxidation of some neurotransmitters, and is relatively poor in antioxidant capacity, which makes it particularly vulnerable to oxidative damage[40] and might help to explain the neurotoxic effects of thinner. Nevertheless, additional knowledge is needed about the interaction of oxidative stress with other pathological mechanisms, such as apoptosis or necrosis.
Lung
Oxidative stress effects were observed on lung tissues of rats exposed for 5 weeks to thinner inhalation. MDA levels significantly increased between the second and the fifth weeks of thinner inhalation. A decrease in superoxide dismutase activity was observed from the third week until the end of the treatment. Glutathione levels increased in the first 2 weeks of exposure, and then decreased from the third until the fifth week of inhalation treatment. Chronic inflammatory changes, alveolar epithelial proliferation, collapse, emphysematous changes, and interstitial fibrosis were detected in the lung.[34]
In a long-term study, rats were exposed for 12 weeks to high concentrations of thinner. An increase in MDA values was observed, whereas GSH values decreased until 6 weeks and then increased again. SOD levels did not change significantly. Emphysema similar to chronic obstructive disease was observed in the lung.[35]
In a recent study, N-acetylcysteine (NAC), which is a precursor of GSH and can replenish the intracellular GSH stores, was found to act also as a scavenging agent by itself. When administered to rats concomitantly with thinner inhalation, NAC significantly lowered the tissue MDA levels throughout the 8-week treatment, as compared to the rats exposed to thinner only. In addition, tissue GSH levels of the rats given NAC while inhaling thinner were significantly higher than those of rats that inhaled thinner without NAC treatment. However, although the MDA and GSH levels indicated that oxidative stress caused by thinner inhalation was reduced by NAC, no beneficial effect on lung morphology was observed by light microscopy.[36]
Kidney
Epicutaneous administration of toluene in pigs caused progressing nuclear pyknosis and junctional separation between the basement membrane and the basal cells; it also induced spongiosis before the junctional separation.[41] Renal function was measured in workers exposed to a mixture of toluene and xylene. Renal function impairment indicators included total proteinuria, albuminuria, and urinary excretion of muramidase; the levels of these parameters suggested mild tubular lesions.[42]
Acute renal failure induced by toluene-containing adhesive was reported. Histopathological changes induced by thinner inhalation were tubular damage in the form of patches and severe tubulointersticial nephrits in kidneys.[43]
The effects of thinner inhalation and smoking on rat kidney were studied for 6 weeks, and evidence of interstitial cell infiltration and interstitial nephritis characterized by fibrosis was observed. In addition, focal necrosis in the epithelium of proximal tubules was seen in the kidney of rats that were exposed to thinner fumes and cigarette smoke.[44]
Blood
There have been a few studies about the oxidative DNA damage caused by toluene.[16] Studies have shown the oxidative effects of thinner inhalation on lipid peroxidation, levels of antioxidant enzymes; in addition, glutathione depletion was observed in the plasma of adolescents with inhalant abuse and people working with paint thinner.[2,45]
