Abstract
Understanding precursors to distress and emotional well-being (EWB) experienced in anticipation of radiotherapy would facilitate the ability to intervene with this emotional upset (i.e., higher distress, lower EWB). Thus the present study tested an expectancy-based model for explaining emotional upset in breast cancer patients prior to radiotherapy. Women affected by breast cancer (N=106) were recruited and participants completed questionnaires prior to commencing radiotherapy. Structural equation modeling was used test a cross-sectional model, which assessed the ability of dispositional optimism (Life Orientation Test-Revised - two factors), response expectancies (VAS items), medical (type of surgery, cancer stage, chemotherapy history) and demographic (age, race/ethnicity, education, marital status) variables to predict both EWB (Functional Assessment of Chronic Illness Therapy - Emotional Well-being Subscale) and distress (Profile of Mood States - Short Version). The model represented a good fit to the data accounting for 65% of the variance in EWB and 69% in Distress. Significant predictors of emotional upset were pessimism, response expectancies, Latina ethnicity, cancer stage, and having had a mastectomy. These variables explained a large portion of emotional upset experienced prior to radiotherapy for breast cancer and are important to consider when aiming to reduce distress and improve EWB in this context.
Keywords: distress, quality of life, breast neoplasm, radiotherapy, optimism, response expectancies
Objective
More than 192,000 American women were diagnosed with breast cancer in 2009 making breast cancer the leading site of new female cancer cases in the United States (American Cancer Society, 2009). Radiotherapy is an effective treatment for breast cancer improving the survival rate after breast-conserving surgery (Vinh-Hung & Verschraegen, 2004). Although medically beneficial, radiotherapy is not without costs. Studies have found that radiotherapy can be physically and psychologically distressing for breast cancer patients and that approximately 30–50% of women experience moderate to severe levels of distress and a decline in quality of life during the course of radiotherapy treatment (Browall et al., 2008; Knobf & Sun, 2005; Mose et al., 2001; Schnur, Ouellette, Bovbjerg, & Montgomery, 2009; Schnur, Ouellette, DiLorenzo, Green, & Montgomery, 2010; Sollner, Maislinger, Konig, Devries, & Lukas, 2004; Stiegelis, Ranchor, & Sanderman, 2004; Wengstrom, Haggmark, Strander, & Forsberg, 2000). It is important to understand emotional well-being (EWB) and distress prior to radiotherapy because literature suggests that increased distress prior to breast cancer treatments (i.e. surgery, chemotherapy) can contribute to distress and physical side effects during and after these treatments (David, Montgomery, & Bovbjerg, 2006; DiLorenzo et al., 1995; Montgomery et al., 2003; Montgomery & Bovbjerg, 2004; Ozalp, Sarioglu, Tuncel, Aslan, & Kadiogullari, 2003; Schnur et al., 2008). Thus, understanding predictors of distress prior to radiotherapy would facilitate the ability to intervene with distress as soon as possible.
In the radiotherapy setting in particular, less emotional distress experienced prior to treatment was found to be related to a better quality of life after treatment (Browall et al., 2008) and distress experienced prior to the first treatment was found to be predictive of anxiety during the course of treatment (Mose et al., 2001). Only one study, to our knowledge, has explored the prevalence (48–53% of patients) and potential predictors (i.e., age, tumor stage, lymph node status, application of systemic therapy) of distress (i.e., afraid of radiotherapy, distressed because the carcinoma affected their breast) prior to radiotherapy (Mose et al., 2001). Results indicated that only younger age was associated with distress at this point in the treatment trajectory. However, this study did not use a validated measure of distress or identify all potential predictors.
There is considerable evidence supporting that individual differences in expectancies, both general (i.e., optimism, pessimism) and specific (i.e., response expectancies) are especially applicable to understanding the variability in anticipatory emotional distress and well-being in the cancer setting (Carver et al., 1994; David et al., 2006; Epping-Jordan et al., 1999; Montgomery et al., 2003; Stanton & Snider, 1993). That is, the literature demonstrates that a higher level of optimism, defined as generalized favorable expectancies for the future (Scheier & Carver, 1985), is associated with lower levels of emotional distress, anxiety, and depression in people affected by cancer (David et al., 2006; Epping-Jordan et al., 1999). Studies exploring the measurement of dispositional optimism (LOT-R; Bryant, 2004; Chang, Maydeu-Olivares, & D'Zurilla, 1997; Marshall, Wortman, Kusulas, Hervig & Vickers, 1992) have shown that two factors often emerge (i.e., high optimism, low pessimism) and exhibit differential predictive ability. In general, the pessimism subscale is more predictive of distress than is the optimism subscale (Mroczek, Spiro, Aldwin, Ozer, &.Bossé, 1993; Robinsen-Whelen, Kim, MacCallum, & Kiecolt-Glaser, 1997). This unique ability of pessimism to predict distress was maintained in a recent study of women diagnosed with cancer (Zenger, Glaesmer, Hockel, & Hinz, 2010). Therefore, it is optimal to examine optimism and pessimism as distinct factors. As for response expectancies, defined as anticipations of non-volitional outcomes, research suggests that the more distress expected by those affected by cancer, the more distress they experience (Kirsch, Mearns, & Catanzaro, 1990; Sucala & Szentagotai-Tatar, 2010).
