Abstract
Quadriceps avoidance and higher flexion strategy have been assumed as effects of ACL deficiency on knee joint function during gait. However, the effect of ACL deficiency on anteroposterior stability of the knee during gait is not well defined. In this study, ten patients with unilateral acute ACL ruptures and the contralateral side intact performed gait on a treadmill. Flexion angles and anteroposterior translation of the ACL injured and the intact controlateral knees were measured at every 10% of the stance phase of the gait (from heel strike to toe-off) using a combined MRI and dual fluoroscopic image system (DFIS). The data indicated that during the stance phase of the gait, the ACL-deficient knees showed higher flexion angles compared to the intact contralateral side, consistent with the assumption of a higher flexion gait strategy. However, the data also revealed that the ACL-deficient knees had higher anterior tibial translation compared to the intact contralateral side during the stance phase of the gait. The higher flexion gait strategy was not shown to correlate to a reduction of the anterior tibial translation in ACL deficient knees. These data may provide indications for conservative treatment or surgical reconstruction of the ACL injured knees in restoration of the knee kinematics during daily walking activities.
Keywords: Anterior cruciate ligament, Gait, Kinematics
INTRODUCTION
Numerous studies have demonstrated that ACL deficiency could lead to further meniscus tear and cartilage degeneration1, 2. The post-injury joint degeneration has been mainly attributed to altered joint kinematics caused by ACL deficiency3, 4. Therefore, understanding the effect of ACL injuries on knee joint motion is critical for development of conservative treatment or surgical reconstruction of the ACL injured knees. Historically, in-vitro cadaveric studies have reported on the anterior tibial translation when the knee was subjected to an anterior tibial load or a rotational torque5, 6. Few studies have reported on the knee joint motion in response simulated muscle loads7, 8. Recently, advanced imaging techniques have been used to examine the bony motion of the knee after ACL injuries during down-hill running9 and single leg lunge10–12. Few data, however, have been reported on the influence of ACL deficiency on knee joint motion during gait13–20 - the most commonly performed daily activities.
In literature, the effect of ACL deficiency on knee joint motion during gait has been assumed to be a quadriceps avoidance gait strategy15, where the patients with ACL injuries adapt to a reduced quadriceps contraction or extension joint moment during the midstance phase of the gait cycle. A reduced quadriceps function was thought to reduce the anterior shear force applied to the tibia at low flexion angles of the knee so that to avoid the increased anterior tibial translation due to the rupture of the ACL13, 15, 18. However, many studies have reported other adaptation strategies for ACL deficient patients, showing an increased flexion angle during stance phase of gait in ACL deficient knees14, 16, 17, 20. This higher knee flexion with the increased activity of the hamstring muscles suggested a mechanism exists which may improve sagittal joint stability during locomotion for ACL deficient knees. Although there are some studies that reported the tibiofemoral translation during gait13, 17, the soft tissue artifacts were thought to be a limitation of the skin-marker-based motion capture system, especially in knee joint translation21, 22. In addition, it is still unclear that either the quadriceps avoidance gait or higher flexion strategy can effectively avoid the excessive anterior tibial translation caused by ACL deficiency.
Recently, we validated a combined dual fluoroscopic imaging system (DFIS) and MR image technique23 in determination of the kinematics of the knee during stance phase of gait on a treadmill19, 24. The objective of this study was to determine the flexion angles and anteroposterior tibial translation of the knee after ACL injuries during gait on a treadmill and to compare these data to those measured from the intact contralateral side. We hypothesized that while the ACL deficient knees may adapt to higher flexion gait strategy under low demand activities such as walking, the anterior tibial translation could not be reduced due to the increased flexion angles.
MATERIAL AND METHODS
Patient Recruitment
Ten subjects who suffered from unilateral ACL tear were recruited for this study (5 females and 5 males with an average age of 35.5 ± 8.5 years, body weight of 77.1 ± 9.1 kg, body height of 1.76 ± 0.07 m and body mass index (BMI) of 24.9 ± 2.8 kg/m2). The ACL deficiency of the injured knee was verified through physical examination by an orthopaedic surgeon as well as MRI examination performed as part of this study. Additionally, the status of each injured ACL was confirmed during arthroscopy performed during surgical reconstruction of the ACL after the completion of this study. All knees included in this study were found to have an ACL rupture accompanied with minimal other tissue injuries that do not need surgical intervention. There was no history of injury, surgery or disease in the contralateral knees. The study was approved by our Institutional Review Board, and written consent was obtained from all study participants prior to the experiment.
