Abstract
Objectives
The current study examined the contributions of psychosocial resource and risk factors to the association between socioeconomic status (SES) and metabolic syndrome (MetSyn) risk, in a randomly selected community cohort of 304 middle-aged (40–65 years old) Mexican-American women, a population at elevated cardiometabolic risk.
Methods
Participants underwent a clinical exam and completed measures of demographic factors and psychosocial resource (i.e., personal and social resources) and risk (i.e., negative emotions and cognitions) variables. Confirmatory factor analysis (CFA) and structural equation models (SEMs) were performed in the total sample and in more and less US-acculturated women (defined by language preference) separately.
Results
CFAs revealed single latent constructs for SES (i.e., income, education) and psychosocial resources/risk. For the MetSyn, a 3-factor solution was identified, with blood pressure (systolic and diastolic), lipids (high-density lipoprotein cholesterol and triglycerides), and metabolic variables (glucose and waist circumference) forming separate factors. SEMs showed that an indirect effects model with SES relating to MetSyn factors through psychosocial resources/risk provided a reasonable descriptive and statistical fit in the full and more acculturated sample (RMSEA and SRMR < .08); fit in the less acculturated sample was marginal according to RMSEA =.09. A significant mediated path from low SES to higher waist circumference/fasting glucose via lower psychosocial resources/higher psychosocial risk was identified in the overall and more acculturated samples (p < .05).
Conclusions
In this cohort of healthy, middle-aged Mexican-American women, contributions of psychosocial factors to SES-MetSyn associations were limited to the core underlying metabolic mechanisms, and to more US-acculturated women.
Keywords: Hispanic, Metabolic Syndrome, Psychosocial, Risk Factors, Socioeconomic Status
Low socioeconomic status (SES) and ethnic minority groups are disproportionately vulnerable to type 2 diabetes (Karlamangla, Merkin, Crimmins, & Seeman, 2010) and cardiovascular diseases (CVD; Gonzalez, Rodriguez, & Calero, 1998). In particular, Latinos, the largest and fastest growing US ethnic minority group, and especially those of Mexican-descent, have high rates of cardiometabolic disorders relative to non-Latino Whites (Ervin, 2009; Rojas et al., 2010). Studies contrasting CVD prevalence rates in Latinos and non-Latino Whites have produced mixed findings, and this is an area of ongoing research.
The “metabolic syndrome” (MetSyn) may represent an intermediate stage of risk linking SES with more distal clinical endpoints. The MetSyn is typically defined as the presence of at least three of the following: elevated central adiposity (i.e., large waist circumference), hypertriglyceridemia, reduced high-density lipoprotein cholesterol (HDL-c), elevated blood pressure (BP), and hyperglycemia (Alberti et al., 2009). Abdominal obesity and insulin resistance represent the central underlying physiological mechanisms (Grundy, 2006). Although controversy about its definition and clinical utility is ongoing, the MetSyn predicts markedly elevated risk for incident type 2 diabetes and CVD (Ford, 2005; Gami et al., 2007) and diagnosis can facilitate early interventions targeting lifestyle factors.
Low SES has been associated with higher risk for the MetSyn and its components, with some studies demonstrating steeper gradients in women than in men (for a review, see Kavanagh et al., 2010). The origins of this association are complex and may include SES-related differences in healthcare access, lifestyle factors, physiological stress pathways, and psychosocial functioning. In the latter regard, low SES individuals are believed to display a high-risk psychosocial profile characterized by elevated risk factors (e.g., stress, psychological distress) and reduced resources (e.g., social support, optimism; Gallo & Matthews, 2003; Myers, 2009). In turn, some research links psychosocial factors such as emotional distress, chronic stress, and low social support with the MetSyn (Goldbacher & Matthews, 2007), and a large body of evidence supports their associations with related clinical outcomes, such as CVD (Everson-Rose & Lewis, 2005). Thus, there is a great deal of indirect support for the idea that psychosocial factors contribute to SES-gradients in the MetSyn and related outcomes. However, few studies have directly tested these associations (Matthews, Gallo, & Taylor, 2010), and some show support for psychosocial contributions to SES-MetSyn associations (e.g., Lehman, Taylor, Kiefe, & Seeman, 2005; Matthews, Räikkönen, Gallo, & Kuller, 2008), whereas others identify little evidence that psychosocial variables help explain these relationships (Prescott, Godtfredsen, Osler, Schnohr, & Barefoot, 2007).
It is also notable that limited research to date has focused on psychosocial factors in Latino health or, in particular, on the extent to which such variables contribute to SES-health disparities in Latinos (Gallo, Penedo, Espinosa de los Monteros, & Arguelles, 2009). At the same time, at least some research suggests that SES gradients in cardiometabolic risk are flattened, or inconsistent across Latino subgroups defined by ancestry or nativity (Karlamangla et al., 2010; Kimbro, Bzostek, Goldman, & Rodriguez, 2008). Moreover, it has been hypothesized that social and cultural resources might help explain why, on the whole, Latinos show increased longevity relative to other ethnic groups (e.g., Arias, Eschbach, Schauman, Backlund, & Sorlie, 2010) despite high levels of risk factors including low SES and poor healthcare access. In the only study (to our knowledge) that explored psychosocial factors in the association between SES and MetSyn risk in a Mexican-American sample, psychosocial resources contributed to the relationship between low SES and elevated central adiposity, but not other MetSyn elements (Gallo, Espinosa de los Monteros, Ferent, Urbina, & Talavera, 2007).
The current study examined psychosocial resource and risk variables as possible mechanisms underlying the association of SES with MetSyn risk in a community sample of middle-aged Mexican-American women. Following prior studies suggesting that in Latinos, socioeconomic gradients may vary by nativity or acculturation (Gallo Espinosa de los Monteros et al., 2009; Kimbro, et al., 2008), analyses were also conducted stratified by acculturation level, as defined by language preference. We predicted that women with lower SES and lower psychosocial resources/higher risk would display greater cardiometabolic risk, and that psychosocial factors would contribute to the association between SES and cardiometabolic risk.
