Abstract
Although previous studies have found a protective association between attendance at religious services and depression, the extent to which this association is driven by depressed persons’ dropping out of religious activities is not clear. The authors examined whether early onset of a major depressive episode (MDE) predicted a subsequent decrease in religious service attendance. Data came from 3 follow-up studies of the National Collaborative Perinatal Project birth cohort (mean age = 37 years at last follow-up; n = 2,097; 1959–2001). The generalized estimating equations method was used to calculate the impact of an early MDE diagnosis (before age 18 years) on the likelihood of change in level of religious service attendance from childhood to adulthood. Twenty-seven percent of study participants met the criteria for lifetime MDE (n = 567), of whom 31% had their first onset prior to age 18 years. Women with early MDE onset were 1.42 times more likely (95% confidence interval: 1.19, 1.70) than women with adult-onset MDE or no lifetime MDE to stop attending religious services by the time of the first adult follow-up wave. No significant associations were observed among men. These findings suggest that women are more likely to stop attending religious services after onset of depression. Selection out of religious activities could be a significant contributor to previously observed inverse correlations between religious service attendance and psychopathology during adulthood.
Keywords: causality, depression, religion, sex
While there is considerable interest in the relation between religious activity and common mental disorders, research findings have been inconclusive because of methodological limitations (studies are typically cross-sectional) and the framing of hypotheses. Protective (1, 2), null (3), or inverse (4) correlations with major depressive episode (MDE) or depressive symptoms have been reported and often depend on the study design, the religiosity variable used (5), the age of the cohort studied, or the gender of the study participant. Weak study designs are prevalent. While many researchers and clinicians agree that spirituality and religiosity can be important in an individual patient’s mental health, the potential biologic, psychological, and social processes linking spirituality/religiosity to mental health might be deleterious or salubrious depending on the circumstances. Even so, given surveys showing that patients want their doctors to consider their religiosity and spirituality (6), clinicians have been urged to acknowledge the potential importance of spirituality in their patients’ lives (7) and at least take a spiritual history (8). However, more empirical evidence is needed to better understand the complex association between religious activity and psychopathology.
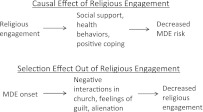
While religious activity may have a causal role in the development of depression, a key issue that plagues much of the research in this area is the question of selection, or reverse causation: People who start to become depressed may stop attending religious services, while others may become even more religiously active when they become depressed (see Figure 1). For example, disengagement from one’s usual social activities is one of the common symptoms of MDE, so it is conceivable that the onset of a depressive episode would precipitate a decline in religious service attendance. Indeed, higher levels of depressive symptoms have been correlated with reporting negative social interactions at church (9), which in turn are associated with church dissatisfaction and decreases in religious engagement (10). This would induce an inverse correlation between church attendance and depressive symptoms, making church attendance appear protective. On the other hand, the presence of emotional problems may also increase the use of religiosity as a coping strategy (11), which could translate into an increase in the frequency of religious activities. This would induce a positive correlation between religiosity and distress, a correlation that has been observed in studies of prayer and mental health (12), as well as studies linking emotional distress to increased likelihood of a future religious conversion (13). It has been well documented that religiosity often changes over the life course (14), with especially important changes occurring during the transition to adulthood (15). The extent to which either of the above-described scenarios plays out in the population could be a major driver of the observed religiosity-depression association.
Figure 1.
Causal and selection models of the relation between engagement in religious activity and first major depressive episode (MDE).
The majority of the studies finding beneficial prospective relations between religiosity and depression have used samples of adults in later middle adulthood or older adulthood (1, 16). Given that the median age of MDE onset is 32 years (with 25% of patients typically experiencing onset before age 19 years) (17), it is uncertain to what extent this reflects a genuine protective effect and to what extent it reflects a tendency for people with recurring episodes of depression to stop attending religious services earlier in life. Indeed, a recent review of psychiatric symptoms among adolescents revealed both protective and deleterious associations with religiosity (18), suggesting the presence of bidirectional relations in this age group (19). Even longitudinal studies limited to older adults are likely to be prone to selection effects, since one of the above-mentioned scenarios is likely to have already occurred. Therefore, a life-course perspective with data on religious activity and psychopathology spanning more than 1 stage of the life course is most optimal for understanding the complex association between religiosity and psychopathology.
