Abstract
Background:
To compare oral midazolam (0.5 mg/kg) versus oral clonidine (4 μg/kg) as a premedication in pediatric patients aged between 2-12 years with regard to sedation and anxiolysis.
Methods:
Sixty pediatric patients belonging to the American Society of Anesthesiologists class I and II between the age group of 2-12 years scheduled for elective surgery were randomly allocated to receive either oral midazolam (group I) 30 min before induction or oral clonidine (group II) 90 min before induction of anesthesia. The children were evaluated for levels of sedation and anxiety at the time of separation from the parents, venepuncture, and at the time of mask application for induction of anesthesia.
Results:
After premedication, the percentage of children who were sedated and calm increased in both the groups. The overall level of sedation was better in the children in the clonidine group, but children in the midazolam group had a greater degree of anxiolysis at times of venepuncture and mask application. In addition, midazolam did not cause significant changes in hemodynamics unlike clonidine where a significant fall in blood pressure was noted, after premedication, but preinduction.
Conclusion:
We conclude that under the conditions of the study, oral midazolam is superior to clonidine as an anxiolytic in pediatric population. Clonidine with its sedative action especially at the time of separation from parents along with its other perioperative benefits cannot be discounted.
Keywords: Anxiolysis, oral clonidine, oral midazolam, pediatric anesthesia, premedication, sedation
INTRODUCTION
Anxiety and fear of operation, injections, physicians, operation theater environment, and parental separation are all traumatizing experiences in young children resulting in postoperative maladaptive behavioral changes.[1] Premedication should yield a patient who is calm, free of anxiety and pain, sedated, but easily arousable and fully co-operative. Oral premedication is widely used in pediatric anesthesia to reduce preoperative anxiety and ensure smooth induction.
The prospects of sedation and analgesia provided by one drug in single oral dose and excellent oral bioavailability of clonidine prompted us to study its efficacy as premedication in pediatric patients and compare it with oral midazolam, a gold standard premedication, in pediatric patients.[2] In this study, a comparison was made of their sedative and anxiolytic effects at the time of separation of children from their parents that was fixed at 30 and 90 min following oral midazolam and oral clonidine, respectively and subsequently at the time of child traumatizing interventions like venepuncture and mask application during induction of anesthesia.
METHODS
This was a prospective, randomized, observational study. After obtaining approval from hospital ethics committee and written informed consent from parents; 60 children aged 2–12 years of the American Society of Anesthesiologists (ASA) grade I and II, scheduled for elective surgery were enrolled in this study. The sample size chosen for the study was based on a pilot study of five cases done in the preliminary stage, following which 60 subjects were set after consultation with a statistician, which would enable a power of 80%. We excluded patients with central nervous system disorders, obesity (weight >95th percentile for age), gastrointestinal disorders that affect drug absorption, those on sedative medications, and those with previous reactions to clonidine or benzodiazepines. The children were randomly assigned to one of the two groups. Group I subjects received oral midazolam 0.5 mg/kg(maximum of 15 mg) along with oral atropine 0.04 mg/kg,30 min before induction. Group II received oral clonidine4 μg /kg (maximum of 200 μg) along with oral atropine 0.04 mg/kg, 90 min before induction. Since oral preparations of midazolam are not widely available, we used the injection form of midazolam mixed in honey to make it palatable. Oral clonidine was prepared by dissolving crushed tablets of clonidine 100 μg as per body weight. The medications were diluted to a fixed volume with honey to mask the bitter taste by the pharmacist to maintain the double-blinded nature of the study. The doses and the times of administration were based on published data from dose ranging studies.[2,3] The timing of wheeling the child away from the parents and subsequent venepuncture and mask application was strictly followed 30 min after oral midazolam and 90 min after oral clonidine. Children were evaluated for levels of sedation and anxiety at the time of separation from the parents, venepuncture, and at the time of mask application for induction of anesthesia. All the measurements of sedation and anxiety and the vital signs in this study were completed by the same investigator to minimize interobserver variability. The investigator graded sedation according to a 4 point sedation score (1=alert, 2=awake, 3=drowsy, 4=asleep), where a score of 3 and 4 was considered adequate sedation. Grading of anxiety was done by four point scoring, 1=poor (afraid and agitated and difficult to control, panicky), 2=fair (fearful, moderate apprehension, moaning), 3=good (slightly apprehensive, but withdrawn from the surroundings), 4=excellent (no fear, calm and sleepy, friendly), where a score of 3 and 4 was considered to be adequate anxiolysis.
