Summary
This technical report describes the successful use of the newly introduced Distal Access Catheter, initially designed to work with the Merci Retrieval System with the Penumbra aspiration system as the main aspiration catheter. Both devices, one a clot retriever and the other a thrombo-aspiration device, can be used and deployed via the same catheter saving time during acute stoke intervention. Moreover, the larger inner diameter of the distal access catheter may allow more effective clot aspiration.
Key words: stroke, distal access cather, DAC, outreach catheter, penumbra system, merci, acute stroke intervention, neurointervention
Introduction
Ongoing advances in endovascular revascularization therapy, namely the introduction of devices engineered specifically for neurovascular use, have opened a new era in treating stroke patients beyond the three hour window or more recently 4.5 hour window1.
One of the important aspects of revascularization therapy is the time to achieve vessel revascularization. A typical patient that has experienced a stroke loses 1.9 million neurons (14 billion synapses) a minute until the stroke is completed or the vessel is re-canalized2. A technically challenging part of the therapy is to choose between different devices available to treat acute ischemic stroke.
We describe a case of left M1 occlusion that we initially treated using the Merci clot retrieval system (Concentric Medical, Inc. Mountain View, CA, USA) with the Outreach™ Distal Access Cather (DAC) (Concentric Medical). Following partial clot retrieval, the same DAC was used as the Penumbra aspiration catheter. The advantages of this technique were:
1) superior trackability
2) more rapid and effective aspiration due to larger inner diameter
3) saving time and cost. The case illustrates the clinical feasibility of using the DAC as a clot aspiration catheter and its compatibility with the Penumbra separator.
Case Report
The patient was a 65-year-old right-handed Caucasian woman with a medical history of hypertension, dyslipidemia and left carotid endarterectomy (CEA) performed 12 days prior to her presentation.
She was transferred from an outside hospital where she had a left carotid stenting and immediate post-procedure period suffered from right-sided weakness and global aphasia with National Institute of Health Severity Stroke Scale (NIHSSS) of 16. Stat head Computed tomography (CT) showed no evidence of intracranial hemorrhage with an early sign of hypo-attenuation at the basal ganglia. Immediate brain magnetic resonance imaging (MRI) and head and neck angiography (MRA) was obtained and revealed deep basal ganglia infarct with sparing of the large cortical area and complete middle cerebral artery / M1 segment occlusion at its origin. Systemic thrombolytics were not administered due to recent femoral artery puncture and recent CEA.
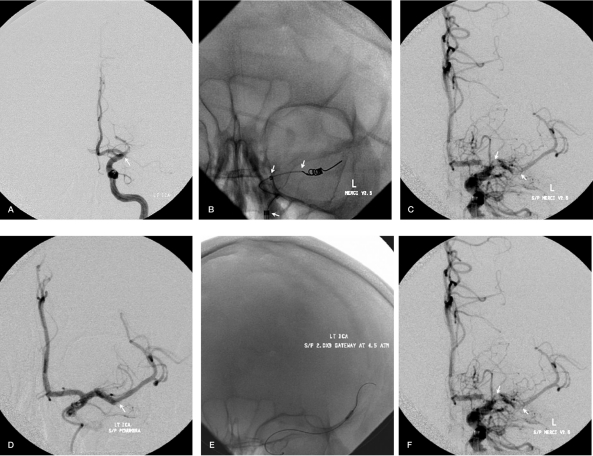
She was transferred via flight-for-life to our comprehensive stroke center for possible mechanical thrombectomy. Digital subtraction angiography (DSA) of the left carotid showed changes consistent with CEA and stenting of the left common carotid artery (CCA) with no sign of thrombosis. Complete occlusion of the left middle cerebral artery (MCA) at its origin from the left internal carotid artery (ICA) was documented (Figure 1 A,C).
Figure 1.
A-F) Mechanical thrombectomy in acute stroke pre and post-procedure DSA. Selective left-ICA images showing complete occlusion of left-MCA / M1 division at its origin (arrow) (A). Merci 2.5 V series deployed via the Microcatheter using triaxial system (Neuron Guide, DAC and the Microcatheter from proximal to distal, arrows) (B). Post Merci left ICA run showing improvement in the cerebral flow, with residual clot at the M1, A1 and Inferior MCA division (arrows) (C). The Penumbra device was then used via the DAC with significant improvement but persistent M2 inferior division clot (arrow) (D). Gateway balloon deployed in MCA inferior division to disrupt the clot (E), with final left ICA angiogram showing complete revascularization of the Left MCA artery (F); Abbreviations: DSA; digital subtraction angiography. ICA; internal carotid artery. MCA; middle cerebral artery. DAC; distal access catheter.