In the present study, we addressed the issue of selection effects in the relation between religious activity and depression over time by analyzing religious service attendance from childhood to middle adulthood, together with information on the onset of MDE. In previous research with a subset of the current sample, current attendance at religious services was found to be correlated with lower lifetime odds of an MDE diagnosis (20). In the current analysis, patterns of religious service attendance were examined among persons with early (before age 18 years), later (age 18 years onwards), and no lifetime diagnosis of MDE. Specifically, we hypothesized that persons with early depression onset would be more likely to change their levels of religiosity as they transitioned to adulthood. Given that the majority of persons in this sample attended religious services as children (4), we expected the religious change to be in the direction of stopping religious service attendance. Furthermore, given known differences in depression and religiosity by gender (21, 22), all analyses were conducted separately for women and men.
MATERIALS AND METHODS
Sample
Participants in this study were from 3 follow-up studies based on random subsamples from a Providence, Rhode Island, birth cohort—one of the National Collaborative Perinatal Project cohorts (23). The birth cohort included 4,140 mother-infant pairs enrolled between 1959 and 1965. The sampling unit was the offspring, so approximately 25% of the mothers appeared in the data set more than once, given the enrollment of twins or siblings born to a family already enrolled in the study. The subsequent studies, based on independently drawn subsamples of children from the initial National Collaborative Perinatal Project, were each conducted via a combination of in-person structured interviews and mailed questionnaires. The first of these follow-up studies was conducted between 1987 and 1991 (mean age = 22.6 years; standard deviation (SD), 2.0), including 660 participants (24); the second occurred in 1996 (mean age = 33.6 years; SD, 1.8), with 718 participants (25); and the third was conducted in 2001 (mean age = 39.1 years; SD, 1.9), with 1,577 participants (26). The response rates exceeded 70% for all 3 studies, and there were no differences between follow-up studies in terms of race/ethnicity, gender, family history of psychiatric disorder, or family-of-origin socioeconomic status (SES). In general, women were more likely to participate in the follow-up studies than men. A total of 2,436 persons participated in at least 1 of these follow-up studies; 100 had missing values for family-of-origin SES, 4 did not provide information on race/ethnicity, 232 had no data on childhood religious service attendance, and 3 did not report adult attendance; this resulted in a final analyzed sample of 2,097 persons, representing 1,652 unique families. Furthermore, because subsamples were drawn independently for each follow-up study, random subsets of participants were included in more than 1 study. Thus, additional analyses were performed on the 488 persons with complete data who were effectively tracked longitudinally through participation in at least 2 of the 3 follow-up studies.
Measures
Assessment of participants’ lifetime experience of MDE, as well as age of first MDE onset, was performed in each wave of the study by trained interviewers using the Composite International Diagnostic Interview, based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM), Third Edition (in the first study) and the DSM, Fourth Edition (in the second and third studies). Given evidence that the small changes in criteria between the 2 versions of the DSM have not been associated with significant differences in disease estimates in community settings (27) or in the present data set (28), the current analysis combined data from both sets of diagnostic criteria. For the present study, age of onset was defined as childhood MDE when onset occurred before age 18 years and adult MDE when onset occurred at age 18 years or later. This will be referred to as “young” or “early” onset of MDE and “later” or “adult” onset of MDE, respectively. In cases where a participant reported different ages of MDE onset during different study interviews, the younger age was used.
Religious service attendance was determined by the question, “Do you go to a church or temple or other place of worship?” If the participant said yes, a second question inquired, “How often do you go to the church or temple or other place of worship, once in a while or regularly?” These questions were asked twice, once in reference to the present time and again in reference to “while you were growing up.” For the purpose of the analysis, respondents who reported going to a place of worship once in a while or regularly were treated as religiously active. Combining questions on religious activity during both the current adult interview and while growing up allowed for the creation of 4 distinct variables representing 3 different attendance patterns. Always attended refers to persons who reported being religiously active both while growing up and currently as adults; started after childhood refers to those who did not attend services while growing up but reported currently attending at the first adult wave; stopped after childhood refers to those who did attend services while growing up but were no longer attending at the first adult wave; and never attended refers to those who did not attend religious services while growing up and continued to not attend at the first adult wave. Because study participants were of varying ages during their first adult interview, the exact timing of changes in religious service attendance could not be determined, beyond knowing that such a change occurred at or after the transition to adulthood.
