Summary
We describe the case of a patient with an aneurysm of the P2 segment of the PCA with a persistent anastomosis between the posteromedial choroidal artery and the P3 segment of the posterior cerebral artery.
Key words: aneurysm, posterior cerebral artery, anastomosis
Introduction
Aneurysms of the posterior cerebral artery (PCA) are rare, representing approximately 1% of all intracranial aneurysms1-3. Contrary to aneurysms at other locations these aneurysms are more often related to a focal arterial dissection. We describe the imaging findings, anatomy and endovascular treatment of an unusual case of an aneurysm at the P2 segment of the PCA in which the PCA territory was supplied through a posteromedial choroidal artery-P3 segment anastomosis. This anastomosis can be elucidated from failure of regression of an embryological collateral pathway at the P3 level.
Case Report
A 60-year-old woman with acute headache was admitted to our tertiary care referral center. CT and CTA disclosed subarachnoid hemorrhage (Fisher grade 4) due to rupture of a right posterior cerebral artery aneurysm.
Diagnostic angiography, including three dimensional rotational angiography (3DRA), was performed under general anesthesia and systemic heparinization on a single-plane angiographic unit (Philips Integris Allura Neuro, Philips Medical Systems, Best, The Netherlands). Angiography confirmed the presence of an aneurysm of the P2 segment of the right posterior cerebral artery (PCA) with a proximal stenosis. In addition, a prominent posteromedial choroidal artery with a persistent and well-developed choroidal branch was identified with distal anastomosis at the P3 level with the main PCA (Figure 1). This anastomotic pathway allowed safe occlusion of the aneurysm and the proximal P2 segment of the PCA. Occlusion was performed with detachable coils (Guglielmi detachable coils; Boston Scientific, Fremont, CA, USA). After aneurysm and proximal P2 segment occlusion, excellent filling of the distal P2 segment of the right main PCA and thalamogeniculate arteries as well as P3 and P4 segments was preserved through the anastomosis (Figure 2). Heparinization was continued for 48 hours after treatment, followed by 80 mg aspirin daily for three months. The patient made a good clinical and neurological recovery and was discharged two weeks after the hemorrhagic event.
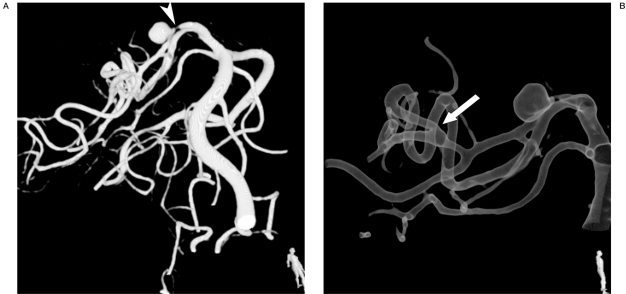
Figure 1.
Volume rendered (A) and gradient rendered (B) images obtained from 3DRA show dissecting aneurysm of P2 segment of the main trunk of right PCA. A P2 segment stenosis proximal to the aneurysm is present (A; arrowhead). A prominent posteromedial choroidal artery is identified with distal main PCA anastomosis at P3 level (B; arrow).
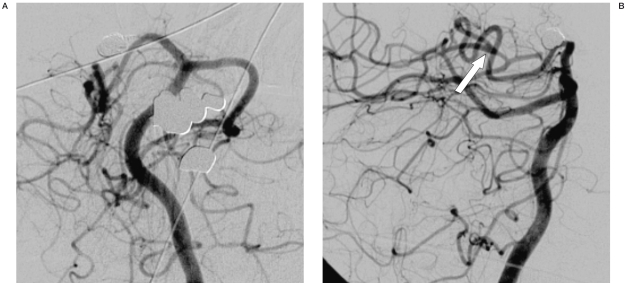
Figure 2.
2DSA shows complete occlusion of the aneurysm after coil placement and parent vessel occlusion (A). Excellent filling of the distal P2 segment of the right main PCA and thalamogeniculate arteries as well as distal PCA branches is preserved via a persistent posteromedial choroidal artery-main PCA anastomosis (B; arrow).
Seven-months follow-up MRI/MRA performed at 3T (Intera R10; Philips Medical Systems, Best, The Netherlands) showed persistent occlusion of the aneurysm on MRA and absence of any infarcts on high resolution T2-weighted images.
Discussion
Aneurysms at the P2 segment of the PCA account for less than 1% of all intracranial aneurysms. At this specific localization, a focal dissection is most often the underlying cause, due to mechanical compression or disruption of the vessel wall at the level of the tentorial edge. We describe an aneurysm in a stenosed segment at this specific P2 segment of the PCA in which a persistent anastomosis of the posteromedial choroidal artery and the P3 segment of the main PCA trunk is preserved. This unusual but favorable anatomy allowed safe occlusion of both the aneurysm and the parent artery, but more importantly, points to a long-lasting vessel narrowing probably already present in very early childhood.