General anesthesia was administered in a standardized manner and surgery proceeded. Vital signs were compared using the student ‘t’ test; the sedation and anxiolysis score were compared using the Mann–Whitney–Wilcoxon test and the chi-square analysis. A P value <.05 was considered statistically significant.
RESULTS
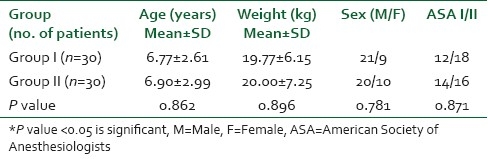
Patients in both the groups had comparable demographic characteristics (age, weight, gender, and ASA grade) [Table 1].
Table 1.
Distribution of subjects according to demographic profile
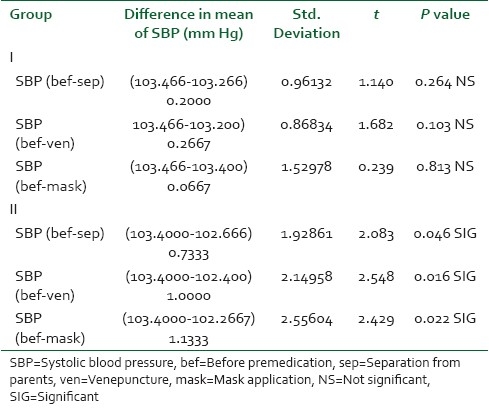
No patient developed hypotension, bradycardia or hypoxemia (oxygen saturation, 95%) from the time of administration of the premedication to the time of induction of anesthesia. However, the paired difference of the systolic blood pressures in the clonidine group was significantly decreased compared to the midazolam group [Table 2].
Table 2.
Comparison of systolic blood pressure recordings
After premedication, the percentage of children who were sedated and calm increased with time in both the groups. At the time of separation from parents, 80% of children belonging to the clonidine group were adequately sedated (sedation score 3 and 4) compared to 30% in the midazolam group, the overall difference in sedation between the two groups was found to be statistically very highly significant with a P value of <0.001 [Table 3]. However, the degree of sedation reduces on interventions, such as venepuncture and mask application, which goes along the lines of the unique feature of arousabilty on stimulation that is seen with clonidine[3] [Tables 4 and 5].
Table 3.
Comparison of sedation score at the time of separation from parents
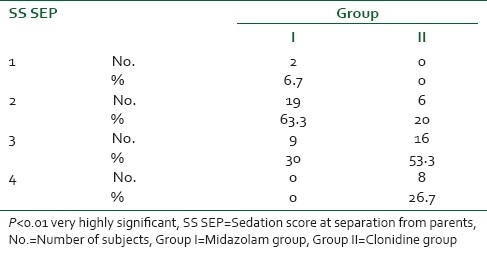
Table 4.
Comparison of sedation score at venepuncture
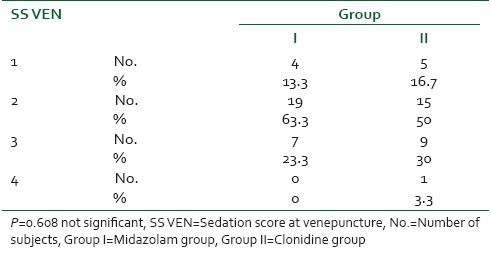
Table 5.
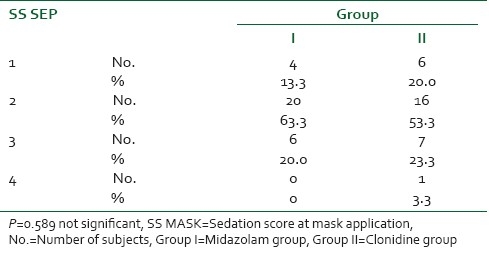
Comparison of sedation score at mask application
At the time of venepuncture, 33.3% of children belonging to the clonidine group were adequately sedated compared to 23.3% in the midazolam group. The difference in sedation between the two groups was found to be statistically significant with a P value of <0.05 [Table 4].