In addition to expectancy-related factors, medical (e.g., history of chemotherapy, type of surgery, stage of cancer; (Broeckel, Jacobsen, Horton, Balducci, & Lyman, 1998; Glanz & Lerman, 1992; Moyer & Salovey, 1996)) and demographic factors (e.g., age, race, ethnicity, education, and marital status; (Avis, Crawford, & Manuel, 2004; Avis, Crawford, & Manuel, 2005; Carver, Smith, Petronis, & Antoni, 2006; Costanzo, Ryff, & Singer, 2009; Epping-Jordan et al., 1999; Henselmans et al., 2010; Schootman, Deshpande, Pruitt, Aft, & Jeffe, 2010)) have also been shown to contribute to breast cancer patients' levels of distress and EWB. In the studies that have found significant associations between these factors and distress, distress was typically higher when women had chemotherapy (Broeckel et al., 1998), had a mastectomy (Arndt, Stegmaier, Ziegler, & Brenner, 2008), were diagnosed with a higher stage of cancer (Weitzner, Meyers, Stuebing, & Saleeba, 1997), were younger (Costanzo et al., 2009), of Latina ethnicity (Janz, 2009), less educated (Ashing-Giwa, 2009) and not married (Carver, Smith, Antoni, Petronis, Weiss, & Derhagopian, 2005). However, the relationships of these factors with distress are not consistently significant across studies (e.g., Mosher, DuHamel, Egert, & Smith, 2010; Schnoll, Harlow, Stolback, & Brandt, 1998; Weitzner et al., 1997) and have yet to be explored prior to radiotherapy for breast cancer.
The goal of the present study was to identify expectancy, medical, and demographic predictors of anticipatory distress and emotional well-being prior to undergoing breast cancer radiotherapy. These predictors were incorporated into one model, which allowed us to determine the unique predictive ability of each construct. Based on previous research, we hypothesized that: (1) high optimism and low pessimism would be positively associated with EWB and negatively associated with distress (Carver et al., 2005; Montgomery et al., 2003); and (2) response expectancies for distress would be negatively associated with EWB and positively associated with distress (Kirsch et al., 1990). No direction was hypothesized for the association of demographic and medical factors with distress and EWB; however, these relationships were explored.
Design
Participants and Procedures
Patients were referred by physicians at two radiation oncology practices in large urban teaching hospitals. Consecutive patients were recruited, confirmed eligible, and consented by research assistants in an exam room prior to radiotherapy planning sessions. Data were collected in this setting. Patients were recruited from November 2004 through March 2010 and were compensated $50 for study participation. All study procedures were approved by the Institutional Review Board.
Eligibility criteria for the present study included being: scheduled for external beam breast cancer radiotherapy; able to speak and read English (as the questionnaires were in English); over age 18; not pregnant; and having Stage 0, I, II or III breast cancer. Exclusion criteria were uncontrolled mental illness or medical illness (as determined by medical chart review) and metastatic disease.
Main Outcome Measures
The Profile of Mood States Short Version (POMS-SV; Shacham, 1983) is a shortened version of the classic mood adjective checklist (McNair, Lorr, & Droppleman, 1971). It has 37 items, six different subscales (i.e., tension-anxiety, depression-dejection; anger-hostility; vigor-activity; fatigue-inertia; confusion-bewilderment) and also offers an average distress score (Total Mood Disturbance). The average distress score is calculated by summing up the individual items that range from 0 (not at all) to 4 (extremely; with a score of 1 indicating a little distress), and dividing by 37. The vigor-activity subscale is reverse scored and included in the total of the other subscales. There is evidence that the scale has strong psychometric properties when used with breast cancer patients (DiLorenzo, Bovbjerg, Montgomery, Jacobsen, & Valdimarsdottir, 1999) and it was internally consistent in the present sample (α = .95).
The Functional Assessment of Chronic Illness Therapy - Emotional Well-being Subscale (FACT-G; Webster, Cella, & Yost, 2003) was used to asses emotional well-being (EWB). The six items ask participants to indicate their emotional state with items such as “I feel sad” on a scale from 0 (not at all) to 4 (very much). The FACT-G is a well-validated measure of quality of life (Webster et al., 2003) that has normative data available for breast cancer patients (Brady et al., 1997). The EWB subscale is scored by summing the six items (possible range of scores from 0–24) so that higher scores indicate greater emotional well-being (i.e. lower distress). These items were internally consistent in the present sample (α = .76).
The Life Orientation Test (LOT-R; Scheier, Carver, & Bridges, 1994) is a 10-item measure assessing dispositional optimism (consisting of three items that assess optimism, three items that assess pessimism, and 4 filler items). The present study used a bidimensional model of the LOTR in which optimism and pessimism are evaluated as separate independent predictors. High scores on the pessimism subscale indicate low pessimism. The subscales of optimism (α = .76) and pessimism (α = .82) were internally consistent in this sample.
Response Expectancies were assessed with four Visual Analog Scale (VAS) items asking patients' to indicate their expectations for how emotionally upset, depressed, stressed, or relaxed they will be while undergoing radiotherapy. VAS scores range from 0 to 100 based on how many millimeters from the left participants made their mark on a line anchored by statements such as “not at all upset” to “as upset as I could be.” VAS assessment of expectations has been previously used with breast cancer patients and has been shown to be related to distress (Montgomery & Bovbjerg, 2004). The four response expectancy items assessed in the present sample were internally consistent when combined into a single scale (α = .84).
The Demographic Questionnaire is a face-valid self-report questionnaire used for assessing age, race/ethnicity, education, and marital status.
Medical charts were abstracted to obtain relevant medical history variables including type of surgery (lumpectomy vs. mastectomy), cancer stage (0, I, II, III), and chemotherapy history (yes/no).
Overview of the Analytic Strategy
Prior to undertaking the formal analyses described below, the data were examined to determine the distributional characteristics of the variables to be employed. There was no evidence to suggest any significant departures from normality. In addition, graphical inspection of the data indicated that there were no outliers. Initial correlation analyses were conducted (SPSS 17.0) to determine which demographic variables were significantly related to the total EWB score and mean total distress (i.e., Total Mood Disturbance measured by the POMS). Only variables with significant associations to the outcomes were included in the proposed model.