Methods
Sample and Recruitment
The current study is part of a larger investigation of sociocultural factors in cardiometabolic risk (i.e., “Nuestra Salud,” or Our Health) in healthy, middle-aged Mexican-American women from communities near the US-Mexico border in San Diego County. Participants were randomly recruited using telephone and mail procedures, with stratification according to SES to ensure representation of diverse social status levels. Women were screened by telephone, and those who were aged 40–65 years, Mexican-American, literate, not pregnant, and free of chronic health problems (i.e., CVD, diabetes, liver and kidney diseases, chronic inflammatory conditions, etc.) and medications with autonomic effects (e.g., stimulants, steroids, major tranquilizers) were eligible. In total, 656 women were screened, 363 (55.3% of those screened) were eligible, and 321 (88.4% of those eligible) agreed to participate. The current study includes 304 women who completed the psychosocial assessment and physical exams.
Procedures
Assessments were conducted during two consecutive home visits, by trained, bilingual research technicians. Self-report measures of sociodemographic and psychosocial characteristics were administered in the participant’s preferred language, and a physical exam with venous blood draw was performed following an overnight fast. The San Diego State University and the University of California, San Diego Institutional Review Boards approved all study procedures and all participants provided written informed consent. (For a detailed description of methods, see: Gallo, Jiménez, Shivpuri, Espinosa de Los Monteros, & Mills, 2011).
Metabolic Syndrome
Blood pressure and waist circumference were assessed using a standardized protocol based on published guidelines. Assays for lipids (HDL-c and triglycerides) and plasma glucose were conducted by Quest Diagnostics, West Hills, CA laboratories, which adheres to guidelines set forth by the College of American Pathologists (Neeley, 1972; Warnick, 2000). Although a single construct is believed to underlie the MetSyn, studies using exploratory and confirmatory factor analysis (i.e., EFA and CFA) have shown that the MetSyn comprises multiple factors (e.g., Ferguson, Funkhouser, & Roseman, 2010). Accordingly, the current study tested several measurement models as described in detail below. Because participants were selected to be healthy, continuous representations of risk factors were considered optimal.
Socioeconomic status
Self-reported education and household income were used to represent SES. Educational attainment was recoded into six categories for analysis; total monthly household income was assessed on an ordinal scale in $500 increments.
Psychosocial Resource and Risk Variables
Participants completed a series of measures evaluating inter and intrapersonal resource factors. The six-item Life Engagement Test (LET; Scheier et al., 2006) was used to examine purposeful engagement in valued life activities. Self-esteem was assessed with the six-item version of Rosenberg’s Self-Esteem Scale (Simmons, Rosenberg, & Rosenberg, 1973). Two of the six items showed no variance in the present study, and were excluded from the scale to improve its psychometric properties. An abbreviated version of the Medical Outcomes Study Support Scale (Sherbourne & Stewart, 1991) from the Women’s Health Initiative study (Matthews et al., 1997) evaluated perceived social support. Pessimism was assessed using three items from the Life Orientation Test—Revised (LOT-R; Scheier, Carver, & Bridges, 1994). We only examined the negatively worded items because, consistent with prior studies, we found that the scale comprised two factors (Kubzansky, Kubzansky, & Maselko, 2004), and that SES was linked to “pessimism” but not “optimism” items (Gallo, et al., 2007).
To evaluate psychosocial risk, participants completed measures assessing negative cognitive-emotional factors.1 Anxiety was assessed with the 10-item Trait Anxiety Inventory (Spielberger, Sydeman, Owen, & Marsh, 1999). Depression was assessed with the 20-item Center for Epidemiological Studies-Depression Scale Revised (CES-DR; Eaton, Muntaner, Smith, Tien, & Ybarra, 1999). Cynical hostility was measured using a six-item version (Janicki-Deverts, Cohen, & Doyle, 2010) of the Cook-Medley cynicism subscale (Barefoot, Dodge, Peterson, Dahlstrom, & Williams, 1989). Loneliness (Hughes, Waite, Hawkley, & Cacioppo, 2004) and hopelessness (Everson et al., 1996) were assessed with three and two-item scales, respectively, that have been linked with CVD in prior research. Analyses of internal consistency revealed adequate reliability across most scales (αs = 0.72 to 0.92 for the total sample). For three of the shorter scales (hopelessness, self-esteem, and pessimism), reliability was relatively low at α= 0.64, 0.55, and 0.62, respectively.
Health-Related Covariates and Other Demographic Variables
Analyses controlled for age (in years) and use of medications potentially relevant to MetSyn indicators [i.e., a composite variable reflecting use of lipid-lowering (n = 7), BP-lowering (n = 2), and glucose-regulating (n = 1) medications2]. Participants also provided information about employment status, insurance coverage, marital status, and country of origin. Language of the survey was included as a proxy for acculturation, with English indicating greater acculturation to US mainstream culture. Specifically, interviewers inquired as to language of preference for study materials (surveys, fasting instructions, etc.), and the participant’s choice was recorded for analyses. Although providing a limited representation of the complex, multi-dimensional acculturation process (Thomson & Hoffman-Goetz, 2009), language is a reliable indicator that correlates well with scores on more elaborate scales (Cruz, Marshall, Bowling, & Villaveces, 2008),
Statistical Analyses
Descriptive statistics were calculated and between-group comparisons evaluated differences between the acculturation subgroups on sociodemographic and target study variables. Confirmatory factor analyses were then conducted to evaluate the measurement models for each latent variable. For MetSyn, we tested three models based on prior research: 1) a single-factor model with systolic and diastolic blood pressure (SBP, DBP), triglycerides, HDL-c, glucose, and waist as indicators; 2) a two-factor model with SBP and DBP, and triglycerides, glucose, HDL-c, and waist, loading on separate factors and 3) a three-factor model, with SBP and DBP, triglycerides and HDL-c, and waist and glucose, representing separate factors. Single-factor CFAs were specified for the latent variables representing psychosocial resources (life engagement, self-esteem, social support, and low pessimism) and risk (anxiety, depression, hopelessness, hostility, and loneliness). Initial, item-level multigroup CFA models supported the metric invariance of each indicator (measure) across language subgroups. The SES latent variable comprised two observed variables (income, education), and was evaluated in a broader CFA model. Subsequently, two competing structural equation models (SEMs) were tested. Model 1 was the indirect effects only model, i.e., with structural paths from SES to MetSyn latent factors through psychosocial constructs. Building on Model 1, Model 2 added direct structural paths from SES to the MetSyn. Age and medication usage were specified as covariates for the MetSyn latent variables. All measurement models and SEMs were tested in the overall sample and separately in each acculturation subgroup.