Three-Dimensional Knee Model
The technique used in this study has been applied extensively to investigate knee joint kinematics7, 10, 19, 24. First, each knee was scanned in a relaxed extending position using a 3-T MR scanner (MAGNETOM Trio, Siemens, Malvern, PA) and a double-echo water excitation sequence. The MRI scans were used to generate sagittal plane images (512×512 pixels) with a field view of 16×16 cm and 1 mm spacing. The images were then imported into solid modeling software (Rhinoceros, version 4.0, Robert McNeel & Associates, Seattle, WA) and manually digitized to outline the contours of the femur and tibia. These outlines were used to reconstruct 3D geometric models of the knee.
Dual-Orthogonal Fluoroscopic System Setup
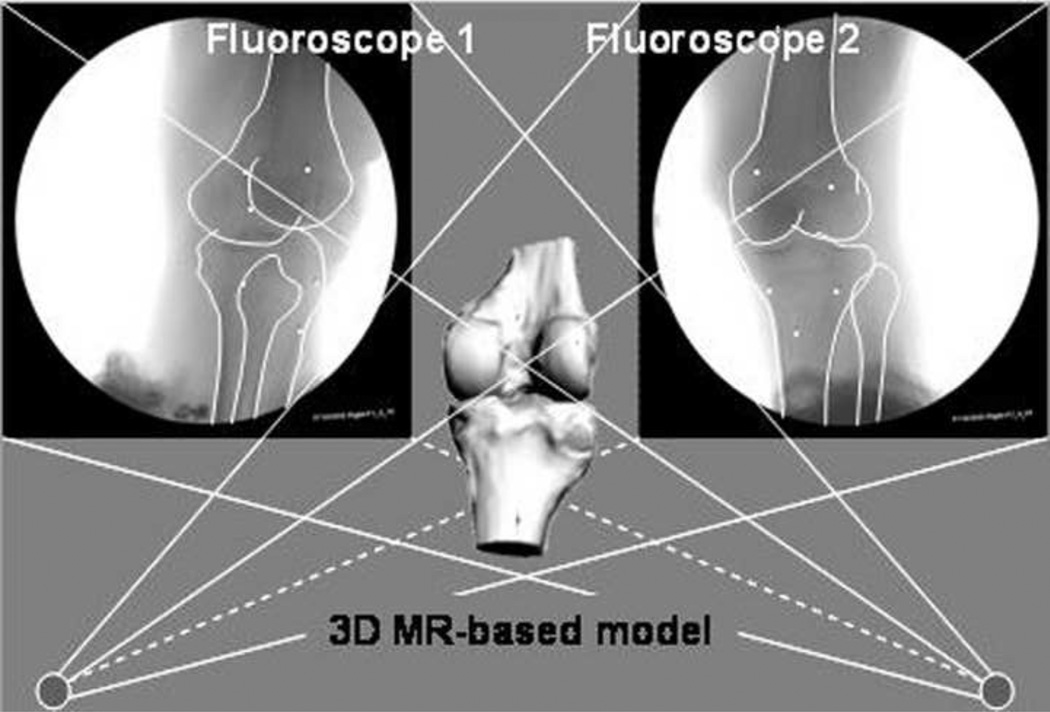
Next, the dual fluoroscopic imaging system setup, previously validated for treadmill gait analysis25, was used to determine the kinematics of both injured and intact contralateral knees during the stance phase of gait (Fig. 1). The subjects practiced the gait on the treadmill for one minute at a treadmill speed of 2.5 miles per hour (equivalent to 1.12 m/s). Two thin pressure sensors (force sensor resistor (FSR), Interlink Electronics, Camarillo, CA) were fixed to the bottom of each shoe, recording the heel strike (0%) and toe-off (100%) of the injured and the contralateral sides that was defined as the stance phase of the leg during the treadmill gait. Two laser-positioning devices, attached to the fluoroscopes, helped to align the target knee within the field of view of the fluoroscopes during the stance phase. Each knee was then imaged during three consecutive strides at a frame rate of 30 Hz using snapshots with an 8 ms pulse width23, 26. Fluoroscopic imaging was done during separate trials.