The patient underwent mechanical thrombectomy using Merci 2.5 firm V series Retriever; Penumbra System™ (Penumbra, Inc. Alameda, CA, USA), using the DAC, and Gateway angioplasty balloon ™ (Boston Scientific Inc. Fremont, CA, USA) with good re-canalization (Figure 1B,D).
Interventional Technique
The NeuronTM Guide catheter (Penumbra, Inc. Alameda, CA, USA) was placed distally at the carotid siphon to obtain maximum support for use of the mechanical stroke devices. Selective ICA arteriogram revealed complete occlusion of the MCA at its origin from the carotid terminus (TICI 0) with patent left A1 segment. The 0.18" microcatheter was loaded into the DAC 0.44" and the system was introduced into the Neuron guide catheter and advanced distal to the clot over the 0.14" microwire.
The Merci V 2.5 Firm clot retriever device was then deployed (Figure 1B) and retracted very slowly in attempt at capturing the clot with continuous suctioning and negative pressure applied via a 60 cc Syringe with no significant recanalization. Repeated Merci attempt was performed resulting in partial recanalization with residual clot at the origin of the left MCA and ACA as well as the inferior division MCA (Figure 1C).
Given the disruption of the clot and loss of its integrity, it was felt that aspiration of the remaining clots is the next step that would likely remove the fragmented clot pieces. The Penumbra device was advanced this time using DAC as primary reperfusion catheter connected to the Penumbra suctioning system removing the residual clot through aspiration and using the Penumbra Separator microwire for back and forth clot disruption. Good proximal recanalization was achieved after Penumbra system use with complete resolution of the M1 and A1 proximal clots (Figure 1D).
However, a distal clot in the proximal MCA inferior division was disrupted using 2 mm x 9 mm Gateway TM angioplasty balloon deployed via DAC (Figure 1E) that was inflated across the remaining proximal M2 thrombus with successful recanalization of distal parietal branches of the inferior division. Post procedure head CT scan showed no evidence of intracranial hemorrhage. Her discharge NIHSS was 6. At eight month clinical follow-up she was able to walk independently and take care of her daily activities with mild receptive aphasia with a modified Rankin Scale of 2.
Discussion
Some of the main obstacles to finding the optimal ischemic stroke therapy endovascular device include faster and safer deployment, distal support, trackability and accessibility especially into the clot, and efficacy in achieving fast and complete recanalization.
The Merci Retrieval System and Penumbra aspiration system use different mechanisms for mechanical thrombectomy: the Penumbra system aspirates clots3, whereas the Merci system pulls them out4.
The outreach DAC was designed to provide more agility and trackability to the whole Merci system to achieve a higher rate of clot retrieval. The principle is to provide distal support to the microcatheter and aligning the pulling force on the clot in line with the vessel towards the DAC therefore achieving safer and more effective clot retrieval.
While using DAC as a perfusion catheter the advantage was its large inner lumen and shorter length. Both these qualities increase the effective flow rate out of the catheter; according to Hagen Poiseuille equation F = ΔP π d4 / 128 μ L.Where: F is the flow rate, ΔP is the pressure change, L is the length of catheter, μ is the dynamic viscosity, d is the diameter, π is the mathematical constant.
We compared the DAC with the largest Penumbra reperfusion catheter to find the comparative flow rate ratio: DAC/ Penumbra = 1.5 times greater flow when compared to Penumbra which may be related to the lumen diameter and shorter length of the DAC.
The DAC is the largest catheter that can be easily tracked into the anterior intracranial vessel such as M1 or A1 segments. The NeuronTM guide catheter provides significant support during neuro-endovascular procedures 5, but it only tracks up to the distal ICA.
The ability to bring this DAC catheter into the intracranial circulation would provide several neuro-endovascular devices with the proximal support they need as well as potential use for aspiration with the Penumbra system and Separator as illustrated in this case.
Conclusions
The distal access catheter is safe and technically feasible when used with the Penumbra separator and suctioning system. This application may provide an effective alternative to the use of the Penumbra original reperfusion catheter saving time and cost. The decision to use the DAC as reperfusion catheter lies in the hands of the particular interventionalist and further studies are needed prior to its widescale use.
References
- 1.Hacke W, Kaste M, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL. Time Is Brain--Quantified. Stroke; Stroke. 2006;37(1):263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 3.Zaidat OO, et al. for Penumbra Stroke Pivotal Trial Investigators. The Penumbra Stroke Trial: Effects of Revascularization on Patient Outcomes. Neurology. 2008;70(11) Sup 1 [Google Scholar]
- 4.Smith WS, Sung G, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39(4):1205. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 5.Park MS, Stiefel MF, et al. Intracranial placement of a new compliant guide catheter: technical note. Neurosurgery. 2008;63(3):E616–617. doi: 10.1227/01.NEU.0000324918.46479.DD. [DOI] [PubMed] [Google Scholar]