For the 488 persons who participated in more than 1 adult follow-up study, adult religious service attendance as reported at the first adult interview was used. In 12% of this sample, there was a discrepancy in a participant’s retrospectively reported childhood religious attendance between follow-up studies, and in these cases data from the earliest available wave of data collection (most proximal to childhood) were used. Information on frequency of current service attendance from multiple follow-up studies was used to create a variable representing a pattern of multiple changes in frequency of religious service attendance (such as stopped, started, then stopped again).
Covariates used in the analyses included gender (male/female), age at last follow-up, race/ethnicity (white/other), religious affiliation of the participant’s family of origin (Catholic vs. other), and SES of the family of origin. Family-of-origin SES was measured at entry into the birth cohort, using a 10-point scale adapted from the US Census Bureau based on household income and the education and occupation of the head of the household (29).
Analysis
The main analyses modeled changes in religious service attendance between childhood and adulthood as a function of the timing of MDE onset. First, A Cochran-Armitage test of trend or a t test was performed for demographic and religious service attendance variables in relation to the 3 MDE onset variables. Thus, the main independent variable in the analysis was the presence of an early MDE diagnosis (vs. a late diagnosis or no diagnosis as the reference category). A separate model was fitted for each of the 3 dependent variables of interest: 1) a model predicting stopping attendance at religious services (vs. continuing) was fitted among 1,900 participants who reported attending services during childhood; 2) a model predicting starting attendance at religious services (vs. continuing to not attend) was fitted among 204 participants who reported not attending services in childhood; and 3) a model predicting multiple changes in service attendance (vs. none or 1 change) was fitted in the entire subset of the sample with data from more than 1 follow-up study (n = 488). Specifically, the generalized estimating equations method (PROC GENMOD in SAS; SAS Institute, Inc., Cary, North Carolina) was used to estimate risk ratios and 95% confidence intervals associated with each pattern of religious service attendance, while adjusting for induced correlations resulting from the presence of siblings in the sample (30). Analyses were stratified by gender, and all models included adjustment for family-of-origin SES, race/ethnicity, and age at last follow-up. Given evidence that, for the majority of the sample, the independent variable (early-onset MDE) and potentially the outcome (change in service attendance) occurred before the completion of the participant’s education, educational attainment was not included as a covariate.
RESULTS
Consistent with the demographic characteristics of the area from which the sample was drawn, the majority of participants were white (84.0%) and had Catholic family backgrounds (66.2%). The mean age at the participants’ final point of data collection was 37.1 years (SD, 4.3). In total, 27.0% of participants had lifetime MDE, with 8.3% having onset before age 18 years and 18.7% having onset at 18 years or older. There was no statistically significant association between MDE onset and any of the demographic variables (Table 1).
Table 1.
Sociodemographic Characteristics and Patterns of Religious Service Attendance in the Combined Study Sample, by Gender and Age at Onset of First Major Depressive Episode, National Collaborative Perinatal Project, 1959–2001
| Gender and Age at Onset of First Major Depressive Episode |
||||||||||||
| Female |
Male |
|||||||||||
| <18 Years (n = 106) |
≥18 Years (n = 245) |
Never Depressed (n = 778) |
<18 Years (n = 68) |
≥18 Years (n = 148) |
Never Depressed (n = 752) |
|||||||
| No. or Mean (SD) | % | No. or Mean (SD) | % | No. or Mean (SD) | % | No. or Mean (SD) | % | No. or Mean (SD) | % | No. or Mean (SD) | % | |
| Mean family-of-origin SES scorea | 4.92 (2.1) | 5.18 (2.0) | 5.28 (2.0) | 4.59 (1.6) | 5.23 (2.1) | 5.12 (2.1) | ||||||
| White race/ethnicity vs. other | 88 | 83.0 | 220 | 89.8 | 647 | 83.2 | 58 | 85.3 | 126 | 85.1 | 621 | 82.6 |
| Catholic religious affiliation vs. other | 63 | 59.4 | 170 | 69.4 | 523 | 67.3 | 45 | 66.2 | 95 | 64.2 | 491 | 65.3 |
| Stability of religious service attendance between childhood and adulthood | ||||||||||||
| Always attended services | 36 | 34.0 | 114 | 46.5 | 421 | 54.1* | 32 | 47.1 | 63 | 42.6 | 321 | 42.7 |
| Started attending after childhood | 3 | 2.8 | 12 | 4.9 | 28 | 3.6 | 2 | 2.9 | 4 | 2.7 | 24 | 3.2 |
| Stopped attending after childhood | 59 | 55.7 | 108 | 44.1 | 290 | 37.3* | 27 | 39.7 | 66 | 44.6 | 356 | 47.3 |
| Never attended services | 8 | 7.6 | 11 | 4.5 | 39 | 5.0 | 7 | 10.3 | 15 | 10.1 | 51 | 6.8 |
| Changed attendance more than once vs. once or neverb | 10 | 25.6 | 13 | 17.8 | 27 | 18.4 | 4 | 19.1 | 6 | 13.6 | 34 | 20.7 |
Abbreviations: SD, standard deviation; SES, socioeconomic status.
