Abstract
This ecological inquiry compares cancer mortality rates in the U.S. to the predictor of natural background radiation (via land elevation means) along with eight other predictors thought to be associated with cancer mortality. Age-adjusted cancer mortality in 2006 was compared to the predictors of mean land elevation, percent of smokers, educational attainment, percent of population without health insurance, income, obesity, health perception, physical activity, and diet. Among the six predictors considered appropriate for multiple linear regression, three were found to be statistically significant; from strongest to weakest, these three were: smoking, land elevation, and educational attainment. The predictors of smoking and educational attainment have long been considered associated with cancer mortality. The finding that the predictor of land elevation / natural background radiation is inversely related to cancer mortality is another piece of evidence supporting the theory of radiation hormesis. In this study, land elevation / natural background radiation ranked second in predictive strength regarding cancer mortality, behind smoking and ahead of educational attainment. Since this is an ecological inquiry, no causal inferences can be made.
Keywords: Radiation effects, background radiation, cancer, mortality
INTRODUCTION
Various well-known factors have been linked with cancer including radiation, smoking, diet, obesity, physical inactivity (NCI, 2009a); inadequate health insurance coverage (McDavid et al. 2003); educational attainment (Albano et al. 2007); and income (Boyd et al. 1999). Although not necessarily reported as a predictor of cancer mortality, health perception has been linked with total mortality (Wannamethee and Shaper, 1991).
There is controversy as to whether low level radiation (i.e., <5 rem) is hazardous. One viewpoint is that even the lowest amount of radiation is a health risk (Preston, 2008) while another viewpoint is that low level radiation is innocuous (Nair et al. 1999) and yet another view is that it may provide a health benefit through hormesis (Allright et al. 1983; Jagger, 1998; Luckey, 2006; Scott and Di Palma, 2006). The variable radiation can be indirectly studied by assessing land elevation, which is directly related to natural background radiation (NBR) (NRC, 2009). One mechanism advanced by Scott and Di Palma (2006) for explaining radiation hormesis is that low level radiation “stimulates the removal of precancerous neoplastically transformed and other genomically unstable cells form the body (medical radiation hormesis).” Prekeges (2003) notes that low level radiation stimulates protective mechanisms thereby leading to improved health.
In the interest of expanding on Jaegger’s research, where six states were studied, the purpose of the present study is to explore the relationship between cancer mortality and the aforementioned predictor variables, with particular focus on land elevation-related NBR, for all 50 states and the District of Columbia.
METHODS
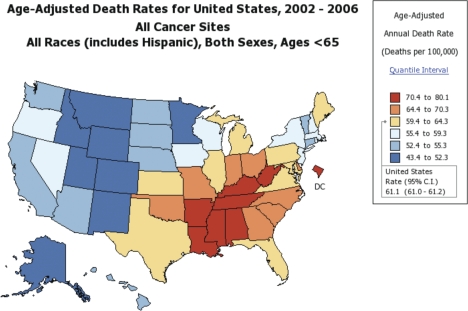
The response variable was average age-adjusted cancer mortality rates, measured by deaths per 100,000 people, for 2002–2006, all sites cancer, both genders, all races including Hispanic, below age 65 for the 51 jurisdictions in the U.S. (50 states and Washington, D.C.) (NCI, 2009b; Figure 1). The age category of <65 years old was used to assess mortality rate below the age of: a) life expectancy, which in 2004 was 77.8 (75.2 for males and 80.4 for females) (United States Life Tables, 2007) and b) the median age at the time of death for all-sites cancer which was age 73 during 2002–2006 (NCI, 2009c).
FIGURE 1.
