Summary
The landmark at the opposite end of an occluded segment can be used for probing the occluded subclavian artery to be recanalized. Using this technique in three patients with symptomatic subclavian artery occlusion, we found the landmark-wire technique to be safe and effective for reopening completely occluded subclavian arteries. We also introduced a technique in which a protective device can be safely used throughout the stenting procedure.
Key words: subclavian artery, stenting, occlusion
Introduction
Percutaneous transluminal angioplasty and stenting have recently been regarded as an alternative treatment for symptomatic subclavian artery (SCA) stenosis including subclavian or coronary steal phenomenon1-3. However, traditional surgical treatment with subclavian-carotid bypass or transposition is frequently chosen for occluded SCA because of the difficulties encountered both passing through an occlusion and in stenting4. We present a safe and effective technique used while probing through the occluded segment of an SCA and leading to successful recanalization using a landmark at the opposite end of the occlusion.
Methods
Among 19 consecutive patients who underwent SCA and brachiocephalic artery stent insertion at our institute, there were three patients (two men, one woman; age range, 53-60 years) with symptomatic left SCA occlusion from May 2006 to June 2008 (Table 1). The risk factors in this patients included hypertension (n = 2), smoking (n = 2), and hyperlipidemia (n = 1). Symptoms included dizziness, arm weakness, coolness and absent or weak pulse and/or BP difference (> 20 mmHg) in both arms. Angiography showed both the steal phenomenon and prevertebral segment occlusion in two patients, although the left vertebral artery (VA) in patient 3 originated directly from the aortic arch (Figure 1).
Table 1.
Summary of patients.
|
Pt No. |
Age/ Sex |
Presenting symptoms |
Onset |
Device (diameter x length mm) |
F/U Study & Result |
Clinical F/U period |
Comments |
|
|---|---|---|---|---|---|---|---|---|
| Balloon pre/post | Stent | |||||||
| 1 | 53/M | Dizziness, arm weakness |
12 m | Ultra-soft SV 4x2 Ultra-soft SV 7x2 |
Precise 10x4 |
29 m CTA Good patency |
31 m | - |
| 2 | 60/M | Arm pain & tingling sense |
7 m | Maverick 2x1.5 Ultra-soft SV 5x2 Ultra-soft SV 7x2 |
Precise 9x4 |
12 m CTA Good patency |
20 m | Protective device was used |
| 3 | 58/F | Arm coolness & tingling sense |
10 m | Maverick 3x2 Ultra-soft SV 6x2 |
Precise 8 x4 |
10 m CTA Good patency |
10 m | VA arose directly from the aorta |
| Note.- CTA = CT angiography, VA = vertebral artery, Ultra-soft SV (BostonScientific Scimed Inc. | ||||||||
| MN, U.S.A.), Maverick (Boston Scientific Corp., Natick, Massachusetts), Precise (Cordis Corp, Miami,FL, USA). | ||||||||
| All the lesions were in the left subclavian artery. | ||||||||
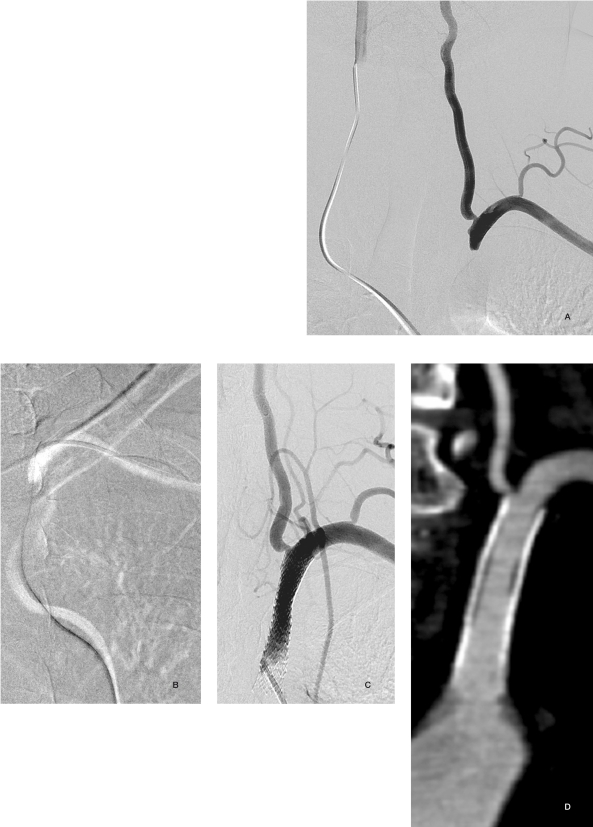
Figure 1.