A structural equation model (SEM) with latent variables was used to test the proposed expectancy-based model. This model included paths from all of the predictors (i.e., optimism, pessimism, response expectancies, medical and demographic variables) to each of the two outcome variables (i.e., EWB, distress). A number of the latent constructs included in this model are based on scales having multiple items. Prior to conducting the SEM, individual items representing the Optimism, Pessimism, Response Expectancies, EWB, and Distress latent constructs were randomly combined into item parcels reflecting the constructs that these items represent. Creating item parcels increases the reliability of the item parcel responses, leads to fewer parameters being estimated, is more likely to yield normally distributed factor indicators, and yields more stable parameter estimates (Hau & Marsh, 2004). Two item parcels for each construct were developed.
The analyses employed LISREL v. 8.8 (Joreskog & Sorbom, 2007). Because of the small amount of missing data (6.04%), Full Information Maximum Likelihood (FIML) was used for parameter estimation. The statistical analyses employed in this study involved estimates of the variance/covariance matrix in the presence of missing data and these estimates were only used to obtain starting values for the FIML procedure.
In the missing data case, LISREL only reports the FIML Chi-Square and its associated degrees of freedom as well as the point estimate for the root mean square error of approximation (RMSEA). To determine the fit of the model to the observed data, the Chi-Square statistic and the RMSEA and its corresponding test of close fit were used. The 90% confidence limit (CI) as well as a significance test of close fit for the latter measure is provided. Evidence for a good fit is indicated by a non-significant Chi-Square, a RMSEA less than .08 (Browne & Cudek, 1993), and a non-significant p-value for the RMSEA's test of close fit.
Results
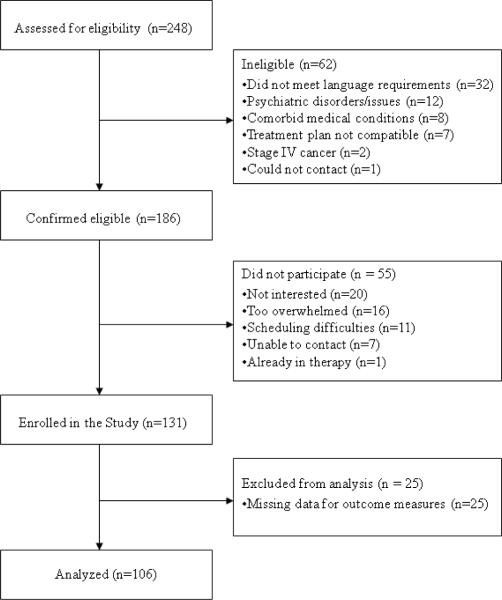
A total of 106 women completed all of the questionnaires reported in the present study. The flow of the recruitment of consecutive study participants is displayed in Figure 1 and their descriptive characteristics are presented in Table 1. A cross-sectional design was used for the present analysis. In an effort to address potential sources of bias, participants were not prescreened for distress, were recruited consecutively, and the Principal Investigator did not collect data.
Figure 1.
Flow diagram of study participants
Table 1.
Descriptive statistics of demographic variables
| Age | M = 56.40 (12.40) Years |
| Marital Status | 51.5% Married |
| Education | 58.3% College Graduates |
| Race | 69.9% White; 24.3% Black; 1.9% Asian; 3.9% other |
| Ethnicity | 20.0% Latina |
| History of Chemotherapy | 39.00% |
| Type of Surgery | 68% Lumpectomy |
| 32% Mastectomy | |
| Stage | 68.6% Stage 0 or 1 |
| 31.4% Stages 2 or 3 |
The correlations among the variables included in the model are displayed in Table 2. The mean distress score (Total Mood Disturbance) in this sample was 1.07 (SD = 0.78) and the overall mean score for EWB was 18.38 (SD = 4.36). Each included predictor was significantly correlated with one of the outcome variables when analyzed individually. Additionally, all of the predictors were hypothesized to have significant paths to both outcome variables (EWB and Distress).
Table 2.
Correlations among variables included in the hypothesized model
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Optimism Cluster 1 | -- | 0.46*** | 0.32*** | 0.31*** | −0.25* | −0.12 | 0.16 | −0.04 | −0.17 | −0.06 | −0.07 | 0.21* | 0.33*** | −0.29*** | −0.27*** |
| 2. Optimism Cluster 2 | -- | 0.25* | −0.15 | −0.19 | −0.10 | −0.04 | −0.14 | −0.22* | −0.15 | −0.04 | 0.22* | 0.28** | −0.40*** | −0.20* | |
| 3. Pessimism Cluster 1 | -- | 0.59*** | 0.22* | −0.18 | 0.06 | −0.04 | −0.12 | −0.09 | −0.09 | 0.36*** | 0.25* | −0.35*** | −0.31** | ||
| 4. Pessimism Cluster 2 | -- | −0.25* | −0.21 | 0.15 | 0.14 | −0.02 | 0.03 | −0.04 | 0.34*** | 0.16 | −0.42*** | −0.31** | |||
| 5. Response Expectancy Cluster 1 | -- | 0.69*** | −0.09 | 0.13 | 0.05 | 0.11 | 0.21 | −0.46*** | −0.22* | 0.51*** | 0.46*** | ||||
| 6. Response Expectancey Cluster 2 | -- | 0.16 | 0.01 | 0.09 | 0.10 | 0.19 | −0.49*** | −0.29** | 0.41*** | 0.51*** | |||||
| 7. Age | -- | −0.06 | −0.19* | −0.15 | −0.13 | 0.24* | 0.20* | −0.13 | −0.24* | ||||||
| 8. History of Chemotherapy | -- | 0.39*** | .71*** | −0.10 | −0.02 | −0.17 | 0.19* | 0.09 | |||||||
| 9. Type of Surgery | -- | .52*** | 0.06 | −0.19 | −0.36*** | 0.15 | 0.15 | ||||||||
| 10. Stage | -- | 0.07 | −0.03 | 0.03 | 0.20* | 0.19* | |||||||||
| 11. Latina Ethnicity | -- | −0.37*** | −0.28** | 0.27** | 0.33*** | ||||||||||
