Abstract
Aims:
The aim of our study was to compare the effects of suprascapular nerve block in patients with frozen shoulder and diabetes mellitus unresponsive to intraarticular steroid injections.
Settings and Design:
Ten patients without improvement of sign and symptoms after intraarticular injections were made a suprascapular nerve block.
Methods:
Pain levels and active range of movement of patients were recorded at initial attendance and after 1, 4, and 12 weeks. All patients’ simple pain scores, total pain scores, and range of motion of their shoulders were improved significantly after suprascapular nerve block.
Statistical Analysis:
In this study, the statistical analyses were performed by using the SPSS 8.0 program (SPSS Software, SPSS Inc., USA). To compare pre- and post-injection results of simple pain score, total pain score, shoulder abduction and external rotation, Wilcoxon test was used.
Results:
Patient's simple pain scores, total pain scores also abduction, external rotation and internal rotation angles were improved significantly after suprascapular nerve block.
Conclusion:
Effective results after suprascapular nerve blockage was obtained for the treatment of refractory frozen shoulder cases.
Keywords: Frozen shoulder, nerve block, suprascapular nerve
INTRODUCTION
Frozen shoulder or adhesive capsulitis is a common problem in general practice presenting as pain that may be severe and as a progressive loss of movement resulting in a loss of function. Painful stiffness of the shoulder is an ill-defined clinical entity that is difficult to assess and delicate to treat.[1]
It is associated with synovitis and capsular contracture. It can be idiopathic or may be associated with another systemic disease. By far the most common cause of secondary frozen shoulder is diabetes mellitus. Unfortunately frozen shoulder in diabetes mellitus is often more severe and is more resistant to treatment.[2] Therapeutic options for the management of this problematic issue are limited and include simple analgesic, nonsteroidal anti-inflammatory drugs, intraarticular steroid injections, and manipulation under general anesthesia or arthroscopic capsular release.[3–8] All these modalities have their limitations particularly in patients with comorbidities and older age.
Bearing in mind that suprascapular nerve block is a safe method that its therapeutic effects can immediately be seen, the aim of our study was to compare the effects of it. Suprascapular nerve block in patients with frozen shoulder and diabetes mellitus unresponsive to intraarticular steroid injections.
METHODS
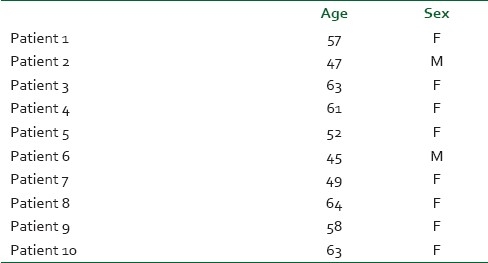
Ten patients with diabetes mellitus and frozen shoulder refractory to treatment with intraarticular corticosteroid injections were included in the study group [Table 1].
Table 1.
Age and gender of patients
All intraarticular steroid injections (a mixture of 40 mg methylprednisolone acetate and 4 mL 1% lidocaine) was made into glenohumeral joint using a 21 G × 50 mm needle via a posterior approach by the same doctor. The injections were repeated up to a total of 3 doses.
All these 10 patients had a painful stiff shoulder inability to use the affected arm for daily activities of life and pain at night causing sleep disturbances and inability to lie on the affected side. The patients have normal laboratory tests except blood glucose levels. Normal laboratory tests also included normal sedimentation rate, C-reactive protein, thyroid hormone, and rheumatoid factor levels.
Ten patients without improvement of sign and symptoms after intraarticular injections were made a suprascapular nerve block.
All suprascapular nerve blocks were done by the same two doctors under fluoroscopic guidance and nerve stimulator. A mixture of 40 mg methylprednisolone acetate and 5 mL 1% lidocaine was injected using 21 G × 50 mm needle. The point of injection was approximately 2 cm cephaloid to the midpoint of the spine of scapula. Following nerve blockage all patients were given verbal and written instructions about a home-based exercise program.