Thinner inhalation induced oxidative damage in the DNA of rat lymphocytes. This oxidative damage was correlated with the other, widely used biomarkers of oxidative stress, increased MDA and decreased GSH levels in brain and liver.[39] Inhalation of thinner induces oxidative stress in the plasma of rats. Nevertheless, thinner inhalation does not damage DNA by inducing single- or double-strand breaks; moreover, thinner does not alter DNA repair. This may indicate that oxidative stress, a well-documented effect of thinner inhalation, does not induce genotoxic effects.[46]
Toluene exposure increased oxidative stress parameters (MDA and protein carbonyl levels) in human erythrocytes after in vivo and in vitro exposure. Osmotic fragility in erythrocytes was altered only after in vitro exposure to toluene, and new synthesis of membrane components is important. The erythrocytes tested were from individuals exposed to toluene in the work place.[47]
DISCUSSION
The aim of this review has been to describe oxidative stress effects of thinner inhalation in animal models of solvent abuse. The current evidence suggests that oxidative stress is a common mechanism of many toxic substances. Many pathways play a key role in how thinner induces oxidative stress. We have discussed some of these pathways: metabolism of thinner components, enzymes (P450), metabolites (quinones), inflammatory reactions or indirectly via its solvent-like actions affecting lipid membranes. These pathways are not exclusive of one another indeed, all mechanisms contribute to the ability of thinner to induce oxidative stress. This mechanism plays a major role by which thinner induces brain damage. The evidence that thinner-induced oxidative stress plays a role in cell injury is showed in two studies. Administration of antioxidant can prevent or ameliorate the toxic action of thinner in the nervous system. In rats, learning and memory deficits induced by thinner inhalation are reversed by melatonin.[37] Melatonin administration significantly reduced lipid peroxidation and elevated glutathione levels in brain in this study. In contrast, N-acetylcystein (an oxygen radical scavenger) administration reduces the level oxidative stress effects on lungs. Nevertheless, pathological examinations did not show any beneficial effect of N-acetylcystein application. On the other hand, oxidative stress is related to apoptosis in only one study.[36]
Thinner consists of a large numbers of components in a complex mixture, widely used in home and industry. Real life always involves simultaneous exposures to multiple solvents, indicating the need for experimental work with combinations of substances. However, assessing the effects of chemical mixtures is a complex topic. In the case of studying thinner, problems like: the variability of its composition among the different types on the market and the complex toxicokinetics chemical interactions between thinner components. Future studies are required to further clarify thinner metabolic interactions.
ACKNOWLEDGEMENT
The authors thank Dr. Dorothy Pless for her language assistance.
Footnotes
Source of Support: PROMEP- SEP Project 103.5/10/7310
Conflict of Interest: None declared
REFERENCES
- 1.Basu D, Jhirwal OP, Singh J, Kumar S, Mattoo SK. Inhalant abuse by adolescents: a new challenge for Indian physicians. Indian J Med Sci. 2004;58:245–9. [PubMed] [Google Scholar]
- 2.Dundarz MR, Turkbay T, Akay C, Sarici SU, Aydin A, Denli M, et al. Antioxidant enzymes and lipid peroxidation in adolescents with inhalant abuse. Turk J Pediatr. 2003;45:43–5. [PubMed] [Google Scholar]