Fig. 1.
Each subject performed gait on a treadmill at 2.5 MPH and both intact contralateral and ACL deficient knees were scanned by the DFIS.
After experiment, the series of fluoroscopic images captured from heel strike to toe off were imported into the modeling software and placed in calibrated planes to reproduce the geometry of the fluoroscopes during the testing. In this study, we selected images at 10% increments during the stance phase. The 3D MR-based femur and tibia models (left or right) were also imported into the software and manipulated until the projections of the bony models matched the outlined silhouettes of the bones captured on the two fluoroscopic images (Fig. 2). The series of matched femur and tibia models reproduced the motion of the subject’s knee during the entire stance phase19, 23, 24.
Fig. 2.
Virtual reproduction of the fluoroscopic setup and tibiofemoral kinematics. The 3D MR-based models of the femur and tibia were matched to their projections on the fluoroscopic images.
Knee Kinematics
A consistent coordinate system was used to estimate the kinematics of both knees of each subject based on the series of matched bone models. The bone model of the right tibia (femur) was first mirrored and well aligned with the left tibial (femoral) model of the same subject and a common coordinate system was created for both left and mirrored right tibia (femur). Then, the coordinate system of the mirrored right tibia (femur) along with its coordinate system was mirrored back10. This coordinate system was then used to analyze the kinematics of both left and right knees. Because the same coordinate system was used on both the intact and ACL deficient knees, we were able to reduce the variability of our measurements caused by differences in coordinate systems.
The long axis of the tibia was parallel to the posterior wall of the tibial shaft and passed through the center point between the tibial spine10. Two circles were created to cover the posterior edges of both medial and lateral tibial plateaus. The line connecting to the centroids of two circles was defined as the medial-lateral axis. The anterior-posterior axis was perpendicular to the anterior-posterior and medial-lateral axes. The line that was parallel to the shaft of the femur was defined as the long axis of the femur. The transepicondylar line was obtained by linking the most pivot points on the medial and lateral condyles. The long axis passed the midpoint of the transepicondylar line (defined as the femoral center). Anteroposterior tibiofemoral translation was defined as the motion of the femoral center along the anterior axis in the tibial coordinate system. Flexion of the knee was defined as the angle between the long axes of the femur and tibia, projection onto the sagittal plane of the tibia24, 25.
In this fashion, anterior-posterior translations of the femur and flexion angles of the knee were determined during the stance phase of a treadmill gait. For comparison to previous published literatures, we converted the femoral translation to that of the tibia relative to the femur.
Statistical Analysis
We compared the flexion angles and the anteroposterior tibial translation of the ACL deficient and intact contralateral knees at every 10% of the stance phase of the gait. A repeated measure ANOVA was used for data analysis. A Newman-Keuls post hoc analysis was performed if the ANOVA detected a difference. A p<0.05 was defined as statistical significance.