A 60-year-old man presented with the left arm pain. Angiogram obtained by a catheter introduced via the femoral route revealed the proximal end of the occluded left subclavian artery (SCA) (A). Another catheter tip via the brachial route was placed at the distal end of the occlusion as a landmark. After passing a guidewire through the occluded segment, angioplasty was followed by stenting (B). The final angiogram revealed good patency of the recanalized SCA. After stenting, the patient's symptoms disappeared and he was without symptom recurrence during the 12-month follow-up (C). There was no restenosis detected on CT angiogram 13 months later (D).
Dual antiplatelet medication (100 mg aspirin and 75 mg clopidogrel) was administered at least three days prior to the procedure in all patients 5-8. All procedures were performed under local neuroleptic anesthesia. Technical success was defined as angiographic residual stenosis less than 20% and a gradient of less than 5 mmHg across the treated lesion. Patients were clinically evaluated 10 to 31 months following the procedure. Patency of the stented segment was demonstrated by means of DS or CTA. Clinical failure was defined as renewed clinical symptoms caused by recurrent obstruction of the SCA.
Landmark-wire technique
After careful evaluation of the color-coded duplex sonography, CTA, and/or MRA of the aortic arch vessels, we initially punctured both the femoral artery and the branchial artery. A 6-8F guiding catheter was placed into the ostium of the LSA, and a 4-6F catheter was inserted into the ipsilateral brachial artery. Systemic heparinization was given to make the activated coagulation time more than 250 seconds.
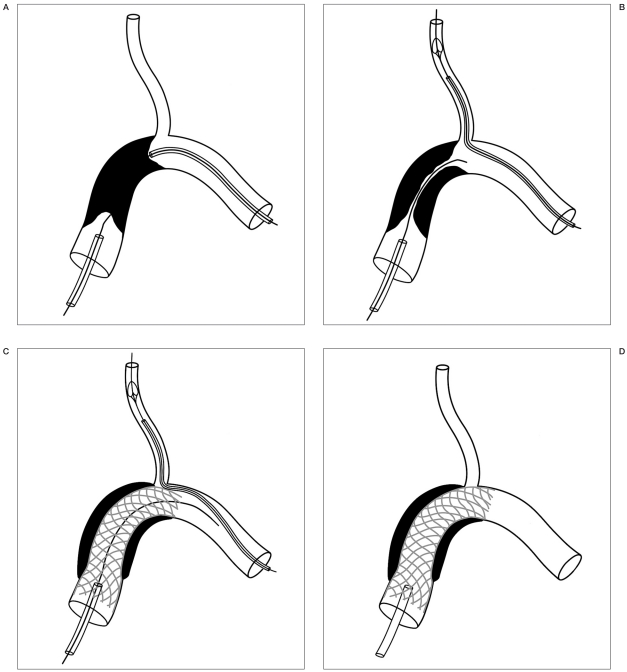
Bilateral selective angiograms or the roadmap were obtained to demonstrate both ends of the occluded LSA. A guidewire was inserted via the femoral guiding catheter into the occluded lesion. Under the landmark of the catheter and/or guidewire which were inserted via the brachial artery into the opposite end of the occluded segment, we probed and crossed through the occluded segment using a catheter via the femoral route. Once a stiff guidewire such as Conquest (Asahi Intecc Co, Ltd, Aichi, Japan), crossed through the occluded segment, we performed predilation using an angioplasty balloon, followed by stent placement and postdilation. A protection device was inserted into the VA via the brachial route in patient 2 (Figure 2). A 5-mm SpiderFX1 (eV3, Plymouth, MN) embolic protection device was placed in the left vertebral artery via the ipsilateral brachial artery to prevent thromembolic phenomenon into the VA (Figure 2). After the procedure, the patients received 100 mg of aspirin once daily as a permanent medication and 75 mg of clopidogrel once daily for at least six months following the procedure5,6,8.
Figure 2.