- 3.Patrick ME, Collins LM, Smith E, Caldwell L, Flisher A, Wegner L. A prospective longitudinal model of substance use onset among South African adolescents. Subst Use Misuse. 2009;44:647–62. doi: 10.1080/10826080902810244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reza J, Salazar G, Trejo A. Evaluation of composition and evaporation behavior of commercial thinner samples expended in mexico city. Rev Int Contam Ambient. 1997;13:87–95. [Google Scholar]
- 5.Saito J, Ikeda M. Solvent constituents in paint, glue and thinner for plastic miniature hobby. Tohoku J Exp Med. 1988;155:275–83. doi: 10.1620/tjem.155.275. [DOI] [PubMed] [Google Scholar]
- 6.IARC in “IARC Monographs on the Evaluation of Carcinogenic Risks to Humans”. Lyon, France: World Health Organization; 1982. pp. 93–148. [Google Scholar]
- 7.Yucel M, Takagi M, Walterfang M, Lubman DI. Toluene misuse and long-term harms: A systematic review of the neuropsychological and neuroimaging literature. Neurosci Biobehav Rev. 2008;32:910–26. doi: 10.1016/j.neubiorev.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Kyrklund T, Kjellstrand P, Haglid K. Brain lipid changes in rats exposed to xylene and toluene. Toxicology. 1987;45:123–33. doi: 10.1016/0300-483x(87)90098-9. [DOI] [PubMed] [Google Scholar]
- 9.Lebel CP, Schatz RA. Effect of toluene on rat synaptosomal phospholipid methylation and membrane fluidity. Biochem Pharmacol. 1989;38:4005–11. doi: 10.1016/0006-2952(89)90680-1. [DOI] [PubMed] [Google Scholar]
- 10.Lebel CP, Schatz RA. Altered synaptosomal phospholipid metabolism after toluene: Possible relationship with membrane fluidity, Na+, K(+)-adenosine triphosphatase and phospholipid methylation. J Pharmacol Exp Ther. 1990;253:1189–97. [PubMed] [Google Scholar]
- 11.Engelke M, Diehl H, Tahti H. Effects of toluene and n-hexane on rat synaptosomal membrane fluidity and integral enzyme activities. Pharmacol Toxicol. 1992;71:343–7. doi: 10.1111/j.1600-0773.1992.tb00559.x. [DOI] [PubMed] [Google Scholar]
- 12.Marsh D. Protein modulation of lipids, and vice-versa, in membranes. Biochim Biophys Acta. 2008;1778:1545–75. doi: 10.1016/j.bbamem.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Hayashi M. Oxidative stress in developmental brain disorders. Neuropathology. 2009;29:1–8. doi: 10.1111/j.1440-1789.2008.00888.x. [DOI] [PubMed] [Google Scholar]
- 14.Ellinger-Ziegelbauer H, Stuart B, Wahle B, Bomann W, Ahr HJ. Comparison of the expression profiles induced by genotoxic and nongenotoxic carcinogens in rat liver. Mutat Res. 2005;575:61–84. doi: 10.1016/j.mrfmmm.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Roberts RA, Laskin DL, Smith CV, Robertson FM, Allen EM, Doorn JA, et al. Nitrative and oxidative stress in toxicology and disease. Toxicol Sci. 2009;112:4–16. doi: 10.1093/toxsci/kfp179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murata M, Tsujikawa M, Kawanishi S. Oxidative DNA damage by minor metabolites of toluene may lead to carcinogenesis and reproductive dysfunction. Biochem Biophys Res Commun. 1999;261:478–83. doi: 10.1006/bbrc.1999.1041. [DOI] [PubMed] [Google Scholar]
- 17.Backes WL, Sequeira DJ, Cawley GF, Eyer CS. Relationship between hydrocarbon structure and induction of P450: Effects on protein levels and enzyme activities. Xenobiotica. 1993;23:1353–66. doi: 10.3109/00498259309059445. [DOI] [PubMed] [Google Scholar]
- 18.Fialkow L, Wang Y, Downey GP. Reactive oxygen and nitrogen species as signaling molecules regulating neutrophil function. Free Radic Biol Med. 2007;42:153–64. doi: 10.1016/j.freeradbiomed.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 19.Victor VM, De la Fuente M. Immune cells redox state from mice with endotoxin-induced oxidative stress. Involvement of NF-kappaB. Free Radic Res. 2003;37:19–27. doi: 10.1080/1071576021000038522. [DOI] [PubMed] [Google Scholar]