|
| |||||||||||||||
| 12. Emotional Well Being Cluster 1 | -- | 0.58*** | −0.61*** | −0.67*** | |||||||||||
| 13. Emotional Well Being Cluster 2 | -- | −0.51*** | −0.58*** | ||||||||||||
| 14. Distress Cluster 1 | -- | 0.68*** | |||||||||||||
| 15. Distress Cluster 2 | -- | ||||||||||||||
p <.05
p >01
p <.001
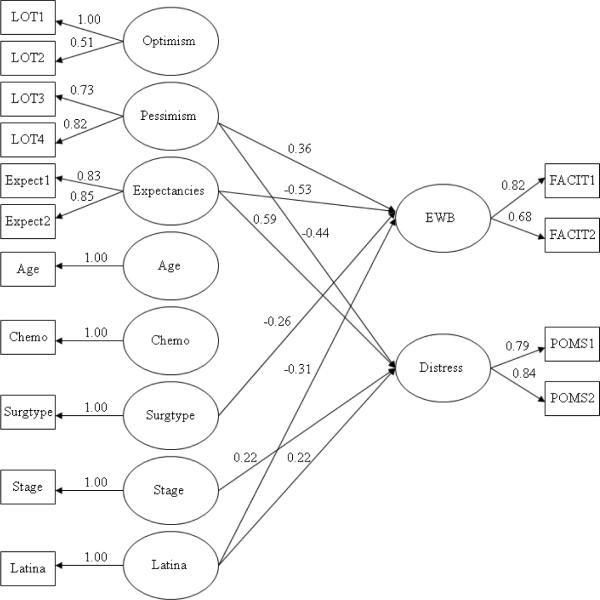
The removal of non-significant paths was the only modification necessary to fit the hypothesized model. The non-significant paths removed were: from Optimism, Age, and History of Chemotherapy to both EWB and Distress; Type of Surgery to Distress; Cancer Stage to EWB. Figure 2 illustrates the significant path coefficients for the structural model. The Goodness of Fit indices indicated that the hypothesized model in Figure 2 yielded a good fit to the data after all statistically non-significant paths were constrained to zero, FIML Chi-Square (80 d.f.) = 94.45, p = 0.14; RMSEA = 0.040 (90% C.I. 0.0, 0.070), p = 0.68. All measurement models were statistically significant. This model accounted for 65% of the variance in EWB and 69% of the variance in Distress.
Figure 2.
Final expectancy-based model for explaining distress and emotional-well being prior to radiotherapy
Notes. The model was a good fit to the data, FIML Chi-Square (80 d.f.) = 94.45, p = 0.14; RMSEA = 0.040 (90% C.I. 0.0, 0.070), p = 0.68. Optimism = high scores on the first factor of the LOT-R; Pessimism = high scores on the second factor of the LOT-R; Expectancies = response expectancies for distress; Age = chronological age; Chemo = history of chemotherapy; Surgtype = mastectomy (1), lumpectomy (0); Stage = stage 0 or I (0), stage II or III (1); Latina = Latina ethnicity (1), not of Latina ethnicity (0); EWB = emotional well-being as measured by the FACT-G (i.e., low distress); Distress = total mood disturbance as assessed by the POMS-SV.
Variables that significantly explained the variance in EWB were Pessimism, Response Expectancies, Type of Surgery, and Latina Ethnicity. The direction of the paths were such that those who had lower pessimism (high scores on Pessimism indicate low pessimism), lower response expectancies for distress, a lumpectomy and were not Latina had higher EWB (i.e., less emotional upset). Variables that significantly explained the variance in Distress were Pessimism, Response Expectancies, Cancer Stage and Latina Ethnicity. The direction of these paths indicated that those who were high in pessimism, had higher response expectancies for distress, had a higher cancer stage and were Latina reported greater distress.
Conclusion
The proposed expectancy-based model for predicting emotional well-being (EWB) and distress prior to the commencement of radiotherapy for breast cancer represented a good fit to the data. This model successfully explained two-thirds of the variance in EWB and Distress in women at this point in the treatment process. Specifically, the model indicated the following. First, women who were less pessimistic felt better emotionally at the start of radiotherapy. Second, women who expected to be more distressed throughout the course of their radiotherapy felt worse emotionally at the start of treatment. Third, more emotional upset (i.e., greater distress, less emotional well-being) was reported by Latina women, women with stage II or III cancer compared to those with stage 0 or I, and women who had a mastectomy (as opposed to a lumpectomy).
Pessimism was significantly related to EWB and Distress in breast cancer patients prior to radiotherapy whereas Optimism was not significantly related to either outcome. These results support the value of investigating Optimism and Pessimism as separate factors and are consistent with previous studies that have found that pessimism is a stronger predictor of distress than is optimism (Mroczek et al., 1993; Robinson-Whelen, et al., 1997; Zenger, 2010). Upon examination of responses to the specific items which comprise the optimism and pessimism subscales of the LOT, it appears that the pessimism subscale primarily focuses on the ability of the self to prevent negative outcomes (e.g., belief in the role of one's own ability) whereas the optimism subscale focuses on external explanations for positive outcomes (e.g., faith in a higher power; Sohl, Moyer, Lukin, & Knapp-Oliver, 2010). Consequently, our findings suggest that belief in the ability of the self to prevent future negative outcomes may be more important for protecting against negative emotions than is the belief that external forces will create positive outcomes. Thus interventions aiming to strengthen the belief in one's own ability to prevent negative outcomes may reduce the experience of anticipatory distress.