Cancer map of U.S. for 2006. From The National Cancer Institute, cited 12-31-09 at: http://statecancerprofiles.cancer.gov/
The following nine predictor variables were included in the study: 1) Mean elevation by state measured in feet (referred to now as “elevation”) (U.S. Census Bureau, 2009a); 2) percent of population who smoke in 2003 and reported having smoked 100 or more cigarettes in their lifetime and who currently smoke everyday or some days (referred to now as “smoking”) (U.S. Census Bureau, 2009b); 3) percent of persons 25 and older in 2003 achieving high school diploma or higher (referred to now as “high school+”) (U.S. Census Bureau, 2009c); 4) percent of population ages 18–64 without any type of health insurance coverage in 2003 (referred to now as “no insurance”) (CDC, 2009a); 5) personal per capita income in 2003 (referred to now as “income”) (U.S. Census Bureau, 2009d); 6) obesity (BMI 30.0 – 99.8) in 2003 (referred to now as “obesity”) (CDC, 2009b); 7) “excellent” health perception in 2003 (with the question “how is your general health?”) (referred to now as “health perception”) (CDC, 2009c); 8) physical activity in 2003 (“adults with 20+ minutes of rigorous physical activity three or more days per week”) (referred to now as “physical activity”) (CDC, 2009d) and 9) diet in 2003 (“adults who have consumed fruits and vegetables five or more times per day”) (referred to now as “diet”) (CDC, 2009e). Predictor variables are primarily for 2003 to have an approximate three year period where the predictors were in force. The variable income for the year 2003 was not readily available so the income for the year 2004 was used. Maps for general land elevation and cancer mortality rates in the U.S. are provided in Figures 1 and 2.
FIGURE 2.
From USGS. Cited 12-16-09 at: http://ned.usgs.gov/images/nedus2.gif
Data analysis
Analysis consisted of Pearson correlation and multiple linear regression (MLR). Assumptions for the data were assessed as follows: a) Variables were considered to not exhibit distributions significantly different from normal if their skew values fell within −1.96 and +1.96 (Pett, 1997); b) two variables (cancer and predictor) were considered to exhibit a linear relationship if they had at least a moderate Pearson correlation coefficient (r ∼ 0.400) that was statistically significant (<0.05); c) the variance of the residuals was considered homogeneous if White’s test was >0.05 (UCLA, 2009). In addition, the variables were assumed to represent the general population since they were derived from the 51 U.S. jurisdictions. In multiple linear regression (MLR), collinearity was considered present among predictor variables if the variance inflation factor (VIF) was >4.0 (Garson, 2009). These assumptions are considered necessary for regression analysis (Munro, 2001). Predictors that exhibited VIF >4.0 were removed in subsequent MLR modeling, one-at-a-time per model, beginning with the highest VIF value, until satisfactory VIF (<4) was achieved. Then predictors having the highest p-values were removed, one-at-a-time, beginning with the highest, until each predictor exhibited a statistically significant p-value (<0.05). Predictor variables were compared for relative predictive strength for the response variable (cancer mortality) by way of assessing their: a) standardized estimates and b) p-values (two-tailed). Correlations, MLR, White’s test, Skewness, and VIF were performed in SAS 9.2 (Cary, NC). All skew values exhibited values between −1.96 and +1.96.
RESULTS
Correlation and MLR
Moderate strength, statistically significant correlations were observed in correlations of cancer with: 1) elevation (r = −0.656, p <0.0001); 2) high school+ (r = −0.601, p = <0.0001); 3) smoking (r = 0.729, p <0.0001); 4) obesity (r = 0.638, p <0.0001); 5) health perception (r = −0.531, p <0.0001); and 6) physical activity (r = −0.672, p <0.0001; Table 1).
TABLE 1.
Correlations with cancer mortality and six predictors from strongest to weakest.
| Predictor | Coefficient | p-value for coefficient |
|---|---|---|
| Smoking | 0.729 | <0.0001 |
| Physical activity | −0.671 | <0.0001 |
| Elevation | −0.656 | <0.0001 |
| Obesity | 0.638 | <0.0001 |
| High school+ | −0.601 | <0.0001 |
| Health perception | −0.530 | <0.0001 |
| Diet | −0.246 | 0.08 |
| Income | −0.203 | 0.1 |
| Insurance | 0.189 | 0.1 |
Bold = moderate strength (∼ 0.400), statistically significant (p <0.05) correlation coefficients.