At the time of mask application, 26.6% of children belonging to the clonidine group were adequately sedated compared to 20.0% in the midazolam group. The difference in sedation between the two groups was found to be statistically significant with a P value of <0.05 [Table 5].
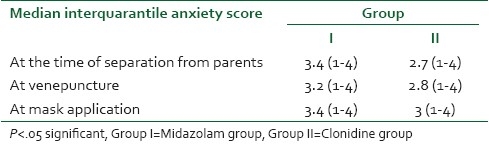
On comparison of anxiolysis score, children belonging to the midazolam group had adequate anxiolysis compared to the clonidine group as depicted by median interquarantile range which was found to be statistically significant with a P value of <0.05 [Table 6].
Table 6.
Comparison of anxiety scores
DISCUSSION
Sedation and anxiolysis are the essential components of anesthesia before surgery in pediatric patients. Currently, the most commonly used sedative premedicants in the preoperative holding area is midazolam (85%), followed by ketamine (4%), fentanyl (3%), and meperidine (2%) with oral route being used most commonly.[4] Clonidine, α2–adrenergic agonist is an upcoming preanesthetic agent in pediatric patients and hence has been compared with midazolam, the most common premedication used in children.
The results of our study suggest that oral midazolam (0.5 mg/kg) effectively reduce the anxiety associated with parental separation, venipuncture, and mask application, while oral clonidine (4 μg/kg) is a better sedative in the preoperative period. The doses of midazolam and clonidine used in this study have been established as optimum for preanesthetic sedation.[3,5]
Since oral preparations of midazolam are not widely available, we used the injection form of midazolam mixed in honey to make it palatable. Injection midazolam has been mixed with plain syrups, flavored syrups, apple juice, etc, to mask the bitter taste and make it more palatable for oral administration.[6] Limitation of the study was that potential alteration in the absorption of drugs based on pH changes induced by the diluent - honey in this case was not addressed in the study.
On studying the vital signs in our study group, it was observed that no child in the study developed significant bradycardia, hypotension, or hypoxemia. However, the paired difference of the systolic blood pressures in the clonidine group was significantly decreased compared to the midazolam group. These results are comparable to the results of Reimer et al.[7] and Malde et al.[8]
In our study, at the time of separation from parents, 30% in the midazolam group and 80% of the children were adequately sedated. The degree of sedation and anxiolysis in our study using 0.5 mg/kg midazolam are far greater than the results obtained by Feld et al.[7] This 10 fold greater success in effective separation from parents in our study may be attributed to the fixed time interval of separation of children from their parents (20 to 30 min) after premedication compared to wide time interval (30 to 80 min) limiting interpretation of the pharmacodynamic effects of oral midazolam.
The results of excellent anxiolysis after an oral dose of 0.5 mg/kg midazolam at the time of separation from parents are comparable to the results of McMillan et al.[9] and Debnath et al.[10] who also used a 0.5 mg/kg dose.
Tazeroulti et al.[11] found the quality of induction was less satisfactory after clonidine than after midazolam premedication in their study. The inadequate anxiolysis after clonidine in their study may be because of the short 30 min delay between premedication and induction. This, however, cannot explain the poor anxiolysis after clonidine in our study and the study done by Fazi[12] where induction of anesthesia was done 90 min after premedication. In contrast, Almenrader et al.[13] compared the clinical effects of oral midazolam and oral clonidine as a premedication. Oral clonidine appeared to be superior anxiolytic compared to oral midazolam. Quality of mask induction was equally successful in both groups. The contrasting results to ours obtained by Almenrader et al.[13] may be on account of a different study population.
Midazolam provided significantly superior anxiolysis at times of venepuncture and mask application. [Table 5] Overall, the results of our study show that the overall degree of sedation was greater in the children in the clonidine group, but children in the midazolam group had a greater degree of anxiolysis.
This superior picture of excellent anxiolysis with little change in hemodynamics conforms to the superiority of midazolam as a premedication in children. However, this was somewhat scarred by strange behavior of one of the children premedicated with midazolam. This child, who was calm, friendly, and playful, became violent and aggressive after premedication with midazolam. Such paradoxical reaction has been documented[14] to midazolam premedication before and the reason for which is not well understood, although it has been linked to genetic characteristics and personality problems. Paradoxical reactions to benzodiazepines include restlessness, violent behavior, physical assault, act of self-injury, and need for restraints.