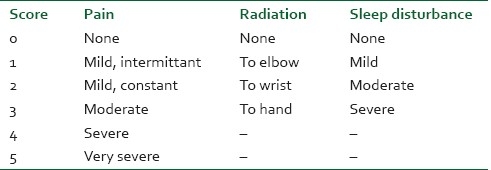
Pain levels and range of movement of patients were recorded active at initial attendance and after 1, 4, and 12 weeks postinjection. Patients graded their pain using the scale shown in Table 2.[9] The first column was simple pain score and the sum of the 3 columns was recorded as the total pain score.
Table 2.
Scale used to grade severity of pain
Active range of movements including abduction and external rotation at 0 degree abduction were measured using a goniometry, internal rotation were measured by the ability of the patient to reach his back with his hand (vertebral levels) by the same doctor.
Statistical analysis
In this study, the statistical analyses were performed by using the SPSS 8.0 program (SPSS Software, SPSS Inc., USA). To compare preinjection and postinjection results of simple pain score, total pain score, shoulder abduction, and external rotation, Wilcoxon test was used. A P value <0.05 was considered statistically significant.
RESULTS
All the patients’ simple pain scores, total pain scores, and range of motion of their shoulders before block, 1, 4, and 12 weeks after block are given in Tables 3 and 4.
Table 3.
Simple and total pain scores of the patients before block, at first week, fourth week and twelfth week
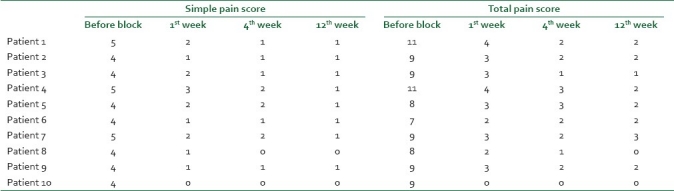
Table 4.
Range of shoulder motion of the patients before block, at first week, fourth week and twelfth week
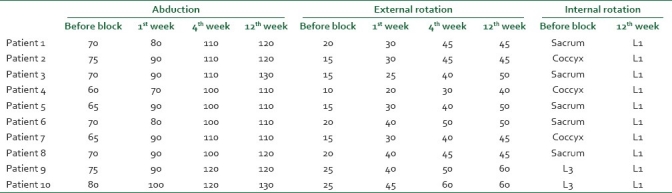
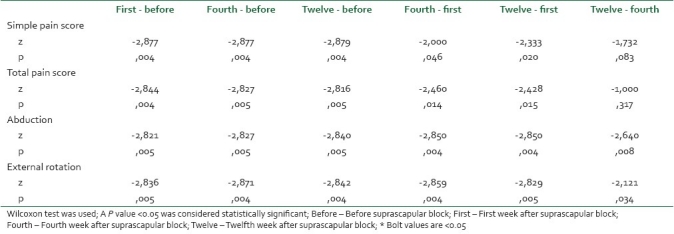
Patient's simple pain scores, total pain scores also abduction, external rotation, and internal rotation angles were improved significantly after suprascapular nerve block [Table 5].
Table 5.
To compare pre- and post-injection results of simple- and total-pain score, shoulder abduction and external rotation between the weeks
DISCUSSION
Frozen shoulder is a disabling condition that causes restriction and pain in the shoulder joint. The term frozen shoulder was first introduced by Codman in 1934. He described a painful shoulder condition of insidious onset that was associated with stiffness and difficulty of sleeping on the affected side.[3]
Diagnosis of frozen shoulder usually depends on clinical basis with a painful stiff shoulder for at least 4 weeks, inability to use the affected arm with restriction of movement and loss of full function, pain at night causing sleep disturbance and inability to lie on the affected side.
Frozen shoulder can be a primary or idiopathic or may be associated with many other systemic diseases, such as diabetes mellitus, hyperhypothyroidism, hypoadrenalism, Parkinson's disease, cardiac disease, pulmonary disease, and stroke.[10]
The incidence of frozen shoulder in diabetes patients is reported to be 10%–36% and this disease is often more severe and is more resistant to treatment in this subgroup of patients. Although there are many treatment modalities, such as nonsteroidal anti-inflammatory drugs, physical therapy, intraarticular steroid injections, manipulation under general anesthesia, and arthroscopic capsular release and some combination of these, the results reported and clinician's experience about these treatment options is inconsistent. Also refractory frozen shoulder cases pose a great challenge to doctors and to patient's quality of life.