Six predictors were considered appropriate for MLR. White’s test revealed p-values greater than 0.15 for all models. Elevation, smoking and high school+ revealed statistically significant (p <0.05) predictive strength values for p > t with smoking exhibiting the most statistically significant p-value (p <0.0001; Table 2). Among these three predictors, smoking exhibited the strongest standardized estimate (0.411) followed by elevation (−0.312) and high school+ (−0.310; Table 2).
TABLE 2.
Parameter estimates from strongest to weakest for multiple linear regression model.
| Predictor | Coefficient | p-value for coefficient |
|---|---|---|
| Smoking | 0.411 | <0.0001 |
| Elevation | −0.313 | 0.0004 |
| High school+ | −0.310 | 0.0002 |
| Health perception | 0.215 | 0.0970 |
| Physical activity | −0.194 | 0.0946 |
| Obesity | 0.161 | 0.1360 |
Bold = three strongest predictors evidenced by comparatively larger standard estimate and statistically significant p-values.
DISCUSSION
Interpretation of the MLR standardized estimates (UCLA, 2009) for elevation, where the standardized estimate is a negative value (= −0.313), a one standard deviation (of 1821 feet) increase in mean jurisdiction elevation could theoretically lead to a 0.313 standard deviation decrease in cancer mortality. A one standard deviation for cancer mortality = 8.47. Thus, we have the formula 8.47_ 0.313 = 2.65, which theoretically means 2.65 fewer deaths per 100,000 persons for every 1821 feet increase in mean jurisdiction elevation. For smoking, where the standard estimate is a positive value (= 0.411), a one standard deviation increase in smoking (= 3.30% more smokers in the population) could theoretically lead to a 0.411 standard deviation increase in cancer mortality. Thus, we have the formula 0.411_ 8.47 = 3.48 which theoretically means 3.48 more deaths per 100,000 persons for every 3.30% increase in smokers in the population. Of course prediction, as is the case in any statistical analysis, demonstrates neither causation nor certainty.
The possible link between cancer mortality and land elevation is consistent with the finding of Jagger (1998) who observed that cancer mortality was 1.26 times greater in low elevation Gulf states of Louisiana, Mississippi, and Alabama) compared to Rocky Mountain states (Idaho, Colorado, and New Mexico). In high NBR areas in China cancer mortality was also lower compared to lower NBR areas (Tao et al. 2000). On the other hand, a small increased risk of cancer has been found for nuclear workers exposed to low levels of radiation (Cardis et al. 2005). Clearly, the topic of low level radiation effects are not well understood (Hendry et al. 2009). In addition, since this is an ecological study, causal inferences cannot be made (Grimes and Schulz, 2002) though the establishment of a cause-and-effect relationship is a difficult task (Hill, 1965). Still, ecological studies can be the beginning of more rigorous research that seeks to determine cause-and-effect relationships (Grimes and Schulz, 2002). Other limitations to the study include: a) we make the assumption that population mobility has a negligible effect on the lag time between NBR exposure and cancer mortality; b) there is one year of cancer mortality (2002 in 2002–2006) that precedes the predictor year; and c) there may be other factors related to decreased mortality at high altitudes, such as the possible mechanism triggered by lower concentrations of oxygen. Weinberg (1987) for example theorizes that diminished oxygen at higher elevations may provide a protective effect in regard to cancer (and cardiovascular disease).
CONCLUSION
In this study’s multiple linear regression analyses, smoking was the strongest statistically significant predictor for cancer mortality (increased smoking → increased cancer mortality) followed by elevation (increased elevation along with its increased NBR → decreased cancer mortality), and then high school+ level education (increased levels of high school or higher → decreased cancer mortality). The indirect relationship between natural background radiation and cancer mortality suggests the possibility of radiation hormesis. In addition, since elevation ranked higher than obesity and physical activity, factors traditionally linked with cancer mortality, elevation (and natural background radiation) appears to be a factor in cancer mortality reduction.