* P < 0.01 (Cochran-Armitage trend test among females).
The SES of the participant’s family of origin was measured at entry into the birth cohort, using a 10-point scale adapted from the US Census Bureau based on household income and the education and occupation of the head of the household (29).
Out of a subset of 488 participants for whom data were available from multiple adult waves.
Most participants reported attending religious services in childhood (90.3%), a percentage that was equally distributed among men and women (89.4% and 91.1%, respectively), while 50.6% reported attending services at their first adulthood assessment (46.1% and 54.4% for men and women, respectively). In other words, as participants moved into adulthood, the majority either continued to attend religious services (“always” category: 50.6% women and 43.0% men) or stopped attending (40.5% women and 46.4% men). Relative stability of religious service attendance was observed among participants for whom data on multiple adult time points were available (n = 488). For example, of those who attended services both as children and in early adulthood, 78% (138 out of 176) continued to attend in middle adulthood. Of those who stopped attending services between childhood and the first adult wave, 66.9% (170 out of 254) remained nonattendees at the next follow-up.
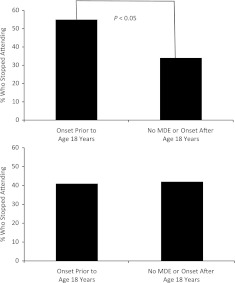
Patterns of change in religious service attendance over time differed across categories of MDE diagnosis (young, adult, or never) (Table 1). Fifty-six percent of women who became depressed before age 18 years stopped attending religious services as they transitioned into adulthood, as compared with 37.2% of those who had not become depressed during the study and 44.1% of those who became depressed at age 18 years or later. Thus, the most common religious trajectory for women with early onset was a decrease in religious service attendance, while for women with later onset or those with no diagnosis, the most common trajectory was that of always attending. In other words, early onset of depression predicted a decrease in religious activity between childhood and adulthood among women in comparison with women with no lifetime MDE or later-onset MDE. This pattern was not observed among men (see Figure 2). Although the sample size decreased significantly, women with early onset appeared to be somewhat more likely to have changed their religious attendance multiple times in adulthood (25.6% vs. 18.4% of those with no lifetime MDE). The patterns of religious service attendance among women with adult MDE onset were more similar to those of women with no lifetime MDE than to those of women with early onset.
Figure 2.
Likelihood of stopping attendance at religious services between childhood and the first adult follow-up according to onset of a major depressive episode (MDE) among females (top) and males (bottom) in the combined study sample, National Collaborative Perinatal Project, 1959–2001.
Multivariate regression results (Table 2) confirmed this finding: Women with early depression onset were 42% more likely to stop attending religious services than those without lifetime MDE or those with adult onset (risk ratio = 1.42, 95% confidence interval: 1.19, 1.70). Early MDE onset did not predict a future decrease in religious service attendance among men. Neither men nor women were more likely to start being religiously active after the onset of depression (Table 2), although this should be interpreted with caution because of the small cell sizes. The small difference in the percentage of women with early onset who changed their religious attendance multiple times in adulthood was not statistically significant in the fully adjusted regression model (Table 2).
Table 2.