The suprascapular nerve supplies sensory fibers to about 70% of the shoulder joint including the superior and posterosuperior regions of the shoulder joint and capsule and acromioclavicular joint.
In recent years suprascapular nerve blockage has been started to gain popularity in an effort to find more effective and simple treatment option for frozen shoulder and chronic shoulder pain.[11,12] Pathoanatomically, the common denominator is an inflammatory vascular proliferation followed by thickening, scarri[ng, and retraction of the joint capsule. Pain is playing an integral part of the frozen shoulder pathology and breaking that symbiotic relationship between pain and shoulder joint stiffness is mandatory to achieve a satisfactory result.
Our results display that suprascapular nerve blockage may effectively increase patient's pain tolerability which in turn more intense physical therapy can be tolerated by the patient. Although our study have limitations of having no control group and a small patient number, effective results after nerve blockage is increasing our hope for the treatment of refractory frozen shoulder cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tasto JP, Elias DW. Adhesive capsulitis. Sports Med Arthrosc. 2007;15:216–21. doi: 10.1097/JSA.0b013e3181595c22. [DOI] [PubMed] [Google Scholar]
- 2.Janda DH, Hawkins RJ. Shoulder manipulation in patients with adhesive capsulitis and diabetes mellitus: A clinical note. J Shoulder Elbow Surg. 1993;2:36–8. doi: 10.1016/S1058-2746(09)80135-3. [DOI] [PubMed] [Google Scholar]
- 3.Anton HA. Frozen shoulder. Can Fam Physician. 1993;39:1773–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Brue S, Valentin A, Forssblad M, Werner S, Mikkelsen C, Cerulli G. Idiopathic adhesive capsulitis of the shoulder: A review. Knee Surg Sports Traumatol Arthrosc. 2007;15:1048–54. doi: 10.1007/s00167-007-0291-2. [DOI] [PubMed] [Google Scholar]
- 5.Holloway GB, Schenk T, Williams GR, Ramsey ML, Iannotti JP. Arthroscopic capsular release for the treatment of refractory postoperative or post-fracture shoulder stiffness. J Bone Joint Surg Am. 2001;83-A:1682–7. doi: 10.2106/00004623-200111000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Kivimäki J, Pohjolainen T. Manipulation under anesthesia for frozen shoulder with and without steroid injection. Arch Phys Med Rehabil. 2001;82:1188–90. doi: 10.1053/apmr.2001.24169. [DOI] [PubMed] [Google Scholar]
- 7.Nicholson GP. Arthroscopic capsular release for stiff shoulders: Effect of etiology on outcomes. Arthroscopy. 2003;19:40–9. doi: 10.1053/jars.2003.50010. [DOI] [PubMed] [Google Scholar]
- 8.Pajareya K, Chadchavalpanichaya N, Painmanakit S, Kaidwan C, Puttaruksa P, Wongsaranuchit Y. Effectiveness of physical therapy for patients with adhesive capsulitis: A randomized controlled trial. J Med Assoc Thai. 2004;87:473–80. [PubMed] [Google Scholar]
- 9.Jones DS, Chattopadhyay C. Suprascapular nerve block for the treatment of frozen shoulder in primary care: A randomized trial. Br J Gen Pract. 1999;49:39–41. [PMC free article] [PubMed] [Google Scholar]
- 10.Sheridan MA, Hannafin JA. Upper extremity: Emphasis on frozen shoulder. Orthop Clin North Am. 2006;37:531–9. doi: 10.1016/j.ocl.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Karatas GK, Meray J. Suprascapular nerve block for pain relief in adhesive capsulitis: Comparison of 2 different techniques. Arch Phys Med Rehabil. 2002;83:593–7. doi: 10.1053/apmr.2002.32472. [DOI] [PubMed] [Google Scholar]
- 12.Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2003;62:400–6. doi: 10.1136/ard.62.5.400. [DOI] [PMC free article] [PubMed] [Google Scholar]