Procedure diagram of recanalization using the landmark-wire technique and a protective device in the vertebral artery via the brachial artery. We assumed that the stent covered the vertebral artery ostium because retrieval of the protection device would be difficult in a case of such jailing. The left subclavian artery occlusion (A) with patent vertebral artery lumen was probed using a stiff guidewire (B). Stenting was performed with a protective device in the vertebral artery. Note the retrieval catheter already positioned in the vertebral artery in order to smoothly remove the protective device (C, D).
Results
Technical success was achieved in all three patients. We uneventfully crossed the guidewire through the occlusive lesion using the landmark-wire technique via the femoral catheter in all patients. We then predilated stenosis with a balloon followed by stenting. The last angiogram showed regained antegrade flow without significant residual stenosis after stenting in all patients. There were no adverse events during the procedure and no symptom recurrence without restenosis during the 10 to 31 month follow-up period.
Discussion
Surgical treatment for SCA stenosis consisting of carotid-subclavian bypass or subclaviancarotid transposition has been replaced by percutaneous transarterial techniques9. Compared to the 90%-100% success rate of SA stenosis, as SCA occlusions have approximately a 70% treatment success rate because of the difficulty of passing a stent through an occluded segment, surgery is still recommended as the most appropriate treatment for a total SCA occlusion 10,11. However, the surgical complication rate can be as high as 21% with numerous neurologic events, lymphatic fistula, and even postoperative hemorrhage requiring repeat surgery in 3.3% of all patients12.
Although a both-ended approach to the occluded segment has been used to recanalize SCA occlusion13, to the best of our knowledge the landmark-wire technique has not been described in the literature as a method of recanalization for an occluded SCA. A catheter and/or guidewire used as a landmark at the opposite end of an occlusion, can guide the probing direction thus preventing unnecessary vessel injury or repeated contrast agent injection during coronary angioplasty for chronic total occlusion14. The transbrachial approach can be tried first because the catheter and the guidewire are unstable in the aortic arch especially in cases of osteal occlusion 4. However, in our series, we could pass the occluded lesion via the femoral route by using stable engagement of the guiding catheter and the rigid guidewires which were developed for the purpose of probing the occluded segment13. Even though we could cross the occluded segment via the femoral route in this study, the guidewire can also cross the lesion via the brachial route. The simultaneous availability of this double-ended approach is a definite advantage of the landmark-wire technique because probing at the opposite end of occlusion is only possible when the probing guidewire is against the resistance or has been passed in the wrong direction. However, it is noteworthy that probing through the atherosclerotic occlusion can carry a potential risk of subintimal dissection leading to penetration or even rupture of the vessel wall even though there is no immediate evidence of such a penetration injury.
We have achieved a good stent position with the self-expanding nitinol stents used in our patients because flexibility in this curved region is critical even though balloon-expandable stents have been recommended for accurate positioning and in order to reduce migration8,11,13,15. The reason we chose self-expandable stents is that they tend to have good opposition against the vessel wall which has a different luminal diameter due to tapering.
The at least 20-second delay of blood flow reversal after reopening an occlusion explains the rarity of an embolism occurring in the vertebral artery in patients with subclavian steal phenomenon16,17. However, as embolisms occurred in up to 4.3% of patients, it suggests that embolic protection systems may be required while performing SCA interventions1,2,18. Considering the anatomic difference between the carotid and vertebral arteries, the use of protective devices can be limited throughout the recanalization procedure 18. Therefore, we introduced a technique in which a protective device can be safely used throughout the stenting procedure, as described in Figure 2.
Conclusions
The landmark-wire technique using a bothended approach is safe and effective for use while probing an occluded segment of the SCA and leads to an improved recanalization success rate. The landmark-wire technique also allows a protective device to be safely used throughout the stenting procedure.
Acknowledgement
We acknowledge Sun Moon Whang, B.S. and Eun Hye Kim, R.N. in the patient data collection and the assistance of Eun Ja Yoon, Hyun Hee Koo, R.N. in manuscript preparation, and we thank Bonnie Hami, M.A for English editorial assistance. This study was supported by a grant (2003-143) from the Asan Institute for Life Sciences, Seoul, Korea.