In conclusion, this study failed in demonstrating clonidine as a better alternative to midazolam as an anxiolytic preoperatively. However, clonidine with excellent sedative properties and other perioperative benefits like decrease in anesthetic requirements, reduced need for supplementary analgesics postoperatively, reduced incidence of shivering and postoperative vomiting, and decreased incidence of sevoflurane emergence agitation cannot be discounted as a viable alternative to midazolam in pediatric patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kain ZN, Wang SM, Mayes LC, Caramico LA, Hofstadter MB. Distress during induction of anesthesia and postoperative behavioral outcomes. Anesth Analg. 1999;88:1042–7. doi: 10.1097/00000539-199905000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Levine MF, Spahr-Schopfer IA, Hartley E, Lerman J, MacPherson Oral midazolam premedication in children: The minimum time interval for separation from parents. Can J Anaesth. 1993;40:726–9. doi: 10.1007/BF03009769. [DOI] [PubMed] [Google Scholar]
- 3.Mikawa K, Maekawa N, Nishina K, Takao Y, Obara H. Efficacy of oral clonidine premedication in children. Anesthesiology. 1993;79:926–31. doi: 10.1097/00000542-199311000-00009. [DOI] [PubMed] [Google Scholar]
- 4.McCann ME, Kain ZN. The Management of Preoperative Anxiety in Children: An Update. Anesth Analg. 2001;93:98–105. doi: 10.1097/00000539-200107000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Feld LH, Negus JB, White PF. Oral midazolam preanesthetic medication in pediatric outpatients. Anesthesiology. 1990;73:831–4. doi: 10.1097/00000542-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Kain ZN, Mayes LC, Wang SM, Caramico LA, Hofstadter MB. Parental presence during induction of anaesthesia versus sedative premedication: Which intervention is more affective? Anaesthesiology. 1998;89:1147–56. doi: 10.1097/00000542-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Feld LH, Negus JB, White PF. Oral midazolam preanesthetic medication in pediatric outpatients. Anesthesiology. 1990;73:831–4. doi: 10.1097/00000542-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Malde AD, Pagedar RA, Jagtap SR. Oral clonidine in children: Efficacy as premedicant and postoperative analgesic as compared to diazepam. Indian J Anaesth. 2006;50:27–31. [Google Scholar]
- 9.McMillan CO, Spahr Schopfer IA, Sikich N, Hartley E, Lerman J. Premedication of children with oral midazolam. Can J Anaesth. 1992;32:545–50. doi: 10.1007/BF03008315. [DOI] [PubMed] [Google Scholar]
- 10.Debnath S, Pande Y. A comparative study of oral premedication in children with ketamine and midazolam. Indian J Anaesth. 2003;47:45–7. [Google Scholar]
- 11.Tazeroualti N, De Groote F, De Hert S, De Ville A, Dierick A, Van der Linden P. Oral clonidine vs.midazolam in prevention of sevoflurane-induced agitation in children. Br J Anaesth. 2007;98:667–71. doi: 10.1093/bja/aem071. [DOI] [PubMed] [Google Scholar]
- 12.Fazi L, Jantzen EC, Rose JB, Kurth CD, Watcha MF. A comparison of oral clonidine and oral midazolam as pre-anesthetic medications in the pediatric tonsillectomy patient. Anesth Analg. 2001;92:56–61. doi: 10.1097/00000539-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Almenrader N, Passariello M, Coccetti B, Haiberger R, Pietropaoli P. Premedication in children: A comparison of oral midazolam and oral clonidine. Paediatr Anaesth. 2007;17:1143–9. doi: 10.1111/j.1460-9592.2007.02332.x. [DOI] [PubMed] [Google Scholar]
- 14.Golparvar M, Saghaei M, Sajedi P, Razavi S. Paradoxical reaction following intravenous midazolam premedication in pediatric patients – A randomized placebo controlled trial of ketamine for rapid tranquilization. Paediatr Anaesth. 2004;14:924–30. doi: 10.1111/j.1460-9592.2004.01349.x. [DOI] [PubMed] [Google Scholar]