Additionally, it is noteworthy that specific response expectancies for how emotionally upset, depressed, stressed, or relaxed patients predicted they would be while undergoing radiotherapy were significantly related to both EWB and Distress even when controlling for dispositional expectancies (e.g., Pessimism). Previous research has found an effect of response expectancies for cancer treatment-related physical side effects (e.g., pain, nausea, fatigue) on these same side effects (Sohl, Schnur, & Montgomery, 2009) and of response expectancies for anxiety on fear and avoidance in various samples (Kirsch, 1997). It has also been documented that both breast cancer-related pre-surgical distress and specific response expectancies are distinctly predictive of post-surgical outcomes (e.g., pain, nausea, fatigue; Montgomery & Bovbjerg, 2004; Montgomery, Schnur, Erblich, Diefenbach, & Bovbjerg, 2010). However, the present study is the first, to our knowledge, to explore how response expectances for distress are associated with the EWB and distress experienced by breast cancer radiotherapy patients. Furthermore, the results from this study suggest that modifying response expectancies for distress would improve EWB and reduce distress experienced by women prior to radiotherapy. Future studies should investigate if response expectancies and distress prior to radiotherapy are related to distress experienced during the treatment as well as subsequent to the treatment.
Implications of the result that Latina ethnicity was associated with both less EWB and greater Distress are unclear. However, Latina ethnicity was also found to be associated with elevated distress in previous work (Carver, et al., 2006; Janz, 2009). A review exploring ethnicity and cancer outcomes concluded that there is rarely a direct association between ethnicity and outcomes (Meyerowitz, Richardson, Hudson, & Leedham, 1998). To fully understand the relationship between Latina ethnicity and anticipatory distress, the heterogeneity within participants classified as Latina would need to be explored further in a study that includes possible mediators such as income, knowledge, level of acculturation and cultural values (Janz, 2009; Meyerowitz et al., 1998; Sammarco, 2010).
Of the other demographic and medical indicators investigated in the present study (i.e., race, age, marital status, education, history of chemotherapy, surgery type, stage), type of surgery was found to have a significant influence on EWB and stage was associated with elevated distress such that mastectomy and higher stage were associated with worse emotional outcomes. Type of surgery (Schnur et al., 2008; Arndt, Stegmaier, Ziegler, & Brenner, 2008; Jim, Andrykowski, Munster, & Jacobsen, 2007) and stage (Weitzner et al., 1997) have previously been found to be significant predictors of distress in breast cancer-related procedures in some studies although these effects have not been demonstrated in other samples (Henselmans et al., 2010; Mosher et al., 2010; Moyer & Salovey, 1999). The present study supports findings that demographic and medical variables may predict distress. However, in the context of the inconsistent results found in the general literature, these relationships are also likely explained by mediating constructs (e.g., coping strategies, worry; Schnoll et al., 1998; Schnur et al., 2008).
Clinical implications include that women with stage II or III cancer, who have had a mastectomy, are Latina, are highly pessimistic, and/or expect to be distressed, may have elevated risk for experiencing distress prior to radiotherapy. Disseminating this information to clinicians who care directly for these women may encourage additional referrals to psychological support for those who are especially at risk for distress. In addition, future psychological interventions may screen for women who are likely to experience elevated distress using these medical, demographic, and psychological factors. The prevalence of distress in the current study, whereas 59% of women reported either no or little distress and 41% indicated more than a little distress, is consistent with the existing literature (Browall et al., 2008; Mose et al., 2001; Sollner, Maislinger, Konig, Devries, & Lukas, 2004). Although screening for distress would likely strengthen the size of effects found for intervention studies (Schneider et al., 2010), it may be important to address any level of distress present in anticipation of radiotherapy reduce subsequent distress and promote emotional well-being proactively.
Interventions to reduce pessimism and improve response expectancies for distress are also implied by the present results. The ability of an intervention to alter dispositional pessimism, traditionally considered to be a stable trait, is not certain. One intervention conducted in patients with breast cancer did find improved scores on the LOT-R for those who originally had low scores on this measure (Antoni et al., 2001). Therefore, it may be feasible to modify dispositional pessimism. Interventions (e.g., hypnosis) have been found to be successful in modifying response expectancies prior to other breast cancer-treatment-related procedures (Montgomery, Hallquist, Schnur, David, Silverstein, & Bovbjerg, 2010). Such interventions may also be effective if implemented prior to radiotherapy (Montgomery et al., 2007; Schnur, Kafer, Marcus, & Montgomery, 2008; Schnur et al., 2008).
Limitations and Future Directions
This study is not without its limitations. First, the cross-sectional design is not ideal for determining a causal relationship. This is the first empirical study to investigate indicators of general distress and EWB prior to radiotherapy for breast cancer and informs future prospective work to clarify the direction of these relationships. Second, a larger sample that would allow for more complex analyses would be ideal for further assessment of constructs that may mediate the influence of demographic and medical variables on Distress and EWB. In particular, Latina women comprised 20% of the sample. Larger samples of some of the subgroups represented here would be of interest. Thirdly, other stable constructs (e.g., neuroticism, trait anxiety) may have further explained the variance of Distress and EWB. However, to strengthen the power of our model and reduce multicollinearity, we decided to focus on the influence of cognitive expectancy factors. Additionally, although the present model did explain two-thirds of the variance in distress and EWB, only intrapsychic constructs were included (e.g., optimism, response expectancies). It is possible that interpersonal constructs (e.g., physician-patient relationship, social support) may contribute to the unexplained variance. Fourth, this study was restricted to external beam radiotherapy for breast cancer. It is not clear how the results will generalize to other cancer radiotherapy populations (e.g., prostate) or other types of radiotherapy (e.g., MammoSite).