The maximum likelihood robust (MLR) estimation procedure employed by MPlus (Muthén & Muthén, 2006) was used to estimate model parameters. This procedure provides a chi-square test statistic [Yuan-Bentler T2 (Y-Bχ2 for current purposes); Yuan & Bentler, 2000); and standard errors that are adjusted for multivariate non-normality and missing data. Two descriptive fit indexes have been recommended (Bentler, 2007): (a) the root mean square error of approximation (RMSEA) and (b) the standardized root mean square residual (SRMR). Both parameters represent descriptive fit indices of overall model fit, with values .05 or less indicative of good fit and .08 or less indicative of acceptable fit. Competing (nested) models can be compared statistically using the chi-square difference test (ΔY-Bχ2) and descriptively using indices such as the RMSEA and SRMR.
Minimal missing data was evident; 95% of participants had complete data, and bivariate statistical analyses revealed no statistically significant differences in target study variables for those with missing versus complete data (all ps > .05).
Results
Descriptive Statistics
Table 1 shows descriptive statistics for all study variables for the entire sample and each acculturation subgroup. On average, women were 49.76 years old (SD = 6.58). Relative to less acculturated women, more acculturated women were more likely to be employed, have health coverage, and to have been born in the US (all ps < .001). In addition, group mean differences reached or approached statistical significance for education (p < .001), income (p < .001), hostility (p = .05), support (p = .001), and HDL-c (p = .02), with the more US-acculturated group having significantly higher mean values for all indicators, with the exception of hostility.
Table 1.
Descriptive statistics for sociodemographic variables, metabolic syndrome components, and psychosocial risk and resource factors across the entire sample, and within each acculturation subgroup
| Overalla N (%) |
More- Acculturatedb N (%) |
Less- Acculturatedc N (%) |
P-value | |
|---|---|---|---|---|
| Educational attainment | < .001 | |||
| < High school diploma/GED | 105 (34.5) | 12 (9.6) | 93 (52.0) | |
| ≥ High school diploma/GED | 199 (65.5) | 113 (90.4) | 86 (8.0) | |
| Household monthly incomed | < .001 | |||
| <$3000 | 124 (41.6) | 26 (21.1) | 98 (55.7) | |
| ≥$3000 | 175 (58.4) | 97 (78.9) | 49 (44.3) | |
| Working full or part time | 197 (64.8) | 96 (76.8) | 101 (56.4) | < .001 |
| Health Coverage | 217 (71.4) | 109 (87.2) | 108 (60.3) | < .001 |
| Married or cohabitating | 221 (72.7) | 92 (73.6) | 129 (72.1) | 0.80 |
| Born in the United States | 76 (25.0) | 68 (54.4) | 8 (4.5) | < .001 |
| M (SD) | M (SD) | M (SD) | P-value | |
| Metabolic Syndrome | ||||
| DBP (mmHg) | 73.08 (8.50) | 73.46 (8.86) | 72.80 (8.25) | 0.51 |
| SBP (mmHg) | 117.45 (14.45) | 116.12 (13.60) | 118.37 (14.99) | 0.18 |
| Waist Circumference (cm) | 87.91 (12.73) | 86.65 (13.45) | 88.79 (12.17) | 0.15 |
| Plasma Glucose (mg/dl) | 90.32 (23.35) | 91.26 (30.84) | 89.66 (16.26) | 0.56 |
| HDL-c (mg/dl) | 57.00 (15.33) | 59.54 (16.16) | 55.22 (14.51) | 0.02 |
| Serum Triglycerides (mg/dl) | 133.17 (67.69) | 128.07 (68.66) | 136.73 (66.97) | 0.27 |
| Psychosocial Resource Factors | ||||
| Life Engagement | 21.23 (2.80) | 21.04 (2.52) | 21.36 (2.98) | 0.33 |
| Self-Esteem | 5.68 (0.68) | 5.68 (0.66) | 5.68 (0.71) | 0.97 |
| Social Support | 19.59 (6.68) | 21.13 (6.10) | 18.51 (6.86) | 0.001 |
| (Low) Pessimism | 5.71 (1.85) | 5.53 (1.60) | 5.83 (2.00) | 0.17 |
| Psychosocial Risk Factors | ||||
| Anxiety | 16.33 (4.76) | 16.02 (4.48) | 16.54 (4.96) | 0.35 |
| Depression | 28.01 (10.75) | 26.94 (9.18) | 28.77 (11.70) | 0.15 |
| Hopelessness | 3.43 (1.41) | 3.34 (1.33) | 3.49 (1.46) | 0.39 |
| Hostility | 2.32 (1.82) | 2.08 (1.72) | 2.49 (1.86) | 0.05 |
| Loneliness | 1.90 (2.07) | 1.78 (2.01) | 1.99 (2.10) | 0.40 |
Note. DBP = Diastolic blood pressure. SBP = Systolic blood pressure. HDL-c = High-density lipoprotein cholesterol.
n = 304.
n = 125.
n = 179.
Five missing data points; income and education categories were collapsed for descriptive purposes. eOne missing data point.
One missing data point.
