Abstract
Background:
Laparoscopy is one of the most common surgical procedures and is the procedure of choice for most of the elective abdominal surgeries performed preferably under endotracheal general anesthesia. Technical advances in the field of laparoscopy have helped to reduce surgical trauma and discomfort, reduce anesthetic requirement resulting in shortened hospital stay. Recently, regional anaesthetic techniques have been found beneficial, especially in patients at a high risk to receive general anesthesia. Herewith we present a case series of laparoscopic appendectomy in eight American Society of Anaesthesiologists (ASA) I and II patients performed under spinal-epidural anaesthesia.
Methods:
Eight ASA Grade I and II adult patients undergoing elective Laparoscopic appendectomy received Combined Spinal Epidural Anaesthesia. Spinal Anaesthesia was performed at L2-L3 interspace using 2 ml of 0.5% (10 mg) hyperbaric Bupivacaine mixed with 0.5ml (25 micrograms) of Fentanyl. Epidural catheter was inserted at T10-T11 interspace for inadequate spinal anaesthesia and postoperative pain relief. Perioperative events and operative difficulty were studied. Systemic drugs were administered if patients complained of shoulder pain, abdominal discomfort, nausea or hypotension.
Results:
Spinal anaesthesia was adequate for surgery with no operative difficulty in all the patients. Intraoperatively, two patients experienced right shoulder pain and received Fentanyl, one patient was given Midazolam for anxiety and two were given Ephedrine for hypotension. The postoperative period was uneventful.
Conclusion:
Spinal anaesthesia with Hyperbaric Bupivacaine and Fentanyl is adequate and safe for elective laparoscopic appendectomy in healthy patients but careful evaluation of the method is needed particularly in compromised cardio respiratory conditions.
Keywords: Epidural, hyperbaric bupivacaine, laparoscopy, regional, spinal
INTRODUCTION
The development of laparoscopic surgery has revolutionized surgical procedures and thus has influenced the practice and techniques of anesthesia. Laparoscopic surgeries are normally performed under endotracheal general anesthesia to prevent aspiration and respiratory embarrassment secondary to induction of pneumoperitoneum.
Recent evidence suggests that regional anesthesia has a significant role in the care of patients undergoing laparoscopy.[1] There are many published reports of laparoscopic cholecystectomy and inguinal hernia repair under segmental thoracic spinal anesthesia and epidural anesthesia.[2–5] Herewith we present a case series of laparoscopic appendectomy in 8 healthy patients performed under combined spinal–epidural anesthesia.
METHODS
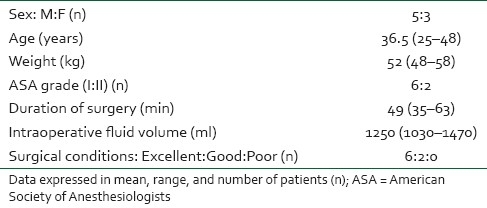
After the approval of Institutional Ethical Committee and written informed consent, 8 American Society of Anesthesiologists (ASA) Grade I and II patients underwent elective laparoscopic appendectomy under combined spinal epidural anesthesia [Table 1]. Exclusion criteria included those with the presence of any condition contraindicating elective surgery or spinal anesthesia.
Table 1.
Patient characteristics and outcome indicators
The patients were explained during the preoperative visit by the anesthesiologist that any anxiety, pain, or discomfort occurring during surgery would be dealt with intravenous medications or if they wished, conversion to general anesthesia. During and after the procedure, the patients were encouraged to report any discomfort, abdominal or shoulder pain, nausea and vomiting. All patients received oral alprazolam 0.5 mg and ranitidine 150 mg on the night prior to surgery. In the preoperative room an 18 g IV line secured and all patients received adequate preloading with 15 ml/kg of Ringer's lactate solution over 30 min and inj. ondansetron 4 mg intravenously. The patients were then shifted to the operation theater and all routine monitors namely, non invasive blood pressure, peripheral oxygen saturation by pulse oximetry (SpO2) and electrocardiogram were attached and after obtaining baseline vital signs, oxygen at 5 L/min was commenced through a face mask.
The patients were positioned in left lateral position, and under strict aseptic precautions the T10–T11 epidural space was accessed using an 18G Tuohy needle and loss-of-resistance technique and epidural catheter was threaded cephalad and fixed at 4 cm within the epidural space. Spinal anesthesia was then performed with 2 ml that is, 10 mg of 0.5% heavy bupivacaine with 25 μg of inj. fentanyl injected into L2–L3 subarachnoid space through a 27G pencil point spinal needle after free flow of cerebrospinal fluid. The patients were turned to the supine position and a 10 degree Trendelenburg tilt was given to achieve the required level of block.