REFERENCES
- Albano JD, Ward E, Jemal A, Anderson R, Cokkinides VE, Murray T, Henley J, Liff J, Thun MJ. Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute. 2007;99:1384–1394. doi: 10.1093/jnci/djm127. [DOI] [PubMed] [Google Scholar]
- Allright SP, Colgan PA, McAulay IR, Mullins E. Natual background radiation and cancer mortality in the Republic of Ireland. International Journal of Epidemiology. 1983;12(4):414–418. doi: 10.1093/ije/12.4.414. [DOI] [PubMed] [Google Scholar]
- Boyd C, Zhang-Salomons J, Grrome PA, Mackillop WJ. Associations between community income and cancer survival in Ontario, Canada, and the United States. Journal of Clinical Oncology. 1999;17:2244–2255. doi: 10.1200/JCO.1999.17.7.2244. [DOI] [PubMed] [Google Scholar]
- Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, Howe G, Kaldor J, Muirhead CR, Schubauer-Berigan M, Yoshimura T, Bermann F, Cowper G, Fix J, Hacker C, Heinmiller B, Marshall M, Thierry-Chef I, Utterback D, Ahn YO, Amoros E, Ashmore P, Auvinen A, Bae JM, Solano JB, Biau A, Combalot E, Deboodt P, Diez Sacristan A, Eklof M, Engels H, Engholm G, Gulis G, Habib R, Holan K, Hyvonen H, Kerekes A, Kurtinaitis J, Malker H, Martuzzi M, Mastauskas A, Monnet A, Moser M, Pearce MS, Richardson DB, Rodriguez-Artalejo F, Rogel A, Tardy H, Telle-Lamberton M, Turai I, Usel M, Veress K. Risk of cancer after low doses of ionizing radiation: retrospective cohort study in 15 countries. British Medical Journal. 2005 doi: 10.1136/bmj.38499.599861.EO. (online). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System. Health care access/coverage - 2003. 2009a. [Cited 2009 Dec 21]. Available from: http://apps.nccd.gov.
- Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System. Overweight and obesity (BMI) – 2003. 2009b. [Cited 2009 Dec 21]. Available from: http://apps.nccd.gov.
- Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System. Health status - 2003. 2009c. [Cited 2009 Dec 21]. Available from: http://apps.nccd.gov.
- Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System. Physical activity - 2003. 2009d. [Cited 2009 Dec 17]. Available from: http://apps.nccd.gov.
- Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System. Fruits and vegetables - 2003. 2009e. [Cited 2009 Dec 17]. Available from: http://apps.nccd.gov.
- Garson G. Testing of assumptions. Statnotes. 2009. Feb 26, [Internet]. North Carolina State University. [Cited 2009 Feb 27]. Available from: http://faculty.chass.ncsu.edu/garson/PA765/assumpt.htm.
- Grimes DA, Schulz KF. Descriptive studies: what they can and cannot do. The Lancet. 2002;359:145–149. doi: 10.1016/S0140-6736(02)07373-7. [DOI] [PubMed] [Google Scholar]
- Hendry JH, Simon SL, Wojcik A, Sohrabi M, Burkart W, Cardis E, Laurier D, Tirmarche M, Hayata I. Human exposure to high natural background radiation: what can it teach us about radiation risks. 2009. Journal of Radiological Protection. 29:A29–A42. doi: 10.1088/0952-4746/29/2A/S03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AB. The environment and disease: association or causation. Proceedings of the Royal Society of Medicine. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger J. Natural background radiation and cancer death in Rocky Mountain States and Gulf Coast states. Health Physics. 1998;75(4):428–430. doi: 10.1097/00004032-199810000-00012. [DOI] [PubMed] [Google Scholar]
- Luckey TD. Radiation hormesis: the good, the bad, and the ugly. Dose Response. 2006;4(3):169–190. doi: 10.2203/dose-response.06-102.Luckey. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDavid K, Tucker TC, Sloggett A, Coleman MP. Cancer survival in Kentucky and health insurance coverage. Archives of Internal Medicine. 2003;163:2135–2144. doi: 10.1001/archinte.163.18.2135. [DOI] [PubMed] [Google Scholar]
- Munro B. Philadelphia: Lippincott; 2001. Statistical methods for health care research. [Google Scholar]
- Nair MK, Nambi KSV, Amma NS, Gangadharan P, Jayalekshmi P, Jayadevan S, Cherian V, Reghuram KN. Population study in the high natural background radiation area in Kerala, India. Radiation Research. 1999;152:S145–148. [PubMed] [Google Scholar]
- National Cancer Institute (NCI) The majority of cancers are linked to the envirnment.[Cited 2009 Nov 30]] 2009a. Available from: http://www.cancer.gov.