RESULTS
Flexion
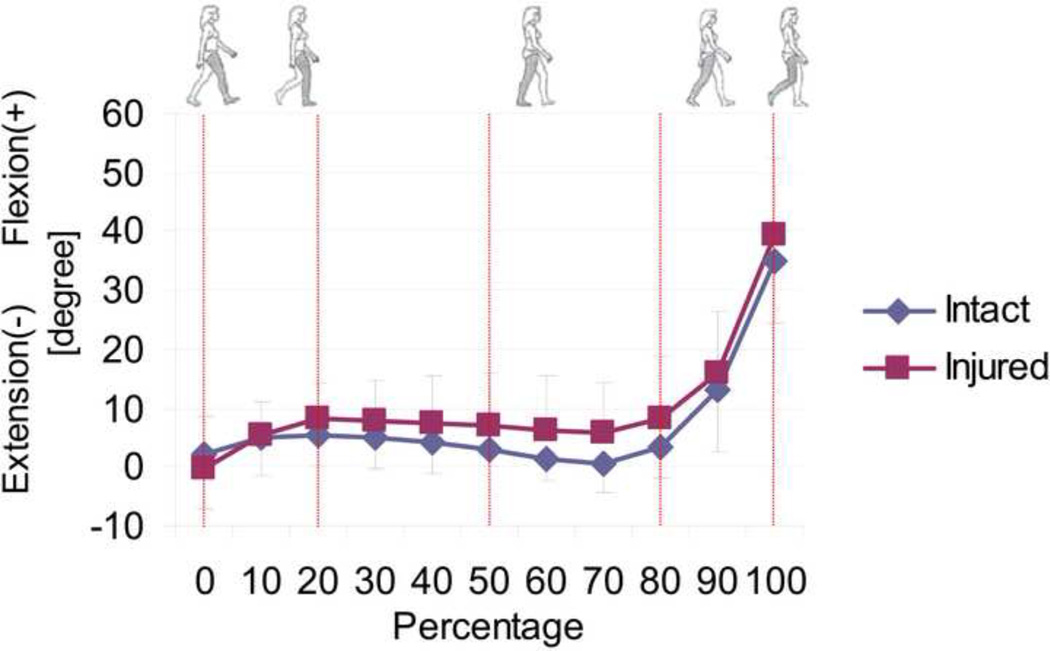
Both the ACL deficient and normal knees demonstrated a similar flexion pattern along the stance phase of the gait cycle (Fig. 3). More specifically, both groups extended similarly at heel strike (2.2 ± 9.2° in normal group and −0.5 ± 9.3° in ACL deficient group) and flexed during 0 to 20%. The flexion reached the first peak with 8.3 ± 5.9° and 5.3 ± 5.1° in the ACL deficient and normal knees, respectively, at 20% of the stance phase. Thereafter, the ACL deficient knees kept to rotate in higher flexion angles during the rest of the stance phase compared to the normal knees. At the end of the stance phase, the ACL deficient knees flexed to the second peak with 39.2 ± 13.1° and normal knees flexed to 34.8 ± 10.4°.
Fig. 3.
Flexion-extension angle of the knee joint for the intact and ACL deficient groups during the stance phase of treadmill gait.
Anteroposterior tibial translation
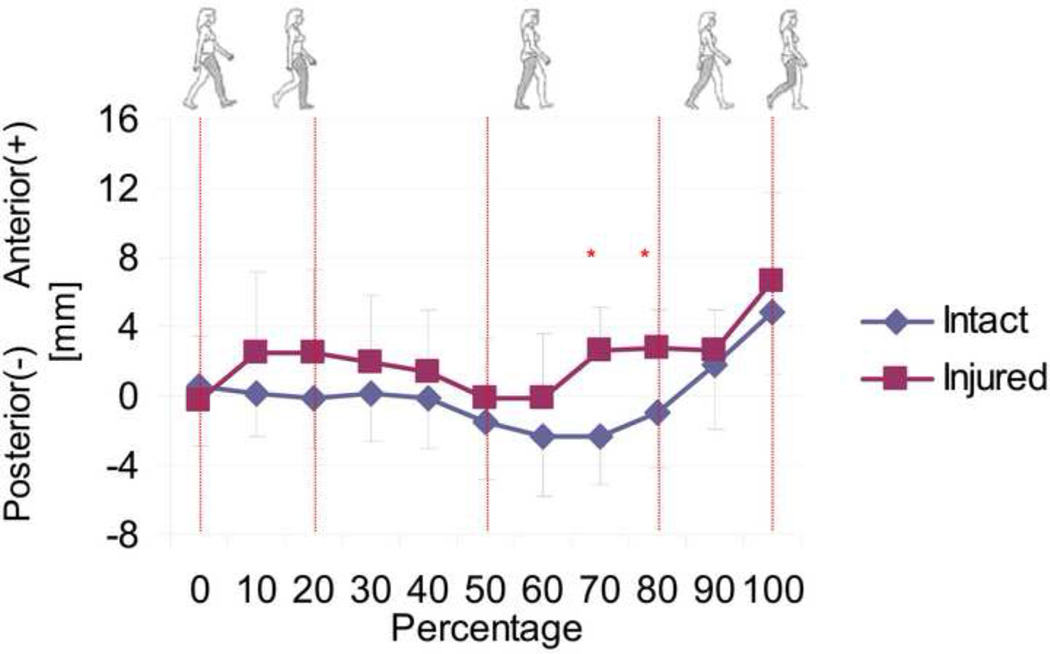
The ACL deficient knees showed significant differences in anteroposterior translation (tibia relative to femur) during the late stance phase of the gait cycle (p<0.05, Fig. 4). At heel strike, both groups showed similar anterior tibial translation (0.6 ± 3.5 mm in normal group and −0.3 ± 3.8 mm in ACL deficient group, p>0.05). The anterior tibial translation was 2.5 ± 4.9 mm in ACL deficient knees which is higher than that in the normal knees (−0.1 ± 2.9 mm) at 20% of the stance phase (p>0.05). Thereafter, the ACL deficient knees kept to move more anteriorly during the rest of the stance phase compared to the normal knees. During the 70 and 80% of the stance phase, the tibia in deficient knees shifted more anteriorly (2.7 ± 2.4 and 2.8 ± 2.1 mm) than that in the normal group (−2.4 ± 2.7 and −1.0 ± 3.2, p<0.05). At the end of the stance phase, the ACL deficient knees had an anterior tibial translation of 6.6 ± 5.1 mm and normal knees of 4.9 ± 3.6 mm (p>0.05).