Model Testing
Measurement Models and Interfactor Correlations
The one-factor model for MetSyn did not fit well in the overall sample or in either acculturation group (RMSEA and SRMR all >.08). The fit for the two-factor model was acceptable in the overall sample and the more-acculturated subgroup according to the SRMR (both <.08), but did not fit well in less acculturated women (RMSEA and SRMR both >.08). Fit for the three-factor model was more consistent across samples. Acceptable model fit was established for the more acculturated sample according to both descriptive fit indices, Y-Bχ2(df=6) = 10.24, p = .11, RMSEA = .075, SRMR = .04. The SRMR indicated acceptable model fit in both the overall sample, Y-Bχ2(df=6) = 24.20, p < .05, RMSEA = .10, SRMR = .04, and in the less-acculturated subgroup, Y-Bχ2(df=6) = 19.14, p < .05, RMSEA = .11, SRMR = .05. In nested model comparisons, the three-factor model fit statistically (ΔY-Bχ2s(2) = 15.15 to 28.89; all ps < .001) and descriptively (ΔRMSEA and ΔSRMR > .02) better than the two-factor model. Thus, the three-factor model was used in SEM analyses. The factor loadings for each MetSyn latent variable are presented in Table 2. The magnitudes of these loadings were consistent across samples with the exception of the loading for waist, which was significantly smaller in magnitude in less acculturated women (p < .05). Interfactor correlations among the three MetSyn latent variables were positive and significant across samples, ranging from 0.27 to 0.85 (see Table 2).
Table 2.
Factor loadings for the final measurement models and associations among latent variables for the overall sample/more-acculturated sample (English speaking)/less acculturated sample (Spanish-speaking).
| Variables | SES | Psychosocial Resources/ Risk |
MetSyn1 | MetSyn2 | MetSyn3 |
|---|---|---|---|---|---|
| Factor Loadings | |||||
| Income | 1.00/1.00/1.00 | ||||
| Education | .71/.48/.76 | ||||
| Life engagement | 1.00/1.00/1.00 | ||||
| Self-esteem | .60/.61/.60 | ||||
| Social support | .46/.53/.42 | ||||
| (Low)Pessimism | −.41/−.55/−.34 | ||||
| Anxiety | −.82/−.73/−.85 | ||||
| Depression | −.67/−.44/−.76 | ||||
| Hopelessness | −.47/−.44/−.51 | ||||
| Hostility | −.40/−.42/−.39 | ||||
| Loneliness | −.68/−.65/−.69 | ||||
| DBP | 1.00/1.00/1.00 | ||||
| SBP | .82/.95/.76 | ||||
| Triglycerides | 1.00/1.00/1.00 | ||||
| HDL-c | −.66/−.68/−.63 | ||||
| Glucose | 1.00/1.00/1.00 | ||||
| Waist | .69/.93/.40 | ||||
| Age-controlled correlations among latent factors (r) | |||||
| SES | --- | ||||
| Psychosocial Resources/Risk | .43/.44/.43 | --- | |||
| MetSyn1 | −.09/−.22/−.03 | .01/−.16*/.11 | --- | ||
| MetSyn2 | −.19/−.19/−.14 | −.09/−.14/−.04 | .34/.43/.27 | --- | |
| MetSyn3 | −.21/−.25/−.17 | −.08/−.22/.02 | .70/.70/.70 | .82/.85/.78 | --- |
Notes. DBP = diastolic blood pressure. HDL-c = high-density lipoprotein cholesterol. SBP = systolic blood pressure. SES = socioeconomic status. MetSyn = metabolic syndrome. Statistically significant correlations (p < .05) are bold and marginally significant correlations (p < .10) are underlined.
Significant difference (p < .05) in strength of bivariate association between acculturation groups.
Next, CFA models were fit for the psychosocial risk and resource latent variables individually and simultaneously. Although all single-factor CFA models fit well (all RMSEA and SRMR values < .05), the interfactor correlations between the risk and resource latent variables were extremely high (rs > .80 across samples), suggesting collinearity. Accordingly, a more parsimonious single factor psychosocial resources/risk latent variable was tested and fit adequately in the overall sample, Y-Bχ2(df=27) = 121.24, p< .05, RMSEA = .080, SRMR = .071. Likewise, stratified analyses showed an acceptable fit in the more, Y-Bχ2(df=27) = 71.18, p < .05, RMSEA = .082, SRMR = .075, and less acculturated subgroups, Y-Bχ2(df=27) = 85.65, p < .05, RMSEA = .096, SRMR = .080. All factor loadings were statistically significant, with absolute values ranging from 0.34 to 0.85, as shown in Table 2. To evaluate correlations among the latent factors, a five-factor CFA was conducted. As shown in Table 2, SES was significantly and negatively associated with MetSyn1 in the more acculturated sample, with MetSyn2 in the overall and more acculturated sample (the association approached statistical significance in the less acculturated sample), and with MetSyn3 the overall sample and both acculturation subgroups. Higher SES was associated with higher psychosocial resources/lower risk across all samples, and related significantly and negatively to MetSyn3 in the more acculturated sample.
Structural Equation Models
Tests of the two SEMs showed that Model 1 (indirect effects only) fit reasonably well in the overall sample (Y-Bχ2(df=136) = 378.56, p < .05, RMSEA = .077, SRMR = .063) and in both acculturation subgroups (more acculturated, Y-Bχ2(df=136) = 230.65, p < .05, RMSEA = .075, SRMR = .073; less acculturated, Y-Bχ2(df=136) = 345.80, p < .05, RMSEA = .093, SRMR = .074); however, fit according to the RMSEA was marginal in the less acculturated subgroup. Model 2 (indirect and direct effects) fit statistically better than Model 1 in the overall sample (ΔY-Bχ2(3) = 12.80, p = .005) and in the less acculturated subgroup (ΔY-Bχ2(3) = 10.38, p = .015), but there was no difference in descriptive fit between these two models in either sample (ΔRMSEA = .000 –.001, ΔSRMR = .003 – .004). In the more acculturated subgroup, Models 1 and 2 did not demonstrate a statistical (ΔY-Bχ2(3) = 2.03, p = .57) or descriptive (ΔRMSEA = .001, ΔSRMR = .002) difference in fit. Emphasizing descriptive fit, the more parsimonious Model 1 was determined to be the “better-fitting” model.