- National Cancer Institute (NCI) Age-adjusted death rates for United States, 2002–2006. 2009b. [Cited 2009 Dec 31]. Available from http://statecancerprofiles.cancer.gov.
- National Cancer Institute (NCI) SEER Stat Fact Sheets. Surveillance Epidemiology and End Results. 2009c. National Cancer Institute. [Cited 2009 Oct 5]. Available from: www.seer.cancer.gov.
- Pett MA. Nonparametric statistics for health care research. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- Prekeges JL. Radiation hormesis, or, could all that radiation be good for us? Journal of Nuclear Medicine Technology. 2003;31:11–17. [PubMed] [Google Scholar]
- Preston RJ. Update on linear non-threshold dose-response model and implications for diagnostic radiology procedures. Health Physics. 2008;95(5):541–546. doi: 10.1097/01.HP.0000326332.80829.63. [DOI] [PubMed] [Google Scholar]
- Scott BR, Di Palma J. Sparsely ionizing diagnostic and natural background radiations are likely pre-veting cancer and other genomic-instability-associated diseases. Dose Response. 2006;5:230–255. doi: 10.2203/dose-response.06-002.Scott. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Z, Zha Y, Akiba S, Sun Q, Zou J, Li J, Liu Y, Kato H, Sugahara T, Wei L. Cancer mortality in high background radiation areas of Yangjiang, China during period between 1979 and 1995. Radiation Research. 2000;41(Suppl):31–41. doi: 10.1269/jrr.41.s31. [DOI] [PubMed] [Google Scholar]
- UCLA: Academic Technology Services, Statistical Consulting Group Regression with SAS. 2009. Available from: http://www.ats.ucla.edu/stat/sas/webbooks/reg/chapter2/sasreg2.htm.
- U.S. Nuclear Regulatory Commission (NRC) Doses in our daily lives. 2009. Available from: www.nrc.gov/
- U.S. Census Bureau . 2009a. Section 6. Geography and Environment. [Cited 2009 Dec 16]. Available from: www.census.gov. [Google Scholar]
- U.S. Census Bureau The 2006 Statistical Abstract. Table 191. 2009b. [Cited 2009 Nov 29]. Available from: www.census.gov.
- U.S. Census Bureau . 2009c. Table 13. [Cited 2009 Nov 29]. Available from: www.census.gov. [Google Scholar]
- U.S. Census Bureau Table 659. Personal per capita income. Income, expenditures, poverty and wealth. Statistical Abstract of the United States – 2008. 2009d. [Cited 2009 Dec 21]. Available from: www.census.gov.
- United States Life Tables, 2004 . National Vital Statistics Report. 9. Vol. 56. Centers for Disease Control and Prevention; 2007. [Cited 2009 Oct 5] Available from: www.cdc.gov. [PubMed] [Google Scholar]
- Wannamethee G, Shaper AG. Self-assessment of Health Status and Mortality in Middle-Aged British Men. International Journal of Epidemiology. 1991;20(1):239–245. doi: 10.1093/ije/20.1.239. [DOI] [PubMed] [Google Scholar]
- Weinberg CR, Brown KG, Hoel DG. Altitude, radiation, and mortality from cancer and heart disease. Radiation Research. 1987;112:381–390. [PubMed] [Google Scholar]