Fig. 4.
Anteroposterior translation of the tibia relative to the femur for the intact and ACL deficient knees during the stance phase of treadmill gait. Asterisk denotes statistically significant difference at p<0.05.
DISCUSSION
This study investigated the flexion angle and the anterior-posterior translation of the ACL-deficient and intact contralateral knees during the stance phase of gait on a treadmill. In general, the ACL-deficient knees tended to flex more and have more anterior tibial translation compared to the intact contralateral side. The results confirmed our hypothesis on the effect of ACL deficiency on the motion of the knee during gait on a treadmill.
The gait is the mostly performed activity of daily living. The kinematic changes during gait after ACL deficiency may have profound effect on the health of the joint. In literature, kinematics of the ACL deficient knees has been mostly studied by using skin-marker based motion analysis systems13, 14, 16–18, 20. Some of these studies reported that ACL deficient knees showed higher flexion in mid to late stance phases14, 20 or throughout the stance phase16. Other studies have shown that the ACL-deficient knees tended to flex less throughout the mid-and terminal stance phase of gait15, 18, 27, 28, some of which showed less external flexion moment and supported the “quadriceps avoidance” assumption of the deficient knee during gait to decrease anterior shear force on the tibia15. However, our data showed higher flexion angle from the midstance phase to toe off which means the ACL deficient group tended to use the higher flexion strategy during gait.
Few previous studies have investigated anterior tibial translation of ACL deficient knees during gait cycle13, 17, 29. Andriacchi et al. did not observe a significant difference in anteroposterior translation during gait cycle, except at the terminal swing13. Gao et al. also did not find significant difference in anteroposterior translation between ACL deficient and normal knees17. Our data showed in average a significant increase in anterior tibial translation in the terminal stance phase in ACL deficient knees compared to the intact contralateral side. We should note that there are several different features in our study compare to the other reported studies. Our study was performed on the same subjects with one knee injured and one knee intact. In addition, a treadmill gait, although not a free and natural walking, may provide a controlled testing conditions for all subjects. Finally, the combined DFIS and MRI modeling technique allowed an improved accuracy in measurements of knee joint kinematics since the kinematics was measured from the bony structures of the knee.
Beard et al.14 and Robers et al.20 found the increasing firing of EMG in ACL deficient groups with higher flexion during stance phase. Theoretically, the increase in knee flexion allows the hamstring muscles acting across the knee joint to have a greater component of the muscle force along the tibial plateau surface and therefore be more effective in reducing sagittal subluxation of the tibia in relation to the femur. In the “quadriceps avoidance” gait strategy, because of less quadriceps forces might occur, less anterior load may be applied to the tibia. The physiological response of these two adaptation strategies was thought to lead to avoid the excessive anterior tibial translation during the stance phase of the gait cycle15. However, our data showed an increased anterior tibial translation in the ACL deficient knees during the stance phase of gait, even though the flexion angles are higher than the intact knees. This kinematic response of the knee during gait could not be explained by both higher flexion and quadriceps avoidance strategies. Future studies should include the EMG measurement and dual fluoroscopic images to examine the correlation between the neuromuscular activities with the joint motions in the ACL injured knees. Our data may also suggest that conservative or surgical treatment of the ACL deficient knees may need to restore normal knee flexion-extension capability.