Heart rate, blood pressure, and SpO2 were recorded every minute for 15 min and every 5 min thereafter. The level of sensory (pinprick) block was assessed and recorded every minute until the start of surgery and every 15 min thereafter. Once the block was considered adequate (minimum block T5—as assessed by pinprick), surgery was commenced using carbon dioxide (CO2) insufflation at a maximum pressure limit of 12 mmHg and a minimal tilt of the table.
Pain was treated with inj. fentanyl 50 μg, anxiety with inj. midazolam 2 mg and hypotension with inj. ephedrine 3 mg, all as IV boluses as and when required during the intraoperative period. The epidural injections were to be administered only if systemic analgesic drugs were ineffective in controlling pain. Surgeons were prepared to ask for general anesthesia if they felt that the anesthetic technique was adding to technical difficulty for the surgical procedure. An orogastric tube was inserted to decompress the stomach only if the surgeon demanded for it. They were also requested to rank technical difficulty associated with the procedure.
The surgical procedure of laparoscopic appendectomy was carried out according to standard protocol. Operative time as well as any intraoperative events was recorded.
RESULTS
The combined spinal epidural technique was successful in all the 8 patients at the first attempt. No patient experienced problems during injection of the anesthetic solution or insertion of the epidural catheter.
An effective sensory block till T5 (range T4–T6) developed within 10 min in all patients. Surgical conditions were excellent in 6 and good in 2 patients, took an average of 49 (SD 14) min and were completed 60 (SD 20) min after spinal injection. The cardiovascular changes were minimal, 2 patients requiring ephedrine, although a mean of 1250 (SD 220) ml of crystalloid was infused intraoperatively [Table 1].
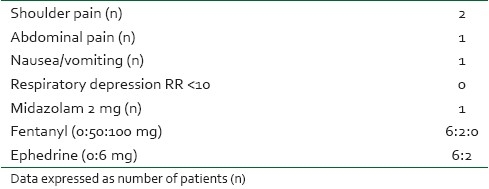
The first indication of regression of sensory block was observed 60 min after intrathecal injection with the median upper level decreasing by two segments at 75 min [Table 2]. Two patients described right shoulder pain, and one patient abdominal discomfort late in the procedure, all responding to moderate doses of fentanyl. One patient received midazolam 2 mg for anxiety. Epidural drug injection was not required in any of the patients. The procedure was successfully performed by laparoscopy under spinal anesthesia in all the patients. Nausea/vomiting or any signs of respiratory depression were not noticed, oxygen saturation being more than 95% throughout the intraoperative period [Table 3].
Table 2.
Anesthetic outcome
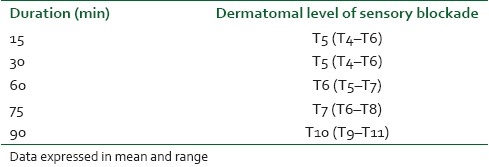
Table 3.
Perioperative side effects and medication
Postoperatively all patients received epidural infusion of 0.125% bupivacaine with fentanyl 2 μg/ml at the rate of 5–10 ml/hr for pain relief. One patient experienced mild nausea and some degree of shoulder pain persisted for up to 2 hours, which was mild and did not require any medication.
DISCUSSION
General anesthesia as the only suitable technique for laparoscopic procedures is a concept of the past as it does not facilitate adequate postoperative analgesia or an emesis-free recovery, two important problems associated with laparoscopic surgeries. The goal of anesthetic management in these patients includes management of pneumoperitoneum, achieving adequate level of sensory blockade, management of shoulder tip pain, provision of postoperative pain relief adequate to prevent deterioration of respiratory mechanics, and ambulation as early as possible. Spinal–epidural anesthesia fulfills all the above criteria and aids in the quick and uneventful postoperative recovery and thus has been suggested to be a suitable alternative anesthetic method for laparoscopic surgeries.[6]
This case series provides an indication regarding safety and adequacy of lumbar spinal anesthesia with hyperbaric bupivacaine with postoperative epidural analgesia in patients undergoing laparoscopic appendectomy.
The epidural technique was performed at the lower thoracic level, the T10–T11 interspace was chosen as it was at the center of the surgical field and was to be activated in case of unsuccessful spinal anesthesia or prolonged surgery and also for postoperative pain control. To avoid any accidental damage to the spinal cord, we performed spinal anesthesia at lumbar level (L2–L3) and the patient was kept in Trendelenburg position for a few minutes to achieve adequate extent of blockade required for the surgery.