Risk Ratio for Early Onset of a Major Depressive Episode in Models Predicting a Change in Religious Service Attendance Between Childhood and Adulthood, National Collaborative Perinatal Project, 1959–2001a
| Gender and Timing of MDE Onset | Model Predicting Stopping Attendanceb |
Model Predicting Starting Attendancec |
Model Predicting Multiple Changes in Attendanced |
|||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Female | ||||||
| No MDE onset/adult MDE onset | 1 | Referent | 1 | Referent | 1 | Referent |
| First MDE before age 18 years | 1.42 | 1.19, 1.70 | 0.50 | 0.18, 1.39 | 1.47 | 0.84, 2.57 |
| Male | ||||||
| No MDE onset/adult MDE onset | 1 | Referent | 1 | Referent | 1 | Referent |
| First MDE before age 18 years | 0.84 | 0.63, 1.12 | 0.76 | 0.21, 2.77 | 0.92 | 0.38, 2.33 |
Abbreviations: CI, confidence interval; MDE, major depressive episode; RR, risk ratio.
Generalized estimating equations models adjusting for socioeconomic status of the participant’s family of origin, race/ethnicity, and age at last follow-up.
Stopping attendance at religious services versus continuing attendance in adulthood, among females (n = 1,028) and males (n = 865) who attended services during childhood.
Starting attendance at religious services versus continuing to not attend services in adulthood, among females (n = 101) and males (n = 103) who did not attend services during childhood.
Multiple changes in service attendance (vs. 1 change or no changes in attendance) in a subset of 259 females and 229 males for whom data were available at multiple adult time points.
In additional sensitivity analyses, we examined whether incorporating information on changes in frequency of attendance (regular vs. irregular) altered the results (the above analyses referred to the complete cessation or starting of religious service attendance, which was the most common type of change). Recategorizing the “start” and “stop” categories to include any increase or decrease in frequency of attendance (including complete cessation) weakened the statistical significance of the results but did not alter the direction of association. Furthermore, persons who attended services regularly during childhood were no less likely to stop attending than those who attended irregularly (47% vs. 50%). Finally, the findings were robust across varying age cutoffs for early age of depression onset, the addition of controls for early childhood adversity, and models limited to individual follow-up studies (results available from the authors).
DISCUSSION
Our results showed that women with early onset of major depression (before age 18 years) were 1.42 times more likely to stop attending religious services after transitioning to adulthood than women with later onset or no lifetime MDE. This finding, combined with the relatively early onset of depressive disorders, suggests that selection out of religious activities could be a significant contributor to previously observed inverse correlations between religious participation and psychopathology during adulthood. There was little evidence of an increase in religious service attendance subsequent to the onset of depression, although this may have resulted from the fact that over 90% of participants reported attending religious services during childhood, resulting in very small numbers of attendance starters in adulthood. To our knowledge, this is one of the first studies to have shown an impact of selection effects in the association between religiosity and major depression (31). Prior work with data from a subset of the current sample revealed that current religious service attendance was correlated with lower lifetime odds of MDE (20). The findings from the current study suggest that at least part of that association is driven by women who stop being religiously active after they become depressed. The impact of religious activity itself, or a change in religious activity, on the course of depression remains unknown.
The topic of reverse causation or selection out of religious activity and its relation to health outcomes has most commonly been discussed in the context of high-risk behaviors. Specifically, there is evidence for selection out of religiosity with regard to outcomes such as delinquency or drug use (32). Researchers studying these outcomes report that religious adolescents who experiment with drugs are more likely to stop being religiously engaged, even as, overall, original participation in religious activities lowers the risk of drug initiation (33). At this stage of development, selection as well as reciprocal effects of religious engagement may be playing out simultaneously (19, 34). Additionally, there is evidence that persons who experience distress related to their religious community (resulting from negative social interactions or conflict with religious teachings, such as conflict that arises when adolescents become sexually active) are more likely to decrease their level of engagement with that community (35, 36) independently of their age. These studies support the hypothesis that specific behavioral and health-related events can precipitate a decrease in a person’s level of religious engagement. Furthermore, it is plausible that the perception of negative interactions in religious communities is precipitated in the context of depression and its frequently generated cognitive distortions. The degree to which the depressive symptoms originate independently of the religious community and simply influence the person’s perceptions of the community or are a result of negative experiences within the community which serve as “tipping points” in the onset of an MDE cannot be determined. Either pathway could contribute to the selection effect proposed to be present in the literature on religious activity and depression. Although in the current analysis we found evidence of selection associated with early onset of MDE, later MDE onset might similarly lead to changes in religious activity.