There were several potential limitations associate with this study. During gait analysis, the DFIS could only image the knee during stance phase of the gait. It is technically difficult to record the knee positions during swing phase. Treadmill walking instead of level walking was investigated in this study. Recent reports demonstrated that in healthy subjects the differences in kinematics between the treadmill walking and level walking are minimal and the overall patterns of these two activities are similar30. Furthermore, contralateral uninjured knees were used as normal control knees. Kozanek et al recently demonstrated that there was no statistically significant difference between the in vivo kinematics of the uninjured contralateral knee joint of patients with acute unilateral ACL deficiency and subjects without knee injury during lunge activity19. The potentially benefit for using contralateral knees is that we could directly compare the differences between two legs of the same individual. The inter-subjects variable would be eliminated. Future investigation should include comparison with the gait kinematics data of normal subjects.
In summary, this study examined the changes in flexion angles and anteroposterior translation of the knee after ACL injury during the stance phase of gait. In ACL deficient knees, the tibia tends to shift more anteriorly. The increased flexion angle was not accompanied by a restoration of anterior tibial translation. These kinematic changes could lead to abnormal tibiofemoral cartilage contact during daily walking, thus may represent a biomechanical mechanism of joint degeneration after ACL injuries of the knee. A surgical reconstruction or conservative treatment aimed at correcting these abnormalities is necessary to restore the normal flexion capability of the ACL injured knees during gait.
Combined DFIS and MR image based technique was used to investigate treadmill gait of the knee.
Higher flexion angles and anterior tibial translations were found in ACL deficient knees during stance phase of gait.
Higher flexion gait strategy of ACL injured knees could not compensate the anterior tibial translation effectively.
Acknowledgements
The authors would like to gratefully acknowledge the financial support of the National Institute of Health (R01 AR055612) and the Department of Orthopaedic Surgery at Massachusetts General Hospital.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 2.Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29(2):226–231. doi: 10.1177/03635465010290021801. [DOI] [PubMed] [Google Scholar]
- 3.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 4.Buckwalter JA, Lane NE. Athletics and osteoarthritis. Am J Sports Med. 1997;25(6):873–881. doi: 10.1177/036354659702500624. [DOI] [PubMed] [Google Scholar]
- 5.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22(1):85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 6.Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon . A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84-A(6):907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Li G, Zayontz S, Most E, DeFrate LE, Suggs JF, Rubash HE. In situ forces of the anterior and posterior cruciate ligaments in high knee flexion: an in vitro investigation. J Orthop Res. 2004;22(2):293–297. doi: 10.1016/S0736-0266(03)00179-7. [DOI] [PubMed] [Google Scholar]
- 8.Torzilli PA, Deng X, Warren RF. The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med. 1994;22(1):105–112. doi: 10.1177/036354659402200117. [DOI] [PubMed] [Google Scholar]
- 9.Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(4):975–983. doi: 10.1177/0363546503261709. [DOI] [PubMed] [Google Scholar]
- 10.Defrate LE, Papannagari R, Gill TJ, Moses JM, Pathare NP, Li G. The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency: an in vivo imaging analysis. Am J Sports Med. 2006;34(8):1240–1246. doi: 10.1177/0363546506287299. [DOI] [PubMed] [Google Scholar]
- 11.Li G, Moses JM, Papannagari R, Pathare NP, DeFrate LE, Gill TJ. Anterior cruciate ligament deficiency alters the in vivo motion of the tibiofemoral cartilage contact points in both the anteroposterior and mediolateral directions. J Bone Joint Surg Am. 2006;88(8):1826–1834. doi: 10.2106/JBJS.E.00539. [DOI] [PubMed] [Google Scholar]