Summary
In summary, pessimism, response expectancies for distress, higher cancer stage, having had a mastectomy and Latina ethnicity each contributed to explaining two-thirds of the variance in distress and EWB prior to radiotherapy for breast cancer. Thus, these are highly relevant constructs to consider in further research that aims to understand anticipatory distress in this population. The data provide a solid foundation for future prospective studies designed to determine the direction of causality between these variables. Clarifying the predictors of distress experienced in anticipation of radiotherapy will inform the development of interventions to address such predictors and ultimately improve breast cancer patients' quality of life.
Acknowledgements
This work was supported by the National Cancer Institute (5R25CA081137; R25CA122061; K07CA131473) and the American Cancer Society (#RSGPB-04-213-01-CPPB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. The authors would like to thank Ms. Bianca Love and Ms. Bari Scheckner for their invaluable assistance and all of the study participants for so graciously sharing their experiences.
References
- American Cancer Society . Cancer Facts and Figures 2009. American Cancer Society; Atlanta: 2009. [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, Yount SE. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20:20–33. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Arndt V, Stegmaier C, Ziegler H, Brenner H. Quality of life over 5 years in women with breast cancer after breast-conserving therapy versus mastectomy: a population-based study. Journal of Cancer Research & Clinical Oncology. 2008:1311–1318. doi: 10.1007/s00432-008-0418-y. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa KT. Examining the impact of socioeconomic status and socioecologic stress on physical and mental health quality of life among breast cancer survivors. Oncology Nursing Forum. 2009;36:79–88. doi: 10.1188/09.ONF.79-88. [DOI] [PubMed] [Google Scholar]
- Avis NE, Crawford S, Manuel J. Psychosocial problems among younger women with breast cancer. Psycho-Oncology. 2004;13:295–308. doi: 10.1002/pon.744. [DOI] [PubMed] [Google Scholar]
- Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. Journal of Clinical Oncology. 2005;23:3322–3330. doi: 10.1200/JCO.2005.05.130. [DOI] [PubMed] [Google Scholar]
- Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, Deasy M, Cobleigh M, Shimoto G. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. Journal of Clininical Oncology. 1997;15:974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- Broeckel JA, Jacobsen PB, Horton J, Balducci L, Lyman GH. Characteristics and correlates of fatigue after adjuvant chemotherapy for breast cancer. Journal of Clininical Oncology. 1998;16:1689–1696. doi: 10.1200/JCO.1998.16.5.1689. [DOI] [PubMed] [Google Scholar]
- Browall M, Ahlberg K, Karlsson P, Danielson E, Persson L, Gaston-Johannson F. Health-related quality of life during adjuvant treatment for breast cancer among postmenopausal women. European Journal of Oncology Nursing. 2008;12:180–189. doi: 10.1016/j.ejon.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudek R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 445–455. [Google Scholar]
- Bryant FB. Distinguishing hope and optimism: Two sides of a coin, or two separate coins? Journal of Social and Clinical Psychology. 2004;23:273–302. [Google Scholar]
- Carver CS, Pozo-Kaderman C, Harris SD, Noriega V, Scheier MF, Robinson DS, Ketchman A, Moffat FL, Jr., Clark KC. Optimism versus pessimism predicts the quality of women's adjustment to early stage breast cancer. Cancer. 1994;73:1213–1220. doi: 10.1002/1097-0142(19940215)73:4<1213::aid-cncr2820730415>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Carver CS, Smith RG, Antoni MH, Petronis VM, Weiss S, Derhagopian RP. Optimistic personality and psychosocial well-being during treatment predict psychosocial well-being among long-term survivors of breast cancer. Health Psychology. 2005;24:508–516. doi: 10.1037/0278-6133.24.5.508. [DOI] [PubMed] [Google Scholar]
- Carver CS, Smith RG, Petronis VM, Antoni MH. Quality of life among long-term survivors of breast cancer: different types of antecedents predict different classes of outcomes. Psycho-Oncology. 2006;15:749–758. doi: 10.1002/pon.1006. [DOI] [PubMed] [Google Scholar]
- Chang EC, Maydeu-Olivares A, D'Zurilla TJ. Optimism and pessimism as partially independent constructs: Relationship to positive and negative affectivity and psychological well-being. Personality and Individual Differences. 1997;23:433–440. [Google Scholar]
- Costanzo ES, Ryff CD, Singer BH. Psychosocial adjustment among cancer survivors: Findings from a National Survey of Health and Well-Being. Health Psychology. 2009;28:147–156. doi: 10.1037/a0013221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David D, Montgomery GH, Bovbjerg DH. Relations between coping responses and optimism-pessimism in predicting anticipatory psychological distress in surgical breast cancer patients. Personality and Individual Differences. 2006;40:203–213. doi: 10.1016/j.paid.2005.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLorenzo TA, Bovbjerg DH, Montgomery GH, Jacobsen PB, Valdimarsdottir H. The application of a shortened version of the profile of mood states in a sample of breast cancer chemotherapy patients. British Journal of Health Psychology. 1999;4:315–325. [Google Scholar]
- DiLorenzo TA, Jacobsen PB, Bovbjerg DH, Chang H, Hudis C, Sklarin N. Sources of anticipatory emotional distress in women receiving chemotherapy for breast cancer. Annals of Oncology. 1995;6:705–711. doi: 10.1093/oxfordjournals.annonc.a059288. [DOI] [PubMed] [Google Scholar]