Our results suggest that women, but not men, are more likely to stop being religiously active after they become depressed. In other words, men’s decrease in religious activity is uncorrelated with depression, even as their overall likelihood of dropping out of religious services is slightly higher than women’s (40% of women stop attending services after childhood vs. 46% of men). Prior research has shown that women (37) and Catholics (38) are generally less likely than men and Protestants to stop being religiously active in early adulthood. It is possible that women are likely to stop being religiously engaged only in the context of a significant life change, of which depression onset would be an example. Although the small denomination-specific sample size precluded a full examination, our data do suggest that the link between early depression onset and the stopping-services pattern is somewhat stronger among Catholic women (vs. non-Catholic women).
Furthermore, other factors related to depression risk may also be related to a decrease in religious engagement. For example, an analysis of this same data set found that early-life exposure to residential instability and family disruption were significant determinants of early depression onset (39)—two factors that are also associated with a decrease in religious activity.
The present analysis had several noteworthy limitations. This analysis focused only on major depressive disorder, which was the most prevalent diagnosis in this sample. Therefore, the extent to which the presence of other psychiatric disorders induces similar patterns of religious service attendance could not be inferred. The study population comprised the Rhode Island cohort of the National Collaborative Perinatal Project and thus was not representative of a larger US population. The analysis was also limited by an imprecise reference to childhood for level of religious activity, which may be prone to recall bias. Among participants with data from multiple waves, 12% changed their recollection of childhood service attendance. However, the presence or direction of this change was not correlated with current religiosity levels or any number of demographic factors (40). Imputation of missing values for childhood attendance (yes/no) also did not yield meaningfully different results. Furthermore, it remains unknown whether use of the phrase “while growing up” elicited memories of young childhood or memories of adolescence. Since the level of religious activity at the time of MDE onset for persons with onset prior to age 18 years remained unknown, it was not possible to determine the original temporal (or causal) association between childhood religious activity and risk of early-onset MDE. This limitation also did not allow for testing hypotheses related to changes in religious service attendance predicting new onset of MDE. Finally, this analysis focused only on religious service attendance, and it is possible that other domains of religiosity might exhibit a different pattern of association with depression or depressive symptoms (5).
In conclusion, our findings raise a question about whether some of the “action” in the often-reported religion-depression association occurs much earlier in life than previously hypothesized. Future studies stretching from childhood throughout adulthood are needed to adequately address this question, avoiding some of the pitfalls of the typical cross-sectional examination of this relation. Although our findings do not rule out a causal role of religious activity in MDE onset earlier in the life course, the findings do raise substantive questions as to the causative models frequently proposed when assuming that religious involvement is the precursor to health, especially in older adults. Researchers must address, to the extent possible, the possibility of reverse causation when examining the relation between religious engagement and health outcomes.
Acknowledgments
Author affiliations: Department of Psychiatry and Behavioral Sciences, School of Medicine, Duke University, Durham, North Carolina (Joanna Maselko); Duke Global Health Institute, Duke University, Durham, North Carolina (Joanna Maselko); Department of Health Behavior and Health Education, School of Public Health, University of Michigan, Ann Arbor, Michigan (R. David Hayward); Department of Family and Community Health, School of Nursing, University of Pennsylvania, Philadelphia, Pennsylvania (Alexandra Hanlon); Department of Community Health, Division of Biology and Medicine, Brown University, Providence, Rhode Island (Stephen Buka); and Department of Psychiatry, School of Medicine, Vanderbilt University, Nashville, Tennessee (Keith Meador).
This work was supported by the National Institute of Mental Health (grant MH17119).
Conflict of interest: none declared.