References
- 1.Henry M, Henry I, et al. Percutaneous transluminal angioplasty of the subclavian arteries. Int Angiol. 2007;26:324–340. [PubMed] [Google Scholar]
- 2.Shah N, Nee LM, Raval AN. Percutaneous revascularization of subclavian artery chronic occlusion with dual cerebral artery protection. Catheter Cardiovasc Interv. 2008;71:992–994. doi: 10.1002/ccd.21520. [DOI] [PubMed] [Google Scholar]
- 3.Sixt S, Rastan A, et al. Results after balloon angioplasty or stenting of atherosclerotic subclavian artery obstruction. Catheter Cardiovasc Interv. 2009;73:395–403. doi: 10.1002/ccd.21836. [DOI] [PubMed] [Google Scholar]
- 4.Cinar B, Enc Y, et al. Carotid-subclavian bypass in occlusive disease of subclavian artery: More important today than before. Tohoku J Exp Med. 2004;204:53–62. doi: 10.1620/tjem.204.53. [DOI] [PubMed] [Google Scholar]
- 5.Taylor DW, Barnett HJ, et al. Low-dose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: A randomised controlled trial. Asa and carotid endarterectomy (ace) trial collaborators. Lancet. 1999;353:2179–2184. doi: 10.1016/s0140-6736(99)05388-x. [DOI] [PubMed] [Google Scholar]
- 6.Suh DC, Kim JK, et al. Intracranial stenting of severe symptomatic intracranial stenosis: Results of 100 consecutive patients. Am J Neuroradiol. 2008;29:781–785. doi: 10.3174/ajnr.A0922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suh DC, Kim JK, et al. Prognostic factors for neurologic outcome after endovascular revascularization of acute symptomatic occlusion of the internal carotid artery. Am J Neuroradiol. 2007;28:1167–1171. doi: 10.3174/ajnr.A0492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pyun HW, Suh DC, et al. Concomitant multiple revascularizations in supra-aortic arteries: Short-term results in 50 patients. Am J Neuroradiol. 2007;28:1895–1901. doi: 10.3174/ajnr.A0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schillinger M, Haumer M, et al. Outcome of conservative versus interventional treatment of subclavian artery stenosis. J Endovasc Ther. 2002;9:139–146. doi: 10.1177/152660280200900201. [DOI] [PubMed] [Google Scholar]
- 10.Domenig CM, Linni K, et al. Subclavian to carotid artery transposition: Medial versus lateral approach. Eur J Vasc Endovasc Surg. 2008;35:551–557. doi: 10.1016/j.ejvs.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Schillinger M, Haumer M, et al. Risk stratification for subclavian artery angioplasty: Is there an increased rate of restenosis after stent implantation? J Endovasc Ther. 2001;8:550–557. doi: 10.1177/152660280100800603. [DOI] [PubMed] [Google Scholar]
- 12.Linni K, Ugurluoglu A, et al. Endovascular management versus surgery for proximal subclavian artery lesions. Ann Vasc Surg. 2008;22:769–775. doi: 10.1016/j.avsg.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Sadato A, Satow T, et al. Endovascular recanalization of subclavian artery occlusions. Neurol Med Chir (Tokyo) 2004;44:447–453. doi: 10.2176/nmc.44.447. discussion 454-445. [DOI] [PubMed] [Google Scholar]
- 14.Saito S. Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc Interv. 2008;71:8–19. doi: 10.1002/ccd.21316. [DOI] [PubMed] [Google Scholar]
- 15.Zaytsev AY, Stoyda AY, et al. Endovascular treatment of supra-aortic extracranial stenoses in patients with vertebrobasilar insufficiency symptoms. Cardiovasc Intervent Radiol. 2006;29:731–738. doi: 10.1007/s00270-002-0085-3. [DOI] [PubMed] [Google Scholar]
- 16.Ringelstein EB, Zeumer H. Delayed reversal of vertebral artery blood flow following percutaneous transluminal angioplasty for subclavian steal syndrome. Neuroradiology. 1984;26:189–198. doi: 10.1007/BF00342413. [DOI] [PubMed] [Google Scholar]
- 17.De Vries JP, Jager LC, et al. Durability of percutaneous transluminal angioplasty for obstructive lesions of proximal subclavian artery: Long-term results. J Vasc Surg. 2005;41:19–23. doi: 10.1016/j.jvs.2004.09.030. [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez A, Gil-Peralta A, et al. Angioplasty and stenting for total symptomatic atherosclerotic occlusion of the subclavian or innominate arteries. Cerebrovasc Dis. 2002;13:107–113. doi: 10.1159/000047759. [DOI] [PubMed] [Google Scholar]