- Epping-Jordan JE, Compas BE, Osowiecki DM, Oppedisano G, Gerhardt C, Primo K, Krag DN. Psychological adjustment in breast cancer: processes of emotional distress. Health Psychology. 1999;18:315–326. doi: 10.1037//0278-6133.18.4.315. [DOI] [PubMed] [Google Scholar]
- Glanz K, Lerman C. Psychosocial impact of breast cancer: A critical review. Annals of Behavioral Medicine. 1992;14:204–212. [Google Scholar]
- Hau K, Marsh HW. The use of item parcels in structural equation modeling: Non-normal data and small sample sizes. British Journal of Mathematical and Statistical Psychology. 2004;57:327–351. doi: 10.1111/j.2044-8317.2004.tb00142.x. [DOI] [PubMed] [Google Scholar]
- Henselmans I, Helgeson VS, Seltman H, De Vries J, Sanderman R, Ranchor AV. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychology. 2010;29:160–168. doi: 10.1037/a0017806. [DOI] [PubMed] [Google Scholar]
- Janz NK. Racial/ethnic differences in quality of life after diagnosis of breast cancer. Journal of Cancer Survivorship. 2009;3:212–222. doi: 10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jim H, Andrykowski M, Munster P, Jacobsen P. Physical symptoms/side effects during breast cancer treatment predict posttreatment distress. Annals of Behavioral Medicine. 2007;34:200–208. doi: 10.1007/BF02872674. [DOI] [PubMed] [Google Scholar]
- Joreskog K, Sorbom D. LISREL. Version 8.8 Scientific Software International, Inc.; Lincolnwood, IL: 2007. [Google Scholar]
- Kirsch I. Response expectancy theory and application: A decennial review. Applied & Preventive Psychology. 1997;6:69–79. [Google Scholar]
- Kirsch I, Mearns J, Catanzaro SJ. Mood-regulation expectancies as determinants of dysphoria in college students. Journal of Counseling Psychology. 1990;37:306–312. [Google Scholar]
- Knobf MT, Sun Y. A longitudinal study of symptoms and self-care activities in women treated with primary radiotherapy for breast cancer. Cancer Nursing. 2005;28:210–218. doi: 10.1097/00002820-200505000-00010. [DOI] [PubMed] [Google Scholar]
- Marshall GN, Wortman CB, Kusulas JW, Hervig LK, Vickers RR., Jr. Distinguishing optimism from pessimism: Relations to fundamental dimensions of mood and personality. Journal of Personality and Social Psychology. 1992;62:1067–1074. [Google Scholar]
- McNair D, Lorr M, Droppleman L. Profile of Mood States. EDITS/Educational and Industrial Testing, Inc.; San Diego: 1971. [Google Scholar]
- Meyerowitz BE, Richardson J, Hudson S, Leedham B. Ethnicity and cancer outcomes: Behavioral and psychosocial considerations. Psychological Bulletin. 1998;123:47–70. doi: 10.1037/0033-2909.123.1.47. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Bovbjerg DH. Presurgery distress and specific response expectancies predict postsurgery outcomes in surgery patients confronting breast cancer. Health Psychology. 2004;23:381–387. doi: 10.1037/0278-6133.23.4.381. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Bovbjerg DH, Schnur JB, David D, Goldfarb A, Weltz C, Schechter C, Graff-Zivin J, Tatrow K, Price DD, Silverstein J. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. Journal of the National Cancer Institute. 2007;99:1304–1312. doi: 10.1093/jnci/djm106. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, David D, Goldfarb AB, Silverstein JH, Weltz CR, Birk JS, Bovbjerg DH. Sources of anticipatory distress among breast surgery patients. Journal of Behavioral Medicine. 2003;26:153–164. doi: 10.1023/a:1023034706298. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Hallquist MN, Schnur JB, David D, Silverstein JH, Bovbjerg DH. Mediators of a brief hypnosis intervention to control side effects in breast surgery patients: Response expectancies and emotional distress. Journal of Consulting and Clinical Psychology. 2010;78:80–88. doi: 10.1037/a0017392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery GH, Schnur JB, Erblich J, Diefenbach MA, Bovbjerg DH. Presurgery psychological factors predict pain, nausea, and fatigue one week after breast cancer surgery. Journal of Pain and Symptom Management. 2010;39:1043–1052. doi: 10.1016/j.jpainsymman.2009.11.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mose S, Budischewski KM, Rahn AN, Zander-Heinz AC, Bormeth S, Bottcher HD. Influence of irradiation on therapy-associated psychological distress in breast carcinoma patients. International Journal of Radiation Oncology Biology Physics. 2001;51:1328–1335. doi: 10.1016/s0360-3016(01)01711-4. [DOI] [PubMed] [Google Scholar]
- Mosher CE, DuHamel KN, Egert J, Smith MY. Self-efficacy for coping with cancer in a multiethnic sample of breast cancer patients: associations with barriers to pain management and distress. The Clinical Journal of Pain. 2010;26:227–234. doi: 10.1097/AJP.0b013e3181bed0e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer A, Salovey P. Psychosocial sequelae of breast cancer and its treatment. Annals of Behavorial Medicine. 1996;18:110–125. doi: 10.1007/BF02909583. [DOI] [PubMed] [Google Scholar]
- Moyer A, Salovey P. Predictors of social support and psychological distress in women with breast cancer. Journal of Health Psychology. 1999;4:177–191. doi: 10.1177/135910539900400212. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A, Aldwin CM, Ozer DJ, Bossé R. Construct validation of optimism and pessimism in older men: Findings from the normative aging study. Health Psychology. 1993;12:406–409. doi: 10.1037//0278-6133.12.5.406. [DOI] [PubMed] [Google Scholar]
- Ozalp G, Sarioglu R, Tuncel G, Aslan K, Kadiogullari N. Preoperative emotional states in patients with breast cancer and postoperative pain. Acta Anaesthesiologica Scandinavica. 2003;47:26–29. doi: 10.1034/j.1399-6576.2003.470105.x. [DOI] [PubMed] [Google Scholar]