- 12.Van de Velde SK, Bingham JT, Hosseini A, Kozanek M, DeFrate LE, Gill TJ, Li G. Increased tibiofemoral cartilage contact deformation in patients with anterior cruciate ligament deficiency. Arthritis Rheum. 2009;60(12):3693–3702. doi: 10.1002/art.24965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38(2):293–298. doi: 10.1016/j.jbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Beard DJ, Soundarapandian RS, O'Connor JJ, Dodd CAF. A deficient anterior cruciate ligament does not lead to quadriceps avoidance gait. Gait and Posture. 1996;4(2):83–88. doi: 10.1016/s0966-6362(99)00038-7. [DOI] [PubMed] [Google Scholar]
- 15.Berchuck M, Andriacchi TP, Bach BR, Reider B. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;72(6):871–877. [PubMed] [Google Scholar]
- 16.Fuentes A, Hagemeister N, Ranger P, Heron T, de Guise JA. Gait adaptation in chronic anterior cruciate ligament-deficient patients: Pivot-shift avoidance gait. Clin Biomech (Bristol, Avon) 2011;26(2):181–187. doi: 10.1016/j.clinbiomech.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 17.Gao B, Zheng NN. Alterations in three-dimensional joint kinematics of anterior cruciate ligament-deficient and -reconstructed knees during walking. Clin Biomech (Bristol, Avon) 2010;25(3):222–229. doi: 10.1016/j.clinbiomech.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N. Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med. 2003;31(1):75–79. doi: 10.1177/03635465030310012401. [DOI] [PubMed] [Google Scholar]
- 19.Kozanek M, Van de Velde SK, Gill TJ, Li G. The contralateral knee joint in cruciate ligament deficiency. Am J Sports Med. 2008;36(11):2151–2157. doi: 10.1177/0363546508319051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts CS, Rash GS, Honaker JT, Wachowiak MP, Shaw JC. A deficient anterior cruciate ligament does not lead to quadriceps avoidance gait. Gait Posture. 1999;10(3):189–199. doi: 10.1016/s0966-6362(99)00038-7. [DOI] [PubMed] [Google Scholar]
- 21.Benoit DL, Ramsey DK, Lamontagne M, Xu L, Wretenberg P, Renstrom P. Effect of skin movement artifact on knee kinematics during gait and cutting motions measured in vivo. Gait Posture. 2006;24(2):152–164. doi: 10.1016/j.gaitpost.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Stagni R, Fantozzi S, Cappello A, Leardini A. Quantification of soft tissue artefact in motion analysis by combining 3D fluoroscopy and stereophotogrammetry: a study on two subjects. Clin Biomech (Bristol, Avon) 2005;20(3):320–329. doi: 10.1016/j.clinbiomech.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 23.Li G, Van de Velde SK, Bingham JT. Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech. 2008;41(7):1616–1622. doi: 10.1016/j.jbiomech.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 24.Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–1884. doi: 10.1016/j.jbiomech.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li G, Kozanek M, Hosseini A, Liu F, Van de Velde SK, Rubash HE. New fluoroscopic imaging technique for investigation of 6DOF knee kinematics during treadmill gait. J Orthop Surg Res. 2009;46 doi: 10.1186/1749-799X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tashman S. Comments on "validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion". J Biomech. 2008;41(15):3290–3291. doi: 10.1016/j.jbiomech.2008.07.038. author reply 3292–3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeVita P, Hortobagyi T, Barrier J. Gait biomechanics are not normal after anterior cruciate ligament reconstruction and accelerated rehabilitation. Med Sci Sports Exerc. 1998;30(10):1481–1488. doi: 10.1097/00005768-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Shiavi R, Limbird T, Frazer M, Stivers K, Strauss A, Abramovitz J. Helical motion analysis of the knee--II. Kinematics of uninjured and injured knees during walking and pivoting. J Biomech. 1987;20(7):653–665. doi: 10.1016/0021-9290(87)90032-7. [DOI] [PubMed] [Google Scholar]
- 29.Ciccotti MG, Kerlan RK, Perry J, Pink M. An electromyographic analysis of the knee during functional activities. II. The anterior cruciate ligament-deficient and -reconstructed profiles. Am J Sports Med. 1994;22(5):651–658. doi: 10.1177/036354659402200513. [DOI] [PubMed] [Google Scholar]
- 30.Lee SJ, Hidler J. Biomechanics of overground vs. treadmill walking in healthy individuals. J Appl Physiol. 2008;104(3):747–755. doi: 10.1152/japplphysiol.01380.2006. [DOI] [PubMed] [Google Scholar]