Glossary
Abbreviations
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- MDE
major depressive episode
- SD
standard deviation
- SES
socioeconomic status
References
- 1.Norton MC, Singh A, Skoog I, et al. Church attendance and new episodes of major depression in a community study of older adults: the Cache County Study. J Gerontol B Psychol Sci Soc Sci. 2008;63(3):P129–P137. doi: 10.1093/geronb/63.3.p129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kendler KS, Liu XQ, Gardner CO, et al. Dimensions of religiosity and their relationship to lifetime psychiatric and substance use disorders. Am J Psychiatry. 2003;160(3):496–503. doi: 10.1176/appi.ajp.160.3.496. [DOI] [PubMed] [Google Scholar]
- 3.Dew RE, Daniel SS, Goldston DB, et al. A prospective study of religion/spirituality and depressive symptoms among adolescent psychiatric patients. J Affect Disord. 2010;120(1–3):149–157. doi: 10.1016/j.jad.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 4.Maselko J, Buka S. Religious activity and lifetime prevalence of psychiatric disorder. Soc Psychiatry Psychiatr Epidemiol. 2008;43(1):18–24. doi: 10.1007/s00127-007-0271-3. [DOI] [PubMed] [Google Scholar]
- 5.Koenig HG, George LK, Peterson BL. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry. 1998;155(4):536–542. doi: 10.1176/ajp.155.4.536. [DOI] [PubMed] [Google Scholar]
- 6.Ehman JW, Ott BB, Short TH, et al. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med. 1999;159(15):1803–1806. doi: 10.1001/archinte.159.15.1803. [DOI] [PubMed] [Google Scholar]
- 7.Blazer DG. Religion, spirituality, and mental health: what we know and why this is a tough topic to research. Can J Psychiatry. 2009;54(5):281–282. doi: 10.1177/070674370905400501. [DOI] [PubMed] [Google Scholar]
- 8.Borneman T, Ferrell B, Puchalski CM. Evaluation of the FICA Tool for Spiritual Assessment. J Pain Symptom Manage. 2010;40(2):163–173. doi: 10.1016/j.jpainsymman.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 9.Krause N, Ellison CG, Wulff KM. Church-based emotional support, negative interaction, and psychological well-being: findings from a national sample of Presbyterians. J Sci Study Relig. 1998;37(4):725–741. [Google Scholar]
- 10.Ingersoll-Dayton B, Krause N, Morgan D. Religious trajectories and transitions over the life course. Int J Aging Hum Dev. 2002;55(1):51–70. doi: 10.2190/297Q-MRMV-27TE-VLFK. [DOI] [PubMed] [Google Scholar]
- 11.Baetz M, Larson DB, Marcoux G, et al. Canadian psychiatric inpatient religious commitment: an association with mental health. Can J Psychiatry. 2002;47(2):159–166. doi: 10.1177/070674370204700206. [DOI] [PubMed] [Google Scholar]
- 12.Ellison CG. Race, religious involvement and depressive symptomatology in a southeastern U.S. community. Soc Sci Med. 1995;40(11):1561–1572. doi: 10.1016/0277-9536(94)00273-v. [DOI] [PubMed] [Google Scholar]
- 13.Kirkpatrick L. A longitudinal study of changes in religious belief and behavior as a function of individual differences in adult attachment style. J Sci Study Relig. 1997;36(2):207–217. [Google Scholar]
- 14.McCullough ME, Enders CK, Brion SL, et al. The varieties of religious development in adulthood: a longitudinal investigation of religion and rational choice. J Pers Soc Psychol. 2005;89(1):78–89. doi: 10.1037/0022-3514.89.1.78. [DOI] [PubMed] [Google Scholar]
- 15.Smith C, Snell P, Longest K. Religious trajectories from the teenage years. In: Smith C, Snell P, editors. Souls in Transition: The Religious and Spiritual Lives of Emerging Adults. New York, NY: Oxford University Press; 2009. pp. 211–256. [Google Scholar]
- 16.King DE, Cummings D, Whetstone L. Attendance at religious services and subsequent mental health in midlife women. Int J Psychiatry Med. 2005;35(3):287–297. doi: 10.2190/DEB0-B55Y-7EW6-8D7B. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 18.Dew RE, Daniel SS, Armstrong TD, et al. Religion/spirituality and adolescent psychiatric symptoms: a review. Child Psychiatry Hum Dev. 2008;39(4):381–398. doi: 10.1007/s10578-007-0093-2. [DOI] [PubMed] [Google Scholar]