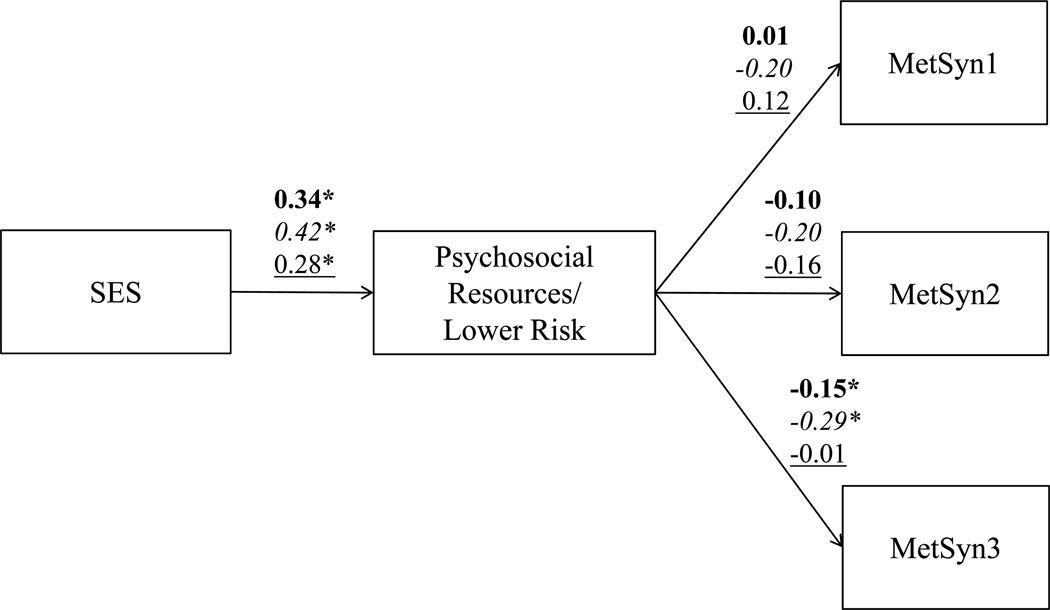
Standardized structural/path coefficients for Model 1 are presented in Figure 1. Higher SES was significantly related to greater psychosocial resources/lower risk in all three samples (R2overall = .12, R2English = .18, R2Spanish = .10). Greater psychosocial resources/lower risk related to lower levels on the MetSyn3 latent variable (i.e., waist and fasting glucose) in the overall (R2overall = .04) and more acculturated subgroups (R2English = .08). Because the compound paths making up the mediated effect were statistically significant in the overall sample and more acculturated subgroup, MacKinnon's asymmetric confidence interval (MacKinnon, Fritz, Williams, & Lockwood, 2007) was calculated to determine if the mediated effect was statistically significant in these groups. Significant mediated effects were found for the overall sample (95% asymmetric CI = −0.11 to −0.01) and the more acculturated group (95% asymmetric CI = −0.07 to −0.02). Finally, to determine whether the compound structural paths that composed the mediated paths from SES to MetSyn3 via psychosocial resources/risk differed as a function of acculturation level, two single degree of freedom ΔY-B χ2 tests were conducted. No statistically significant difference was found for the structural/path coefficient from SES to psychosocial resources/risk (p > .05); however, a statistically significant difference was observed for the structural/path coefficient from psychosocial resources/risk to MetSyn3 (p = .03), suggesting a stronger relationship for the more acculturated group.
Figure 1.
Results of analyses investigating the indirect pathways from SES to MetSyn 1 (systolic and diastolic blood pressure), MetSyn 2 (serum triglycerides and high-density lipoprotein cholesterol), and MetSyn 3 (plasma glucose and waist circumference) via the psychosocial resources/risk latent variable. Standardized structural/path coefficients represent overall sample, more US acculturated (English speaking), less US acculturated (Spanish speaking). Analyses control for age (in years) and use of medications potentially relevant to MetSyn indicators. *p < .05.
Discussion
The limited research examining psychosocial influences in the MetSyn has produced mixed results (Goldbacher & Matthews, 2007), and few studies have examined psychosocial contributions to SES-MetSyn associations (Matthews et al., 2010) or explored psychosocial pathways in SES-health gradients in Latinos (Gallo, Penedo et al., 2009). The current study examined psychosocial resource and risk factors as mediating mechanisms connecting SES with the MetSyn in middle-aged Mexican-American women. The contribution of psychosocial factors was limited to central metabolic physiological pathways in the MetSyn (i.e., glucose regulation/abdominal obesity), and to more US-acculturated women only. These results are consistent with other studies showing that the origins of MetSyn are multifactorial.
As predicted, single factors were found to underlie indicators of SES, psychosocial resources, and psychosocial risk factors. However, the resource and risk latent factors were highly correlated, suggesting that in the current sample, they formed two poles of a single dimension, rather than representing distinct constructs. A unitary latent construct approach is supported by research suggesting dynamic and reciprocal associations between cognitive-emotional factors and inter and intrapersonal resources (e.g., Smith, Glazer, Ruiz, & Gallo, 2004). Moreover, these variables are purported to affect cardiometabolic health through similar bio-behavioral pathways (Krantz & McCeney, 2002) and may share common environmental and neurobiological origins.
The prediction that MetSyn components would form a unified representation of cardiometabolic risk was not supported. Rather, a three-factor solution comprising blood pressure (SBP, DBP), lipids (HDL-c and triglycerides), and metabolic factors (fasting glucose/waist circumference) was identified. Further, model fit was least optimal in the less acculturated group, and the factor loading for waist circumference was significantly lower in this subgroup relative to more acculturated women. Previous research has produced mixed findings regarding a single versus multiple factor structure of the MetSyn (Ferguson, et al., 2010; Pladevall, et al., 2006). It has been suggested that in part, multiple factor solutions might emerge simply because highly correlated indicators of a common pathway (e.g., blood pressure represented by SBP and DBP) tend to form distinct factors. However, when mean arterial pressure was included in place of SBP and DBP in the current study, the factor structure did not change (data not shown). Furthermore, bivariate associations showed that the blood pressure factor was weakly correlated with the lipids and metabolic factors, suggesting more than one physiological pathway. Few investigations have explored sex and race differences in the factor structure of the MetSyn, but a recent study suggests that gender-ethnic stratified models may be more appropriate than general models (Ferguson et al.). Examining the structure of the MetSyn in Mexican-American women is beyond the scope of the current study, particularly given the relatively small sample size. Nonetheless, the observed differences in the MetSyn structure across acculturation groups, even in this relatively homogenous sample, suggest the need for further research.