To understand the anatomy of the PCA and the possible collateral pathways between the PCA and the posteromedial choroidal artery (and anterior choroidal artery), knowledge of the embryological development of the vascular precursors is essential. The thalamus and hypothalamus develop from the diencephalon, the basal medial part of the telencephalon forms the basal ganglia, whereas the cerebral hemispheres develop from the more lateral telencephalic diverticula. The arterial supply towards these primitive brain structures and the mesencephalon and choroid plexus is through several prominent embryonic vessels arising from a common stem at the caudal end of the posterior communicating artery. Telencephalic branches of the posteromedial choroidal artery and diencephalic artery anastomose at the level of the ambient cistern laterocaudal to lamina quadrigemina of the mesencephalon4. In the normal situation these anastomotic pathways regress during further development. In our patient a well-developed anastomosis persisted representing this anastomotic pathway. It could now be identified as a communication between the posterior cerebral artery and the posteromedial choroidal artery at the P3-P4 junction. Such an anastomosis has been described previously5, but the size of the anastomosis in this particular situation is remarkable and it is hypothesized that this collateral persisted and developed to such an extent because of long-lasting narrowing of the P2 segment. At a very early stage of the development of the PCA, a focal arterial stenosis must have been present, forming a focal weak point which later in life developed to an aneurysm that subsequently ruptured. Because of the well-developed collateral we do not propose this aneurysm as a true dissecting one, although this specific area at the tentorial edge is a site with a tendency for the development of dissecting aneurysms. The segment of the PCA at the free edge of the tentorium is the site where arachnoid trabeculae are present in the cisternal space in close contact with the PCA itself. These trabeculae are already present during embryological development. A causative relation with the development of dissecting aneurysms both in general as in this specific case is apparent6.
Left untreated, dissecting aneurysms of the posterior circulation have a very high mortality rate3. Occlusion of the aneurysm with the parent artery, although destructive in nature, is an effective treatment for these aneurysms1-3. Detailed knowledge of the intracranial connections facilitates the difficult decisions to be made in case of a dissecting aneurysm in which vessel occlusion is often the only treatment option. If no collateral supply is present the supply to the distal territory depends on distal leptomeningeal anastomosis, no test occlusion is possible under these circumstances. Definitive occlusive treatment is supported by the reports of Hallaq and Ciceri1,2. Hallaq et Al described ten patients, referred for endovascular treatment of P2 segment aneurysms. Endovascular parent artery occlusion at the aneurysmal neck was performed in nine cases without subsequent neurologic deficits 2. They concluded that acute parent artery occlusion in a P2 segment aneurysm is safe related to the potential for collateral supply and the hemodynamic balance between the anterior choroidal arteries and the posterior choroidal arteries, and the pericallosal and anterior and middle cerebral vessels to the PCA. They stated that the main reason for absence of any adverse events was that the aneurysm was located distal to the origin of the thalamoperforating vessels arising from the P1 segment. It should be noted, however, that perforating arteries also arise from the P2 segment, including the thalamogeniculate and peduncular perforating arteries7,8. Ciceri et Al found a relatively low incidence of visual field defect (1/7 or 14.2%) in patients in whom treatment of the PCA aneurysm required permanent artery occlusion related to the rich anastomotic collaterals that exist between the territory of the PCA and that of other arteries, including anterior choroidal arteries, superior cerebellar artery, posterior pericallosal artery and superior temporal branches of the middle cerebral artery3. They also state, however, that these anastomotic collaterals are not easily recognizable and often cannot be adequately evaluated prior to planned artery occlusion and therefore conclude that it is impossible to be certain whether or not parent vessel occlusion will be tolerated. In this specific patient the very rare collateral supply allowed safe obliteration of the aneurysm with occlusion of the parent P2 segment without neurologic sequelae.
References
- 1.Rooij WJ, Sluzewski M, Beute GN. Endovascular treatment of posterior cerebral artery aneurysms. Am J Neuroradiol. 2006;27:300–305. [PMC free article] [PubMed] [Google Scholar]
- 2.Hallaq P, Piotin M, Moret J. Endovascular occlusion of the posterior cerebral artery for the treatment of P2 segment aneurysms: retrospective review of a 10-year series. Am J Neuroradiol. 2002;23:1128–1136. [PMC free article] [PubMed] [Google Scholar]
- 3.Ciceri EF, Klucznik RP, et al. Aneurysms of the posterior cerebral artery: classification and endovascular treatment. Am J Neuroradiol. 2001;22:27–34. [PMC free article] [PubMed] [Google Scholar]
- 4.Lasjaunias P, Berenstein A, Terbrugge KG. Surgical Neuroangiography. 2nd ed. Vol 1. Berlin, Germany: Springer Verlag; 2001. Clinical vascular anatomy and variations; pp. 517–518. [Google Scholar]
- 5.Zeal AA, Rhoton AL., Jr Microsurgical anatomy of the posterior cerebral artery. J Neurosurg. 1978;48(4):534–559. doi: 10.3171/jns.1978.48.4.0534. [DOI] [PubMed] [Google Scholar]
- 6.Chong WKW, Lee SK, Terbrugge KG. 3T MRI-3D DSA fusion technique on posterior cerebral artery dissecting aneurysm: understanding a potential pathophysiologic mechanism. Interventional Neuroradiology. 2006;12:215–221. doi: 10.1177/159101990601200303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Milisavljevic MM, Marinkovic SV, et al. The thalamo-geniculate perforators of the posterior cerebral artery: the microsurgical anatomy. Neurosurgery. 1991;28:523–530. [PubMed] [Google Scholar]
- 8.Brassier G, Morandi X, et al. Origin of the perforating arteries of the interpeduncular fossa in relation to the termination of the basilar artery. Interventional Neuroradiology. 1998;4:109–120. doi: 10.1177/159101999800400202. [DOI] [PubMed] [Google Scholar]