Another major concern was the consequence of paralyzing the primary expiratory muscles, those of the anterior abdominal wall. However, our study included ASA Grade I and II patients without respiratory disease, and thus this effect would have little consequence; therefore, there were no concerns about respiratory status at any time. In particular, no patient experienced dyspnea during abdominal insufflation perhaps because of the use of minimal tilt of the operating table and the use of low intra-abdominal gas pressure (maintained at 10 mmHg).
Under regional anesthesia the respiratory mechanism remains intact, and diaphragm the main inspiratory muscle is unaffected allowing the patient to adjust minute ventilation without any significant changes in ventilatory parameters or CO2 levels.[7] In a study conducted by Ciofolo et al., the ventilatory measurements and arterial blood gases were maintained within normal limits at different stages during laparoscopy under epidural anesthesia.[8]
Cardiovascular changes were also minimal even though the spinal hyperbaric bupivacaine spread to affect most of the spinal cord segments responsible for sympathetic outflow. With adequate IV fluids, the patients who all were ASA grade I and II remained conscious, thus avoiding significant central depression of circulation or respiration and the differential blocking effects of bupivacaine may have prevented any significant cardiovascular changes.
Other side effects were both infrequent and easily managed, especially shoulder tip pain, a common problem after laparoscopic surgery which occurred in 2 of our patients. Avoidance of extreme degrees of head-down tilt, so that blood and other irritant fluids did not run onto the diaphragm may have been the reason for the low incidence of side effects in our patients. The continuous epidural analgesia started in the postoperative period also led to a smooth and uneventful recovery.
In conclusion, laparoscopic appendectomy was successfully performed under combined spinal epidural anesthesia without any significant complications and thus can be an effective anesthetic technique for laparoscopic surgeries, but careful evaluation of the technique is appropriate particularly in patients with compromised cardiorespiratory conditions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Collins LM, Vaghadia H. Regional anaesthesia for laparoscopy. Anesthesiol Clin North America. 2001;19:43–55. doi: 10.1016/s0889-8537(05)70210-8. [DOI] [PubMed] [Google Scholar]
- 2.van Zundert AA, Stultiens G, Jakimowicz JJ, Peek D, van der Ham WG, Korsten HH, et al. Laparoscopic cholecystectomy under segmental thoracic spinal anaesthesia: A feasibility study. Br J Anaesth. 2007;98:682–6. doi: 10.1093/bja/aem058. [DOI] [PubMed] [Google Scholar]
- 3.Gramatica L, Brasesco OE, Luna AM, Martinessi V, Panebianco G, Labaque F, et al. Laparoscopic cholecystectomy performed under regional anesthesia in patients with chronic obstructive pulmonary disease. Surg Endosc. 2002;16:472–5. doi: 10.1007/s00464-001-8148-0. [DOI] [PubMed] [Google Scholar]
- 4.Pursnani KG, Bazza Y, Calleja M, Mughal MM. Laparoscopic cholecystectomy under epidural anesthesia in patients with chronic respiratory disease. Surg Endosc. 1998;12:1426–8. doi: 10.1007/s004649900785. [DOI] [PubMed] [Google Scholar]
- 5.Chowbey PK, Sood J, Vashistha A, Sharma A, Khullar R, Soni V, et al. Extraperitoneal endoscopic groin hernia repair under epidural anesthesia. Surg Laparosc Endosc Percutan Tech. 2003;13:185–90. doi: 10.1097/00129689-200306000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, Hatzitheofilou C. Spinal vs general anesthesia for laparoscopic cholecystectomy. Arch Surg. 2008;143:497–501. doi: 10.1001/archsurg.143.5.497. [DOI] [PubMed] [Google Scholar]
- 7.van Zundert AA, Stultiens G, Jakimowicz JJ, van den Borne BE, van der Ham WG, Wildsmith JA. Segmental spinal anaesthesia for cholecystectomy in a patient with severe lung disease. Br J Anaesth. 2006;96:464–6. doi: 10.1093/bja/ael036. [DOI] [PubMed] [Google Scholar]
- 8.Ciofolo MJ, Clergue F, Seebacher J, Lefebvre G, Viars P. Ventilatory effects of laparoscopy under epidural anesthesia. Anesth Analg. 1990;70:357–61. doi: 10.1213/00000539-199004000-00003. [DOI] [PubMed] [Google Scholar]