Significant, moderate correlations were observed between higher SES and higher psychosocial resources/lower risk across all samples. Statistically significant but modest inverse associations were found between SES and each MetSyn subcomponent in more acculturated participants; in contrast, SES was related significantly only to the “metabolic” MetSyn construct (i.e., fasting glucose and waist circumference) in less acculturated participants. Associations between psychosocial resources/risk and the MetSyn constructs were inconsistent. Lower psychosocial resources/higher risk related to higher levels on the central physiological components of the syndrome (i.e., abdominal obesity/fasting glucose), but only in more acculturated women. Finally, when considering aggregate information regarding descriptive fit, statistical fit, and parsimony, an indirect effects model with SES predicting the MetSyn latent factors through psychosocial resources/risk fit the data best for all samples. The mediated pathway from higher SES to lower levels on the metabolic factor (i.e., fasting glucose/waist circumference) via psychosocial resources/risk was statistically significant in the overall and more US-acculturated samples. The finding that psychosocial variables were most relevant to understanding metabolic aspects of the MetSyn is consistent with another study of Mexican-American women, which showed that psychosocial resources contributed to the association between SES and waist circumference but not other MetSyn components (Gallo et al., 2007)
Although a substantial body of research suggests an inverse association between SES and MetSyn risk, this relationship has seldom been tested in discrete Latino subgroups. Moreover, the “paradox” of better than expected health outcomes in Latinos (e.g., lower mortality rates) relative to non-Latino whites despite low SES, poor healthcare access, and other risks could imply resilience to adversity and risk, at least in some subgroups. Indeed, prior research shows that prevalence rates (Pabon-Nau, Cohen, Meigs, & Grant, 2010) and SES-gradients in cardiometabolic conditions (Gallo, Espinosa de los Monteros, et al., 2009; Karlamangla, et al., 2010) vary across different Latino sub-populations. In the current study we found a clearer SES-gradient in cardiometabolic health in the more-acculturated segment of our sample – a finding that has also been observed previously (Gallo, Espinosa de los Monteros, et al.; Kimbro, et al., 2008), but not consistently (Karlamangla, et al.). We also found that psychosocial factors were less germane to understanding SES-MetSyn associations in less-acculturated women. The scales assessing psychosocial resource and risk factors showed similar psychometric properties in both language versions, and a similar relationship with SES. However, because in general the psychosocial measures were not specifically developed for or adequately validated in Mexican-Americans of diverse SES, it is possible that they may be less sensitive to quantifying psychosocial risk in this population. Alternatively, other factors, such as culture-specific risks and resources (e.g. discrimination stress, strong family ties), structural influences on health (e.g., health care access, neighborhood environments) or lifestyle factors may play a larger role in SES-MetSyn associations in less-acculturated Mexican-Americans. Overall, these findings support the need for additional research that partitions the large, heterogeneous US Latino population into meaningful subgroups, to better understand their health and health disparities and to inform more effective prevention and intervention efforts.
Limitations
The current study was cross-sectional in design, which precludes determination of directionality. Although it seems more plausible that SES or psychosocial variables affect MetSyn than the reverse, there is some evidence indicating that these constructs are reciprocally related (e.g., Pulkki-Råback et al., 2009). Longitudinal studies (e.g., Matthews et al., 2008) can provide a more robust test of the hypothesized contributions of psychosocial factors to SES-health disparities. Limitations of measurement are also relevant to interpreting the current findings. As noted, psychosocial measures were not designed for this population and may be less sensitive to capturing health-related risks in Spanish-speaking (low-acculturated) women. Moreover, psychometric properties for some scales (self-esteem, pessimism) were not optimal, and the resulting error variance may have contributed to a reduction in statistical power. In addition, traditional markers of SES, such as education and income, may be less accurate measures of status in immigrants, and this may have contributed to less consistent associations of SES with cardiometabolic health in Spanish-speaking women. Alternative indicators of SES, such as subjective perceptions of social status, could be a useful adjunct to traditional markers in ethnic minority and immigrant samples (De Castro, Gee, & Takeuchi, 2009). The current analyses included a composite SES-measure that combined education and income, which, though a parsimonious approach that allowed modeling shared latent variance, obscured possible differences in pathways that might explain associations of income versus education with cardiometabolic risk. Level of acculturation was assessed with a single proxy marker, as a convenient method of exploring whether the socioeconomic gradients of interest varied by acculturation level. However, proxy indictors have limited sensitivity and lack the ability to elucidate the processes that link acculturation with health. A more nuanced consideration of the association of acculturation with cardiometabolic risk, and relevant explanatory pathways, was beyond the scope of the current study and will be the focus of future reports. The sample size was also relatively small, and this may have impeded our ability to identify psychosocial mechanisms where effect sizes for associations with parameters of the MetSyn were small. Finally, although the focus on a specific, well-characterized, gender-ethnic-regional subgroup helps to sharpen the lens through which to examine SES-effects in health, the findings should not be presumed to generalize to other Latino populations.
Conclusions
In conclusion, the current study adds to the small body of literature that has directly examined psychosocial factors as a pathway in the relationship between SES and cardiometabolic health, in a well-defined, at-risk population that has received little attention in the literature to date. SES showed a consistent, inverse association of small magnitude with all MetSyn variables in more US-acculturated women, but was inversely related only to central adiposity/glucose regulation in less US-acculturated individuals. Furthermore, the contributions of psychosocial resource and risk factors were limited to associations of SES with metabolic factors of the MetSyn, and to more acculturated individuals only. It is notable that central adiposity and insulin resistance form the primary pathophysiological pathways underlying the MetSyn, which supports the potential clinical relevance of these findings. Nonetheless, psychosocial factors are likely to represent only a single piece of the puzzle underlying socioeconomic gradients in cardiometabolic health. Additional pathways, such as healthcare access, health behaviors, social and physical features of environments, and neurobiological mechanisms, must also be considered in efforts to explain and intervene with health disparities.