- Robinson-Whelen S, Kim C, MacCallum RC, Kiecolt-Glaser JK. Distinguishing optimisim from pessimism in older adults: is it more important to be optimistic or not to be pessimistic? Journal of Personality and Social Psychology. 1997;73:1345–1353. doi: 10.1037//0022-3514.73.6.1345. [DOI] [PubMed] [Google Scholar]
- Sammarco A. Quality of life, social support, and uncertainty among Latina and Caucasian breast cancer survivors: A comparative study. Oncology Nursing Forum. 2010;37:93–99. doi: 10.1188/10.ONF.93-99. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS. Optimism, coping and health: Assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Schneider S, Moyer A, Knapp-Oliver SK, Sohl SJ, Cannella D, Targhetta V. Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. Journal of Behavioral Medicine. 2010;33:1–14. doi: 10.1007/s10865-009-9227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnoll RA, Harlow LL, Stolback LL, Brandt U. A structural model of the relationships among stage of disease, age, coping, and psychological adjustment in women with breast cancer. Psycho-Oncology. 1998;7:69–77. doi: 10.1002/(SICI)1099-1611(199803/04)7:2<69::AID-PON286>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Bovbjerg DH, David D, Tatrow K, Goldfarb AB, Silverstein JH, Weltz CR, Montgomery GH. Hypnosis decreases presurgical distress in excisional breast biopsy patients. Anesthesia and Analgesia. 2008;106:440–444. doi: 10.1213/ane.0b013e31815edb13. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Kafer I, Marcus C, Montgomery GH. Hypnosis to manage distress related to medical procedures: A meta-analysis. Contemporary Hypnosis. 2008;25:114–128. doi: 10.1002/ch.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnur JB, Montgomery GH, Hallquist MN, Goldfarb AB, Silverstein JH, Weltz CR, Kowalski AV, Bovbjerg DH. Anticipatory psychological distress in women scheduled for diagnostic and curative breast cancer surgery. International Journal of Behavioral Medicine. 2008;15:21–28. doi: 10.1007/BF03003070. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Ouellette SC, Bovbjerg DH, Montgomery GH. Breast cancer patients' experience of external-beam radiotherapy. Qualitative Health Research. 2009;19:668–676. doi: 10.1177/1049732309334097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnur JB, Ouellette SC, DiLorenzo TA, Green S, Montgomery GH. Qualitative analysis of skin toxicity among breast cancer radiotherapy patients. Psycho-Oncology. 2010 doi: 10.1002/pon.1734. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schootman M, Deshpande AD, Pruitt SL, Aft R, Jeffe DB. National estimates of racial disparities in health status and behavioral risk factors among long-term cancer survivors and non-cancer controls. Cancer Causes and Control. 2010;21:1387–1395. doi: 10.1007/s10552-010-9566-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shacham S. A shortened version of the Profile of Mood States. Journal of Personality Assessment. 1983;47:305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- Sohl SJ, Moyer A, Lukin K, Knapp-Oliver SK. Why are optimists optimistic? Individual Differences Research. 2010 Ahead of print. [PMC free article] [PubMed] [Google Scholar]
- Sohl S, Schnur J, Montgomery G. A Meta-Analysis of the Relationship between response expectancies and cancer-rreatment-related side effects. Journal of Pain and Symptom Management. 2009;38:775–784. doi: 10.1016/j.jpainsymman.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sollner W, Maislinger S, Konig A, Devries A, Lukas P. Providing psychosocial support for breast cancer patients based on screening for distress within a consultation-liaison service. Psycho-Oncology. 2004;13:893–897. doi: 10.1002/pon.867. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Snider PR. Coping with a breast cancer diagnosis: A prospective study. Health Psychology. 1993;12:16–23. doi: 10.1037//0278-6133.12.1.16. [DOI] [PubMed] [Google Scholar]
- Stiegelis HE, Ranchor AV, Sanderman R. Psychological functioning in cancer patients treated with radiotherapy. Patient Education and Counseling. 2004;52:131–141. doi: 10.1016/s0738-3991(03)00021-1. [DOI] [PubMed] [Google Scholar]
- Sucala ML, Szentagotai-Tatar A. Optimism, pessimism and negative mood regulation expectancies in cancer patients. Journal of Cognitive and Behavioral Psychotherapies. 2010;10:13–24. [Google Scholar]
- Vinh-Hung V, Verschraegen C. Breast-conserving surgery with or without radiotherapy: pooled-analysis for risks of ipsilateral breast tumor recurrence and mortality. Journal of the National Cancer Instititute. 2004;96:115–121. doi: 10.1093/jnci/djh013. [DOI] [PubMed] [Google Scholar]
- Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Quality of Life Outcomes. 2003;1:79. doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzner MA, Meyers CA, Stuebing KK, Saleeba AK. Relationship between quality of life and mood in long-term survivors of breast cancer treated with mastectomy. Supportive Care in Cancer. 1997;5:241–248. doi: 10.1007/s005200050067. [DOI] [PubMed] [Google Scholar]
- Wengstrom Y, Haggmark C, Strander H, Forsberg C. Perceived symptoms and quality of life in women with breast cancer receiving radiation therapy. European Journal of Oncology Nursing. 2000;4:78–88. doi: 10.1054/ejon.1999.0052. [DOI] [PubMed] [Google Scholar]
- Zenger M, Glaesmer H, Hockel M, Hinz A. Pessimism predicts anxiety, depression and quality of life in female cancer patients. Japanese Journal of Clinical Oncology. 2010 doi: 10.1093/jjco/hyq168. Ahead of print. [DOI] [PubMed] [Google Scholar]