- 20.Dotan Y, Lichtenberg D, Pinchuk I. Lipid peroxidation cannot be used as a universal criterion of oxidative stress. Prog Lipid Res. 2004;43:200–27. doi: 10.1016/j.plipres.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Michel F, Bonnefont-Rousselot D, Mas E, Drai J, Therond P. [Biomarkers of lipid peroxidation: analytical aspects] Ann Biol Clin (Paris) 2008;66:605–20. doi: 10.1684/abc.2008.0283. [DOI] [PubMed] [Google Scholar]
- 22.Stadtman ER, Levine RL. Free radical-mediated oxidation of free amino acids and amino acid residues in proteins. Amino Acids. 2003;25:207–18. doi: 10.1007/s00726-003-0011-2. [DOI] [PubMed] [Google Scholar]
- 23.Cadet J, Douki T, Gasparutto D, Ravanat JL. Oxidative damage to DNA: Formation, measurement and biochemical features. Mutat Res. 2003;531:5–23. doi: 10.1016/j.mrfmmm.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Mattia C, LeBel C, Bondy S. Effects of toluene and its metabolites on cerebral reactive oxygen species generation. Biochem Pharmacol. 1991;42:879–82. doi: 10.1016/0006-2952(91)90048-a. [DOI] [PubMed] [Google Scholar]
- 25.Mattia CJ, Ali SF, Bondy SC. Toluene-induced oxidative stress in several brain regions and other organs. Mol Chem Neuropathol. 1993;18:313–28. doi: 10.1007/BF03160122. [DOI] [PubMed] [Google Scholar]
- 26.Edelfors S, Hass U, Hougaard KS. Changes in markers of oxidative stress and membrane properties in synaptosomes from rats exposed prenatally to toluene. Pharmacol Toxicol. 2002;90:26–31. doi: 10.1034/j.1600-0773.2002.900106.x. [DOI] [PubMed] [Google Scholar]
- 27.Burmistrov SO, Arutyunyan AV, Stepanov MG, Oparina TI, Prokopenko VM. Effect of chronic inhalation of toluene and dioxane on activity of free radical processes in rat ovaries and brain. Bull Exp Biol Med. 2001;132:832–6. doi: 10.1023/a:1013106315140. [DOI] [PubMed] [Google Scholar]
- 28.Boveris A, Cadenas E, Reiter R, Filipkowski M, Nakase Y, Chance B. Organ chemiluminescence: Noninvasive assay for oxidative radical reactions. Proc Natl Acad Sci U S A. 1980;77:347–51. doi: 10.1073/pnas.77.1.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.El-Nabi Kamel MA, Shehata M. Effect of toluene exposure on the antioxidant status and apoptotic pathway in organs of the rat. Br J Biomed Sci. 2008;65:75–9. doi: 10.1080/09674845.2008.11732801. [DOI] [PubMed] [Google Scholar]
- 30.Wilkins-Haug L. Teratogen update: Toluene. Teratology. 1997;55:145–51. doi: 10.1002/(SICI)1096-9926(199702)55:2<145::AID-TERA5>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 31.Tokunaga I, Gotohda T, Ishigami A, Kitamura O, Kubo S. Toluene inhalation induced 8-hydroxy-2’-deoxyguanosine formation as the peroxidative degeneration in rat organs. Leg Med (Tokyo) 2003;5:34–41. doi: 10.1016/s1344-6223(03)00004-x. [DOI] [PubMed] [Google Scholar]
- 32.Escobar A, Aruffo C. Chronic thinner intoxication: Clinico-pathologic report of a human case. J Neurol Neurosurg Psychiatry. 1980;43:986–94. doi: 10.1136/jnnp.43.11.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borne J, Riascos R, Cuellar H, Vargas D, Rojas R. Neuroimaging in drug and substance abuse part II: Opioids and solvents. Top Magn Reson Imaging. 2005;16:239–45. doi: 10.1097/01.rmr.0000192154.34563.6b. [DOI] [PubMed] [Google Scholar]
- 34.Ulakoglu EZ, Saygi A, Gumustas MK, Zor E, Oztek I, Kokoglu E. Alterations in superoxide dismutase activities, lipid peroxidation and glutathione levels in thinner inhaled rat lungs: Relationship between histopathological properties. Pharmacol Res. 1998;38:209–14. doi: 10.1006/phrs.1998.0354. [DOI] [PubMed] [Google Scholar]