Acknowledgements
This study was supported by grant number 1R01HL081604 (Gallo PI) from the National Heart Lung and Blood Institute, National Institutes of Health (NHLBI/NIH). Author Smriti Shivpuri was supported by 1T32HL079891 (NHLBI/NIH) and Karla Espinosa de los Monteros by F31HL087732 (NHLBI/NIH) during their work on the study. This research was also supported in part by grant number 1P20MD002293 (NCMHD/NIH), San Diego Partnership to Reduce Diabetes and CVD in Latinos. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of the NIH. We are grateful to Dr. Wendy Davila-Fraga, project manager, and all other research staff who assisted with this project. Sincere thanks are also due to the participants of “Nuestra Salud” for their invaluable contributions to this research.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea.
Exposure to stress is often highlighted as a potential mechanism in psychosocial perspectives on health disparities (Gallo & Matthews, 2003; Myers, 2009), although available empirical evidence is limited (Matthews & Gallo, 2010; Matthews, Gallo, & Taylor, 2010). In the current cohort, as in a prior study (Matthews et al., 2008), we found inconsistent evidence for an association between SES and stress. The pattern is complicated, varying according to measure type (e.g., chronic stress, life events, perceived stress) and domain (e.g., work related versus interpersonal stress). To allow more thorough attention to the complexity of these relationships, associations between SES and stress will be reported in a separate manuscript.
Although women with hypertension and treated diabetes were excluded from the study, three women were found to be taking blood pressure (n = 2) or glucose affecting (n = 1) medications for other reasons.
Contributor Information
Linda C. Gallo, San Diego State University
Addie L. Fortmann, San Diego State University
Scott C. Roesch, San Diego State University
Elizabeth Barrett-Connor, University of California at San Diego School of Medicine.
John P. Elder, San Diego State University
Karla Espinosa de los Monteros, San Diego State University.
Smriti Shivpuri, San Diego State University.
Paul J. Mills, University of California at San Diego School of Medicine
Gregory A. Talavera, San Diego State University
Karen A. Matthews, University of Pittsburgh School of Medicine
References
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Smith SC., Jr Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- Arias K, Eschbach K, Schauman WS, Backlund EL, Sorlie PD. The Hispanic mortality advantage and ethnic misclassification on US death certificates. American Journal of Public Health. 2010;100(S1):S171–S177. doi: 10.2105/AJPH.2008.135863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB., Jr The Cook-Medley hostility scale: Item content and ability to predict survival. Psychosomatic Medicine. 1989;51(1):46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- Bentler PM. On tests and indices for evaluating structural models. Personality & Individual Differences. 2007;42(5):4. [Google Scholar]
- Cruz TH, Marshall SW, Bowling JM, Villaveces AS. The validity of a proxy acculturation scale among U.S. Hispanics. Hispanic Journal of Behavioral Sciences. 2008;30(4):425–446. [Google Scholar]
- De Castro A, Gee G, Takeuchi D. Examining alternative measures of social disadvantage among Asian Americans: The relevance of economic opportunity, subjective social status, and financial strain for health. Journal of Immigrant and Minority Health. 2009;5:659–671. doi: 10.1007/s10903-009-9258-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M. Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESDR) In: Masten W, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. Mahwah, NJ: Lawrence Elrbaum; 1999. [Google Scholar]
- Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. National Health Statistics Reports. 2009;(13):1–7. [PubMed] [Google Scholar]
- Everson SA, Goldberg DE, Kaplan GA, Cohen RD, Pukkala E, Tuomilehto J, Salonen JT. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosomatic Medicine. 1996;58(2):113–121. doi: 10.1097/00006842-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annual Review of Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- Ferguson TF, Funkhouser E, Roseman J. Factor analysis of metabolic syndrome components in the Coronary Artery Risk Development in Young Adults (CARDIA) study: Examination of factors by race-sex groups and across time. Ann Epidemiol. 2010;20(3):194–200. doi: 10.1016/j.annepidem.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Diabetes Care. 2005;28(7):1769–1778. doi: 10.2337/diacare.28.7.1769. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Espinosa De Los Monteros K, Ferent V, Urbina J, Talavera G. Education, psychosocial resources, and metabolic syndrome variables in Latinas. Annals of Behavioral Medicine. 2007;34(1):14–25. doi: 10.1007/BF02879917. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Espinosa De Los Monteros K, Allison M, Diezroux AV, Polak JF, Morales LS. Do socioeconomic gradients in subclinical atherosclerosis vary according to acculturation level? Analyses of Mexican-Americans in the Multi-Ethnic Study of Atherosclerosis. Psychosomatic Medicine. 2009;71:756–762. doi: 10.1097/PSY.0b013e3181b0d2b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, Jiménez JA, Shivpuri S, Espinosa De Los Monteros K, Mills PJ. Domains of chronic stress, lifestyle factors, and allostatic load in middle-aged Mexican-American women. Annals of Behavioral Medicine. 2011;41(1):21–31. doi: 10.1007/s12160-010-9233-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Penedo FJ, Espinosa De Los Monteros K, Arguelles W. Resiliency in the face of disadvantage: Do Hispanic cultural characteristics protect health outcomes? Journal of Personality. 2009;77:1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: A systematic review and meta-analysis of longitudinal studies. Journal of the American College of Cardiology. 2007;49(4):403–414. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- Goldbacher EM, Matthews KA. Are psychological characteristics related to risk of the metabolic syndrome? Annals of Behavioral Medicine. 2007;34(3):240–253. doi: 10.1007/BF02874549. [DOI] [PubMed] [Google Scholar]