- 19.Possel P, Martin NC, Garber J, et al. Bidirectional relations of religious orientation and depressive symptoms in adolescents: a short-term longitudinal study. Psycholog Relig Spiritual. 2011;3(1):24–38. [Google Scholar]
- 20.Maselko J, Gilman SE, Buka S. Religious service attendance and spiritual well-being are differentially associated with risk of major depression. Psychol Med. 2009;39(6):1009–1017. doi: 10.1017/S0033291708004418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hintikka J, Koskela K, Kontula O, et al. Gender differences in associations between religious attendance and mental health in Finland. J Nerv Ment Dis. 2000;188(11):772–726. doi: 10.1097/00005053-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 23.Niswander KR, Gordon MJ. The Women and Their Pregnancies: The Collaborative Perinatal Study of the National Institute of Neurological Diseases and Stroke. Washington, DC: US GPO; 1972. [Google Scholar]
- 24.Klebanoff MA, Zemel BS, Buka S, et al. Long-term follow-up of participants in the Collaborative Perinatal Project: tracking the next generation. Paediatr Perinat Epidemiol. 1998;12(3):334–346. doi: 10.1046/j.1365-3016.1998.00125.x. [DOI] [PubMed] [Google Scholar]
- 25.Buka SL, Satz P, Seidman L, et al. Defining learning disabilities: the role of longitudinal studies. Thalamus. 1998;16:14–29. [Google Scholar]
- 26.Kahler CW, Daughters SB, Leventhal AM, et al. Personality, psychiatric disorders, and smoking in middle-aged adults. Nicotine Tob Res. 2009;11(7):833–841. doi: 10.1093/ntr/ntp073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eaton WW, Anthony JC, Gallo J, et al. Natural history of Diagnostic Interview Schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry. 1997;54(11):993–999. doi: 10.1001/archpsyc.1997.01830230023003. [DOI] [PubMed] [Google Scholar]
- 28.Gilman SE, Kawachi I, Fitzmaurice GM, et al. Socioeconomic status in childhood and the lifetime risk of major depression. Int J Epidemiol. 2002;31(2):359–367. [PubMed] [Google Scholar]
- 29.Myrianthopoulos NC, French KS. An application of the U.S. Bureau of the Census socioeconomic index to a large, diversified patient population. Soc Sci Med. 1968;2(3):283–299. doi: 10.1016/0037-7856(68)90004-8. [DOI] [PubMed] [Google Scholar]
- 30.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 31.Horowitz JL, Garber J. Relation of intelligence and religiosity to depressive disorders in offspring of depressed and nondepressed mothers. J Am Acad Child Adolesc Psychiatry. 2003;42(5):578–586. doi: 10.1097/01.CHI.0000046831.09750.03. [DOI] [PubMed] [Google Scholar]
- 32.Uecker JE, Regnerus MD, Vaaler ML. Losing my religion: the social sources of religious decline in early adulthood. Soc Forces. 2007;85(4):1667–1692. [Google Scholar]
- 33.Benda BB, Corwyn RF. A test of a model with reciprocal effects between religiosity and various forms of delinquency using 2-stage least squares regression. J Soc Serv Res. 1997;22(3):27–52. [Google Scholar]
- 34.Regnerus MD, Smith C. Selection effects in studies of religious influence. Rev Relig Res. 2005;47(1):23–50. [Google Scholar]
- 35.Dudley R. Youth religious commitment over time: a longitudinal study of retention. Rev Relig Res. 1999;41(3):110–121. [Google Scholar]
- 36.Hoge D. Why Catholics drop out. In: Bromley D, editor. Falling From the Faith: Causes and Consequences of Religious Apostasy. Newbury Park, CA: Sage Publications; 1988. pp. 81–99. [Google Scholar]
- 37.Hayes B. Gender difference in religious mobility in Great Britain. Br J Sociol. 1996;47(4):643–656. [Google Scholar]
- 38.Brinkerhoff MB, Mackie MM. Casting off the bonds of organized religion—a religious-careers approach to the study of apostasy. Rev Relig Res. 1993;34(3):235–258. [Google Scholar]
- 39.Gilman SE, Kawachi I, Fitzmaurice GM, et al. Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychol Med. 2003;33(8):1341–1355. doi: 10.1017/s0033291703008377. [DOI] [PubMed] [Google Scholar]
- 40.Hayward R, Meador KG, Maselko J. Predictors of changing one’s recollection of religious identity over time. Int J Psychol Relig. 2012;22(1):79–88. doi: 10.1080/10508619.2012.635064. [DOI] [PMC free article] [PubMed] [Google Scholar]