- 35.Ilgazli A, Sengul C, Maral H, Ozden M, Ercin C. The effects of thinner inhalation on superoxide dismutase activities, malondialdehyde and glutathione levels in rat lungs. Clin Chim Acta. 2004;343:141–4. doi: 10.1016/j.cccn.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Dillioglugil MO, Ilgazli A, Maral H, Sengul C, Ozdemir G, Ercin C. Protective effects of N-acetylcysteine on the peroxidative changes of rat lungs exposed to inhalation of thinners. Respirology. 2005;10:615–9. doi: 10.1111/j.1440-1843.2005.00758.x. [DOI] [PubMed] [Google Scholar]
- 37.Baydas G, Reiter RJ, Nedzvetskii VS, Yasar A, Tuzcu M, Ozveren F, et al. Melatonin protects the central nervous system of rats against toluene-containing thinner intoxication by reducing reactive gliosis. Toxicol Lett. 2003;137:169–74. doi: 10.1016/s0378-4274(02)00400-9. [DOI] [PubMed] [Google Scholar]
- 38.Baydas G, Ozveren F, Tuzcu M, Yasar A. Effects of thinner exposure on the expression pattern of neural cell adhesion molecules, level of lipid peroxidation in the brain and cognitive function in rats. Eur J Pharmacol. 2005;512:181–7. doi: 10.1016/j.ejphar.2005.02.038. [DOI] [PubMed] [Google Scholar]
- 39.Martinez-Alfaro M, Palma-Tirado L, Sandoval-Zapata F, Carabez-Trejo A. Correlation between formamidopyrimidine DNA glycosylase (Fpg)-sensitive sites determined by a comet assay, increased MDA, and decreased glutathione during long exposure to thinner inhalation. Toxicol Lett. 2006;163:198–205. doi: 10.1016/j.toxlet.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 40.Warner DS, Sheng H, Batinic-Haberle I. Oxidants, antioxidants and the ischemic brain. J Exp Biol. 2004;207:3221–31. doi: 10.1242/jeb.01022. [DOI] [PubMed] [Google Scholar]
- 41.Kronevi T, Wahlberg J, Holmberg B. Histopathology of skin, liver, and kidney after epicutaneous administration of five industrial solvents to guinea pigs. Environ Res. 1979;19:56–69. doi: 10.1016/0013-9351(79)90034-3. [DOI] [PubMed] [Google Scholar]
- 42.Franchini I, Cavatorta A, Falzoi M, Lucertini S, Mutti A. Early indicators of renal damage in workers exposed to organic solvents. Int Arch Occup Environ Health. 1983;52:1–9. doi: 10.1007/BF00380601. [DOI] [PubMed] [Google Scholar]
- 43.Taverner D, Harrison DJ, Bell GM. Acute renal failure due to interstitial nephritis induced by ‘glue-sniffing’ with subsequent recovery. Scott Med J. 1988;33:246–7. doi: 10.1177/003693308803300208. [DOI] [PubMed] [Google Scholar]
- 44.Cobanoglu B, Ozercan IH, Ozercan MR, Yalcin O. The effect of inhaling thinner and/or cigarette smoke on rat kidneys. Inhal Toxicol. 2007;19:303–8. doi: 10.1080/08958370601141890. [DOI] [PubMed] [Google Scholar]
- 45.Halifeoglu I, Canatan H, Ustundag B, Ilhan N, Inanc F. Effect of thinner inhalation on lipid peroxidation and some antioxidant enzymes of people working with paint thinner. Cell Biochem Funct. 2000;18:263–7. doi: 10.1002/1099-0844(200012)18:4<263::AID-CBF882>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 46.Martinez-Alfaro M, Carabez-Trejo A, Gallegos-Corona MA, Pedraza-Aboytes G, Hernandez-Chan NG, Leo-Amador GE. Thinner inhalation effects on oxidative stress and DNA repair in a rat model of abuse. J Appl Toxicol. 2010;30:226–32. doi: 10.1002/jat.1488. [DOI] [PubMed] [Google Scholar]
- 47.Karabulut I, Balkanci ZD, Pehlivanoglu B, Erdem A, Fadillioglu E. Effect of toluene on erythrocyte membrane stability under in vivo and in vitro conditions with assessment of oxidant/antioxidant status. Toxicol Ind Health. 2009;25:545–50. doi: 10.1177/0748233709346758. [DOI] [PubMed] [Google Scholar]