- Gonzalez MA, Rodriguez AF, Calero JR. Relationship between socioeconomic status and ischaemic heart disease in cohort and case-control studies: 1960–1993. International Journal of Epidemiology. 1998;27(3):350–358. doi: 10.1093/ije/27.3.350. [DOI] [PubMed] [Google Scholar]
- Grundy SM. Metabolic syndrome: Connecting and reconciling cardiovascular and diabetes worlds. Journal of the American College of Cardiology. 2006;47(6):1093–1100. doi: 10.1016/j.jacc.2005.11.046. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janicki-Deverts D, Cohen S, Doyle WJ. Cynical hostility and stimulated Th1 and Th2 cytokine production. Brain Behav Immun. 2010;24(1):58–63. doi: 10.1016/j.bbi.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlamangla AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001–2006. Annals of Epidemiology. 2010;20(8):617–628. doi: 10.1016/j.annepidem.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh A, Bentley RJ, Turrell G, Shaw J, Dunstan D, Subramanian SV. Socioeconomic position, gender, health behaviours and biomarkers of†cardiovascular disease and diabetes. Social Science & Medicine. 2010;71:1150–1160. doi: 10.1016/j.socscimed.2010.05.038. [DOI] [PubMed] [Google Scholar]
- Kimbro RT, Bzostek S, Goldman N, Rodriguez G. Race, ethnicity, and the education gradient in health. Health Affairs. 2008;27(2):361–372. doi: 10.1377/hlthaff.27.2.361. [DOI] [PubMed] [Google Scholar]
- Krantz DS, Mcceney MK. Effects of psychological and social factors on organic disease: A critical assessment of research on coronary heart disease. Annual Review of Psychology. 2002;53:341–369. doi: 10.1146/annurev.psych.53.100901.135208. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Kubzansky PE, Maselko J. Optimism and pessimism in the context of health: Bipolar opposites or separate constructs? Personality & Social Psychology Bulletin. 2004;30(8):943–956. doi: 10.1177/0146167203262086. [DOI] [PubMed] [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosomatic Medicine. 2005;67(6):846–854. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavioral Research Methods. 2007;39(3):384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? In: Adler N, editor. Annals of the New York Academy of Sciences. Vol. 1186. New York: The New York Academy of Sciences; 2010. pp. 146–173. The Biology of Disadvantage: Socioeconomic Status and Health) [DOI] [PubMed] [Google Scholar]
- Matthews KA, Räikkönen K, Gallo LC, Kuller LH. Association between socioeconomic status and metabolic syndrome in women: Testing the reserve capacity model. Health Psychology. 2008;27(5):576–583. doi: 10.1037/0278-6133.27.5.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Shumaker SA, Bowen DJ, Langer RD, Hunt JR, Kaplan RM, Ritenbaugh C. Women's Health Initiative. Why now? What is it? What's new? American Psychologist. 1997;52(2):101–116. doi: 10.1037//0003-066x.52.2.101. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus. Los Angeles: 2006. p. Muthén & Muthén. [Google Scholar]
- Myers HF. Ethnicity and socio-economic status-related stresses in context: An integrative conceptual model. Journal of Behavioral Medicine. 2009;32(1):9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- Neeley WE. Simple automated determination of serum or plasma glucose by a hexokinase/glucose-6-phosphate dehydrogenase method. Clin Chem. 1972;18(6):509–515. [PubMed] [Google Scholar]
- Pabon-Nau L, Cohen A, Meigs J, Grant R. Hypertension and diabetes prevalence among U.S. hispanics by country of origin: The National Health Interview Survey 2000–2005. Journal of General Internal Medicine. 2010;25(8):847–852. doi: 10.1007/s11606-010-1335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pladevall M, Singal B, Williams LK, Brotons C, Guyer H, Sadurni J, Haffner S. A single factor underlies the metabolic syndrome: A confirmatory factor analysis. Diabetes Care. 2006;29(1):113–122. doi: 10.2337/diacare.29.1.113. [DOI] [PubMed] [Google Scholar]
- Prescott E, Godtfredsen N, Osler M, Schnohr P, Barefoot J. Social gradient in the metabolic syndrome not explained by psychosocial and behavioural factors: Evidence from the Copenhagen City Heart Study. European Journal of Cardiovascular Prevention & Rehabilitation. 2007;14(3):405–412. doi: 10.1097/HJR.0b013e32800ff169. [DOI] [PubMed] [Google Scholar]
- Pulkki-Råback L, Elovainio M, Kivimäki M, Mattsson N, Raitakari OT, Puttonen S, Keltikangas-Jarvinen L. Depressive symptoms and the metabolic syndrome in childhood and adulthood: A prospective cohort study. Health Psychology. 2009;28(1):108–116. doi: 10.1037/a0012646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas R, Aguilar-Salinas CA, Jiménez-Corona A, Shamah-Levy T, Rauda J, Avila-Burgos L, Ponce EL. Metabolic syndrome in Mexican adults: Results from the National Health and Nutrition Survey 2006. Salud Publica de Mexico. 2010;52(Suppl 1):S11–S18. doi: 10.1590/s0036-36342010000700004. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality & Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, Zdaniuk B. The life engagement test: Assessing purpose in life. Journal of Behavioral Medicine. 2006;29(3):291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS Social Support Survey. Social Science & Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Simmons RG, Rosenberg F, Rosenberg M. Disturbance in the Self-Image at Adolescence. American Sociological Review. 1973;38(5):553–568. [PubMed] [Google Scholar]
- Smith TW, Glazer K, Ruiz JM, Gallo LC. Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. Journal of Personality. 2004;72(6):1217–1270. doi: 10.1111/j.1467-6494.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Sydeman SJ, Owen AE, Marsh BJ. Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI) In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 2nd ed. Mahwah, NJ: Erlbaum; 1999. pp. 993–1021. [Google Scholar]
- Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Social Science & Medicine. 2009;69(7):983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- Warnick GR. Measurement of cholesterol and other lipoprotein constituents in the clinical laboratory. Clinical Chemistry and Laboratory Medicine. 2000;38(4):287–300. doi: 10.1515/CCLM.2000.041. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology. 2000;30(1):165–200. [Google Scholar]